Abstract
Purpose
Nearly one-third of patients diagnosed with colorectal cancer (CRC) will ultimately develop metastatic disease. While a small percentage of patients can be considered for curative resection, more patients have limited disease that can be considered for local therapy. Challenges remain in defining oligometastatic CRC as well as developing treatment strategies guided by high level evidence.
Methods
In this review, we present the challenges in defining oligometastatic CRC and summarize the current literature on treatment and outcomes of local therapy in patients with metastatic CRC.
Results
For patients with liver- and/or lung-confined CRC metastases, surgical resection is the standard of care given the potential for long-term progression-free and overall survival. For patients with liver- or lung-confined disease not amenable to surgical resection, non-surgical local therapies, such as thermal ablation, hepatic arterial infusion pump (HAIP), or stereotactic body radiation therapy (SBRT), should be considered. For patients with more advanced disease, such as lymph node or bony metastases, the role of metastasis-directed therapy is controversial. Emerging data suggests that SBRT to ablate all metastases can improve progression-free and overall survival.
Conclusion
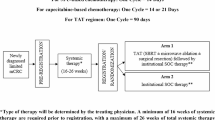
Multidisciplinary management is critical for patients with metastatic CRC due to the complexity of their cases and the nuanced patient, tumor, biological, and anatomical factors that must be weighed when considering local therapy. High-quality prospective randomized data in CRC are needed to further clarify the role of local ablative therapy in patients with unresectable oligometastatic CRC with ongoing studies including the RESOLUTE trial (ACTRN12621001198819) and the upcoming NCTN ERASur trial (NCT05673148).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) remains the second leading cause of cancer-related death in the USA with an estimated 150,000 new diagnoses and over 52,000 deaths in 2022 [1]. Approximately 20–25% of patients present with metastatic disease at diagnosis and another nearly 20% develop metastatic disease following curative treatment [2]. A minority of patients with metastatic disease are eligible for curative-intent resection, but many patients develop a limited number of metastatic lesions that might be considered for local therapy [3].
Despite significant retrospective data showing the benefit of local therapy in patients with metastatic CRC (mCRC), primarily in those with liver-only metastases, little prospective data exists to guide management. In addition, with advances in imaging, systemic therapy, and local therapy (including surgery and ablative modalities), an ever-increasing number of metastatic lesions can be detected and treated with local therapy. Challenges remain in defining oligometastatic CRC and determining who should be considered for local or regional therapy. The purpose of this manuscript is to review current definitions of oligometastatic cancer, place CRC in context of those definitions, and summarize the current literature describing treatment and outcomes of local therapy in patients with mCRC.
Defining Oligometastatic Colorectal Cancer
One challenge is in the very definition of oligometastatic disease. It may be nearly impossible to craft a uniform definition applicable for all disease histologies and tumor biology. So, imaging currently serves as the mainstay for defining oligometastatic disease [4]. Experts from the European Society for Radiotherapy and Oncology (ESTRO) and the American Society for Radiation Oncology (ASTRO) performed a systematic review of the literature and Delphi process to formulate a consensus document on identifying and treating oligometastatic disease based on a radiation oncology perspective [5]. This committee agreed that the oligometastatic state is independent of primary tumor type, histology, and metastatic site. In their definition, the maximum number of lesions and/or sites that defined oligometastatic disease was dictated by what could be treated safely with curative-intent ablative radiation therapy rather than an absolute number. However, with limited literature available including more than five sites of disease, the authors felt that five lesions should be an upper bound outside of a clinical trial. The consensus document also highlighted some important disease qualifiers when thinking about the oligometastatic state. The definition was further elucidated in another consensus statement from ESTRO and EORTC [6]. As a brief and incomplete summary, they determined that patients can present with either synchronous (de novo) oligometastatic disease where the primary tumor and limited number of metastatic sites are detected simultaneously or metachronous (oligorecurrence) disease where the primary tumor was previously treated and an oligometastatic recurrence follows a certain systemic therapy-free interval. Patients with a history of polymetastatic disease can also have induced oligometastatic disease following a favorable response to systemic therapy. Finally, those with a prior history of oligometastatic disease can recur and have repeat oligometastatic disease following prior systemic or local therapy.
While identification of oligometastatic disease is primarily based on imaging findings, emerging data on molecular subtype may identify subsets of CRC patients that disproportionately benefit from local therapy compared to other patients. Pitroda et al. reported on three distinct subtypes of 134 patients with colorectal liver metastases based on molecular features of their liver tumors [7]. When combined with clinical risk stratification, the molecular subtypes were complementary to identify low-risk, intermediate-risk, and high-risk patient groups with 10-year OS rates of 94%, 45%, and 19%, respectively—thus helping to separate patients who may be able to undergo curative resection of their liver metastases with anticipated long-term survival from those with a high risk of recurrence and likely poor prognosis.
Patient Selection for Local Therapies
The complexity of managing patients with metastatic CRC necessitates the need for a multidisciplinary tumor board with appropriate representation by medical oncology, liver and thoracic surgery, radiation oncology, diagnostic and interventional radiology, and colorectal surgery. Multidisciplinary discussion is particularly important, including a surgical opinion, in patients with liver metastases. Choti et al. used standardized imaging scenarios to survey 190 medical oncologists in the USA regarding resectability and referral for surgical consultation for patients with liver metastases [8]. In eight cases deemed resectable upfront by expert hepatic surgeons, 34.4% of responding medical oncologists felt the case was initially resectable, 41.7% felt neoadjuvant chemotherapy was necessary to allow resection, and 23.9% felt the tumor was unresectable. The likelihood of medical oncologists asking for surgical consultation decreased in proportion with their ranking, with < 5% of medical oncologists recommending consultation for perceived unresectable tumors. The latest guidelines from the American Society of Clinical Oncology stress the importance of multidisciplinary teams in the management of patients with metastatic CRC [9]. As patients presented to a multidisciplinary tumor board have been shown to receive more treatment, including potentially curative treatment, the importance of multidisciplinary care cannot be overstated [10]. In the following sections, we highlight organ sites that are commonly considered for local therapy in patients with metastatic CRC and provide updated evidence to support the potential role of oligometastatic-directed therapy in these clinical scenarios. Table 1 provides a summary of local and regional therapies for patients with mCRC with potential indications and supporting evidence.
Resectable Liver-confined Disease
The liver is the most common site of metastasis in CRC, although only about 20% of these patients are candidates for potentially curative liver resection [3, 11]. While early experiences with hepatic resection of colorectal liver metastases demonstrated 5-year OS rates of approximately 30%, more contemporary experiences with modern systemic therapy now show 5-year OS rates of 50–70% [12,13,14,15,16]. Long-term outcomes have also been reported. Tomlinson et al. described 612 consecutive patients who underwent hepatic resection for colorectal liver metastases with 10-year follow-up [17]. The median disease-specific survival of the entire cohort was 44 months with 102 10-year survivors. While 34% of 5-year survivors suffered a cancer-related death, only one patient experienced a disease-specific death after 10 years of survival.
Advances in surgical resection and improvements in systemic therapy have also increased the numbers of patients eligible for curative-intent resection. Two-stage hepatectomy can be used to resect bilobar disease while minimizing the risk of liver failure [18]. Chavez et al. performed a multi-institutional analysis of 196 patients treated with two-stage hepatectomy for bilateral colorectal liver metastases [18]. Most patients presented with synchronous disease (87.7%) and a median of 7 hepatic metastases. The median OS for the entire cohort was 50 months with 1-, 3-, and 5-year OS of 89%, 64%, and 44%, respectively. Morbidity was acceptable with major complications in 5.1% of patients following the first stage and 23.4% following the second stage, and a 90-day mortality rate of 4.5% following the second stage.
