Abstract
Cell-based therapy is a promising strategy for the repair of spinal cord injury (SCI), and the synergic effects of donor cells are emphasized in recent years. In this study, epidermal neural crest stem cells (EPI-NCSCs) and olfactory ensheathing cells (OECs) were transplanted into the contused spinal cord of rats separately or jointly at 1 week after injury. At 3 and 9 weeks posttransplantation, migration of the donor cells, expression of brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF) and functional recovery of the contused cord were determined by techniques of histopathology, quantitative real-time polymerase chain reaction (qPCR), immunohistochemistry and Basso–Beattie–Bresnahan (BBB) score. The results showed that the migration and distribution of EPI-NCSCs in vivo were promoted by OECs at 3 weeks after transplantation, but they vanished at 9 weeks. The expression of BDNF and GDNF was significantly increased by co-transplantation at molecular and protein level. Although the expression of both factors in EPI-NCSCs- and OECs-injected group was lower than in co-injected group, it was higher than in control groups. Similarly, the best locomotor recovery of the contused cord was acquired from co-injected animals. As we know, this is the first time to study the synergic effects of EPI-NCSCs and OECs, and the data indicates that donor cells migration, expression of neurotrophic factors (NTFs), and recovery of motor function can be improved by EPI-NCSCs and OECs synergistically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord injury (SCI) comprises complex pathophysiological processes which result in complete or partial loss of sensation and mobility and affect the life qualities of patients. In recent years, many laboratories have reported that cell transplantation is a perspective strategy for treating SCI. Following SCI, cell transplantation into the lesion site is essential to provide permissive substrates for protecting nerve cell, decreasing apoptosis, promoting remyelination, and blocking cascade effect of inflammatory reaction (Antonic et al. 2013; Cui et al. 2013; Li et al. 2013). Different cell types, including olfactory ensheathing cells (OECs), Schwann cells (SCs), neural stem cells (NSCs), and marrow stroma cells (MSCs) have been used as donor cells for transplantation after SCI with variable degrees of success (Hooshmand et al. 2009; Quertainmont et al. 2012; Wang et al. 2012; Mayeur et al. 2013).
Epidermal neural crest stem cells (EPI-NCSCs), derived from the embryonic neural crest, is a strong candidate for cell-based therapy, because they combine the advantages of embryonic stem cells and adult stem cells. EPI-NCSCs transplantation is an attractive strategy for causing a significant improvement in sensory connectivity and touch perception following SCI, by expressing neurotrophic factors, angiogenic factors and extracellular proteases, which in combination have the capability of supporting cell survival, neovascularization and modulation of scar formation (Pandamooz et al. 2013). However, the poor migration of grafted EPI-NCSCs in the injured cord remains a major challenge (Sieber-Blum et al. 2006).
OECs play a central role in the repair of SCI due to their abundant production of growth-promoting factors and cell adhesion molecules. OECs have been reported to improve functional recovery via increase of the survival number of NSCs and axonal regeneration in vivo (Shukla et al. 2009). Moreover, OECs are a source of trophic factors, including nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), glial cell-derived neurotrophic factor (GDNF), and ciliary neurotrophic factor (CNTF). They communicate with their environment in virtue of these trophic molecules (Radtke and Kocsis 2012). Importantly, migration of OECs in the injured spinal cord is more active as they induce less astrocyte response in vitro and in vivo and mingle with astrocyte after injection (Santos-Silva et al. 2007; Li et al. 2012).
Recently, it is presumed that combination of two kinds of cells may cause the synergistic effects on repair of SCI (Ban et al. 2011; Gerin et al. 2011). In the present study, EPI-NCSCs and OECs were transplanted into the contused spinal cord separately or jointly at 1 week after injury for determining whether OECs promote EPI-NCSCs migration, and their synergistic effects on the expression of BDNF and GDNF and the recovery of motor function of a clinically relevant model of the contusive SCI.
