Abstract
Background
Status epilepticus (SE) often does not respond to initial treatment. A second-line agent with a less established safety and efficacy profile is then required. This study examined the safety of intravenous (IV) lacosamide (LCM) in a critically ill population and obtained an estimate of effectiveness in patients with refractory SE on continuous video EEG monitoring (cEEG).
Methods
Retrospective review of critically ill patients in SE on cEEG treated with IV LCM from June 2009 to April 2011.
Results
Eighty-four patients in SE (43 F/41 M), mean age 59.6 years, were identified; and 59.5 % had nonconvulsive SE. The most common etiologies were ischemic and hemorrhagic strokes. There were no significant changes in serial blood pressure monitoring, PR prolongation, aspartate aminotransferase (AST), or creatinine pre- and post-LCM. There was a significant increase in alanine aminotransferase (ALT) from days 1–7 (p = 0.031). Fifty-one patients were LCM-naïve. In these patients, cessation of SE on cEEG after LCM occurred in 15.7, 25.5, 58.8, and 82.4 % by 4, 12, 24, and 48 h, respectively.
Conclusion
IV LCM appears safe short term in critically ill patients with SE. The retrospective estimate of effectiveness for LCM appears promising for management in SE. Prospective, randomized controlled studies are needed to better determine the role of LCM in treating SE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Status epilepticus is a neurological emergency with significant morbidity and mortality. It may occur with convulsions or be nonconvulsive. In 40 % of cases, it is often refractory to initial medical therapy [1, 2]. Algorithms have been developed for type, timing, and dosing of subsequent antiepileptics [3]. However, many of these medications are outdated and have significant side effects, particularly affecting the cardiovascular, respiratory, and hepatic systems [4–7]. Additional intravenous antiepileptic drugs (AEDs) have been developed with more favorable side effect profiles, but none have been systematically studied. One such antiepileptic is lacosamide.
Lacosamide (LCM) has a novel mechanism of action by enhancing slow inactivation of the voltage-gated sodium channel without affecting fast inactivation [8–12]. Previous studies have evaluated lacosamide in status epilepticus finding it to be both efficacious and safe [13–16]. The safety in critically ill patients makes it an ideal anticonvulsant in the treatment of status epilepticus. It has been shown to have a low rate of hemodynamic changes, elevated liver function tests, cardiac arrhythmias, renal dysfunction, and hypersensitivity [14]. The difficulty in interpreting many of the safety and effectiveness studies is the smaller sample sizes. The purpose of our study was to evaluate the safety and effectiveness of lacosamide in a larger cohort of critically ill patients with status epilepticus at a tertiary care center.
Methods
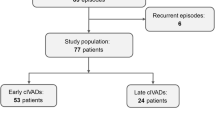
Consecutive patient charts from 2009 to 2011 diagnosed with status epilepticus and treated with at least one dose of intravenous lacosamide at a large tertiary care center were retrospectively reviewed from a prospectively collected database. Patients were noted whether they were lacosamide-naïve for effectiveness analysis. Further inclusion required all patients to be monitored on continuous EEG (cEEG) prior to administration of lacosamide and at least 48 h after administration (Fig. 1). The charts were then reviewed for demographic data, seizure risk factors, seizure history including prior status and AEDs, and current and subsequent status epilepticus treatment. An institutional review board (IRB) approval was obtained prior to the start of data collection.
Safety Assessment
All patients who met inclusion criteria during the study time frame were included in the safety assessment. The safety of lacosamide was evaluated in these patients by reviewing blood pressure pre-lacosamide and again at 1, 4, and 24 h after lacosamide administration. Hypotension was defined as a drop in systolic blood pressure of 20 mmHg at the measured time points when compared to pre-administration. Liver enzymes and creatinine were evaluated pre-lacosamide and 1 and 7 days post-lacosamide. Increase in liver function tests was defined as a twofold increase from the upper limit of normal (>120 U/L for AST and >100 U/L for ALT), and an elevation of creatinine was defined as an elevation of greater than 2.0 mg/dL [14]. The PR intervals on electrocardiogram (EKG) were reviewed pre-lacosamide and post-lacosamide and were considered increased if there was a >20 ms change.
