Abstract
Background
Early brain injury (EBI) following aneurysmal subarachnoid hemorrhage (SAH) is an important predictor of poor functional outcome, yet the underlying mechanism is not well understood. Animal studies suggest that platelet activation and inflammation with subsequent microthrombosis and ischemia may be a mechanism of EBI.
Methods
A prospective, hypothesis-driven study of spontaneous, SAH patients and controls was conducted. Platelet activation [thromboelastography maximum amplitude (MA)] and inflammation [C-reactive protein (CRP)] were measured serially over time during the first 72 h following SAH onset. Platelet activation and inflammatory markers were compared between controls and SAH patients with mild [Hunt–Hess (HH) 1–3] versus severe (HH 4–5) EBI. The association of these biomarkers with 3-month functional outcomes was evaluated.
Results
We enrolled 127 patients (106 SAH; 21 controls). Platelet activation and CRP increased incrementally with worse EBI/HH grade, and both increased over 72 h (all P < 0.01). Both were higher in severe versus mild EBI (MA 68.9 vs. 64.8 mm, P = 0.001; CRP 12.5 vs. 1.5 mg/L, P = 0.003) and compared to controls (both P < 0.003). Patients with delayed cerebral ischemia (DCI) had more platelet activation (66.6 vs. 64.9 in those without DCI, P = 0.02) within 72 h of ictus. At 3 months, death or severe disability was more likely with higher levels of platelet activation (mRS4–6 OR 1.18, 95 % CI 1.05–1.32, P = 0.007) and CRP (mRS4–6 OR 1.02, 95 % CI 1.00–1.03, P = 0.041).
Conclusions
Platelet activation and inflammation occur acutely after SAH and are associated with worse EBI, DCI and poor 3-month functional outcomes. These markers may provide insight into the mechanism of EBI following SAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Admission neurological status after subarachnoid hemorrhage (SAH) reflects the severity of early brain injury (EBI) and is a larger predictor of death or severe disability than any other factor or complication that occurs as a consequence of aneurysm rupture [1, 2]. However, the mechanisms for EBI are not well understood; and no effective therapeutic intervention currently exists.
In both animal and human models, SAH leads to transiently elevated intracranial pressure (ICP) with concomitant inadequate cerebral blood flow and perfusion and, in severe cases, intracranial circulatory arrest [3, 4]. This transient global hypoperfusion (often evidenced by loss of consciousness at ictus) initiates a cascade of events that includes diffuse upregulation of endothelial adhesion molecules, platelet activation, and inflammation, which culminates in microthrombosis, ischemia, vasogenic edema, and EBI [5–7]. Platelets amplify the inflammatory cascade [8]. Once activated, platelets display P-selectin and release chemokines/cytokines that promote leukocyte adherence and transmigration at sites of platelet deposition [8]. Neutrophils also release factors that promote platelet activation [9]. Activated platelets and inflammatory cells can contribute to further endothelial disruption, perpetuating the cycle of microthrombosis and inflammation, even distant from the aneurysm rupture site [5, 7, 10, 11]. Indeed, we have shown in pilot data that measures of platelet activation and markers of inflammation (C-reactive protein) were higher in SAH patients with more severe early neurological injury [12].
In this larger prospective, controlled cohort study, we hypothesize that platelet activation and inflammation will be increased in SAH patients compared to controls and associated with clinical evidence of EBI and worse long-term functional outcomes.
Methods
Study Population
A prospective, hypothesis-driven study was conducted of patients with spontaneous SAH between April/2010 and June/2015 at two tertiary care neurointensive care units at Mount Sinai Hospital (MSH) in New York and Cleveland Clinic (CC). Consecutive patients were enrolled at each institution as the PI (Frontera) moved from MSH to CC, with an intervening 6-month startup time at CC. Study inclusion criteria were defined as spontaneous SAH diagnosed by head computed tomography or lumbar puncture, enrollment within 72 h of hemorrhage onset (prior to the onset of delayed cerebral ischemia or vasospasm), initial blood sampling prior to catheter angiography or aneurysm repair, informed consent and age ≥18 years. Exclusion criteria were defined as secondary SAH (from trauma, dissection, amyloid angiopathy, Moya Moya, vasculitis, arteriovenous malformation), clinical or radiographic evidence of ultra-early vasospasm or delayed cerebral ischemia (DCI), use of irreversible platelet inhibitors within 7 days, use of reversible platelet inhibitors within four half-lives of the first blood draw, intrinsic platelet dysfunction, thrombocytopenia (platelet count <100 per µL), platelet transfusion, use of immunosuppressant drugs including steroids, or known immunocompromised state.