Materials and Methods
Preparation of EPI-NCSCs
EPI-NCSCs were isolated from whisker follicles of adult green fluorescence protein (GFP) rat according to the previous description (Sieber-Blum and Hu 2008; Zhang et al. 2012). Simply, whisker follicles were dissected from adult GFP transgenic rats. Tissue was cleaned, cut first longitudinally and subsequently transversely on cavernous sinus and ring sinus. The bulges were rolled out of the capsule and placed onto collagen-coated culture plates where they adhered to the substratum within 30 min, then the culture medium consisted of 85 % Dulbecco’s Modified Eagle’s Medium (DMEM)/F12, 10 % fetal calf serum, 2 % B27 (all from Gibco, Grand Island, NY, USA), and 10 ng/ml of basic fibroblast growth factor (bFGF, Sigma-Aldrich, St. Louis, MO, USA) was added. On the third day, cells started to emigrate from the bulge explants onto the culture substratum. Afterwards, the bulges were removed and the adhering cells detached by trypsin (Gibco, Grand Island, NY, USA) treatment and subsequently subcultured. It has been shown previously that these cells consist of a pure population of EPI-NCSCs confirmed by the immunohistochemistry staining of nestin, SOX10, and β-III tubulin antibody (all from Gibco, Grand Island, NY, USA). The suspension was collected and adjusted at the concentration of 1.0 × 105/ul for transplantation.
Preparation of OECs
OECs were generated from the olfactory bulbs of adult GFP rats as described previously (Sasaki et al. 2004; Li et al. 2012). Briefly, the olfactory bulbs removed from adult GFP rats were dissected free of meninges and white matter, minced with scalpel blades, and incubated for 25 min in trypsin at 37 °C within the CO2 incubator. Then tissue was dissociated with a very gentle mechanical trituration, washed, and placed in a culture flask in DMEM/F12 medium with 10 % fetal calf serum, 10 ng/ml bFGF, and 2 uM Forskolin (Sigma-Aldrich, St. Louis, MO, USA). After 5–7 days, antibody staining consistently showed that at least 95 % of donor cells were both P75 (1:200 dilution) and S-100 (1:500 dilution; all from Abcam, Cambridge, MA, USA) positive. The suspension was collected and adjusted at the concentration of 1.0 × 105/ul for transplantation.
Spinal Cord Injury and Animal Groups
Adult male Sprague Dawley (SD) rats (200–250 g) were housed according to the Third Military Medical University (TMMU) guidelines, and surgical procedures and postop care were performed in accordance with protocols approved by TMMU Institutional Animal Care and Use Committee. Rats were anesthetized with a single intraperitoneal injection of 1 % pentobarbital (30 mg/kg), and a sterile laminectomy was performed at vertebral levels T10. The spinal cords were contused using an NYU II impactor with a dropping weight 10.0 g from 25 mm above the exposed cord. After injury, the muscle and skin were closed in layers. The procedure resulted in hind limb paralysis in all animals, and some of them suffered hematuria and urinary retention. To prevent the infections, Bicillin (60,000 U/kg, i.m.) was given daily for 7 days with bladder expression twice a day until recovery of the urinate function.
The contused rats were randomly divided into five groups (n = 20/group). Group A was the blank control without transplantation. Group B was injected of 6 ul DMEM/F12. Groups C, D, and E were transplanted with 6 ul suspension of EPI-NCSCs, OECs, and mixed EPI-NCSCs-OECs, respectively, at day 7 after injury.
Cell Transplantation
The transplantation was performed at day 7 after spinal cord injury. The rats were anesthetized again as above and the laminectomy site was re-exposed. Two microliters of cell suspension were injected along the midline of the contused cord at a depth of 0.8 mm at the epicenter of the lesion, and at 1 mm rostral and caudal to the epicenter; a total of 6 μl of cell suspension was used. The cell injections were performed using a 5-ul Hamilton syringe, which remained in place for 5 min after each injection. The control animals were injected at identical volumes of DMEM/F12 at the same sites. After the injection, the muscle and skin were closed with interrupted sutures. Cyclosporin A (10 mg/kg, i.m.) was given daily until euthanasia.
Immunofluorescent Staining and Measurement of the Donor Cells
Three and 9 weeks posttransplantation, the rat spinal cord was perfused and fixed with 4 % paraformaldehyde and postfixed in the same fixative for 24 h, then transferred to 20 % sucrose for 48 h. Segments of the spinal cord (between the T9 and T11) were embedded in optimal cutting temperature compound (OCT, Boster, Wuhan, China) and cut longitudinally on a cryostat (LEICA CM-1900, GE) into serial 15-μm-thick sagittal frozen sections.