Neoadjuvant systemic therapy as conversion chemotherapy can generate sufficient response to transform initially unresectable disease into resectable disease [19]. Because a uniform definition of unresectable versus resectable liver metastases is lacking and likely surgeon specific, it is challenging to determine conversion rates. Reports of conversion from unresectable to resectable disease following systemic therapy range from 10 to 60% [20,21,22,23]. In addition, the optimal systemic therapy for conversion is unknown, and the length of treatment must be balanced with potential hepatotoxicity from systemic therapy. Adding a biologic agent such as bevacizumab, cetuximab, or panitumumab to chemotherapy to increase response rates and facilitate resection is also controversial. In patients with resectable colorectal liver metastases, the utility of perioperative chemotherapy is unclear. EORTC 40983 was a phase III trial of patients with up to four colorectal liver metastases randomized to perioperative FOLFOX4 or surgical resection alone [14, 24]. A benefit in progression-free survival (PFS) with the addition of perioperative systemic therapy was observed compared to surgery alone (3-year PFS from 33.2 to 42.4% in patients who underwent resection, HR = 0.73, 95% CI 0.55–0.97, P = 0.025). However, no benefit in OS was seen at extended follow-up (median follow up 8.5 years, HR = 0.88, 95% CI 0.68–1.14, P = 0.34). A recent network meta-analysis by Sonbol et al. confirmed a disease-free survival (DFS) benefit (HR = 0.73, 95% CI 0.63–0.84) with the addition of perioperative systemic treatment for patients with resectable colorectal liver metastases, but no statistically significant benefit in OS (HR = 0.88, 95% CI 0.74–1.05) [25].
For patients who present with colorectal liver metastases synchronously with discovery of the primary tumor, timing of resection of the primary CRC and liver metastases should be discussed among experienced hepatobiliary and colorectal surgeons. The METASYNC study was a randomized controlled trial of patients with synchronous initially resectable colorectal liver metastases randomized to simultaneous resection of the liver metastases and colorectal primary or to staged resection where the colorectal primary was removed first and the liver metastases were removed 12–14 weeks later [26]. The primary endpoint of the trial was the rate of major complications within 60 days of surgery and was similar between the groups (49% in the simultaneous and 46% in the delayed, OR = 0.84, P = 0.70). At 2 years after randomization, OS (87.2% vs. 69.6%, P = 0.05) and DFS (35.9% vs. 17.4%, P = 0.05) favored the simultaneous resection group, but the study was limited by sample size (85 evaluable patients) and potential imbalance between the arms in numbers of liver metastases and primary tumor location. A meta-analysis consisting of 22 studies and 4494 patients showed no difference in postoperative mortality, morbidity, OS, or DFS between simultaneous and staged resection of synchronous colorectal liver metastases [27].
For those patients with repeat oligometastatic disease isolated to the liver, repeat hepatectomy is warranted if it can be performed safely [28, 29]. In one study from the Colorectal Liver Operative Metastasis International Collaborative, 953 patients were identified of which 218 were found to have an isolated liver recurrence after initial hepatectomy [29]. Of those patients with recurrence, 51 underwent second hepatectomy. Following propensity score matching to counterbalance inherent selection bias between the repeat and no-repeat hepatectomy groups, median OS was 60.1 months in the repeat hepatectomy group versus 33.1 months in the no-repeat group (P = 0.0023).
While surgery remains the most common approach for patients with resectable colorectal liver metastases, a number of local nonsurgical therapies are available for treating liver tumors including thermal ablation. Several ongoing randomized trials are comparing thermal ablation to surgical resection for resectable colorectal liver metastases including NEW-COMET (NCT05129787) and COLLISION (NCT03088150).
Unresectable Liver-confined Disease
Not all patients are eligible for resection of colorectal liver metastases either due to patient health, patient preference, tumor location, or hepatic reserve, and other locoregional treatment modalities should be considered to provide long-term local control. Multidisciplinary management is important given the lack of a clear standard and the wide range of available treatment modalities, institutional specializations, and nuances for selecting the best treatment for the individual patient.
Thermal Ablation
Thermal ablation using either radiofrequency waves or microwaves is an established technique for treating generally small (< 3 cm) colorectal liver metastases [30]. The only prospective study investigating the role of local therapy in patients with unresectable colorectal liver metastases remains EORTC 40004 (Chemotherapy + Local ablation versus Chemotherapy, CLOCC), which was a randomized phase III study investigating the additional value of radiofrequency ablation (RFA) to systemic therapy [31, 32]. Due to slow accrual, the study was amended and downsized to a phase II trial with 119 patients randomized in a 1:1 fashion. The total tumor burden in the liver needed to be ≤ 50% with < 10 liver metastases. Complete treatment of all liver lesions needed to be possible with either RFA alone or in combination with resection. Tumors planned for RFA needed to be < 4 cm in maximum diameter. For patients randomized to systemic therapy alone, resection was permitted if it converted unresectable disease to resectable disease. The primary endpoint of this trial was 30-month survival rate with the primary objective to demonstrate a > 38% 30-month OS rate in the combined modality arm. The primary endpoint was met as the OS rate at 30 months was 61.7% for the combined treatment group. However, the 30-month OS rate for the systemic therapy alone group was higher than anticipated at 57.6% [31]. The median OS was 45.3 months for the combination treatment and 40.5 months for systemic treatment alone (HR = 0.74, 95% CI 0.46–1.19, P = 0.22). The median PFS was 16.8 months in the combination treatment group and 9.9 months in the systemic therapy alone group (HR = 0.63, 95% CI 0.42–0.95, P = 0.025) [31]. An OS advantage was seen on long-term follow-up at a median of 9.7 years in favor of the combined modality therapy arm (HR = 0.58, 95% CI 0.38–0.88, P = 0.01). Overall survival in the combined modality arm, as compared to the systemic therapy alone arm, at 3, 5, and 8 years were 56.9% versus 55.2%, 43.1% versus 30.3%, and 35.9% versus 8.9%, respectively.
Microwave ablation (MWA) is gaining popularity for the treatment of liver metastases due to technical advantages over RFA [33]. A number of retrospective studies have reported favorable local control rates of 70–90% at 1 year and low rates of toxicity following MWA for colorectal liver metastases [34,35,36,37]. A prospective study evaluating the role of MWA as a curative modality in patients with up to 3 hepatic metastases ≤ 2.5 cm in size will be opening soon (NCT05265169).