A control group consisted of antiplatelet-naïve patients with known unruptured intracranial aneurysms and planned elective, prophylactic aneurysm repair via either clipping or coiling. This group was selected so that we could control for platelet activation and inflammation that may occur with aneurysm formation or following an aneurysm repair procedure. The control group was subjected to the same exclusion criteria as the SAH group. The study was approved by the MSH and CC Institutional Review Boards (IRB). All patients or their surrogates were consented for participation in this study.
Laboratory Studies
Venous blood was sampled serially at three time points: 0–24, 24–48, and 48–72 h of aneurysm rupture, prior to the clinical or radiographic onset of delayed cerebral ischemia (vasospasm), which typically occurs within 3–14 days following aneurysm rupture [1]. In a subgroup of SAH patients, simultaneous jugular and peripheral venous sampling was performed to compare measurements representative of cerebral venous drainage (jugular bulb catheter sampling) to peripheral venous samples (which could be contaminated by systemic inflammation related to critical illness). Control patients underwent venous blood testing before and 24 h after elective aneurysm repair. The initial blood sample in SAH and control patients was collected prior to digital subtraction angiography and/or aneurysm repair to evaluate for platelet activation or inflammation that may be induced as part of the aneurysm repair process.
Platelet activation was measured using thromboelastography (TEG®; Haemoscope Corporation, IL, USA). TEG is an FDA-approved point-of-care device that measures the speed and strength of clot formation. The TEG parameter MA (maximum amplitude) measures platelet and fibrin contribution to clot formation [13]. Elevated TEG MA indicates clot strength and is a marker of platelet activation [13–16] (normal range 51.0–69.0 mm).
Inflammation was assessed by measuring C-reactive protein (CRP) and the percent neutrophils in venous blood collected at 0–24, 24–48, and 48–72 h after aneurysm rupture. Blood samples for all biomarkers of platelet activation and inflammation were collected at the same time.
Clinical and Outcome Measures
The time of aneurysm rupture was recorded as the patient reported time of first headache or the time last known at baseline, if the headache onset time was unknown. EBI was assessed at admission using the Hunt–Hess grade [17, 18]. Admission neurological severity was dichotomized as severe EBI (Hunt–Hess 4–5) versus mild EBI (Hunt–Hess 1–3). To corroborate our findings, other admission measures of neurological injury were also assessed including the Glasgow Coma Scale (GCS) [19] and the National Institutes of Health Stroke Scale (NIHSS) [20]. All neurological batteries were performed after resuscitation (including external ventricular drain placement) to eliminate confounding factors that may adversely affect the neurological exam. Delayed cerebral ischemia was defined as clinical neurological deterioration accompanied by radiographic/angiographic evidence of reversible vessel narrowing or infarction detectable by CT or MRI due to vasospasm [1].
Functional outcomes were assessed at 3 months via phone interview using the modified Rankin Scale (mRS) dichotomized as 0–3 (good functional outcome) versus 4–6 (poor outcome) [21, 22].
Statistical Analysis
The sample size for this study was calculated to detect a difference in platelet activation (TEG MA values) between patients with mild (Hunt–Hess 1–3) and severe (Hunt–Hess 4–5) EBI. Preliminary data showed that mild and severe Hunt–Hess grade patients were admitted in a ratio of 4:1. Based on pilot data showing a mean MA of 65.4 mm and a standard deviation of 5.0 mm, a sample size of 110 patients (88 mild and 22 severe) would be required to detect a 4-mm difference in MA with 80 % power and 0.05 significance level. A priori, a minimum of 20 patients were selected for the control group. This number of controls was selected due to the confines of our budget. Additionally, our study was not designed to test SAH versus controls but rather to distinguish mild from severe EBI early after SAH. Hence, our power calculation did not account for control subjects.