The frozen slides were air dried at room temperature for 10 min and washed with PBS for 10 min. Then they were blocked with 3 % bovine serum albumin (BSA) containing 0.3 % Triton X-100 for 1 h at room temperature and incubated in anti-S-100 antibody (1:500 dilution), anti-β-III tubulin antibody (1:1,000 dilution), and anti-nestin polyclonal antibody (1:1,000 dilution; all from Gibco, Grand Island, NY, USA) overnight at 4 °C. The slides were washed in PBS three times and incubated with fluorescein-conjugate affinipure (FITC) goat anti-rabbit IgG (1:100 dilution) for 2 h at 37 °C. After repeat washing with PBS, the slides were incubated with Hoechst 33342 (1:100 dilution; all from Boster, Wuhan, China) for 30 min at 37 °C and coverslipped with Gel/Mount aqueous mounting media. The sections were observed under fluorescence microscope (Olympus BX50, JPN). For measuring the distribution area, the migration distances and the number of fluorescence cells, images were randomly captured at ×20 under Olympus BX50 light microscope from every fifth section, for a total of five sections from each animal, then montaged by Adobe Photoshop 10.0 and measured by Spot 345 software.
Quantitative Real-Time Polymerase Chain Reaction
According to the mRNA sequence of GDNF and BDNF (http://www.ncbi.nlm.nih.gov/genbank), the primers (Table 1) were designed by the GeneTool software (Biotools, USA). The spinal cord segments (about 10 mm) centered on the injury site were obtained at 3 and 9 weeks after SCI (n = 5/group/time point). They were extracted with TRIzol reagent and DNaseI (all from Invitrogen, Carlsbad, CA, USA). First strand complementary DNA (cDNA) was synthesized using the Rever Tre Ace-a-reverse transcription kit (Toyobo, JPN) according to manufacturer’s instructions. For quantitative PCR (qPCR), 20 μl reactions consisted of 10 μl 2× SYBR Green, 2 μl cDNA template, and 0.5 μl RT-qPCR Primer Set were used. Thermo cycling conditions were as follows: 94 °C for 5 min, 30 cycles of 94 °C for 30 s, 55 °C for 30 s, 72 °C for 30 s, and 72 °C for 10 min. Melting curve analysis showed a single amplification peak for each reaction. Ct values for targets were expressed as relative expression compared to the average of housekeeping genes (β-actin).
Immunohistochemical Staining of BDNF and GDNF
The frozen slides were air dried at room temperature for 10 min and washed with PBS for 10 min (n = 5/group/time point). The sections were permeabilized and blocked with 0.3 % Triton X-100/10 % normal goat serum in 0.01 M PBS for 30 min, then incubated with polyclonal rabbit antibodies anti-BDNF (1:500 dilution) and anti-GDNF (1:500 dilution) overnight at 4 °C. The sections were incubated with secondary biotinylated goat anti-rabbit IgG antibody (1:1,000 dilution; Abcam, Cambridge, MA, USA) for 1 h at room temperature, followed by an avidin–biotin–peroxidase complex (ABC kit, Thermo Fisher Scientific, Rockford, IL, USA). After incubation for 5 min with 0.02 % DAB (Boster, Wuhan, China) and 0.003 % H2O2, the sections were counterstained with hematoxylin. Primary antibody omission controls were used in order to confirm the specificity of the immunohistochemical labeling. The sections were observed under light microscope, then digital images were randomly taken at ×40 from every fifth section in total of five sections from each animal. The positive area of BDNF and GDNF was measured with Spot 345 software and compared with that of the blank control group. The percentage of the positive area in each group to blank control group was calculated.
Assessment of Locomotor Behavior
The locomotor behavior of each rat was assessed weekly until 9 weeks after transplantation using the Basso–Beattie–Bresnahan (BBB) hindlimb locomotor rating scale (n = 10/group) (Basso et al. 1995). The BBB rating scale is a 21-point system based on operationally defined behavioral features that follow the recovery progression from complete paralysis to normal locomotion. The rating scale ranges from 0 to 21, in which score 0 indicates complete hindlimb paralysis, while score 21 denotes completely normal locomotor function. Scores of 1–20 indicate an animal’s altered ability to move the hindlimb joints, to bear weight, and to coordinate forelimb and hindlimb movement.
Statistical Analysis
All values are expressed as mean ± standard deviation (SD). Differences between groups were examined for statistical significance using one-way factorial analysis of variance (ANOVA). A p value <0.05 denoted the presence of a significant difference. The above tests were conducted using SPSS software version 11.0 (SPSS Inc., Chicago, IL, USA).