Stereotactic Body Radiation Therapy
Stereotactic body radiation therapy (SBRT) is a non-invasive ablative therapy that uses an advanced form of radiation therapy planning and delivery to treat tumors to high doses of radiation while minimizing dose to adjacent normal tissues. Multiple retrospective series have reported their results of using SBRT to treat colorectal liver metastases. Joo et al. reported on 70 patients with 103 colorectal liver metastases, where most patients received an SBRT dose of 45–60 Gy in 3–4 fractions [38]. The 2-year PFS rate was 35%, with 59% of patients recurring in the liver outside of the prior SBRT field. The local control rate at 1, 2, and 3 years for all patients was 93%, 73%, and 68%, respectively. Improved local control was observed for higher radiation doses with 1-, 2-, and 3-year local control rates of 93%, 89%, and 89% in patients receiving a dose of 60 Gy in 3–5 fractions. The 2-year OS rate for all patients was 75%. Scorsetti et al. performed a phase II trial of patients with inoperable liver metastases not amenable to RFA, treating the tumors with an SBRT dose of 45–78.5 in 3 fractions [39]. The actuarial 1-, 2, and 3-year local control rates were 95%, 91%, and 85%, respectively, with a median time to local progression of 17 months. No difference in local recurrence was observed between lesions > 3 cm in size and smaller lesions. The actuarial PFS and OS at 2 years was 48% and 65%, respectively. There were no occurrences of radiation-included liver disease or grade ≥ 3 toxicity. A systematic review by Petrelli et al. consisting of 18 studies and 656 patients treated with liver SBRT for CRC liver metastases reported a pooled 1- and 2-year OS of 67.2% and 56.5%, respectively [40]. The pooled 1-year local control rate was 59.3%.
Hepatic Arterial Infusion Pump
Focal therapies, such as thermal ablation and SBRT, treat individual tumors targeted using image guidance. Regional therapies, such as hepatic arterial infusion pump (HAIP) chemotherapy, serve as a method to deliver high doses of drug to liver tumors while minimizing dose to the normal hepatic parenchyma [41]. HAIP chemotherapy for patients with unresectable colorectal liver metastases has shown benefit in multiple prospective trials, although dated systemic therapy limited the applicability of these study results [42, 43]. A case control study by Dhir et al. compared patients with unresectable colorectal liver metastases treated with HAIP in combination with modern systemic therapy (n = 40) versus modern systemic therapy alone (n = 46) [44]. The groups were well matched for burden of disease and treatment. The median OS in the HAIP plus chemotherapy group was 32.8 months compared with 15.3 months for the chemotherapy alone group (P < 0.0001). On multivariate analysis, treatment with HAIP plus systemic therapy remained statistically significant (HR = 0.39, 95% CI 0.21–0.72, P = 0.003).
In addition to the potential for long-term disease control in the liver, patients treated with HAIP chemotherapy for unresectable disease also have a favorable chance at conversion to resection based on available evidence. Pak et al. reported on a single-institution phase II trial of 64 patients with unresectable colorectal liver metastases treated with combination HAIP and modern systemic chemotherapy [45]. The majority of patients had prior chemotherapy (67%) and bilobar disease (95%) with a median of 13 liver tumors. Conversion to resection was achieved in 52% of patients at a median of 5 months from treatment initiation. The median OS from treatment initiation for all patients was 38 months with a median PFS of 13 months.
While the use of HAIP chemotherapy was initially limited to a small number of institutions, an increasing number of centers are gaining expertise with this therapy. Practice will also be informed by the results of ongoing prospective trials, including the PUMP-IT trial (NCT04552093) and a planned NCTN randomized trial evaluating HAIP in patients with persistently unresectable colorectal liver metastases after first-line systemic therapy.
Transarterial Chemoembolization
Transarterial chemoembolization (TACE), another regional therapy, takes advantage of the selective dependence of hepatic metastases on the arterial blood supply while the normal hepatic parenchyma is supplied primarily via the portal circulation [46]. TACE has a limited role in the management of colorectal liver metastases with sparse prospective data to support its use. Fiorentini et al. performed a phase III study in patients with unresectable colorectal liver metastases, randomizing patients to TACE using drug-eluting beads preloaded with irinotecan (DEBIRI) versus systemic therapy alone with irinotecan, fluorouracil, and leucovorin (FOLFIRI) with a primary endpoint of OS [47]. Median OS was improved in the DEBIRI group versus the systemic therapy alone group (22 vs. 15 months, P = 0.031). PFS was also longer in the DEBIRI group with 7 versus 4 months, respectively (P = 0.006). In a separate small, randomized phase II study of 70 treatment-naïve patients with unresectable colorectal liver metastases, Martin et al. investigated adding DEBIRI to modified FOLFOX versus FOLFOX alone, with bevacizumab also permitted in both arms [48]. Despite some imbalances in the arms likely due to the small size of the study, the overall response rates in the DEBIRI arm were superior at 2 (P = 0.01), 4 (P = 0.03), and 6 (P = 0.05) months with similar statistically significant improvements when evaluating the target lesions alone at 2, 4, and 6 months. Upon blinded radiologic review, however, the overall response rate was deemed to be non-significant between the groups. After a median follow-up of 24 months, there was a non-significant improvement in PFS (15 months for DEBIRI vs. 12 months for chemotherapy alone, P = 0.18) between the treatment groups. Toxicity between the two groups was similar and OS was not reported in the study.
Transarterial Radioembolization
Transarterial radioembolization (TARE) with yttrium-90 involves delivering millions of beta-emitting particles into the hepatic arteries, preferentially depositing radiation into liver tumors while sparing normal liver parenchyma [49]. A combined analysis was performed of three multi-center randomized phase III trials investigating the efficacy of combining first-line FOLFOX with TARE versus FOLFOX alone for patients with liver-dominant mCRC [50]. There was no difference in OS between the groups with a median OS of 22.6 months for FOLFOX plus TARE versus 23.3 months for FOLFOX alone (HR = 1.04, 95% CI 0.90–1.19, P = 0.61). While no difference in PFS was observed between the groups, there was a lower cumulative incidence of first progression in the liver in the first 12 months of follow-up in the FOLFOX plus TARE group versus the FOLFOX alone group: 22% versus 39%, respectively.
The use of TARE has also been investigated prospectively with the addition of second-line systemic therapy. The EPOCH trial was a randomized multi-center phase III trial investigating the role of TARE added to standard-of-care second-line systemic therapy for patients with colorectal liver metastases [51]. In this study, 428 patients who progressed on oxaliplatin- or irinotecan-based first-line therapy were randomized to second-line irinotecan- or oxaliplatin-based chemotherapy with or without the addition of TARE. The primary end points of the study were PFS and hepatic PFS. The median PFS was 8 months for the TARE plus chemotherapy group and 7.2 months for the systemic therapy alone group (HR = 0.69, 95% CI 0.54–0.88, P = 0.0013). The median hepatic PFS also favored the TARE plus chemotherapy group with 9.1 versus 7.2 months, respectively (HR = 0.59, 95% CI 0.46–0.77, P < 0.0001). No difference in OS was observed between the groups with 14 months for TARE plus chemotherapy versus 14.4 months for chemotherapy alone (HR = 1.07, 95% CI 0.86–1.32), but the study was not powered or designed for OS. Rates of severe toxicity were high, with more grade 3 or higher adverse events reported in the TARE group than the chemotherapy alone group (68.4% vs. 49.3%).
No prospective studies have compared the efficacy and safety of regional therapies head-to-head, although retrospective studies have been performed. In one retrospective study, Dhir et al. compared patients with unresectable colorectal liver metastases treated as second-line therapy with either HAIP (n = 48) or TARE (n = 49), comparing both outcomes and cost [52]. The groups were similar in terms of tumor and prior treatment characteristics with both groups receiving a median of 3 lines of chemotherapy prior, although more patients treated with TARE underwent prior liver resection (36.7% vs. 12.5%, P = 0.006). Patients treated with HAIP had longer OS from time of unresectable liver metastasis diagnosis than the patients treated with TARE (31.2 vs. 16.3 months, P < 0.001), but the two groups were similar when comparing OS from the time of stage 4 disease diagnosis (34.4 for HAIP vs. 32 for TARE, P = 0.291). To date, there are limited prospective studies comparing local or regional nonsurgical therapy for colorectal liver metastases, and treatment decisions are largely based on institutional preference and referral patterns.
