Abstract
Background
Transcranial Doppler (TCD) is a noninvasive bedside tool for cerebral hemodynamic assessments in multiple clinical scenarios. TCD, by means of measuring systolic and diastolic blood velocities, allows the calculation of the pulsatility index (PI), a parameter that is correlated with intracranial pressure (ICP). Nevertheless, the predictive value of the PI for raised ICP appears to be low, as it is subjected to several, often confounding, factors not related to ICP. Recently, the pulsatile apparent resistance (PaR) index was developed as a PI corrected for arterial blood pressure, reducing some of the confounding factors influencing PI. This study compares the predictive value of PaR versus PI for intracranial hypertension (IH) (ICP > 20 mm Hg) in patients with traumatic brain injury.
Methods
Patients with traumatic brain injury admitted to the neurocritical care unit who required invasive ICP monitoring were included prospectively within 5 days of admission. TCD measurements were performed in both middle cerebral arteries, allowing calculations of the PI and PaR. The optimal cutoff, discriminative power of these parameters for ICP ≥ 20 mm Hg, was assessed by calculating the area under the receiver operator characteristics curve (AUC).
Results
In total, 93 patients were included. A total of 20 (22%) patients experienced IH during the recording sessions. The discriminative power was low for PI (AUC 0.63) but slightly higher for PaR (AUC 0.77). Nonparametric analysis indicated significant difference for PaR when comparing patients with (median 0.169) and without IH (median − 0.052, p = 0.001), whereas PI medians for patients with and without IH were 0.86 and 0.77, respectively (p = 0.041). Regarding subanalyses, the discriminative power of these parameters increased after exclusion of patients who had undergone a neurosurgical procedure. This was especially true for the PaR (AUC 0.89) and PI (AUC 0.72). Among these patients, a PaR cutoff value of − 0.023 had 100% sensitivity and 52.9% specificity.
Conclusions
In the present study, discriminative power of the PaR for discriminating IH was superior to the PI. The PaR seems to be a reliable noninvasive parameter for detecting IH. Further studies are warranted to define its clinical application, especially in aiding neurosurgical decision making, following up in intensive care units, and defining its ability to indicate responses according to the therapies administered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
One of the most serious conditions in patients with severe brain injury (SBI) is intracranial hypertension (IH) [1]. It has been demonstrated that the responses of cerebral vasculature to changes in intracranial pressure (ICP) are much more attenuated than the responses to changes in the arterial blood pressure (ABP) [2], which indicates that IH should be aggressively managed [1, 3]. Moreover, once a patient has suffered with IH, the impairment in cerebral autoregulation (which is a set of cerebrovascular properties to stabilize cerebral blood flow despite the variations of multiple parameters, such as ABP and partial carbon dioxide pressure, for example) [4] will be proportional to the brain injury severity and will remain impaired even after ICP is brought back to standard levels [2].
Which ICP value should trigger therapy remains uncertain [5, 6]. Several authors defend the use of multiple noninvasive diagnostic tools in combination with invasive ICP monitoring, rather than relying exclusively on a predetermined static threshold [7,8,9,10,11,12]. In this setting, transcranial Doppler (TCD) is one of the most applied techniques, because of the automated calculation of the pulsatility index (PI), as an indicator of cerebral perfusion pressure (CPP) [13], or manually estimate CPP and ICP combining cerebral blood velocities (CBvs) with mean ABP [12, 14]. PI is known to correlate with ICP, but over a wide range and large values variation [15, 16].
The recent development of an automated whole TCD waveform analysis allowed the assessment of cerebral hemodynamic changes in older patients [17], patients who underwent a carotid endarterectomy [18], and during fluid resuscitation in sepsis [19]. By comparing the TCD waveform analysis with the ABP waveform a new cerebrovascular resistance index has been conceived, the pulsatile apparent resistance (PaR) index. Theoretically, comparing CBv pulsatility with ABP pulsatility could be a more efficient approach to detect IH than the conventional PI, as IH leads to ICP pulse amplification [20] and an increased mismatch in the relation between ABP (measured mostly in the radial artery) and CBv. Therefore, the aim of the present study was to explore this new TCD-derived parameter regarding its discriminative power for IH, testing the hypothesis that the PaR ability in detecting IH would be higher than that of PI.