Results
Survival, Migration, and Distribution of OECs and EPI-NCSCs
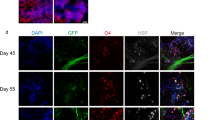
Representative longitudinal sections showed the survival, migration, and distribution of grafted GFP+ cells in the contused spinal cord (Fig. 1). At 3 weeks after transplantation, the green donor cells gathered as masses at injection site in EPI-NCSCs-injected group, lacking migration, and the boundary of graft EPI-NCSCs was clear from the surrounding tissue (Fig. 1a). For OECs-injected group, the donor cells migrated extensively, integrated with the host tissue, and distributed widely (Fig. 1b). For co-injected group, the mixed donor cells migrated from injection site along the longitudinal axis of the host cord and formed cell beam between the injection sites for crossing the injured area (Fig. 1c).
At 3 weeks posttransplantation, migration and distribution of EPI-NCSCs and OECs in the contused cord on the longitudinal frozen sections. a EPI-NCSCs group. b OECs group. c co-transplantation group. A1–C3 were higher magnification of boxed area in a–c. A1–C1 showed GFP+ graft cells. A2–C2 indicated nuclei stained by Hoechst 33342. A3–C3 were merged pictures of GFP+ and Hoechst 33342+. d Semi-quantification of distribution area, migration distance, and number of graft cells. Scale bars a–c = 200 μm, A1–C3 = 50 μm
Semi-quantification data showed that at 3 weeks, the distribution area was 0.342 ± 0.057 mm2 with the migration distance of 0.399 ± 0.071 mm in the EPI-NCSCs group, which was significantly different from 0.626 ± 0.124 mm2 and 1.710 ± 0.223 mm in the OECs group and 0.636 ± 0.182 mm2 and 1.816 ± 0.563 mm in the co-transplantation group (p < 0.05). At 9 weeks, since the number of survival green fluorescence cells was obviously decreased in each group, even no survival green fluorescence cells could be observed in the EPI-NCSCs group, the distribution area and migration distance were only measured in OECs and co-transplantation group. The results indicated that the area and the distance were 0.497 ± 0.082 mm2 and 2.004 ± 0.479 mm in the OECs group and 0.016 ± 0.012 mm2 and 0.301 ± 0.147 mm in the co-transplantation group.
The number of graft cells was more in co-transplantation group than in OECs group, subsequently in EPI-NCSCs group at 3 weeks. As only EPI-NCSCs can be labeled by β-III tubulin and nestin (Hu et al. 2006; Sieber-Blum and Hu 2008), and only OECs can be labeled by S-100 (Sasaki et al. 2004), at 3 weeks, the sections were immunostained for β-III tubulin+/GFP+, nestin+/GFP+, or S-100−/GFP+ for identifying EPI-NCSCs and β-III tubulin−/GFP+, nestin−/GFP+, or S-100+/GFP+ for grafted OECs. The cells count showed that the proportion of EPI-NCSCs was 37.9± 9.2 %, and the others were OECs (Fig. 2).
Expression of BDNF and GDNF
qPCR (Fig. 3) and immunoassaying (Fig. 4) were performed to evaluate the effects of the donor cells on the expression of BDNF and GDNF at molecular and protein levels in the injured cord. In the co-transplanted group, the expression of BDNF and GDNF at both levels was remarkably increased compared with the control group and individual cell transplantation group at 3 weeks posttransplantation (p < 0.05). Whereas, the expression of both factors in co-transplantation group was attenuated at 9 weeks compared with 3 weeks. There was no statistical difference among cell transplantation groups at 9 weeks posttransplantation (p > 0.05).
Immunohistochemical staining of BDNF and GDNF at 3 and 9 weeks after transplantation. (Column A) BDNF at 3 weeks. (Column B) BDNF at 9 weeks. (Column C) GDNF at 3 weeks. (Column D) GDNF at 9 weeks. (A1–D1) the blank control. (A2–D2) DMEM/F12. (A3–D3) EPI-NCSCs. (A4–D4) OECs. (A5–D5) the co-transplantation. (E) Semi-quantification of BDNF. (F) Semi-quantification of GDNF. Scale bars = 100 μm
Locomotor BBB Scores
All animals exhibited gradual improvements in hind limb locomotor function during the 9-week recovery period. The best BBB scores resulted from the co-injected animals, then orderly from the OECs- and EPI-NCSCs-injected animals. BBB scores for cell-injected rats differed significantly from the controls at p < 0.01and p < 0.05 for early and late weeks (Fig. 5).