Effectiveness of Lacosamide
In the lacosamide-naïve patients, we evaluated cessation of status with lacosamide at 4, 12, 24, and 48 h after treatment. We chose these time points based on pharmacokinetics of lacosamide. Lacosamide has been previously shown to have a time to peak of 4 h after oral administration [17]. Anesthetics were weaned prior to the administration of lacosamide. The cEEG reports and raw EEG data were then reviewed for onset and cessation of status epilepticus. The last antiepileptic drug administered before status epilepticus cessation was considered the terminating drug.
Convulsive status epilepticus was diagnosed if there was continued seizure activity for ≥5 min or multiple seizures without return of consciousness. Nonconvulsive status epilepticus was defined as a state of impaired consciousness associated with continuous and/or frequent electrographic epileptiform discharges on EEG lasting ≥10 s [18]. Refractory status epilepticus is failure to respond to a minimum of two AEDs. Cessation of status epilepticus was defined as the end of convulsive activity or resolution of previously documented electrographic seizure activity (i.e., evolution in field, morphology, and/or frequency of spikes, sharp waves, or rhythmic waveforms) for a minimum of 24 h [19]. All treatments were chosen at the discretion of the treating physician. In general, treatment followed algorithms previously proposed [3]. Outcomes were assessed by discharge status.
Differences between the two groups were assessed with descriptive statistics. Student’s t test and one-way analysis of variance (ANOVA; continuous variables with post hoc Dunnett’s) were used to analyze the safety variables. JMP 9 (Marlow, Buckinghamshire, UK) was used for statistical analyses.
Results
Patient Demographics
Eighty-four patients (average age 59.6 years, 51.2 % female) met the inclusion criteria for the safety analysis of lacosamide. The most common identifiable cause of status epilepticus was ischemic stroke (remote or acute, 16.7 %). Other causes included hemorrhagic strokes (subarachnoid, subdural, or intracerebral, 15.5 %), epilepsy (14.3 %), tumor (extra- or intra-axial, 14.3 %), metabolic/transplant (13.1 %), anoxia (9.5 %), remote brain injury (96.0 %), infection (meningoencephalitis or abscess, 6.0 %), neurodegenerative (3.6 %), and reperfusion injury (1.2 %). The majority (59.5 %) of seizures had no clinical signs. The baseline characteristics of the study population are shown in Table 1.
Adverse Events
Cardiac
An EKG was obtained prior to lacosamide in 78 of the 84 patients. The average initial PR interval was 153.7 ms. A post-lacosamide EKG was obtained on average 18.4 days after the initial dose. The post-lacosamide PR interval on this EKG was on average 157.7 ms (Fig. 2a). Eleven patients had an increase of >20 ms on PR interval (average 40.5 ms) from pre- to post-lacosamide EKGs. Overall, there was no significant difference in the pre-PR interval and the post-PR interval (p = 0.4).
Adverse effects of lacosamide a The PR interval on EKG pre- and post-lacosamide. There is no significant difference (p = 0.40). b The effects of lacosamide on systolic and diastolic blood pressure obtained immediately prior to lacosamide and 1, 4, and 24 h after lacosamide. There was no significant difference in SBP (p = 0.88) or DBP (p = 0.23). c The change in liver function tests from pre-lacosamide to 1 day and 7 days after showed no significant difference in AST (p = 0.27, p = 0.09, respectively; shaded boxes), but there was a significant increase from pre- to 7-day ALT (p = 0.69, p = 0.031, respectively; open boxes). d The change in creatinine from pre-lacosamide to 1 day and 7 days post-lacosamide showed no significant difference (p = 0.35). ALT alanine aminotransferase, AST aspartate aminotransferase, DBP diastolic blood pressure, LCM lacosamide, SBP systolic blood pressure
Five patients developed hypotension (average decrease of 26.2 mmHg) at 1 h after administration of lacosamide, eight were hypotensive (average decrease of 31.9 mmHg) at 4 h, and eight were hypotensive (average decrease of 28.3 mmHg) at 24 h after administration of lacosamide. Four of these patients required pressor support by 4 h after administration of lacosamide. Overall, there was no significant difference between the systolic or diastolic blood pressures at 1 (p = 0.43), 4 (p = 0.97), and 24 (p = 0.64) hours after lacosamide (Fig. 2b).
Hepatic
Liver function testing (aspartate aminotransferase [AST] and alanine aminotransferase [ALT]) was available pre- and 1 and 7 days post-lacosamide. At day 1 post-lacosamide, four patients (AST: n = 3, p = 0.27; ALT: n = 1, p = 0.69) developed an elevation in liver function testing (i.e., transaminitis). By day 7 post-lacosamide, eight patients (AST n = 3, p = 0.09; ALT: n = 5, p = 0.031) had transaminitis (Fig. 2c). The cause of worsening liver function was determined to be associated with acute pulmonary embolus resulting in cardiopulmonary arrest or another medication including pentobarbital, phenytoin, and/or antibiotics.