While these local or regional therapies are often used in combination or sequentially in practice, data are lacking regarding the optimal integration of such therapies or the efficacy and safety of such an approach. For patients fit and motivated for surgical resection, upfront use of HAIP has demonstrated favorable response rates potentially increasing the chances of a margin-negative resection and long-term cure. For patients with a limited number of liver lesions who are not candidates for surgery, SBRT and thermal ablation have shown favorable results. For patients with a higher number of lesions that cannot be addressed with SBRT or thermal ablation, both TARE and TACE can be considered in the second-line setting. In all cases, there should be a multidisciplinary discussion involving specialists in the various local and regional therapies, and the final treatment plan should coincide with the patient’s goals and desires [53].
Lung-confined Disease
Surgical Resection
For patients with lung-isolated disease, local therapy such as surgical resection can be considered, although there are no prospective randomized trials showing benefits of such an approach over continued systemic therapy alone. The Pulmonary Metastasectomy in Colorectal Cancer (PulMiCC) trial was a randomized phase III non-inferiority trial conducted in the UK with a plan to register 1350 patients and subsequently randomize 300 patients to either pulmonary metastasectomy or observation [54]. The trial was closed early due to poor accrual after registering 512 patients with 93 consenting to randomization. In both groups, about 30% of patients had undergone prior resection for liver metastases and 55% of patients had 2–4 lung metastases. Other patient characteristics and the use of systemic therapy were well balanced between the groups. The 5-year OS rates were 29.6% for the observation arm and 36.4% for the metastasectomy arm, which were comparable and did not achieve statistical significance (HR = 0.93, 95% CI 0.56–1.56).
Despite limited prospective data, there are a number of large retrospective series highlighting long-term survival following pulmonary metastasectomy for patients with CRC of which several are highlighted here [55,56,57]. Booth et al. reported a population-based study in Ontario that included 709 patients who underwent lung metastasectomy for CRC, with most patients undergoing either segmentectomy (56%) or lobectomy (40%) [55]. The 5- and 10-year OS rates were 40% and 27%, respectively, on par with some surgical series for liver metastases. Lung metastasectomy use also increased over time. Okumura et al. reported on the outcomes of 785 patients with pulmonary metastasis from CRC treated with curative resection at 46 Japanese hospitals [57]. Extrathoracic disease was present in 24% of patients, but all patients received curative treatment to those disease sites. Solitary pulmonary metastasis was present in 74% of patients and 60% of patients underwent wedge resection. The 5-year DFS and OS rates for all patients were 37.1% and 68.1%, respectively. A number of prognostic factors for adverse OS were identified, including disease-free interval of less than 2 years, presence of extrathoracic disease treated curatively prior to lung resection, abnormal serum carcinoembryonic antigen level, three or more radiologic pulmonary metastases, and age of 70 years or older. The 5-year OS rates of low-risk (no risk factors), moderate-risk (1–2 risk factors), and high-risk (≥ 3 risk factors) groups were 89.4%, 72.5%, and 48.9%, respectively. A large retrospective registry study from South Australia compared outcomes of patients who underwent hepatic resection versus those who underwent lung resection for colorectal metastasis [58]. While the proportion of patients who underwent lung resection was relatively small (3.1%), OS between the two cohorts were comparable, supporting the use of lung resection in patients with pulmonary metastases from CRC.
Thermal Ablation
Not all patients are eligible for surgical resection, or they choose against surgery for various reasons including the potential for persistent pain at the surgical site [59]. An effective non-surgical therapy for treating lung metastases is thermal ablation. Hasegawa et al. performed a prospective multicenter phase II trial of patients with technically resectable colorectal lung metastases treated with RFA [60]. Patients were required to have ≤ 5 surgically resectable lung metastases measuring ≤ 3 cm. There were 70 patients included and 100 lung metastases treated, with local and distant tumor progression evaluated by a central diagnostic committee. At a mean follow-up of 57 months, the rate of local tumor progression was 9% at a mean of 12.8 months from RFA. The 3-year rates of PFS were 41% and 84%, respectively. There were no grade 3–4 adverse events and one grade 5 event. Grade 2 pneumothorax events requiring chest tube placement occurred in 20% of patients. Kurilova et al. retrospectively reviewed 50 patients with 90 CRC pulmonary metastases treated with MWA [61]. The median tumor size was 1 cm with a range of 0.3–3.2 cm, and 12% of patients underwent two separate sessions of MWA for bilateral disease. The rates of 1-, 2-, and 3-year local tumor PFS were 93%, 86%, and 86%, respectively. The rates of 1-, 2-, and 3-year OS were 94%, 82%, and 61%. The major complication rate was 13% with most complications involving prolonged hospitalization due to pneumothorax.
Stereotactic Body Radiation Therapy
Data supporting the use of SBRT for colorectal lung metastases is largely based on retrospective reviews of single- or multi-institution experiences. Sharma et al. retrospectively reviewed 118 patents with 202 pulmonary oligometastases treated with SBRT [62]. Nearly 30% of tumors were ≥ 3 cm in size. The local control at 2-, 3-, and 5-years was 83%, 81%, and 77%, respectively, with biologically effective doses (BED) ≥ 100 Gy associated with improved local control. OS at 2, 3, and 5 years was 69%, 55%, and 36%, respectively. Treatment was well tolerated with 6% of patients experiencing grade 3 acute or late toxicities. The largest multi-center retrospective series was reported by Nicosia et al. of 1033 colorectal lung metastases treated with SBRT [63]. The median tumor diameter was 1.3 cm (range, 0.5–5.8 cm). The 2-year freedom from local progression was 75.4% with a rate of 94% for lesions treated with a BED ≥ 125 Gy. The median time to progression of polymetastatic disease, defined as first occurrence of > 5 simultaneous new metastases after SBRT, was 26.8 months.
Whether non-surgical therapies are as effective as surgical resection for pulmonary metastases remains an open question in need of prospective data for guidance. A number of retrospective studies have compared surgical resection to other modalities such as image-guided thermal ablation [64] and SBRT [65, 66], but their conclusions are limited due to study design issues including selection bias. A prospective randomized trial (PUCC-Trial, DRKS00024727) that may help clarify therapy options for patients with pulmonary metastases is being conducted in Germany for patients with ≥ 3 lung metastases randomized to pulmonary metastasectomy versus standard of care treatment (including medical treatment and SBRT, if indicated).
Both Liver and Lung Metastases
For patients with both liver and lung metastases, local therapy to eradicate disease in both organs can be considered, but the data utilizing such an approach is primarily limited to small retrospective series. Shah et al. reported on 39 patients who underwent both hepatic and pulmonary resections for mCRC [67]. The median number of liver lesions removed was 1 (range, 1–6) with the median size of largest metastasis 4 cm (range, 1.7–16 cm). For the lung metastases, the median number of lung lesions removed was 1 (range, 1–5) with nearly 60% of patients undergoing wedge resection with thoracotomy. The median DFS and OS after initial metastasectomy were 19.8 and 87 months, respectively. When comparing outcomes of patients with both liver and lung metastases, those who underwent both liver and lung resection had a significantly longer 5-year OS than patients who did not undergo lung resection for pulmonary metastases (74% vs. 42%, respectively, P = 0.05). Wei et al. performed a phase II single-arm study evaluating the role of metastasectomy in 26 patients with intrahepatic and extrahepatic disease (primarily lung) [68]. Eligible patients with any number of resectable intrahepatic metastases were required to have ≤ 3 foci of extrahepatic disease that was resectable. Nearly 85% of patients had received chemotherapy prior to resection. Protocol surgery was completed in 77% of patients; major complications occurred in 19% of patients and one perioperative death. The median OS from time of first metastasectomy to death was 38 months with a 3-year OS of 53%.