Discussion
It is widely known that SCI can result in a series of pathophysiological changes including apoptosis and nerve cells loss (Rodriguez-Barrera et al. 2013). In recent years, cell transplantation for treating SCI has been an interesting subject, in which the transplanted cells modulating microenvironment for axon regeneration by secreting neurotrophic factors (NTFs) is one of major mechanisms (Rich 1992; Zhao et al. 2004). EPI-NCSCs replacement can be a promising strategy for SCI repair. However, the poor migration of grafted EPI-NCSCs in the injured cord remains a major challenge, which limits its use as a donor cell for the repair of SCI (Sieber-Blum et al. 2006). Cell migration is a fundamental process during the repair of SCI, because grafted cells are usually replaced in sites that differ from those in which they eventually reside (Liu and Rao 2003). Thus, strategies aimed at enhancing the migration of grafted EPI-NCSCs should be very important. It has been well established that OECs express and secret many growth factors and chemotactic factors, including GDNF, NGF, BDNF, and CNTF (Woodhall et al. 2001; Yin et al. 2013). These secreted factors may be required for the growth and the migration of EPI-NCSCs (Sadan et al. 2008; Cornejo et al. 2014; Rosenblum et al. 2014). Hence, in this study, EPI-NCSCs and OECs were co-transplanted into the contused spinal cord at 1 week after injury, showing that the ability of migration of EPI-NCSCs in vivo was enhanced when transplanted with OECs together. The expression of BDNF and GDNF was remarkably increased by the synergism of both grafted cells. Furthermore, co-transplantation of EPI-NCSCs and OECs promoted functional recovery after SCI.
In the present study, it has been semi-quantitatively demonstrated that OECs significantly increased the migratory distance and distribution area of EPI-NCSCs in vivo, but not survival time. Previously, it has been reported that the migratory process are controlled by various factors, and BDNF/GDNF appear as a promising candidate (Mitsuhara et al. 2013). Both factors play an important role in migration of neural stem cells via the manner of time-dependent (Hwang et al. 2009). GDNF receptors are expressed along the migratory pathway (Paratcha et al. 2003). By qPCR assay and immunohistochemical staining, we found that the expression of BDNF and GDNF at both molecular and protein levels was increased by the co-transplantation. Simultaneously, migratory distance of EPI-NCSCs was longer compared to itself transplantation alone. Regarding the mechanism of BDNF and GDNF promoting EPI-NCSCs to migrate, it cannot be answered by this study. It may be related to neurotrophic factors transferring an external signal membrane surface recipient to intracellular and forming pseudopodia in a particular direction to movement (Mitsuhara et al. 2013). Furthermore, the direction of the concentration gradient of NTFs may be also related to the cell migration (Paratcha et al. 2006). BDNF and GDNF mediate these effects via two main signaling receptors, the tyrosine-kinase receptor trkB and the neural cell adhesion molecule (NCAM) (Kaplan and Miller 2000; Paratcha and Ledda 2008). It is known that NCAM can affect these ligand–receptor interactions (Rutishauser 2008). In fact, NCAM has been shown to facilitate the interaction of NTFs with trkB (Muller et al. 2000; Vutskits et al. 2001) and to regulate the expression of p75 (Gascon et al. 2007), thereby modulating the neuronal sensitivity to the trophin. NCAM has been reported to mediate NTFs chemoattractive effect on the migration of enteric and rostral migratory stream neurons, respectively (Natarajan et al. 2002; Paratcha and Ledda 2008).
It is important to answer that how can co-transplantation promote the expression of BDNF and GDNF? Unfortunately, the answer could not be provided by the present data. However, it can be suggested that the interaction of OECs and EPI-NCSCs in the contused cord may promote the autocrine and paracrine of NTFs from the donor cells and the host neural elements, eventually cause higher expression of BDNF and GDNF (Nicolas et al. 2014). Previous studies reported that OECs transplantation can protect injured spinal cord neurons via the downregulation of semaphorin 3A (Sema3A) expression (Wang et al. 2011). Sema3A is an axon growth-mediated factor that has been shown to promote neuronal death and apoptosis, as well as inhibiting axonal regeneration after spinal cord injury via plexinA3 (Ben-Zvi et al. 2008a, b). Besides, Sema3A suppresses the secretion of nerve growth factor through the modulation of the TrkA signaling pathway, subsequently hindering the growth cone and inhibiting axonal regeneration (Ben-Zvi et al. 2008a, b). Although these speculation should be confirmed in the future study, the present results indicated that synergic effects of the donor cells on their migration and NTFs expression was existed.