Methods
This was a single center, retrospective analysis of data collected during a prospective and observational study performed in the Hospital das Clínicas, São Paulo University, Brazil. The study protocol was approved by the local ethics committee on May 23, 2017 (institutional review board 66,721,217.0.0000.0068) and registered under the number NCT03144219 (available at ClinicalTrials.gov). All research was performed in accordance with the relevant guidelines and regulations. Consent for participation was obtained from either legally authorized representatives or the next of kin because patient consent could not be obtained in these severely ill patients.
Participants and Protocol
Patients admitted to the neurocritical care unit were included within 5 days of hospital admission if (1) traumatic brain injury was the primary diagnosis and (2) they had been submitted to insertion of an intraventricular catheter for ICP monitoring. Therefore, all included patients had either exclusively a burr hole for ICP monitoring or underwent a craniotomy or even a craniectomy. Decision for surgical management was based either on the presence of mass lesions greater than 30 cm3, midline shift more than 0.5 cm, or imminent risk of herniation in the case of severe brain swelling on admission computed tomography scans. Excluded were patients with no proper TCD acoustic windows, patients showing signs of brain death (i.e., bilateral unreactive dilated pupils), and those with significant intracranial stenosis, as determined by premeasurement ultrasound. Clinical and laboratory variables were collected simultaneously with TCD assessment.
Materials
Cerebral blood velocity was recorded bilaterally in the middle cerebral arteries (MCAs) with TCD (Doppler Box; DWL Compumedics, Singen, Germany) equipped with a 2-MHz probe. Recordings were performed by one experienced neurosonologist (SB) and initiated after best MCAs signal quality was acquired, without insonation angle variation during the session. Intraventricular ICP was calibrated with patients at head up tilt 30 degrees and measured with the Neurovent monitoring system using a solid-state transducer (Raumedic, Munchberg, Germany). ABP was recorded invasively with a radial artery catheter. The pressure transducer was leveled and zeroed to the intersection of the anterior axillary line and the fifth intercostal space. End-tidal CO2 was measured continuously with an infrared capnograph (Dixtal, DX 1265 End-tidal CO2 CAPNOGARD, Manaus, Brazil).
The continuous recordings of bilateral MCA velocity (MCAv) (in centimeters per second) and ABP (in millimeters of mercury) allowed beat-by-beat waveform analysis. This was integrated into automated whole waveform analysis using Neuromon software (Version 10.3), which derived peak systolic velocity, end diastolic velocity, and mean velocity from the TCD waveforms and their correspondent systolic pressure peak and end diastolic pressure from the ABP signals (Fig. 1). The software also performed advanced waveform analysis, separating the systolic velocities into a first systolic peak (Sys1) and second systolic peak (Sys2). This separation previously allowed distinction between groups when the traditional parameters did not [21].
The improved extraction of parameters found in transcranial Doppler pulse waveform. Sys1 marks maximum stroke, Sys2 marks the ejection phase, and D560 marks diastolic velocity 560 ms after stroke onset (source: Dr. Schaafsma, available at https://www.neuromon.eu/index.php/en/). BV, blood velocity, PVR, peripheral vascular resistance Sys1, first systolic peak, Sys2, second systolic peak
Measurements
Each recording session lasted around 10 min, allowing the acquisition of approximately 700 heartbeats per session. PI and PaR were subsequently determined for bilateral TCD measurements. PI was calculated as (peak systolic velocity−end diastolic velocity)/mean velocity [15]. The apparent resistance (aR) was defined as the relation between synchronized MCAv and ABP at any moment in time:
Theoretically, dividing mean blood pressure (mm Hg) through flow (ml/100g/min) would give a measure for vascular resistance. TCD, however, delivers blood velocity, therefore, it was decided to name this ratio “apparent resistance.”
Under normal conditions, for MCA, the aR is higher during diastole than during systole since cerebrovascular resistance works as a high-pass filter allowing the blood to enter during systole more easily than during diastole [21]. Hence, to obtain a positive value for the PaR:
where in systolic_aR can be defined based on either the Sys1 or the Sys2. Unless in the cases of aortic valve insufficiency or significant arterial stiffness, Sys1 is the highest peak observed. In IH, the resistance elevation is naturally even more pronounced over diastole increasing the PI, but the latter also suffers with influence of the intravascular volume. Therefore, the PaR included in its formula the ABP pulsatility from an extracranial artery (radial artery in this study), by which, in the case of progressive raise in ICP, would show progressive positive values accordingly:
The theory of arterial acceleration predicts that the penetration force of the Sys1 component is largest since it is derived from a peristaltic wave, amplifying the pressure wave from proximal to distal. It predicts that the Sys2 component has less penetration force since this part of the signal is derived from actual cardiac outflow. The diastolic part has even lower penetration force. In the PaR ratio the high apparent resistance during diastole can therefore best be related to the lowest apparent resistance during Sys1 (instead of Sys2) [21].