Demographic and repair procedure variables were compared between the SAH and control group using chi-square analysis for categorical variables and Mann–Whitney U tests for continuous variables. The median platelet activation and inflammatory biomarker values (over the first 72 h from ictus in SAH patients and pre-aneurysm repair in controls) were compared in the following groups: (1) across three groups: controls, mild EBI SAH (Hunt–Hess 1–3), and severe EBI (Hunt–Hess 4–5) SAH patients; (2) all SAH patients versus controls; (3) severe EBI SAH patients versus controls; and (4) severe versus mild EBI SAH patients using the Mann–Whitney U and Kruskal–Wallis tests. The median platelet activation, CRP, and percent neutrophils were compared over each individual level of the Hunt–Hess scale using ordinal logistic regression. Additionally, a Jonckheere–Terpstra test for trend was used to assess the “dose–response” relationship between platelet activation, CRP, and percent neutrophils values and each level of the Hunt–Hess grade. Backwards, stepwise logistic regression analysis was used to evaluate the association of platelet activation, CRP, and percent neutrophils with EBI after adjusting for covariates. Repeated measures analyses (two-way repeated measures analysis of variance [ANOVA] using one-factor repetition) were used to assess the changes in platelet activation, CRP, and percent neutrophils over time. The correlations among jugular and peripheral venous measures of platelet activation, CRP, and percent neutrophils were assessed using Spearman’s correlation coefficient. Logistic regression was used to assess the association between platelet activation, CRP, percent neutrophils, and 3-month dichotomized mRS. All analyses were performed using commercially available SPSS (v. 21, Chicago IL, USA) and SAS (v 9.3, Cary, NC, USA) statistical software. Significance was set at P < 0.05.
Results
A total of 306 patients with SAH were screened for enrollment: 57 were excluded for prior antiplatelet or immunosuppressant use, 8 were excluded after receiving a platelet transfusion at admission, 71 had nonaneurysmal causes of SAH (most commonly trauma), 41 were admitted outside of the time window (over 72 h from ictus), 12 refused consent, and 11 were not enrolled for other reasons. A total of 106 SAH patients (26 from MSH and 80 from CC) and 21 controls (all from CC) met inclusion criteria and were enrolled. Among SAH patients, 24 (23 %) had severe EBI (Hunt–Hess 4–5) and 82 (77 %) had mild EBI (Hunt–Hess 1–3). All 127 subjects underwent platelet activity testing TEG, and an additional 77 (59 SAH and 18 control) had CRP and percent neutrophils testing, which was initiated after the pilot phase of the study. The SAH and control groups were similar in age, although there was a higher proportion of women; and aneurysm clipping was more common in the control group (Table 1).
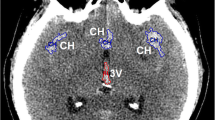
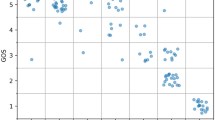
SAH patients with severe EBI (Hunt–Hess grade 4–5) had significantly higher levels of platelet activation and CRP (averaged over 72 h from ictus) compared to those patients and controls with mild EBI (Hunt–Hess 1–3) (Table 2). Similarly, platelet activation and markers of inflammation including CRP and the percent neutrophils increased across each individual level of the Hunt–Hess scale (Fig. 1). A “dose–response” effect was demonstrated such that each level increase in the Hunt-Hess scale was associated with incrementally higher platelet activation (Jonckheere–Terpstra Z statistic 4.0, P < 0.001) and CRP (Jonckheere–Terpstra Z statistic 3.4, P = 0.001). To corroborate these findings, we also examined associations with other clinical neurological scales and found worse median admission GCS Scores and NIHSS scores in patients with higher (greater than median) levels of platelet activation (GCS 13 with higher platelet activation versus 15 in lower platelet activation, P = 0.004; and NIHSS 7 versus 0, P = 0.001). Similarly, patients with elevated CRP had worse median admission GCS scores (10 versus 15, P = 0.002) and NIHSS scores (9 versus 0, P = 0.001). Over the first 72 h from ictus, platelet activation was significantly correlated with markers of inflammation including CRP (Spearman’s correlation coefficient R = 0.599, P < 0.001) and percent neutrophils (Spearman’s correlation coefficient R = 0.311, P = 0.036). The percentage of lymphocytes and percentage of monocytes were not significantly different among SAH patients with mild or severe EBI or compared to controls. Additionally, there was no evidence of disseminated intravascular coagulopathy (DIC) or platelet dysfunction among any of the SAH patients (based on TEG LY30 and MA values).