BDNF and GDNF are necessary for neural regeneration and protecting spared tissue, then for functional recovery (Lang et al. 2013). Both neurotrophic factors play an important regulatory role in neural development, neuron survival, axonal growth, and synaptic remodeling (Hawryluk et al. 2012). Besides promoting neuronal regeneration and blocking nerve cell degeneration consequently improving structure and function of injured spinal cord, they also regulate acetylcholine and dopamine neurotransmitter release (Deng et al. 2013). The results of qPCR and immunohistochemistry in this study revealed that the expression of BDNF and GDNF was the highest in the co-transplantation group, then orderly the cell-injected and the control groups. Although their expression were decreased in the co-transplantation group at 9 weeks compared to 3 weeks may caused by the vanishing of EPI-NCSCs, the co-injected animals got the best performance recovery, suggesting that function repair can be mediated via the BDNF and GDNF, which could be enhanced by synergic effects of EPI-NCSCs and OECs, rather than only the cell replacement.
For cell-based therapy of SCI, both active migration of donor cells and adequate NTFs within the injured spinal cord are essential to establish a permissive environment for promoting neural regeneration, inhibiting scar formation, and blocking necrosis of neurons (Roloff et al. 2013). The nerve degeneration and the neuron death after SCI can be rescued by neurotrophic factors from peripheral target tissue and injured neuron (Wrathall et al. 1998). When the axonal transport being interrupted and survival neurons competing for neurotrophic factors, NTFs must be insufficient for neural regeneration and functional recovery (Fouad et al. 2013). By providing exogenous and endogenous NTFs, the recovery of the structure and the function of injured spinal cord can be improved (Gould and Oppenheim 2004). In this study, cell migration especially for EPI-NCSCs was enhanced by higher expression of BDNF and GDNF mediated by synergic effects of the co-transplantation, consequently motor function of the injured rats was improved.
In summary, this study confirmed previous report that neurotrophic factors are important for repairing the injured spinal cord. However, it was further demonstrated that co-transplantation of OECs and EPI-NCSCs could enhance migration of the donor cells and the expression of BDNF and GDNF, and subsequently improve locomotor recovery of the contused rats.
References
Antonic A, Sena ES, Lees JS et al (2013) Stem cell transplantation in traumatic spinal cord injury: a systematic review and meta-analysis of animal studies. PLoS Biol 11(12):e1001738
Ban DX, Ning GZ, Feng SQ et al (2011) Combination of activated Schwann cells with bone mesenchymal stem cells: the best cell strategy for repair after spinal cord injury in rats. Regen Med 6(6):707–720
Basso DM, Beattie MS, Bresnahan JC (1995) A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma 12(1):1–21
Ben-Zvi A, Ben-Gigi L, Yagil Z et al (2008a) Semaphorin3A regulates axon growth independently of growth cone repulsion via modulation of TrkA signaling. J Cell Signal 20(3):467–479
Ben-Zvi A, Manor O, Schachner M et al (2008b) The Semaphorin receptor PlexinA3 mediates neuronal apoptosis during dorsal root ganglia development. J Neurosci 28(47):12427–12432
Cornejo M, Nambi D, Walheim C et al (2014) Erratum to: effect of NRG1, GDNF, EGF and NGF in the migration of a Schwann cell precursor line. Neurochem Res 39(5):985–986
Cui X, Chen L, Ren Y et al (2013) Genetic modification of mesenchymal stem cells in spinal cord injury repair strategies. Biosci Trends 7(5):202–208
Deng LX, Deng P, Ruan Y et al (2013) A novel growth-promoting pathway formed by GDNF-overexpressing Schwann cells promotes propriospinal axonal regeneration, synapse formation, and partial recovery of function after spinal cord injury. J Neurosci 33(13):5655–5667
Fouad K, Bennett DJ, Vavrek R, Blesch A (2013) Long-term viral brain-derived neurotrophic factor delivery promotes spasticity in rats with a cervical spinal cord hemisection. Front Neurol 4:187
Gascon E, Vutskits L, Jenny B, Durbec P, Kiss JZ (2007) PSA-NCAM in postnatally generated immature neurons of the olfactory bulb: a crucial role in regulating p75 expression and cell survival. Development 134:1181–1190