Furthermore, a negative value for PaR indicates that the apparent resistance during diastole is lower than during systole, meaning that MCAv during diastole is higher and/or during systole is lower than expected based on the ABP signal. Such a situation occurs when cerebrovascular resistance is low, for instance, in carotid artery stenosis [17], after decompressive craniectomy [22] or when facing posttraumatic hyperemia [23]. The latter two conditions found in the present study.
Statistical Analysis
To determine the discriminative power of PaR and PI, bilateral values of both were collected. Patients were divided in two groups based on invasively measured ICP: group 1, normal ICP, and group 2, IH, which was defined as ICP ≥ 20 mm Hg. Baseline variables were presented as median and interquartile range (IQR), whereas categorical baseline data were reported as number and percentage. Discriminative power of PI and PaR for IH was assessed through area under the curve (AUC) obtained from receiver operator characteristics analysis, reported with a 95% confidence interval. An AUC of < 0.7 was considered to represent weak discriminative power, whereas AUC 0.7–0.8 was considered acceptable, 0.8–0.9 strong, and > 0.9 excellent [24]. To obtain an optimal cutoff value for the PaR and PI, the true negative (TN) and false positive (FP) results were equaled to TN and false negative (FN) results according to TN + FP = 0.5 × (TN + FN). This formula was weighted with a factor 0.5 to decrease the FN at the cost of extra FP. The nonparametric Mann–Whitney U-test was used to calculate PI and PaR differences between groups 1 and 2. Subanalyses were performed to determine whether discriminative power of either PI or PaR would improve in specific situations according to type of neurosurgical intervention. All statistical analyses were performed using SPSS for Windows (Version 25).
Results
Baseline Characteristics
Ninety-three patients were included in the final analysis. PaR could not be determined in 17 patients because blood pressure readings were unavailable, yet data of these patients were used to determine discriminative power of PI. The included population was predominantly male (85%) and young (median age 32 years, IQR 21–48). Neurosurgery had been performed in the majority (64%). There was no significant difference in baseline characteristics between groups except for ICP (Table 1). IH was experienced by 20 patients (22%), with a median ICP of 24 mm Hg (IQR 22–29). A post hoc power analysis was performed using the PaR data, resulting in 97.7% power to detect an effect size of 0.38. From the total sample of 93 patients, 78,562 waveforms were obtained for signal processing and parameters averaging. The subanalyses repeated calculations excluding the 23 patients with craniectomy (n = 70) or including closed-skull patients exclusively (n = 33). For these situations, 51,055 and 24,922 CBv and ABP waveforms were assessed, respectively.
PI
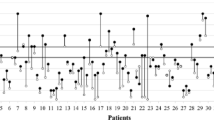
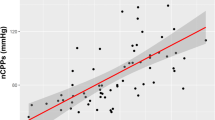
Data of the right MCA were available for 91 patients. Median PI was 0.79 (IQR 0.64–0.96) and slightly higher in patients with IH (median 0.83, IQR 0.72–1.1). The same was observed in left-sided measurements available for 93 patients: median PI was 0.80 (IQR 0.65–0.94) and was slightly increased in IH (median 0.85, IQR 0.73–1.1). Nonparametric testing for mean PI indicated significant differences between patients with normal ICP (median 0.77, n = 73) and patients with elevated ICP (median 0.86, n = 20), U = 511, z = 0.2048, p = 0.041. PI AUC was 0.63 (0.49–0.79) for discriminating ICP > 20 mm Hg (Fig. 2). Fourteen patients with IH (70%) and 30 patients with ICP < 20 mm Hg (41%) presented PI value of 0.73.
PaR Index
Right-sided PaR could be calculated for 76 patients, with a median of 0.046 (IQR − 0.091 to 0.164). It was significantly higher in patients with IH (median 0.107, IQR 0.051–0.241). Left side PaR was determined for 75 patients and tended to be slightly lower (median 0.08, IQR − 0.029 to 0.22), yet also significantly higher in IH (median 0.201, IQR 0.068–0.390; Table 2). Correlations for PI and PaR were best among patients with IH (r 0.77, p < 0.0001), indicating high sensitivity of PaR to discriminate IH (Table 2). PaR nonparametric testing indicated significant differences between patients with normal ICP (median − 0.052, n = 58) and patients with elevated ICP (median 0.169, n = 18), U = 24, z = 3.43, p = 0.001 (Fig. 3). PaR AUC was 0.77 (0.61–0.85) for discriminating ICP > 20 mm Hg (Fig. 2). With a cutoff value of − 0.06, PaR negative predictive value was 93%, with 35% positive predictive value. The positive predictive value increased with progressive PaR values (Supplemental material).