Renal
Creatinine was not significantly different from pre- and 1 and 7 days post-lacosamide (p = 0.18 and p = 0.21, respectively; Fig. 2d). One patient developed acute renal failure at day 7 post-lacosamide. This patient’s creatinine increased by 3.4 mg/dL. None developed acute renal failure by 1 day post-lacosamide.
Discharge
Forty-three patients (51.2 %) were discharged to a rehabilitation facility. Fourteen (16.7 %) were discharged home, and 27 (32.1 %) expired. All but three patients that were discharged were discharged on lacosamide (Table 1).
Effectiveness in Lacosamide-Naïve Patients
Fifty-one patients of the 84 met inclusion for the effectiveness profile arm of this study, i.e., naïve to lacosamide. The average age of the patients in this arm of the study was 60.8 ± 2.6 years. The average length of status was 23.5 ± 3.6 h prior to receiving lacosamide. The average load of lacosamide was 188.3 ± 150.1 mg followed by maintenance doses of 362.7 ± 134.1 mg/day. After receiving lacosamide, the length of status epilepticus was 31.1 ± 4.6 h. Excluding benzodiazepine administration, the majority of patients were given phenytoin or levetiracetam as first or second line with lacosamide being second to fourth line (median third-line agent; Fig. 3). When comparing medication responses at 4, 12, 24, and 48 h in the same patient, lacosamide was found to terminate seizures when coadministered with phenytoin and/or levetiracetam. At 4 h, 15.7 % of lacosamide patients responded which increased to 82.4 % by 48 h. In these patients, lacosamide was the terminating drug in 58.8 % (Table 2).
Lacosamide (LCM) dosing and administration. Excluding benzodiazepine administration, LCM was most often given as the second- to fourth-line medication (average 2.31, median 2). Excluding benzodiazepine administration, phenytoin (PHT) or levetiracetam (LEV) was most commonly given as the first or second line
Discussion
Intravenous lacosamide appears safe in our series of 84 critically ill patients with status epilepticus. The retrospective effectiveness estimate of lacosamide appears promising for status epilepticus. In patients who did not respond to either first- or second-line agents, 15.7 % of patients responded at 4 h and 82.4 % by 48 h after lacosamide. This highlights that the response of lacosamide seems promising in those patients who have failed prior anticonvulsant. The accuracy of the response rates was determined on cEEG.
Our results are similar to previous, smaller studies showing the effectiveness of lacosamide. In the small, retrospective study by Cherry et al. (2011), thirteen episodes of refractory status epilepticus were identified of which 5 (38 %) had cessation (average time of 11.2 h) of seizures after lacosamide and an additional 7 (54 %) had at least a 50 % reduction in seizures [14]. In our study, the duration of status epilepticus after administration of lacosamide is 31.1 h. This length is prolonged by the 17.6 % of patients who did not respond to lacosamide. When these patients are excluded, the response rate to the addition of lacosamide is 17.4 h. Similar effectiveness was shown by Kellinghaus et al. (2011) in his review of 39 patients, showing a response rate of 44 % with 7 of the 17 responders doing so within 6 h of administration, and by Mnatsakanyan et al. [15] who showed a 70 % responder rate in 10 patients with nonconvulsive status epilepticus [9, 15]. The timing of status epilepticus cessation was not provided in this series. We chose our response time points based on pharmacokinetics of lacosamide. It has a time to peak of 1–4 h, has a half-life of 13 h, and reaches steady state by 3 days [20]. Our study strengthens these findings by showing effectiveness in a larger, critically ill population with a broader range of etiologies, seizure types, and predetermined time points.