Extrahepatic or Extrapulmonary Disease
The presence of extrahepatic disease was once thought to be a contraindication to local therapy in patients with colorectal metastases. However, mounting evidence demonstrating reasonable outcomes following resection of liver metastases and limited extrahepatic disease has augmented consideration of this approach in select patients [69, 70]. A retrospective review of 219 patients who underwent resection of colorectal liver metastases and synchronous extrahepatic disease was reported by Leung et al. [71]. Extrahepatic sites included portal lymph nodes, retroperitoneal lymph nodes, ovaries, and peritoneum, among others. The median, 5-, and 10-year OS were 34.4 months, 28%, and 10%, respectively, with disease recurring in 90% of patients at a median of 8 months. Patients with liver metastasis > 3 cm, > 5 liver metastases, and extrahepatic site of disease (including portal, retroperitoneal, or multiple sites) were associated with a poorer prognosis. While 90% recurrence at a median of 8 months may seem dismal, the median PFS with FOLFOX chemotherapy as first-line therapy is approximately 10 months [72]. It remains to be seen if the delay in initiating systematic therapy improves quality of life.
With advances in radiation therapy planning and delivery, motion management, and the development of stereotactic radiosurgery (SRS) and SBRT, ablative therapy is not limited to the liver and lung and can be administered safely and effectively to a number of body sites simultaneously [73]. The SABR-COMET study was a phase II randomized tumor-agnostic study in patients with a controlled primary tumor and 1–5 oligometastases randomized to either SBRT to all sites of disease or standard-of-care (SOC) therapy alone. Extended long-term outcomes from this study were recently published [74]. Most patients had 1–3 lesions (~ 90%), and ~ 80% of the treated sites were lung or bone with other sites treated including liver, adrenal, brain, and lymph nodes. Patients with colorectal primaries included 27% of the control arm and 14% of the SBRT arm. At a median follow-up of 5.7 years, 8-year OS was 27.2% in the SBRT arm versus 13.6% in the control arm (HR = 0.50, 95% CI 0.30–0.84, P = 0.008). For PFS, 8-year estimates were 21.3% for the SBRT arm versus 0% for the control arm (HR = 0.45, 95% CI 0.28–0.72, P < 0.001). There were no new toxicities on extended follow-up with grade ≥ 2 acute or late toxicity observed in 30.3% of patients treated with SBRT versus 9.1% of the control arm (P = 0.019). Finally, chemotherapy use was significantly lower in the SBRT arm versus the control arm (33.3% vs. 54.6%, P = 0.043). The successor study to SABR-COMET, SABR-COMET-10, is ongoing and will include patients with a controlled primary and 4–10 metastatic lesions randomized to SOC treatment with or without the addition of SBRT to all sites of disease [75]. The feasibility of successfully treating up to 10 lesions was recently published by the study team [76]. Sheikh et al. recently published a large multi-institutional retrospective study of 235 patients with metastatic colorectal cancer treated with SBRT to ≤ 5 lesions [77]. The most common sites treated were lung (62.7%) and liver (26.5%). The 1- and 5-year local recurrence rates were 13.6% and 44.3%, respectively. The 2- and 5-year PFS were 26.4% and 14.1%, respectively, while the 2- and 5-year OS were 76.1% and 35.9%, respectively.
The role of local ablative therapy in patients with unresectable oligometastatic CRC will hopefully be clarified by the results of ongoing prospective trials, including the RESOLUTE trial (ACTRN12621001198819) and the upcoming NCTN ERASur trial (NCT05673148).
Future Directions
Well-designed prospective trials are needed to determine how best to treat patients with oligometastatic CRC. Identifying appropriate candidates who may benefit from local therapy remains an open question, particularly for patients with lung, liver, or extrahepatic disease where the role of local therapy is unclear. The role of metastasis-directed therapy in patients with mismatch repair-deficient CRC is also unclear, although neoadjuvant immunotherapy may be highly effective in this subgroup of patients based on early data [78,79,80]. In addition, selecting the correct modality or combination of therapies for an individual patient, or the correct sequencing of therapies to optimize therapy for patients, is unknown. Finally, how to incorporate novel biomarkers such as circulating tumor DNA (ctDNA) in the workflow for such patients is currently unknown; however, preliminary data has shown that using ctDNA can help identify patients at high risk of recurrence following curative-intent hepatectomy for colorectal liver metastases [81].
Conclusions
Oligometastatic CRC remains one of the model malignancies for the use of local therapy in patients with non-localized disease. As local and regional therapies have evolved, however, the definition of oligometastatic CRC clearly needs to mature as well. Technological advances in therapy are outpacing the data to support their use. Prospective trials, perhaps incorporating novel biomarkers, are needed to help identify which patients with metastatic CRC might benefit from the addition of local therapy. The results of ongoing prospective trials—including the RESOLUTE trial (ACTRN12621001198819) and the upcoming NCTN ERASur trial (NCT05673148)—will hopefully clarify the appropriate role of local ablative therapy in patients with unresectable oligometastatic CRC.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33. https://doi.org/10.3322/caac.21708.
Elferink MA, De Jong KP, Klaase JM, Siemerink EJ, De Wilt JH. Metachronous metastases from colorectal cancer: a population-based study in North-East Netherlands. Int J Colorectal Dis. 2015;30:205–12. https://doi.org/10.1007/s00384-014-2085-6.
Riihimaki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016;6:29765. https://doi.org/10.1038/srep29765.
deSouza NM, Tempany CM. A risk-based approach to identifying oligometastatic disease on imaging. Int J Cancer. 2019;144:422–30. https://doi.org/10.1002/ijc.31793.
Lievens Y, Guckenberger M, Gomez D, Hoyer M, Iyengar P, Kindts I, et al. Defining oligometastatic disease from a radiation oncology perspective: an ESTRO-ASTRO consensus document. Radiother Oncol. 2020;148:157–66. https://doi.org/10.1016/j.radonc.2020.04.003.
Guckenberger M, Lievens Y, Bouma AB, Collette L, Dekker A, De Souza NM, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020;21:e18–28. https://doi.org/10.1016/S1470-2045(19)30718-1.
Pitroda SP, Khodarev NN, Huang L, Uppal A, Wightman SC, Ganai S, et al. Integrated molecular subtyping defines a curable oligometastatic state in colorectal liver metastasis. Nat Commun. 2018;9:1793. https://doi.org/10.1038/s41467-018-04278-6.
Choti MA, Thomas M, Wong SL, Eaddy M, Pawlik TM, Hirose K, et al. Surgical resection preferences and perceptions among medical oncologists treating liver metastases from colorectal cancer. Ann Surg Oncol. 2016;23:375–81. https://doi.org/10.1245/s10434-015-4925-1.
Morris VK, Kennedy EB, Baxter NN, Benson AB, 3rd, Cercek A, Cho M, et al. Treatment of metastatic colorectal cancer: ASCO Guideline. J Clin Oncol. 2022;JCO2201690. https://doi.org/10.1200/JCO.22.01690
Lowes M, Kleiss M, Lueck R, Detken S, Koenig A, Nietert M, et al. The utilization of multidisciplinary tumor boards (MDT) in clinical routine: results of a health care research study focusing on patients with metastasized colorectal cancer. Int J Colorectal Dis. 2017;32:1463–9. https://doi.org/10.1007/s00384-017-2871-z.