Subanalyses According to Neurosurgical Procedure
The discriminative power for IH improved for both parameters in patients who did not have neurosurgery (with intact skull apart from a burr hole for invasive ICP measurement). When excluding patients with craniectomy was not observed a great change in results (PaR AUC 0.78 [0.65–0.92]) but analyzing patients with undamaged skull and no surgical manipulation exclusively, the PaR AUC augmented to 0.88 (0.72–1, Fig. 2). In the patient group without neurosurgery, the PI cutoff 0.71 presented 83.3% sensitivity and 47.1% specificity. For PaR the optimal cutoff value was − 0.02 with a sensitivity and negative predictive value of 100% as well as specificity of 53%. For all skull conditions, PaR showed higher AUCs than PI. Nevertheless, for both parameters, linear correlations with either ICP or CPP were poor to fair (Table 3).
Discussion
The results of this study indicate a satisfactory performance for the PaR in identifying IH, which was poor for the PI among 93 patients with SBI. In a subgroup analysis excluding craniectomized patients, the results remained similar but improved significantly once only undamaged skull patients were assessed. The PI, although disclosing a similar behavior, did not reach an AUC > 0.8, even among patients with undamaged skulls. Therefore, whereas PI presented a low but higher linear correlation with ICP and CPP, the PaR presented a higher discriminative power for IH, indicating a potential for the utilization of these parameters in combination.
Previous studies correlating the PI with IH have shown diverse results [15, 16, 25]. Probably the best results for the PI correlation with ICP were observed in the study of Bellner et al. [15], who studied intensive care patients with a wide range of ICP values (from 0 to 112 mm Hg). Such high correlation was not reproduced in the present study (with ICP ranging from 2 to 36 mm Hg) as well as in previous studies [26,27,28]. Moreover, in the present study IH was present despite a much lower PI than observed in the study of Bellner et al. [15], but in agreement of the study of Kaloria et al. [16], which indicates the inaccuracy of PI in assessing IH when used alone, especially during posttraumatic hyperemic stages.
On the contrary, when interpreting the PI in the setting of acute brain injuries, one should take into account that other factors may increase it, such as aging [29], diabetes [30], arterial hypertension [31], sepsis [32], dehydration, blood viscosity [33], ventilation/oxygenation [34], and sedatives as barbiturates [35], among others. Thus, PI elevation may be a better indicator of some degree of CPP reduction than a surrogate marker for IH [36, 37]. In fact, a reliable determination of CPP is the goal when monitoring ICP, but the simplistic assumption of CPP being the exclusive interaction between mean ABP and mean ICP is inaccurate [2, 38]. In fact, given that TCD waveforms are derived from an integration of intravascular volume, cerebrovascular resistance, metabolic reactivity, and arterial ejection capacity, they support strongly and are more reliable in translating actual CPP than the simplistic subtraction of mean ABP for mean ICP [2, 38], as this approach ignores the waterfall mechanism of cerebrovascular resistance [39], the heterogenous distribution of injury severity through the brain [40], and the fact that invasive ABP is normally measured in brachial arteries, which possibly does not correspond precisely with intracranial ABP [41].
Reducing IH discriminative power for noninvasive techniques once the skull has been manipulated by either traumatic brain injury or neurosurgical procedures has been observed previously in studies analyzing TCD [2], invasive [42] and noninvasive ICP pulse morphology [43], and pupillometry [11]. This difference is believed to be due to the changes in intracranial physiology, as the modification in cerebrospinal fluid transit and cerebral autoregulation impairment once the brain is damaged or the skull and dura have been opened [44].
In 2012, new parameters were advocated, making a distinction between two peaks in systole and determining the diastolic velocity at a fixed time after stroke onset instead of the end of diastole, making the diastolic velocity depend less on heart rate [21]. These parameters, conceived for TCD, can also be used for a continuous recording of ABP, in which a first and second peak can also readily be distinguished. Combining the new parameters with the rationale for the PI has led to the PaR, best described as a blood pressure corrected PI. Because the analysis is performed on each signal separately, the procedure does not require synchronization.