Platelet activation (thromboelastography [TEG] MA values) and markers of inflammation (C-reactive protein and percent neutrophils) in controls and across each level of the Hunt–Hess scale. Levels represent averages over the first 72 h from SAH ictus. P values were derived from ordinal logistic regression analysis. Whisker bars represent the standard error of the mean. MA maximum amplitude; CRP C-reactive protein
We evaluated possible confounding conditions that might cause platelet activation or inflammation including the occurrence of meningitis/ventriculitis, pneumonia, urinary tract infection, blood stream infection, seizure, myocardial infarction, neurogenic stunned myocardium, pulmonary edema, and intubation. Only intubation was associated with elevated platelet activation (67 versus 65 mm in those not intubated, P = 0.013). Pneumonia was associated with elevated CRP (6.6 versus 1.4 mg/L in those without pneumonia, P = 0.009) and percent neutrophils (85 vs. 80 %, P = 0.003). Pulmonary edema was also associated with elevated CRP (4.8 vs. 1.1 mg/L in those without pulmonary edema, P = 0.027) and percent neutrophils (84 vs. 80 %, P = 0.046), as was intubation (CRP 6.4 vs. 0.5 mg/L in those not intubated and percent neutrophils 84 vs. 79 %, P = 0.016). None of the other conditions were significantly associated with platelet activation, CRP, or percent neutrophils. Using backward stepwise logistic regression analysis adjusting for intubation, platelet activation was still significantly associated with EBI (adjusted OR 1.13, 95 % confidence interval [CI], CI, 1.0–1.3, P = 0.049).
Patients with increased platelet activation within 72 h of ictus had a higher likelihood of developing DCI later during their hospitalization than those with less early platelet activation (median MA 66.6 mm in those who developed DCI versus > 64.9 mm in those who did not; (odds ratio [OR] for developing DCI with increasing platelet activation: 1.1, 95 % CI 1.0–1.2, P = 0.02). Early elevations in CRP and percent neutrophils over the first 72 h from ictus were not associated with DCI. There was no association of age, gender, or the type of aneurysm repair procedure (clipping or coiling) with platelet activation, CRP, or percent neutrophils.
Over the first 72 h following aneurysm rupture, both platelet activation and CRP increased over time (P < 0.0001 and P = 0.001, respectively; Fig. 2), but the percent neutrophils had a nonsignificant trend toward decreasing over time (P = 0.07).
The effects of the aneurysm repair procedure on platelet activation and inflammation were evaluated (Fig. 3). There was no change in platelet activation in the control group after aneurysm repair (median pre-repair MA 64.9 mm and post-repair 64.9, P = 0.87), and there was a small increase in the SAH group (median pre-repair MA 64.9–65.3 mm post-repair, P = 0.047), though this may not be clinically significant. Both CRP and percent neutrophils increased modestly from pre- to post-aneurysm repair in controls (median pre-repair CRP 0.3 mg/L to 1.5, P < 0.001; median pre-repair percent neutrophils 63–83.5 % post-repair, P = 0.002), and CRP increased in SAH patients (median pre-repair CRP 0.5 mg/L to 2.8 mg/L post-repair, P = 0.003) though percent neutrophils did not (median pre-repair percent neutrophils 84–81.6 % post-repair, P = 0.892). However, post-aneurysm repair platelet activation and CRP were still significantly higher in poor-grade SAH patients compared to controls (median post-repair MA 69.2 mm in Hunt–Hess 4–5 SAH vs. 64.9 mm in controls, P = 0.007; median post-repair CRP 17.6 mg/L in Hunt–Hess 4–5 SAH vs. 1.5 mg/L in controls, P < 0.0001).
In a secondary analysis, jugular and peripheral venous levels of platelet activation and inflammation were compared. This subanalysis was done to determine whether there were substantial differences between jugular venous blood (which represents almost exclusively cerebral venous drainage) and peripheral venous sampling (which could be contaminated by systemic inflammation related to critical illness). A total of 40 patients underwent simultaneous jugular and peripheral venous sampling every 24 h for 3 days following aneurysm rupture. During the first 72 h from ictus, jugular and venous MA, CRP, and percent neutrophils were very similar, though jugular levels were slightly higher (Supplementary Figure 1). There was a significant correlation between jugular and venous platelet activation, CRP, and percent neutrophils (Spearman’s correlation coefficient R = 0.92, 0.99 and 0.90, respectively; all P < 0.0001). Similar increases in jugular and peripheral venous MA and CRP levels occurred over time (Supplementary Figure 1).
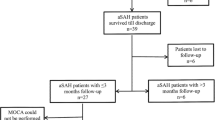
Three-month follow-up data were available in 92/106 (87 %) of SAH patients. Early platelet activation was significantly associated with increased 3-month mortality (OR for mortality with increasing platelet activation: 1.18, 95 % CI, 1.04–1.34, P = 0.011) and worse 3-month functional outcomes (OR for mRS 4–6 with increasing platelet activation: 1.18, 95 % CI, 1.05–1.32, P = 0.007; Table 3). Three-month death or severe disability was also associated with higher markers of inflammation (OR for mRS 4–6 with increasing CRP: 1.02, 95 % CI, 1.00–1.03, P = 0.041).