Adam R, Vinet E. Regional treatment of metastasis: surgery of colorectal liver metastases. Ann Oncol. 2004;15(Suppl 4):iv103–6. https://doi.org/10.1093/annonc/mdh912
Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg. 1995;19:59–71. https://doi.org/10.1007/BF00316981.
Butler J, Attiyeh FF, Daly JM. Hepatic resection for metastases of the colon and rectum. Surg Gynecol Obstet. 1986;162:109–13.
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, et al. Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol. 2013;14:1208–15. https://doi.org/10.1016/S1470-2045(13)70447-9.
Kanemitsu Y, Shimizu Y, Mizusawa J, Inaba Y, Hamaguchi T, Shida D, et al. Hepatectomy followed by mFOLFOX6 versus hepatectomy alone for liver-only metastatic colorectal cancer (JCOG0603): a phase II or III randomized controlled trial. J Clin Oncol. 2021;39:3789–99. https://doi.org/10.1200/JCO.21.01032.
Wei AC, Greig PD, Grant D, Taylor B, Langer B, Gallinger S. Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol. 2006;13:668–76. https://doi.org/10.1245/ASO.2006.05.039.
Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25:4575–80. https://doi.org/10.1200/JCO.2007.11.0833.
Chavez MI, Gholami S, Kim BJ, Margonis GA, Ethun CG, Tsai S, et al. Two-stage hepatectomy for bilateral colorectal liver metastases: a multi-institutional analysis. Ann Surg Oncol. 2021;28:1457–65. https://doi.org/10.1245/s10434-020-09459-6.
Mokdad A, Choti MA, Yopp AC. Conversion chemotherapy for unresectable colorectal liver metastases: are we making a difference? Curr Colorect Canc R. 2015;11:160–7. https://doi.org/10.1007/s11888-015-0271-8.
Barone C, Nuzzo G, Cassano A, Basso M, Schinzari G, Giuliante F, et al. Final analysis of colorectal cancer patients treated with irinotecan and 5-fluorouracil plus folinic acid neoadjuvant chemotherapy for unresectable liver metastases. Br J Cancer. 2007;97:1035–9. https://doi.org/10.1038/sj.bjc.6603988.
Masi G, Loupakis F, Pollina L, Vasile E, Cupini S, Ricci S, et al. Long-term outcome of initially unresectable metastatic colorectal cancer patients treated with 5-fluorouracil/leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) followed by radical surgery of metastases. Ann Surg. 2009;249:420–5. https://doi.org/10.1097/SLA.0b013e31819a0486.
Ychou M, Rivoire M, Thezenas S, Guimbaud R, Ghiringhelli F, Mercier-Blas A, et al. Chemotherapy (doublet or triplet) plus targeted therapy by RAS status as conversion therapy in colorectal cancer patients with initially unresectable liver-only metastases. The UNICANCER PRODIGE-14 randomised clinical trial. Br J Cancer. 2022;126:1264–70. https://doi.org/10.1038/s41416-021-01644-y.
Ye LC, Liu TS, Ren L, Wei Y, Zhu DX, Zai SY, et al. Randomized controlled trial of cetuximab plus chemotherapy for patients with KRAS wild-type unresectable colorectal liver-limited metastases. J Clin Oncol. 2013;31:1931–8. https://doi.org/10.1200/JCO.2012.44.8308.
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371:1007–16. https://doi.org/10.1016/S0140-6736(08)60455-9.
Sonbol MB, Siddiqi R, Uson PLS, Pathak S, Firwana B, Botrus G, et al. The role of systemic therapy in resectable colorectal liver metastases: systematic review and network meta-analysis. Oncologist. 2022. https://doi.org/10.1093/oncolo/oyac212.
Boudjema K, Locher C, Sabbagh C, Ortega-Deballon P, Heyd B, Bachellier P, et al. Simultaneous versus delayed resection for initially resectable synchronous colorectal cancer liver metastases: a prospective, open-label, randomized, controlled trial. Ann Surg. 2021;273:49–56. https://doi.org/10.1097/SLA.0000000000003848.
Feng Q, Wei Y, Zhu D, Ye L, Lin Q, Li W, et al. Timing of hepatectomy for resectable synchronous colorectal liver metastases: for whom simultaneous resection is more suitable—a meta-analysis. PLoS One. 2014;9:e104348. https://doi.org/10.1371/journal.pone.0104348.
Takamoto T, Hashimoto T, Miyata A, Shimada K, Maruyama Y, Makuuchi M. Repeat hepatectomy after major hepatectomy for colorectal liver metastases. J Gastrointest Surg. 2020;24:380–7. https://doi.org/10.1007/s11605-019-04154-8.
Valenzuela CD, Moaven O, Gawdi R, Stauffer JA, Del Piccolo NR, Cheung TT, et al. Outcomes after repeat hepatectomy for colorectal liver metastases from the colorectal liver operative metastasis international collaborative (COLOMIC). J Surg Oncol. 2022. https://doi.org/10.1002/jso.27056.
Lin YM, Paolucci I, Brock KK, Odisio BC. Image-guided ablation for colorectal liver metastasis: principles, current evidence, and the path forward. Cancers (Basel). 2021;13. https://doi.org/10.3390/cancers13163926.
Ruers T, Punt C, Van Coevorden F, Pierie J, Borel-Rinkes I, Ledermann JA, et al. Radiofrequency ablation combined with systemic treatment versus systemic treatment alone in patients with non-resectable colorectal liver metastases: a randomized EORTC Intergroup phase II study (EORTC 40004). Ann Oncol. 2012;23:2619–26. https://doi.org/10.1093/annonc/mds053.
Ruers T, Van Coevorden F, Punt CJ, Pierie JE, Borel-Rinkes I, Ledermann JA, et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J Natl Cancer Inst. 2017;109. https://doi.org/10.1093/jnci/djx015.
Lubner MG, Brace CL, Hinshaw JL, Lee FT Jr. Microwave tumor ablation: mechanism of action, clinical results, and devices. J Vasc Interv Radiol. 2010;21:S192-203. https://doi.org/10.1016/j.jvir.2010.04.007.
Knott EA, Ziemlewicz TJ, Lubner SJ, Swietlik JF, Weber SM, Zlevor AM, et al. Microwave ablation for colorectal cancer metastasis to the liver: a single-center retrospective analysis. J Gastrointest Oncol. 2021;12:1454–69. https://doi.org/10.21037/jgo-21-159.
Shady W, Petre EN, Do KG, Gonen M, Yarmohammadi H, Brown KT, et al. Percutaneous microwave versus radiofrequency ablation of colorectal liver metastases: ablation with clear margins (A0) provides the best local tumor control. J Vasc Interv Radiol. 2018;29(268–275):e1. https://doi.org/10.1016/j.jvir.2017.08.021
Puijk RS, Dijkstra M, van den Bemd BAT, Ruarus AH, Nieuwenhuizen S, Geboers B, et al. Improved outcomes of thermal ablation for colorectal liver metastases: a 10-year analysis from the prospective Amsterdam CORE Registry (AmCORE). Cardiovasc Intervent Radiol. 2022;45:1074–89. https://doi.org/10.1007/s00270-022-03152-9.