The PaR was developed in search for a more reliable noninvasive IH screening tool. Standard representation of MCA blood velocity involves peak systolic, end diastolic, and mean velocity. The PI is calculated as the ratio of peak systolic minus end diastolic blood velocity divided by the mean velocity. An advantage of the PI is elimination of the angle of insonation and cross-sectional area by calculating their ratio, since both factors despite unknown, will contribute to MCA blood velocity in the nominator as well as in the denominator of the ratio [45].
At increased ICP, the ABP has to overcome tissue pressure in order to result in tissue perfusion. The blood velocity signal may become more pulsatile because it depends more on the systolic phase of ABP and diastolic flow may become nulled as is the case, for instance, in reverberating waves or systolic spikes. This explains why the PaR is a better indicator of IH than the PI. At very high ICP, the MCA waveform turns to so called systolic spikes: a signal only containing a Sys1 peak with no flow during late systole nor during diastole [46]. The apparent resistance during diastole will approach infinity (because of division through nearly zero), allowing the PaR to reach extremely high values, at least for as long as some flow remains present. That Sys1 is more resistant to tissue pressure elevation than Sys2 and diastolic flow can be demonstrated in a simple experiment measuring radial artery flow during inflation of a blood pressure cuff positioned around the hand [47]. The sensitivity of the PaR for IH seems to be enhanced by the fact that many patients with SBI without IH manifested with negative, rather than positive values for this ratio. Negative values indicate a decrease in cerebrovascular resistance; in this particular group, this is most likely because of posttraumatic hyperemia.
Strengths of this study are that it was designed to assess neurocritical patients up to 5 days after injury, hence, secondary conditions as sepsis and vasospasm were avoided. In addition, the 10-min sessions for data acquisition precluded significant variations in ABP, oxygenation, and changes in sedation, allowing clear correlations between ICP, ABP and CBv. This improved parametrization of CBv synchronous to ABP slopes may allow the development of a new way to estimate CPP. When a continuous recording of ABP is also available, as it is often the case on the intensive care unit, both signals may be compared automatically. Notwithstanding, the PaR would not be part of a dedicated software exclusively, because physicians can learn its formula and apply it at the bedside.
Limitations of this study are that measurement of MCAv may not reflect the entire brain hemodynamic situation, with potential to underestimate compartmental IH, especially in the posterior fossa. In addition, the calculation of PI in a large segment of the MCA may not reflect the exact cerebrovascular resistance in the pial arteries and capillaries. Furthermore, there were no preoperative and postoperative measurements done in patients who underwent surgery. Future studies are required to explore (1) whether TCD monitoring of patients with SBI at, for instance, 4–6-h intervals, is a safe alternative when invasive ICP measurement is not available, or (2) whether TCD monitoring is a useful adjunct to clinical decision making in patients with invasive ICP measurement.
Conclusions
The PaR index demonstrated better performance than Gosling PI for the screening of raised ICP. This index may be useful to indicate ICP monitoring for those at risk of developing IH during their ICU stay, nevertheless, decompressive craniectomy may decreased PaR IH assessment accuracy. The PaR discriminative power for IH suggests the use of this parameter in combination with PI to raise assumptions on CPP. Future studies must define its applicability role and its role as an outcome marker.
References
Robba C, Citerio G. How I manage intracranial hypertension. Crit Care. 2019;23(1):243. https://doi.org/10.1186/s13054-019-2529-z.
Brasil S, Nogueira RC, Salinet ASM, et al. Contribution of intracranial pressure to human dynamic cerebral autoregulation after acute brain injury. Am J Physiol Regul Integr Comp Physiol. 2023;324(2):R216–26. https://doi.org/10.1152/ajpregu.00252.2022.
Smith M. Cerebral perfusion pressure. Br J Anaesth. 2015;115(4):488–90. https://doi.org/10.1093/bja/aev230.
Brassard P, Labrecque L, Smirl JD, et al. Losing the dogmatic view of cerebral autoregulation. Physiol Rep. 2021;9(15):e14982. https://doi.org/10.14814/phy2.14982.
Wijdicks EFM. 10 or 15 or 20 or 40 mmHg? What is increased intracranial pressure and who said so? Neurocrit Care. 2022;36(3):1022–6. https://doi.org/10.1007/s12028-021-01438-3.