Gerin CG, Madueke IC, Perkins T et al (2011) Combination strategies for repair, plasticity, and regeneration using regulation of gene expression during the chronic phase after spinal cord injury. Synapse 65(12):1255–1281
Gould TW, Oppenheim RW (2004) The function of neurotrophic factor receptors expressed by the developing adductor motor pool in vivo. J Neurosci 24(19):4668–4682
Hawryluk GW, Mothe A, Wang J, Wang S, Tator C, Fehlings MG (2012) An in vivo characterization of trophic factor production following neural precursor cell or bone marrow stromal cell transplantation for spinal cord injury. Stem Cells Dev 21(12):2222–2238
Hooshmand MJ, Sontag CJ, Uchida N, Tamaki S, Anderson SJ, Cummings BJ (2009) Analysis of host-mediated repair mechanisms after human CNS-stem cell transplantation for spinal cord injury: correlation of engraftment with recovery. PLoS ONE 4(6):e5871
Hu YF, Zhang ZJ, Sieber-blum M (2006) An epidermal neural crest stem cell (EPI-NCSC) molecular signature. Cells 24:2692–2702
Hwang DH, Kim BG, Kim EJ (2009) Transplantation of human neural stem cells transduced with Olig2 transcription factor improves locomotor recovery and enhances myelination in the white matter of rat spinal cord following contusive injury. BMC Neurosci 10:117
Kaplan DR, Miller FD (2000) Neurotrophin signal transduction in the nervous system. Curr Opin Neurobiol 10:381–391
Lang BC, Zhang Z, Lv LY et al (2013) OECs transplantation results in neuropathic pain associated with BDNF regulating ERK activity in rats following cord hemisection. BMC Neurosci 14:80
Li BC, Xu C, Zhang JY, Li Y, Duan ZX (2012) Differing Schwann cells and olfactory ensheathing cells behaviors, from interacting with astrocyte, produce similar improvements in contused rat spinal cord’s motor function. J Mol Neurosci 48(1):35–44
Liu G, Rao Y (2003) Neuronal migration from the forebrain to the olfactory bulb requires a new attractant persistent in the olfactory bulb. J Neurosci 23(16):6651–6659
Li Y, Zhang L, Zhang JY, Liu Z, Duan ZX, Li BC (2013) Morphological study of Schwann cells remyelination in contused spinal cord of rats. Chin J Traumatol 16(4):225–229
Mayeur A, Duclos C, Honore A et al (2013) Potential of olfactory ensheathing cells from different sources for spinal cord repair. PLoS ONE 8(4):e62860
Mitsuhara T, Takeda M, Yamaguchi S et al (2013) Simulated microgravity facilitates cell migration and neuroprotection after bone marrow stromal cell transplantation in spinal cord injury. Stem Cell Res Ther 4(2):35
Muller D, Djebbara-Hannas Z, Jourdain P et al (2000) Brain-derived neurotrophic factor restores long-term potentiation in polysialic acid-neural cell adhesion molecule-deficient hippocampus. Proc Natl Acad Sci U S A 97:4315–4320
Natarajan D, Marcos-Gutierrez C, Pachnis V, de Graaff E (2002) Requirement of signalling by receptor tyrosine kinase RET for the directed migration of enteric nervous system progenitor cells during mammalian embryogenesis. Development 129:5151–5160
Nicolas G, Robin JMF, Nick DJ (2014) Cell therapy for spinal cord injuries: what is really going on? Neuroscientist 1:1–16
Paratcha G, Ibanez CF, Ledda F (2006) GDNF is a chemoattractant factor for neuronal precursor cells in the rostral migratory stream. Mol Cell Neurosci 31(3):505–514
Paratcha G, Ledda F (2008) GDNF and GFRalpha: a versatile molecular complex for developing neurons. Trends Neurosci 31:384–391
Paratcha G, Ledda F, Ibanez CF (2003) The neural cell adhesion molecule NCAM is an alternative signaling receptor for GDNF family ligands. Cell 113(7):867–879
Pandamooz S, Naji M, Alinezhad F, Zarghami A, Pourghasem M (2013) The influence of cerebrospinal fluid on epidermal neural crest stem cells may pave the path for cell-based therapy. Stem Cell Res Ther 4(4):84
Quertainmont R, Cantinieaux D, Botman O, Sid S, Schoenen J, Franzen R (2012) Mesenchymal stem cell graft improves recovery after spinal cord injury in adult rats through neurotrophic and pro-angiogenic action. PLoS ONE 7(6):e39500
Radtke C, Kocsis JD (2012) Peripheral nerve injuries and transplantation of olfactory ensheathing cells for axonal regeneration and remyelination: fact or fiction? Int J Mol Sci 13(10):12911–12924