Mimmo A, Pegoraro F, Rhaiem R, Montalti R, Donadieu A, Tashkandi A, et al. Microwave ablation for colorectal liver metastases: a systematic review and pooled oncological analyses. Cancers (Basel). 2022;14. https://doi.org/10.3390/cancers14051305.
Joo JH, Park JH, Kim JC, Yu CS, Lim SB, Park IJ, et al. Local control outcomes using stereotactic body radiation therapy for liver metastases from colorectal cancer. Int J Radiat Oncol Biol Phys. 2017;99:876–83. https://doi.org/10.1016/j.ijrobp.2017.07.030.
Scorsetti M, Comito T, Tozzi A, Navarria P, Fogliata A, Clerici E, et al. Final results of a phase II trial for stereotactic body radiation therapy for patients with inoperable liver metastases from colorectal cancer. J Cancer Res Clin Oncol. 2015;141:543–53. https://doi.org/10.1007/s00432-014-1833-x.
Petrelli F, Comito T, Barni S, Pancera G, Scorsetti M, Ghidini A, et al. Stereotactic body radiotherapy for colorectal cancer liver metastases: a systematic review. Radiother Oncol. 2018;129:427–34. https://doi.org/10.1016/j.radonc.2018.06.035.
Ensminger WD, Gyves JW. Clinical pharmacology of hepatic arterial chemotherapy. Semin Oncol. 1983;10:176–82.
Kemeny NE, Niedzwiecki D, Hollis DR, Lenz HJ, Warren RS, Naughton MJ, et al. Hepatic arterial infusion versus systemic therapy for hepatic metastases from colorectal cancer: a randomized trial of efficacy, quality of life, and molecular markers (CALGB 9481). J Clin Oncol. 2006;24:1395–403. https://doi.org/10.1200/JCO.2005.03.8166.
Lorenz M, Muller HH. Randomized, multicenter trial of fluorouracil plus leucovorin administered either via hepatic arterial or intravenous infusion versus fluorodeoxyuridine administered via hepatic arterial infusion in patients with nonresectable liver metastases from colorectal carcinoma. J Clin Oncol. 2000;18:243–54. https://doi.org/10.1200/JCO.2000.18.2.243.
Dhir M, Jones HL, Shuai Y, Clifford AK, Perkins S, Steve J, et al. Hepatic arterial infusion in combination with modern systemic chemotherapy is associated with improved survival compared with modern systemic chemotherapy alone in patients with isolated unresectable colorectal liver metastases: a case-control study. Ann Surg Oncol. 2017;24:150–8. https://doi.org/10.1245/s10434-016-5418-6.
Pak LM, Kemeny NE, Capanu M, Chou JF, Boucher T, Cercek A, et al. Prospective phase II trial of combination hepatic artery infusion and systemic chemotherapy for unresectable colorectal liver metastases: Long term results and curative potential. J Surg Oncol. 2018;117:634–43. https://doi.org/10.1002/jso.24898.
Breedis C, Young G. The blood supply of neoplasms in the liver. Am J Pathol. 1954;30:969–77.
Fiorentini G, Aliberti C, Tilli M, Mulazzani L, Graziano F, Giordani P, et al. Intra-arterial infusion of irinotecan-loaded drug-eluting beads (DEBIRI) versus intravenous therapy (FOLFIRI) for hepatic metastases from colorectal cancer: final results of a phase III study. Anticancer Res. 2012;32:1387–95.
Martin RC 2nd, Scoggins CR, Schreeder M, Rilling WS, Laing CJ, Tatum CM, et al. Randomized controlled trial of irinotecan drug-eluting beads with simultaneous FOLFOX and bevacizumab for patients with unresectable colorectal liver-limited metastasis. Cancer. 2015;121:3649–58. https://doi.org/10.1002/cncr.29534.
Westcott MA, Coldwell DM, Liu DM, Zikria JF. The development, commercialization, and clinical context of yttrium-90 radiolabeled resin and glass microspheres. Adv Radiat Oncol. 2016;1:351–64. https://doi.org/10.1016/j.adro.2016.08.003.
Wasan HS, Gibbs P, Sharma NK, Taieb J, Heinemann V, Ricke J, et al. First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOXFIRE, SIRFLOX, and FOXFIRE-Global): a combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol. 2017;18:1159–71. https://doi.org/10.1016/S1470-2045(17)30457-6.
Mulcahy MF, Mahvash A, Pracht M, Montazeri AH, Bandula S, Martin RCG 2nd, et al. Radioembolization with chemotherapy for colorectal liver metastases: a randomized, open-label, international, multicenter, phase III trial. J Clin Oncol. 2021;39:3897–907. https://doi.org/10.1200/JCO.21.01839.
Dhir M, Zenati MS, Jones HL, Bartlett DL, Choudry MHA, Pingpank JF, et al. Effectiveness of hepatic artery infusion (HAI) versus selective internal radiation therapy (Y90) for pretreated isolated unresectable colorectal liver metastases (IU-CRCLM). Ann Surg Oncol. 2018;25:550–7. https://doi.org/10.1245/s10434-017-6265-9.
Raphael MJ, Karanicolas PJ. Regional therapy for colorectal cancer liver metastases: which modality and when? J Clin Oncol. 2022;40:2806–17. https://doi.org/10.1200/JCO.21.02505.
Milosevic M, Edwards J, Tsang D, Dunning J, Shackcloth M, Batchelor T, et al. Pulmonary metastasectomy in colorectal cancer: updated analysis of 93 randomized patients – control survival is much better than previously assumed. Colorectal Dis. 2020;22:1314–24. https://doi.org/10.1111/codi.15113.
Booth CM, Nanji S, Wei X, Mackillop WJ. Outcomes of resected colorectal cancer lung metastases in routine clinical practice: a population-based study. Ann Surg Oncol. 2016;23:1057–63. https://doi.org/10.1245/s10434-015-4979-0.
Davini F, Ricciardi S, Zirafa CC, Romano G, Ali G, Fontanini G, et al. Lung metastasectomy after colorectal cancer: prognostic impact of resection margin on long term survival, a retrospective cohort study. Int J Colorectal Dis. 2020;35:9–18. https://doi.org/10.1007/s00384-019-03386-z.
Okumura T, Boku N, Hishida T, Ohde Y, Sakao Y, Yoshiya K, et al. Surgical outcome and prognostic stratification for pulmonary metastasis from colorectal cancer. Ann Thorac Surg. 2017;104:979–87. https://doi.org/10.1016/j.athoracsur.2017.03.021.
Patel D, Townsend AR, Karapetis C, Beeke C, Padbury R, Roy A, et al. Is survival for patients with resectable lung metastatic colorectal cancer comparable to those with resectable liver disease? Results from the South Australian Metastatic Colorectal Registry. Ann Surg Oncol. 2016;23:3616–22. https://doi.org/10.1245/s10434-016-5290-4.
Furrer M, Rechsteiner R, Eigenmann V, Signer C, Althaus U, Ris HB. Thoracotomy and thoracoscopy: postoperative pulmonary function, pain and chest wall complaints. Eur J Cardiothorac Surg. 1997;12:82–7. https://doi.org/10.1016/s1010-7940(97)00105-x.
Hasegawa T, Takaki H, Kodama H, Yamanaka T, Nakatsuka A, Sato Y, et al. Three-year survival rate after radiofrequency ablation for surgically resectable colorectal lung metastases: a prospective multicenter study. Radiology. 2020;294:686–95. https://doi.org/10.1148/radiol.2020191272.