Lacosamide is approved as an adjunctive antiepileptic in the treatment of partial onset seizures and secondarily generalized seizures. It is not FDA-approved for treatment of status epilepticus. However, given the intravenous formulation and favorable side effect profile, it is an additional agent that can be used. It is not clear whether it can be used as a first-line antiepileptic after benzodiazepine in treating status epilepticus or if it should be reserved for refractory status epileptics. Previous studies have shown that response rates may be increased if given earlier (first or second line) compared to later (third or fourth line) [9, 13]. Our results did not find a difference in sequence of administration and response. In our study, lacosamide was given predominantly as a third-line antiepileptic. One patient did receive lacosamide initially after benzodiazepine and did not respond until 12 h after administration. Additionally, the duration of status epilepticus prior to administration of lacosamide may affect response rate. On average, lacosamide was given 25.2 h after onset of status epilepticus. This may explain the improved effectiveness rates compared to the results from Rantsch (2011), which showed only 20 % responder rate when given 208.02 h after status epilepticus onset [19]. Conversely, a single case report of status epilepticus secondary to voltage-gated potassium channel antibodies showed a response to lacosamide 10 weeks after seizure onset [21]. It is not clear in this case whether the patient responded to the lacosamide or to the combination of six prior antiepileptics, or if the seizure resolution was secondary to the natural history of the underlying etiology following treatment with high-dose corticosteroids, plasmapheresis, and intravenous immunoglobulin [21].
In addition to effectiveness being determined by timing of lacosamide administration, the dose is also important. In the electrical hippocampal kindling rat model of status epilepticus, a dose of 3 mg/kg/day was shown to be ineffective [22]. Only at doses of 10 mg/kg/day was there evidence of retardation of the kindling-induced epileptogenesis [22]. In the cobalt/homocysteine model of self-sustaining status epilepticus in rats, lacosamide had a dose-dependent decrease in generalized tonic–clonic seizures (ED50: 45.4 mg/kg) [9, 23]. When coadministered with diazepam, there was a marked synergistic effect reducing the ED50 to 3.85 mg/kg [9, 23].
There may be a different dose response curve in humans with status epilepticus. Our patients had an 82.4 % response rate at 48 h after administration with an average loading dose of 2.6 mg/kg. Our sample size, however, is too small to adequately demonstrate a dose response. This highlights the need for further clinical studies evaluating lacosamide in treating status epilepticus.
Lacosamide has a favorable side effect profile with the most common side effects in clinical trials being drowsiness, nausea, headache, visual disturbance, and dizziness [24]. Many of these side effects can be tolerated in the critically ill. In addition to the favorable side effect profile, the low plasma protein binding and low drug–drug interaction of lacosamide make it an ideal antiepileptic for treating status epilepticus. The rarer side effects of PR prolongation (4.4–6.1 ms in the initial clinical trials), hypotension, transaminitis, and perhaps renal failure are of greater concern. Several of these adverse events were noted in our study. Within one day, five patients (9.8 %) had hypotension and another five patients (9.8 %) had transaminitis. No patient had a change in PR interval or developed acute renal failure within 24 h of administration. Our results show better cardiac tolerability than those described by Cherry et al. [14]. They found that 19 % of their patients developed hypotension at 24 h after lacosamide administration. Our study did show similar hepatotoxicity (9.8 % compared to 7.6 %) [14]. None of our patients developed acute renal failure or a documented rash as previously reported [13].
With any retrospective study, the inability to blind and randomize is a major limitation. Also, adverse events are dependent on documentation. Our study was not intended to show superiority of lacosamide over levetiracetam or phenytoin. We only evaluated patients who did not respond initially to phenytoin or levetiracetam and evaluated the effectiveness of lacosamide in these patients. The strength of this study is the sample size and the accuracy of seizure detection and resolution using cEEG. It is the largest study to date showing the effectiveness and tolerability of lacosamide in a critically ill population and comparing it to other antiepileptics. Ultimately, there is a need for a large, prospective study evaluating lacosamide in status epilepticus and comparing the effectiveness to traditional antiepileptics, such as phenytoin.
In conclusion, this is the largest study to date to demonstrate the effectiveness and tolerability of lacosamide in the critically ill population. Lacosamide is an ideal antiepileptic for use in the critically ill. It does not bind to any other binding sites of anticonvulsants or analgesics [9]. It has similar bioavailability orally or parenterally. It also has a novel mechanism of action including modulating the slow inactivation sodium channel [9]. It has minimal adverse effects and protein binding. Maximum plasma concentration is reached within 1–4 h after intake with linear increase in plasma concentration with increasing dose [9]. These properties make it an ideal medication to be used in critically ill patients when compared to older antiepileptics. A large prospective study is needed to further evaluate the effectiveness of lacosamide in this patient population and compare the effectiveness to phenytoin and levetiracetam.
References
Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339:792–8.
Alldredge BK, Gelb AM, Isaacs SM, et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–7.