Discussion
This study is one of the first, and largest, prospective clinical studies to test the hypothesis that acute elevations in platelet activation and inflammation are associated with EBI following spontaneous SAH. We found that SAH patients with clinical evidence of severe brain injury (measured by the Hunt–Hess grade and corroborated by the NIHSS and GCS scales) had significant elevations in platelet activation and inflammation compared to less severely affected SAH patients (Hunt–Hess 1–3) and controls within 72 h of ictus. Furthermore, there was a “dose–response” effect with incrementally increasing platelet activation and inflammation as Hunt–Hess grade and EBI worsened. Even after controlling for other factors, platelet activation was independently associated with EBI. These biomarkers were not only associated with EBI following SAH but also with worse 3-month functional outcomes.
Our clinical data corroborate a mechanism for EBI in SAH elucidated in animal studies. In a rat endovascular perforation model of SAH [23], platelet aggregates have been observed to occur in microvessels within 10 min of SAH and continue to increase over the first 48 h from vessel rupture [5, 24]. Platelet aggregates may cause microthrombosis, ischemia, and resultant tissue death. Indeed, endothelial and parenchymal apoptosis and neuronal necrosis occur in animals within 10 min of SAH and continue to increase over 24 h from ictus, concomitant with platelet aggregation within microvessels [25]. In humans, we and others have demonstrated that MRI-detected infarctions occur acutely after SAH (and prior to the onset of DCI) [26]. These infarctions occur more commonly in patients with more severe EBI (Hunt–Hess 4–5) and are associated with an increased risk of DCI and worse 3-month functional outcomes [26–28]. Such infarctions may be the result of small vessel microthromboses, particularly since 75 % were observed to be punctate, occurring at the small vessel level [26]. An autopsy study of seven patients who died within 3 days after SAH found a high microclot burden associated with pathological evidence of ischemia, indicating that microthromboses occur acutely and may be a mechanism of EBI after SAH [29].
Platelet activation occurs concomitantly with inflammation. This was demonstrated in our study by simultaneous elevations in CRP, percent neutrophils, and platelet activation in SAH patients compared to controls, and significant correlation coefficients. In animal models, intraluminal platelets initiate or stimulate endothelium and basal lamina disruption, as evidenced by acute loss of collagen IV [30] and increased vessel permeability [10]. Resultant blood brain barrier breakdown and inflammation are evidenced by escape of platelet aggregates and neutrophils into the brain parenchyma [6, 11]. Several other clinical studies have identified an increase in immunologic and inflammatory markers in patients with both unruptured intracranial aneurysms and SAH [31, 32]. We found that platelet activation and CRP increased over the first 72 h from ictus. Though percent neutrophils were initially elevated in SAH patients compared to controls, this biomarker tended to decline over time. This may be due to diapedesis of neutrophils into the brain parenchyma as suggested by animal models, though further study is required to support this hypothesis. It is possible that platelet activation and inflammation may continue to rise during the DCI/vasospasm risk period. Future studies are needed to test this hypothesis.
While inflammation and platelet activation have been reported in association with DCI [33], our study is one of the first to examine an association with EBI. For decades, clinical research in SAH has focused on preventing and treating secondary injury after SAH (i.e., DCI/vasospasm), while EBI has been understudied [34]. Multiple groups have found an association of elevated platelet-activating factor (PAF), platelet aggregation, platelet microparticles (CD41+), elevated thromboxane levels, and microthrombosis with the development of DCI [33, 35]. Autopsy reports have also found diffuse microthromboses in patients who died from cerebral vasospasm following SAH [29, 36, 37]. In fact, the cascade of injury that begins at the time of aneurysm rupture and causes EBI may be in continuum with the pathophysiological events that lead to DCI. Our study identified a significant association of elevated platelet activation and CRP within the first 72 h of ictus with the development of DCI.
To validate the importance of early platelet activation and inflammation, we were able to demonstrate a significant association with poor 3-month functional outcomes, though the association of CRP with 3-month outcomes is small and may not be clinically significant. In smaller cohort studies, others have found that early elevations in biomarkers of inflammation (TNFα, serum neutrophils) and platelet activation (CD41+ platelet microparticles) have been associated with poor outcomes following SAH [38–40].
Additional strengths of this study include the utilization of control patients and the correlation of peripheral and jugular blood biomarkers. First, the control group allowed us to calibrate the effects of aneurysm repair on platelet activation and inflammation and also to adjust for any inflammatory process that may occur as part of aneurysm development [31]. We found modest elevations in platelet activation and CRP after aneurysm repair, but levels were still significantly lower in controls compared to SAH patients with evidence of severe EBI. Second, we were able to verify that peripheral blood sampling was highly correlated with jugular blood measurements, which are directly representative of the cerebral milieu. Because the jugular levels of platelet activation and inflammation were slightly higher than the peripheral levels, and because the primary cause of critical illness is brain injury due to SAH, we believe that the peripheral platelet activation and inflammation levels directly reflect cerebral processes.