Helbok R, Meyfroidt G, Beer R. Intracranial pressure thresholds in severe traumatic brain injury: Con: the injured brain is not aware of ICP thresholds! Intensive Care Med. 2018;44(8):1318–20. https://doi.org/10.1007/s00134-018-5249-y.
Rubiano AM, Figaji A, Hawryluk GW. Intracranial pressure management: moving beyond guidelines. Curr Opin Crit Care. 2022;28(2):101–10. https://doi.org/10.1097/MCC.0000000000000920.
Robba C, Frigieri G, Brasil S, Taccone FS. Early prognostic value of non-invasive intracranial pressure methods in brain-injured patients. Intensive Care Med. 2022. https://doi.org/10.1007/s00134-022-06899-4.
Brasil S, Frigieri G, Taccone FS, et al. Noninvasive intracranial pressure waveforms for estimation of intracranial hypertension and outcome prediction in acute brain-injured patients. J Clin Monit Comput. 2022. https://doi.org/10.1007/s10877-022-00941-y.
Brasil S. Intracranial pressure pulse morphology: the missing link? Intensive Care Med. 2022. https://doi.org/10.1007/s00134-022-06855-2.
Jahns FP, Miroz JP, Messerer M, et al. Quantitative pupillometry for the monitoring of intracranial hypertension in patients with severe traumatic brain injury. Crit Care. 2019;23(1):155. https://doi.org/10.1186/s13054-019-2436-3.
Rasulo FA, Calza S, Robba C, et al. Transcranial Doppler as a screening test to exclude intracranial hypertension in brain-injured patients: the IMPRESSIT-2 prospective multicenter international study. Crit Care. 2022;26(1):110. https://doi.org/10.1186/s13054-022-03978-2.
Robba C, Cardim D, Tajsic T, et al. Non-invasive intracranial pressure assessment in brain injured patients using ultrasound-based methods. Acta Neurochir Suppl. 2018;126:69–73. https://doi.org/10.1007/978-3-319-65798-1_15.
Czosnyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD. Cerebral perfusion pressure in head-injured patients: a noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg. 1998;88(5):802–8. https://doi.org/10.3171/jns.1998.88.5.0802.
Bellner J, Romner B, Reinstrup P, Kristiansson KA, Ryding E, Brandt L. Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg Neurol. 2004;62(1):45–51. https://doi.org/10.1016/j.surneu.2003.12.007.
Kaloria N, Panda NB, Bhagat H, et al. Pulsatility index reflects intracranial pressure better than resistive index in patients with clinical features of intracranial hypertension. J Neurosci Rural Pract. 2020;11(1):144–50. https://doi.org/10.1055/s-0039-3399477.
Schaafsma A. A new method for correcting middle cerebral artery flow velocity for age by calculating Z-scores. J Neurosci Methods. 2018;307:1–7. https://doi.org/10.1016/j.jneumeth.2018.06.009.
Schaafsma M, Glade GJ, Keller PJ, Schaafsma A. Age corrected changes in intracranial hemodynamics after carotid endarterectomy. J Cardiovasc Surg (Torino). 2021;62(4):354–63. https://doi.org/10.23736/S0021-9509.21.11705-7.
de Goede AA, Loef BG, Reidinga AC, Schaafsma A. Fluid resuscitation in septic patients improves systolic but not Diastolic middle cerebral artery flow velocity. Ultrasound Med Biol. 2017;43(11):2591–600. https://doi.org/10.1016/j.ultrasmedbio.2017.06.027.
Czosnyka Z, Keong N, Kim DJ, et al. Pulse amplitude of intracranial pressure waveform in hydrocephalus. Acta Neurochir Suppl. 2008;102:137–40. https://doi.org/10.1007/978-3-211-85578-2_28.
Schaafsma A. Improved parameterization of the transcranial Doppler signal. Ultrasound Med Biol. 2012;38(8):1451–9. https://doi.org/10.1016/j.ultrasmedbio.2012.03.016.
Bor-Seng-Shu E, Hirsch R, Teixeira MJ, De Andrade AF, Marino R Jr. Cerebral hemodynamic changes gauged by transcranial Doppler ultrasonography in patients with posttraumatic brain swelling treated by surgical decompression. J Neurosurg. 2006;104(1):93–100. https://doi.org/10.3171/jns.2006.104.1.93.
Martin NA, Patwardhan RV, Alexander MJ, et al. Characterization of cerebral hemodynamic phases following severe head trauma: hypoperfusion, hyperemia, and vasospasm. J Neurosurg. 1997;87(1):9–19. https://doi.org/10.3171/jns.1997.87.1.0009.
Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978;8(4):283–98. https://doi.org/10.1016/s0001-2998(78)80014-2.
de Riva N, Budohoski KP, Smielewski P, et al. Transcranial Doppler pulsatility index: what it is and what it isn’t. Neurocrit Care. 2012;17(1):58–66. https://doi.org/10.1007/s12028-012-9672-6.
Figaji AA, Zwane E, Fieggen AG, Siesjo P, Peter JC. Transcranial Doppler pulsatility index is not a reliable indicator of intracranial pressure in children with severe traumatic brain injury. Surg Neurol. 2009;72(4):389–94. https://doi.org/10.1016/j.surneu.2009.02.012.
Behrens A, Lenfeldt N, Ambarki K, Malm J, Eklund A, Koskinen LO. Transcranial Doppler pulsatility index: not an accurate method to assess intracranial pressure. Neurosurgery. 2010;66(6):1050–7. https://doi.org/10.1227/01.NEU.0000369519.35932.F2.
Cardim D, Robba C, Donnelly J, et al. Prospective study on noninvasive assessment of intracranial pressure in traumatic brain-injured patients: comparison of four methods. J Neurotrauma. 2016;33(8):792–802. https://doi.org/10.1089/neu.2015.4134.
Tegeler CH, Crutchfield K, Katsnelson M, et al. Transcranial Doppler velocities in a large, healthy population. J Neuroimaging. 2013;23(3):466–72. https://doi.org/10.1111/j.1552-6569.2012.00711.x.
Wielicka M, Neubauer-Geryk J, Kozera G, Bieniaszewski L. Clinical application of pulsatility index. Med Res J. 2020;5(3):201–10. https://doi.org/10.5603/MRJ.a2020.0016.
Kneihsl M, Hofer E, Enzinger C, et al. Intracranial pulsatility in relation to severity and progression of cerebral white matter hyperintensities. Stroke. 2020;51(11):3302–9. https://doi.org/10.1161/STROKEAHA.120.030478.
de Azevedo DS, Salinet ASM, de Lima OM, Teixeira MJ, Bor-Seng-Shu E, de Carvalho NR. Cerebral hemodynamics in sepsis assessed by transcranial Doppler: a systematic review and meta-analysis. J Clin Monit Comput. 2017;31(6):1123–32. https://doi.org/10.1007/s10877-016-9945-2.
Han JE, Kim T, Park JH, et al. Middle cerebral artery pulsatility is highly associated with systemic blood viscosity in acute ischemic stroke within 24 hours of symptom onset. J Neurosonol Neuroimag. 2019;11(2):126–31. https://doi.org/10.31728/jnn.2019.00050.
Kim J. Pictorial essay: transcranial doppler findings of the intracranial and extracranial diseases. J Neurosonol Neuroimag. 2019;11(1):2–21. https://doi.org/10.31728/jnn.2018.00039.
Newell DW. Transcranial Doppler ultrasonography. Neurosurg Clin N Am. 1994;5(4):619–31.
Voulgaris SG, Partheni M, Kaliora H, Haftouras N, Pessach IS, Polyzoidis KS. Early cerebral monitoring using the transcranial Doppler pulsatility index in patients with severe brain trauma. Med Sci Monit. 2005;11(2):CR49-52.
Robba C, Pozzebon S, Moro B, Vincent JL, Creteur J, Taccone FS. Multimodal non-invasive assessment of intracranial hypertension: an observational study. Crit Care. 2020;24(1):379. https://doi.org/10.1186/s13054-020-03105-z.
Brasil S, de Carvalho Nogueira R, Salinet ÂSM, et al. Critical closing pressure and cerebrovascular resistance responses to intracranial pressure variations in neurocritical patients. Neurocrit Care. 2023. https://doi.org/10.1007/s12028-023-01691-8.
Ince J, Minhas JS, Panerai RB. JCBFM point/counterpoint series: point/counterpoint: cerebrovascular resistance is a flawed concept. J Cereb Blood Flow Metab. 2023. https://doi.org/10.1177/0271678x231172854.
Godoy DA, Brasil S, Iaccarino C, Paiva W, Rubiano AM. The intracranial compartmental syndrome: a proposed model for acute brain injury monitoring and management. Crit Care. 2023;27(1):137. https://doi.org/10.1186/s13054-023-04427-4.