Lowenstein DH, Alldredge BK. Status epilepticus. N Engl J Med. 1998;338:970–6.
Litt B, Wityk RJ, Hertz SH, et al. Nonconvulsive status epilepticus in the critically ill elderly. Epilepsia. 1998;39:1194–202.
Shorvon SD. The treatment of status epilepticus. Curr Opin Neurol. 2011;48:35–8.
Trinka E. What is the relative value of the standard anticonvulsants: Phenytoin and fosphenytoin, phenobarbital, valproate, and levetiracetam? Epilepsia. 2009;50:40–3.
Meierkord H, Boon P, Englesen B, et al. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol. 2010;17:348–55.
Doty P, Rudd GD, Stoehr T, Thomas D. Lacosamide. Neurotherapeutics. 2007;4:145–8.
Kellinghaus C, Bernig S, Besselmann M. Intravenous lacosamide as successful treatment for nonconvulsive status epilepticus after failure of first-line therapy. Epilepsy Behav. 2009;14:429–31.
Perucca E, Yasothan U, Clincke G, Kirkpatrick P. Lacosamide. Nat Rev Drug Discov. 2008;7:973–4.
Wehner T, Bauer S, Hamer HM, et al. 6 months of postmarketing experience with adjunctive lacosamide in patients with pharmacoresistant epilepsy at a tertiary epilepsy center in Germany. Epilepsy Behav. 2009;16:423–5.
Beyreuther BK, Freitag J, Heers C, et al. Lacosamide: a review of preclinical properties. CNS Drug Rev. 2007;13:21–42.
Hofler J, Unterberger I, Dobesberger J, et al. Intravenous lacosamide in status epilepticus and seizure clusters. Epilepsia. 2011;52:e148–52.
Cherry S, Judd L, Muniz JC, et al. Safety and efficacy of lacosamide in the intensive care unit. Neurocrit Care. 2012;16:294–8.
Mnatsakanyan L, Chung JM, Tsimerinov EI, Eliashiv DS. Intravenous lacosamide in refractory nonconvulsive status epilepticus. Seizure. 2012;21:198–201.
Moreno Morales EY, Fernandez Peleteiro M, Bondy Pena EC, et al. Observational study of intravenous lacosamide in patients with convulsive verses non-convulsive status epilepticus. Clin Drug Investig. 2015;35:463–9.
Cross SA, Curran MP. Lacosamide: in partial-onset seizures. Drugs. 2009;69:449–59.
Maganti R, Gerber P, Drees C, Chung S. Nonconvulsive status epilepticus. Epilepsy Behav. 2008;12:572–86.
Rantsch K, Walter U, Wittstock M, et al. Efficacy of intravenous lacosamide in refractory nonconvulsive status epilepticus and simple partial status epilepticus. Seizure. 2011;20:529–32.
Fernandez EM, Frank AJ. Lacosamide for the treatment of refractory status epilepticus. Ann Pharmacother. 2011;45:1445–9.
Shiloh-Malawsky Y, Fan Z, Greenwood R, Tennison M. Successful treatment of childhood prolonged refractory status epilepticus with lacosamide. Seizure. 2011;20:586–8.
Brandt C, Heile A, Potschka H, et al. Effects of the novel antiepileptic drug lacosamide on the development of amygdala kindling in rats. Epilepsia. 2006;47:1803–9.
Stohr T, Kupferberg HJ, Stables JP, et al. Lacosamide, a novel anti-convulsant drug, shows efficacy with a wide safety margin in rodent models for epilepsy. Epilepsy Res. 2007;74:147–54.
Chung S, Sperling MR, Biton V, et al. Lacosamide as adjunctive therapy for partial-onset seizures: a randomized controlled trial. Epilepsia. 2010;51:958–67.
Authors’ Contribution
Christopher R. Newey, Minh Le, Christine Ahrens, Pradeep Sahota and Stephen Hantus contributed equally to the writing of the case and formatting the images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christopher R. Newey, Minh Le, Christine Ahrens, and Pradeep Sahota have no financial disclosures to report. Stephen Hantus has served as a consultant and on advisory boards for UCB pharma.
Rights and permissions
About this article
Cite this article
Newey, C.R., Le, N.M., Ahrens, C. et al. The Safety and Effectiveness of Intravenous Lacosamide for Refractory Status Epilepticus in the Critically Ill. Neurocrit Care 26, 273–279 (2017). https://doi.org/10.1007/s12028-016-0322-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0322-2