Implications of this study are that early platelet inhibition may have a protective effect in SAH patients. Platelet inhibition has been found to attenuate platelet activation and platelet leukocyte aggregates formation in animal models of SAH [41]. However, human studies of SAH have shown mixed results with antiplatelet use. A randomized study of aspirin to prevent delayed cerebral ischemia did not show benefit, though aspirin was started late (median of 4 days from ictus), and the study was underpowered to examine functional outcomes [42]. In a study of 226 SAH patients undergoing endovascular coiling, antiplatelet drugs (either aspirin or abciximab in varying doses) did not show any difference in outcome at 2 months or 1 year compared to coiled patients who did not receive an antiplatelet [43]. A limitation of the study was that only 56 patients received antiplatelets during coiling while the rest were prescribed antiplatelets at varying times after coiling. Therefore, the time to dosing of antiplatelets may not have been within a meaningful time window to prevent acute brain injury. Another study noted that baseline aspirin use in patients with known aneurysms was associated with lower rates of aneurysm rupture [44]. Though there was no difference in admission clinical status or outcome of those on aspirin compared to aspirin-naïve patients, all patients on aspirin received a platelet transfusion at admission, which may have attenuated any positive aspirin effects. A meta-analysis of five trials and 699 patients found a trend toward improved outcomes in patients who received antiplatelet agents, though the time to initiation of an antiplatelet ranged from within 48 h (only 13 patients) to 9 days from ictus [45]. Given the limitations in the current literature, further exploration of the early effects of aspirin on the proposed mechanism of acute brain injury after SAH may be useful.
Certain limitations of this study bear mentioning. First, we can only demonstrate an association of platelet activation and inflammation with EBI and worse long-term outcomes; we cannot prove causality. However, we did observe an incremental “dose–response” increase in platelet activation and inflammation as the Hunt–Hess grade and EBI severity increased, which may suggest more than just an association. Second, activated platelets and inflammatory cells may be primarily adherent to the endothelium of small vessels and not shed in the blood. We assume that elevated circulating activated platelets and markers of inflammation correlate with elevated levels of platelets and leukocytes adherent to brain microvessel endothelium. Since our data show a strong correlation between peripheral and jugular venous blood measurements (with jugular levels being slightly higher), it is reasonable to assume that the biomarkers we examined represent the cerebral milieu. Third, this study was not powered to assess the effect of early platelet activation and inflammation on long-term functional outcomes after adjusting for other covariates. Hence, we did not perform a multivariable analysis examining the predictive effect of platelet activation and inflammation on 3-month mRS. Finally, because only 60 % of our patients underwent CRP and percent neutrophils testing, this limited our power to detect the impact of inflammation on 3-month outcomes. Furthermore, CRP and percent neutrophils are relatively nonspecific markers of inflammation. Future studies evaluating cytokine/chemokine inflammatory markers may provide more insight into the mechanisms of EBI.
Conclusions
Increased markers of platelet activation and inflammation occur acutely after SAH and are associated with clinical evidence of EBI, DCI, and worse 3-month functional outcomes on univariate analysis. Further research exploring the mechanistic role that these biomarkers may play in EBI after SAH is warranted.
References
Frontera JA, Fernandez A, Schmidt JM, et al. Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke. 2009;40:1963–8.
Wartenberg KE, Schmidt JM, Claassen J, et al. Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med. 2006;34:617–23 (quiz 24).
Grote E, Hassler W. The critical first minutes after subarachnoid hemorrhage. Neurosurgery. 1988;22:654–61.
Sehba FA, Bederson JB. Mechanisms of acute brain injury after subarachnoid hemorrhage. Neurol Res. 2006;28:381–98.
Sehba FA, Mostafa G, Friedrich V Jr, Bederson JB. Acute microvascular platelet aggregation after subarachnoid hemorrhage. J Neurosurg. 2005;102:1094–100.
Friedrich V, Flores R, Muller A, Bi W, Peerschke EI, Sehba FA. Reduction of neutrophil activity decreases early microvascular injury after subarachnoid haemorrhage. J Neuroinflamm. 2011;8:103.
Sehba FA, Friedrich V. Early micro vascular changes after subarachnoid hemorrhage. Acta Neurochir Suppl. 2011;110:49–55.