Rich KM (1992) Neuronal death after trophic factor deprivation. J Neurotrauma Suppl 1:S61–S69
Rodriguez-Barrera R, Fernandez-Presas AM, Garcia E et al (2013) Immunization with a neural-derived peptide protects the spinal cord from apoptosis after traumatic injury. Biomed Res Int 2013:827517
Roloff F, Ziege S, Baumgartner W, Wewetzer K, Bicker G (2013) Schwann cell-free adult canine olfactory ensheathing cell preparations from olfactory bulb and mucosa display differential migratory and neurite growth-promoting properties in vitro. BMC Neurosci 14:141
Rosenblum S, Smith TN, Wang N. et al. (2014) BDNF pre-treatment of human embryonic-derived neural stem cells improves cell survival and functional recovery after transplantation in hypoxic-ischemic stroke. Cell Transplant. Epub ahead of print
Rutishauser U (2008) Polysialic acid in the plasticity of the developing and adult vertebrate nervous system. Nat Rev Neurosci 9:26–35
Sadan O, Shemesh N, Barzilay R et al (2008) Migration of neurotrophic factors-secreting mesenchymal stem cells toward a quinolinic acid lesion as viewed by magnetic resonance imaging. Stem Cells 26(10):2542–2551
Santos-Silva A, Fairless R, Frame MC et al (2007) FGF/heparin differentially regulates Schwann cell and olfactory ensheathing cell interactions with astrocytes: a role in astrocytosis. J Neurosci 27(27):7154–7167
Sasaki M, Lankford KL, Zemedkun M, Kocsis JD (2004) Identified olfactory ensheathing cells transplanted into the transected dorsal funiculus bridge the lesion and form myelin. J Neurosci 24:8485–8493
Shukla S, Chaturvedi RK, Seth K, Roy NS, Agrawal AK (2009) Enhanced survival and function of neural stem cells-derived dopaminergic neurons under influence of olfactory ensheathing cells in parkinsonian rat. J Neurochem 109(2):436–451
Sieber-Blum M, Hu Y (2008) Mouse epidermal neural crest stem cell (EPI-NCSC) cultures. J. Vis. Exp. 9(15), pii:772
Sieber-Blum M, Schnell L, Grim M, Hu YF, Schneider R, Schwab ME (2006) Characterization of epidermal neural crest stem cell (EPI-NCSC) grafts in the lesioned spinal cord. Mol Cell Neurosci 32(1–2):67–81
Vutskits L, Djebbara-Hannas Z, Zhang H et al (2001) PSA-NCAM modulates BDNF-dependent survival and differentiation of cortical neurons. Eur J Neurosci 13:1391–1402
Wang GY, He XJ, Yuan PW, Li HP, Chang R (2011) Semaphorin 3A expression in spinal cord injured rats after olfactory ensheathing cell transplantation. Neural Regeneration Res 6(10):756–761
Wang Y, Teng HL, Huang ZH (2012) Intrinsic migratory properties of cultured Schwann cells based on single-cell migration assay. PLoS ONE 7(12):e51824
Woodhall E, West AK, Chuah MI (2001) Cultured olfactory ensheathing cells express nerve growth factor, brain-derived neurotrophic factor, glia cell line-derived neurotrophic factor and their receptors. Brain Res Mol Brain Res 88(1–2):203–213
Wrathall JR, Li W, Hudson LD (1998) Myelin gene expression after experimental contusive spinal cord injury. J Neurosci 18(21):8780–8793
Yin DP, Liu L, Cao L (2013) Synergetic effects of ciliary neurotrophic factor and olfactory ensheathing cells on optic nerve reparation. Zhonghua Yan Ke Za Zhi 49(11):1020–1028
Zhao Z, Alam S, Oppenheim RW, Prevette DM, Evenson A, Parsadanian A (2004) Overexpression of glial cell line-derived neurotrophic factor in the CNS rescues motoneurons from programmed cell death and promotes their long-term survival following axotomy. Exp Neurol 190(2):356–372
Zhang JY, Chen LZ, Duan ZX, Li BC (2012) Culture and morphologic characteristics of epidermal neural crest stem cell isolated from GFP adult rat. Chongqing yi xue 41(33):3471–3475
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (81371341), Special Funds for Major State Basic Research Project, China (2012CB518106), and Funds of the State Key Laboratory of Trauma, Burn and Combined Injury (SKLZZ201003).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, J., Liu, Z., Chen, H. et al. Synergic Effects of EPI-NCSCs and OECs on the Donor Cells Migration, the Expression of Neurotrophic Factors, and Locomotor Recovery of Contused Spinal Cord of Rats. J Mol Neurosci 55, 760–769 (2015). https://doi.org/10.1007/s12031-014-0416-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-014-0416-2