Spence JD. Blood pressure gradients in the brain: their importance to understanding pathogenesis of cerebral small vessel disease. Brain Sci. 2019. https://doi.org/10.3390/brainsci9020021.
Brasil S, Solla DJF, Nogueira RC, Jacobsen Teixeira M, Malbouisson LMS, Paiva WS. Intracranial compliance assessed by intracranial pressure pulse waveform. Brain Sci. 2021. https://doi.org/10.3390/brainsci11080971.
Brasil S, Solla DJF, Nogueira RDC, Teixeira MJ, Malbouisson LMS, Paiva WDS. A novel noninvasive technique for intracranial pressure waveform monitoring in critical care. J Personal Med. 2021;11(12):1302.
Bor-Seng-Shu E, Figueiredo EG, Fonoff ET, Fujimoto Y, Panerai RB, Teixeira MJ. Decompressive craniectomy and head injury: brain morphometry, ICP, cerebral hemodynamics, cerebral microvascular reactivity, and neurochemistry. Neurosurg Rev. 2013;36(3):361–70. https://doi.org/10.1007/s10143-013-0453-2.
Boote EJ. AAPM/RSNA physics tutorial for residents: topics in US: Doppler US techniques: concepts of blood flow detection and flow dynamics. Radiographics. 2003;23(5):1315–27. https://doi.org/10.1148/rg.235035080.
Nagai H, Moritake K, Takaya M. Correlation between transcranial Doppler ultrasonography and regional cerebral blood flow in experimental intracranial hypertension. Stroke. 1997;28(3):603–7. https://doi.org/10.1161/01.str.28.3.603.
Schaafsma A. Harvey with a modern twist: how and why conducting arteries amplify the pressure wave originating from the heart. Med Hypotheses. 2014;82(5):589–94. https://doi.org/10.1016/j.mehy.2014.02.016.
Funding
The present study received no funding.
Author information
Authors and Affiliations
Contributions
SB and RCN conceived and designed the study. RCN provided supervision and training. SB performed measurements and wrote manuscript. HR performed data analysis and statistical analysis. AS designed software, performed data analysis and wrote manuscript. SB, RCN, HR, EKH, and AS revised manuscript. All authors agree to be accountable for all aspects of the work. All persons designated as authors qualify for authorship and all those who qualify for authorship are listed. The data that support the findings of this study are available from the corresponding author upon reasonable request. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
AS is owner of MEAR Holding BV, an institution aiming to improve neuromonitoring at the intensive care unit. MEAR Holding BV holds an international patent on “PaR Technology” restricting its commercial application in several countries. SB, RCN, HR, EKH declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
The authors confirm compliance with Ethical approval and informed consent for human studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix: Description of Automatic TCD of ABP Analysis Detecting Sys1, Sys2 and D560
Appendix: Description of Automatic TCD of ABP Analysis Detecting Sys1, Sys2 and D560
Calculate the average waveform from available heartbeats within a 10s. recording
-
1.
Select a 10s period from the continuous signal
-
2.
Remove high frequency noise by applying a 10th order Butterworth filter
-
3.
Calculate its first order derivative to detect heartbeat onset
-
4.
Cut the signal into fragments at each heartbeat onset
-
5.
Remove outliers by excluding single heartbeats deviating from the Euclidian norm reference
-
6.
Calculate the average wave form from the remaining heartbeats
Calculate Sys1, Sys2 and D560 from the average waveform
-
1.
Calculate D560 by taking the average blood velocity over an interval of 80ms centered around the value 560ms after heartbeat onset
-
2.
Determine the location of the incisure of the average waveform
-
3.
Calculate the first and second order derivatives of the systolic part of the average waveform
-
4.
Determine which situation describes the signal best from the location of zero crossings of the first or second order derivatives:
-
1.
Sys1 exclusive (no Sys2)
-
2.
Sys1 dominant (Sys2 shoulder)
-
3.
Sys1-Sys2 balanced (Sys1 and Sys2 separate peaks)
-
4.
Sys2 dominant (Sys1 shoulder)
-
5.
Sys2 exclusive (no Sys1)
-
1.
-
5.
Determine the Sys1 and Sys2 amplitudes from the calculated locations of zero crossings of the first and second order derivatives
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brasil, S., Romeijn, H., Haspels, E.K. et al. Improved Transcranial Doppler Waveform Analysis for Intracranial Hypertension Assessment in Patients with Traumatic Brain Injury. Neurocrit Care 40, 931–940 (2024). https://doi.org/10.1007/s12028-023-01849-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01849-4