Smyth SS, McEver RP, Weyrich AS, et al. Platelet functions beyond hemostasis. J Thromb Haemost. 2009;7:1759–66.
Renesto P, Chignard M. Tumor necrosis factor-alpha enhances platelet activation via cathepsin G released from neutrophils. J Immunol. 1991;146:2305–9.
Friedrich V, Flores R, Muller A, Sehba FA. Luminal platelet aggregates in functional deficits in parenchymal vessels after subarachnoid hemorrhage. Brain Res. 2010;1354:179–87.
Friedrich V, Flores R, Muller A, Sehba FA. Escape of intraluminal platelets into brain parenchyma after subarachnoid hemorrhage. Neuroscience. 2010;165:968–75.
Frontera JA, Aledort L, Gordon E, et al. Early platelet activation, inflammation and acute brain injury after a subarachnoid hemorrhage: a pilot study. J Thromb Haemost. 2012;10:711–3.
Craft RM, Chavez JJ, Bresee SJ, Wortham DC, Cohen E, Carroll RC. A novel modification of the thrombelastograph assay, isolating platelet function, correlates with optical platelet aggregation. J Lab Clin Med. 2004;143:301–9.
Swallow RA, Agarwala RA, Dawkins KD, Curzen NP. Thromboelastography: potential bedside tool to assess the effects of antiplatelet therapy? Platelets. 2006;17:385–92.
Sambu N, Hobson A, Curzen N. “Short” thrombelastography as a test of platelet reactivity in response to antiplatelet therapy: validation and reproducibility. Platelets. 2011;22:210–6.
Khurana S, Mattson JC, Westley S, O’Neill WW, Timmis GC, Safian RD. Monitoring platelet glycoprotein IIb/IIIa-fibrin interaction with tissue factor-activated thromboelastography. J Lab Clin Med. 1997;130:401–11.
Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968;28:14–20.
Oshiro EM, Walter KA, Piantadosi S, Witham TF, Tamargo RJ. A new subarachnoid hemorrhage grading system based on the Glasgow Coma Scale: a comparison with the Hunt and Hess and World Federation of Neurological Surgeons Scales in a clinical series. Neurosurgery. 1997;41:140–7 (discussion 7–8).
Teasdale G, Jennett B. Assessment and prognosis of coma after head injury. Acta Neurochir (Wien). 1976;34:45–55.
Brott T, Adams HP Jr, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–70.
Rankin J. Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 1957;2:200–15.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Sehba FA. Rat endovascular perforation model. Transl Stroke Res. 2014;5:660–8.
Pisapia JM, Xu X, Kelly J, et al. Microthrombosis after experimental subarachnoid hemorrhage: time course and effect of red blood cell-bound thrombin-activated pro-urokinase and clazosentan. Exp Neurol. 2012;233:357–63.
Friedrich V, Flores R, Sehba FA. Cell death starts early after subarachnoid hemorrhage. Neurosci Lett. 2012;512:6–11.
Frontera JA, Ahmed W, Zach V, et al. Acute ischaemia after subarachnoid haemorrhage, relationship with early brain injury and impact on outcome: a prospective quantitative MRI study. J Neurol Neurosurg Psychiatry. 2015;86:71–8.
Hadeishi H, Suzuki A, Yasui N, Hatazawa J, Shimosegawa E. Diffusion-weighted magnetic resonance imaging in patients with subarachnoid hemorrhage. Neurosurgery. 2002;50:741–7 (discussion 7–8).
Sato K, Shimizu H, Fujimura M, Inoue T, Matsumoto Y, Tominaga T. Acute-stage diffusion-weighted magnetic resonance imaging for predicting outcome of poor-grade aneurysmal subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2010;30:1110–20.
Stein SC, Browne KD, Chen XH, Smith DH, Graham DI. Thromboembolism and delayed cerebral ischemia after subarachnoid hemorrhage: an autopsy study. Neurosurgery. 2006;59:781–7 (discussion 7–8).
Sehba FA, Mostafa G, Knopman J, Friedrich V Jr, Bederson JB. Acute alterations in microvascular basal lamina after subarachnoid hemorrhage. J Neurosurg. 2004;101:633–40.
Hussain S, Barbarite E, Chaudhry NS, et al. Search for biomarkers of intracranial aneurysms: a systematic review. World Neurosurg. 2015;84:1473–83.
Chen S, Feng H, Sherchan P, et al. Controversies and evolving new mechanisms in subarachnoid hemorrhage. Prog Neurobiol. 2014;115:64–91.