Kurilova I, Gonzalez-Aguirre A, Beets-Tan RG, Erinjeri J, Petre EN, Gonen M, et al. Microwave ablation in the management of colorectal cancer pulmonary metastases. Cardiovasc Intervent Radiol. 2018;41:1530–44. https://doi.org/10.1007/s00270-018-2000-6.
Sharma A, Baker S, Duijm M, Oomen-de Hoop E, Cornelissen R, Verhoef C, et al. Prognostic factors for local control and survival for inoperable pulmonary colorectal oligometastases treated with stereotactic body radiotherapy. Radiother Oncol. 2020;144:23–9. https://doi.org/10.1016/j.radonc.2019.10.004.
Nicosia L, Franceschini D, Perrone-Congedi F, Casamassima F, Gerardi MA, Rigo M, et al. A multicenter LArge retrospectIve daTabase on the personalization of stereotactic ABlative radiotherapy use in lung metastases from colon-rectal cancer: The LaIT-SABR study. Radiother Oncol. 2022;166:92–9. https://doi.org/10.1016/j.radonc.2021.10.023.
Karam E, Tabutin M, Mastier C, Crignis L, Peyrat P, Martin V, et al. Curative-intent treatment of pulmonary metastases from colorectal cancer: a comparison between imaging-guided thermal ablation and surgery. J Surg Oncol. 2022. https://doi.org/10.1002/jso.27108.
Nelson DB, Tayob N, Nguyen QN, Erasmus J, Mitchell KG, Hofstetter WL, et al. Local failure after stereotactic body radiation therapy or wedge resection for colorectal pulmonary metastases. J Thorac Cardiovasc Surg. 2019;158(1234–1241): e16. https://doi.org/10.1016/j.jtcvs.2019.02.133.
Widder J, Klinkenberg TJ, Ubbels JF, Wiegman EM, Groen HJ, Langendijk JA. Pulmonary oligometastases: metastasectomy or stereotactic ablative radiotherapy? Radiother Oncol. 2013;107:409–13. https://doi.org/10.1016/j.radonc.2013.05.024.
Shah SA, Haddad R, Al-Sukhni W, Kim RD, Greig PD, Grant DR, et al. Surgical resection of hepatic and pulmonary metastases from colorectal carcinoma. J Am Coll Surg. 2006;202:468–75. https://doi.org/10.1016/j.jamcollsurg.2005.11.008.
Wei AC, Coburn NG, Devitt KS, Serrano PE, Moulton CA, Cleary SP, et al. Survival following resection of intra- and extra-hepatic metastases from colorectal cancer: a phase II trial. Ann Surg Oncol. 2016;23:2644–51. https://doi.org/10.1245/s10434-016-5189-0.
Adam R, de Haas RJ, Wicherts DA, Vibert E, Salloum C, Azoulay D, et al. Concomitant extrahepatic disease in patients with colorectal liver metastases: when is there a place for surgery? Ann Surg. 2011;253:349–59. https://doi.org/10.1097/SLA.0b013e318207bf2c.
Pulitano C, Bodingbauer M, Aldrighetti L, de Jong MC, Castillo F, Schulick RD, et al. Liver resection for colorectal metastases in presence of extrahepatic disease: results from an international multi-institutional analysis. Ann Surg Oncol. 2011;18:1380–8. https://doi.org/10.1245/s10434-010-1459-4.
Leung U, Gonen M, Allen PJ, Kingham TP, DeMatteo RP, Jarnagin WR, et al. Colorectal cancer liver metastases and concurrent extrahepatic disease treated with resection. Ann Surg. 2017;265:158–65. https://doi.org/10.1097/SLA.0000000000001624.
Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA, et al. Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wild-type advanced or metastatic colorectal cancer: a randomized clinical trial. JAMA. 2017;317:2392–401. https://doi.org/10.1001/jama.2017.7105.
Chmura S, Winter KA, Robinson C, Pisansky TM, Borges V, Al-Hallaq H, et al. Evaluation of safety of stereotactic body radiotherapy for the treatment of patients with multiple metastases: findings from the NRG-BR001 phase 1 trial. JAMA Oncol. 2021;7:845–52. https://doi.org/10.1001/jamaoncol.2021.0687.
Harrow S, Palma DA, Olson R, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic Radiation for the Comprehensive Treatment of Oligometastases (SABR-COMET): extended long-term outcomes. Int J Radiat Oncol Biol Phys. 2022;114:611–6. https://doi.org/10.1016/j.ijrobp.2022.05.004.
Palma DA, Olson R, Harrow S, Correa RJM, Schneiders F, Haasbeek CJA, et al. Stereotactic ablative radiotherapy for the comprehensive treatment of 4–10 oligometastatic tumors (SABR-COMET-10): study protocol for a randomized phase III trial. BMC Cancer. 2019;19:816. https://doi.org/10.1186/s12885-019-5977-6.
Ashram S, Bahig H, Barry A, Blanchette D, Celinksi A, Chung P, et al. Planning trade-offs for SABR in patients with 4 to 10 metastases: a substudy of the SABR-COMET-10 randomized trial. Int J Radiat Oncol Biol Phys. 2022. https://doi.org/10.1016/j.ijrobp.2022.05.035.
Sheikh S, Chen H, Sahgal A, Poon I, Erler D, Badellino S, et al. An analysis of a large multi-institutional database reveals important associations between treatment parameters and clinical outcomes for stereotactic body radiotherapy (SBRT) of oligometastatic colorectal cancer. Radiother Oncol. 2022;167:187–94. https://doi.org/10.1016/j.radonc.2021.12.018.
Andre T, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N Engl J Med. 2020;383:2207–18. https://doi.org/10.1056/NEJMoa2017699.
Cercek A, Lumish M, Sinopoli J, Weiss J, Shia J, Lamendola-Essel M, et al. PD-1 blockade in mismatch repair-deficient, locally advanced rectal cancer. N Engl J Med. 2022;386:2363–76. https://doi.org/10.1056/NEJMoa2201445.
Chalabi M, Fanchi LF, Dijkstra KK, Van den Berg JG, Aalbers AG, Sikorska K, et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med. 2020;26:566–76. https://doi.org/10.1038/s41591-020-0805-8.
Newhook TE, Overman MJ, Chun YS, Dasari A, Tzeng CD, Cao HST, et al. Prospective study of perioperative circulating tumor DNA dynamics in patients undergoing hepatectomy for colorectal liver metastases. Ann Surg. 2022. https://doi.org/10.1097/SLA.0000000000005461.
Acknowledgements
The authors would like to thank Jennifer Huber for editorial assistance.
Funding
EDM is supported by a NIH/NCI Cancer Center Support Grant (P30 CA16058). PBR is supported by a NIH/NCI Cancer Center Support Grant (P30 CA008748) and a NIH/NCI early career development award (K08 CA255574).
Author information
Authors and Affiliations
Contributions
All authors participated in drafting and critical review of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
EDM has served as a consultant for Varian Medical Systems. KEH reports research relationships with Elekta, Merck, and BioMimetix that are unrelated to the topic of this review. PBR received research funding and serves as a consultant for EMD Serono, receives research funding from XRAD Therapeutics, is a consultant for Faeth therapeutics, and is a consultant for Natera.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miller, E.D., Hitchcock, K.E. & Romesser, P.B. Oligometastatic Colorectal Cancer: A Review of Definitions and Patient Selection for Local Therapies. J Gastrointest Canc 54, 1116–1127 (2023). https://doi.org/10.1007/s12029-022-00900-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-022-00900-5