Boluijt J, Meijers JC, Rinkel GJ, Vergouwen MD. Hemostasis and fibrinolysis in delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage: a systematic review. J Cereb Blood Flow Metab. 2015;35:724–33.
Frontera JA. Clinical trials in cardiac arrest and subarachnoid hemorrhage: lessons from the past and ideas for the future. Stroke Res Treat. 2013;2013:263974.
Vergouwen MD, Bakhtiari K, van Geloven N, Vermeulen M, Roos YB, Meijers JC. Reduced ADAMTS13 activity in delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2009;29:1734–41.
Suzuki S, Suzuki M, Iwabuchi T, Kamata Y. Role of multiple cerebral microthrombosis in symptomatic cerebral vasospasm: with a case report. Neurosurgery. 1983;13:199–203.
Suzuki S, Kimura M, Souma M, Ohkima H, Shimizu T, Iwabuchi T. Cerebral microthrombosis in symptomatic cerebral vasospasm—a quantitative histological study in autopsy cases. Neurol Med Chir. 1990;30:309–16.
Chou SH, Feske SK, Atherton J, et al. Early elevation of serum tumor necrosis factor-alpha is associated with poor outcome in subarachnoid hemorrhage. J Invest Med. 2012;60:1054–8.
Lackner P, Dietmann A, Beer R, et al. Cellular microparticles as a marker for cerebral vasospasm in spontaneous subarachnoid hemorrhage. Stroke. 2010;41:2353–7.
Chou SH, Feske SK, Simmons SL, et al. Elevated peripheral neutrophils and matrix metalloproteinase 9 as biomarkers of functional outcome following subarachnoid hemorrhage. Transl Stroke Res. 2011;2:600–7.
Ishikawa M, Kusaka G, Yamaguchi N, et al. Platelet and leukocyte adhesion in the microvasculature at the cerebral surface immediately after subarachnoid hemorrhage. Neurosurgery. 2009;64:546–53 (discussion 53–54).
van den Bergh WM, MASH Study Group, Algra A, et al. Randomized controlled trial of acetylsalicylic acid in aneurysmal subarachnoid hemorrhage: the MASH Study. Stroke. 2006;37:2326–30.
van den Bergh WM, Kerr RS, Algra A, Rinkel GJ, Molyneux AJ, International Subarachnoid Aneurysm Trial Collaborative Group. Effect of antiplatelet therapy for endovascular coiling in aneurysmal subarachnoid hemorrhage. Stroke. 2009;40:1969–72.
Gross BA, Rosalind Lai PM, Frerichs KU, Du R. Aspirin and aneurysmal subarachnoid hemorrhage. World Neurosurg. 2014;82:1127–30.
Dorhout Mees SM, Rinkel GJ, Hop JW, Algra A, van Gijn J. Antiplatelet therapy in aneurysmal subarachnoid hemorrhage: a systematic review. Stroke. 2003;34:2285–9.
Acknowledgments
Dr. Frontera received funding for this project from the American Heart Association (11CRP5270003) and the Research Program Committee of the Cleveland Clinic (RPC # 2013-1014).
Author contributions
J.A. Frontera was responsible for study design, collecting, analyzing and interpreting data, writing the manuscript, and final approval of the version to be published. J.J. Provencio was responsible for interpreting the data, revising the intellectual content, and final approval of the version to be published. F.A. Sehba was responsible for study design, analyzing and interpreting data, revising the intellectual content and final approval of the version to be published. T.M. McIntyre was responsible for revising the intellectual content, and final approval of the version to be published. A.S. Nowacki was responsible for analyzing and interpreting data and final approval of the version to be published. E. Gordon was responsible for collecting data and final approval of the version to be published. J.M. Weimer was responsible for collecting data and final approval of the version to be published. L. Aledort was responsible for study design, analyzing and interpreting data, revising the intellectual content, and final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary materials.
12028_2016_292_MOESM1_ESM.tif
Supplementary Figure 1. Platelet activation, C-reactive protein (CRP) in jugular and peripheral venous blood over the first 72 hours following aneurysm rupture. Whisker bars represent the standard error of the mean. MA = maximum amplitude, SAH = subarachnoid hemorrhage (TIF 71 kb)
Rights and permissions
About this article
Cite this article
Frontera, J.A., Provencio, J.J., Sehba, F.A. et al. The Role of Platelet Activation and Inflammation in Early Brain Injury Following Subarachnoid Hemorrhage. Neurocrit Care 26, 48–57 (2017). https://doi.org/10.1007/s12028-016-0292-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0292-4