Abstract
Background
The frequency and associations of spontaneous hyperventilation in subarachnoid hemorrhage (SAH) are unknown. Because hyperventilation decreases cerebral blood flow, it may exacerbate delayed cerebral ischemia (DCI) and worsen neurological outcome.
Methods
This is a retrospective analysis of data from a prospectively collected cohort of SAH patients at an academic medical center. Spontaneous hyperventilation was defined by PaCO2 <35 mmHg and pH >7.45 and subdivided into moderate and severe groups. Clinical and demographic characteristics of patients with and without spontaneous hyperventilation were compared using χ 2 or t tests. Bivariate and multivariable logistic regression analyses were conducted to examine the association of moderate and severe hyperventilation with DCI and discharge neurological outcome.
Results
Of 207 patients, 113 (55 %) had spontaneous hyperventilation. Spontaneously hyperventilating patients had greater illness severity as measured by the Hunt–Hess, World Federation of Neurosurgical Societies (WFNS), and SAH sum scores. They were also more likely to develop the following complications: pneumonia, neurogenic myocardial injury, systemic inflammatory response syndrome (SIRS), radiographic vasospasm, DCI, and poor neurological outcome. In a multivariable logistic regression model including age, gender, WFNS, SAH sum score, pneumonia, neurogenic myocardial injury, etiology, and SIRS, only moderate [odds ratio (OR) 2.49, 95 % confidence interval (CI) 1.10–5.62] and severe (OR 3.12, 95 % CI 1.30–7.49) spontaneous hyperventilation were associated with DCI. Severe spontaneous hyperventilation (OR 4.52, 95 % CI 1.37–14.89) was also significantly associated with poor discharge outcome in multivariable logistic regression analysis.
Conclusion
Spontaneous hyperventilation is common in SAH and is associated with DCI and poor neurological outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Induced hyperventilation is an established, albeit controversial, method for treating acute elevations of intracranial pressure (ICP). While the use of prophylactic-induced hyperventilation is considered an appropriate short-term strategy to treat acute ICP elevations, it has also been associated with worse neurological outcome and greater risk of death when used in patients with traumatic brain injury (TBI) [1, 2]. Much less is known about the frequency and clinical impact of spontaneous hyperventilation. A small number of prior observational studies found that hyperventilation can occur in response to severe brain injury and may be associated with worse neurological outcomes [3–7]. However, these studies did not attempt to control for confounding factors, such as illness severity and the presence of pneumonia, and did not focus on patients with subarachnoid hemorrhage (SAH).
Hyperventilation induces cerebral vasoconstriction with a corresponding decrease in cerebral blood flow (CBF) of approximately 2 % for every 1 mmHg (0.13 kPa) decrease in CO2 [8]. As a result, ICP is lowered but decreased CBF may also lead to cerebral ischemia [9–11]. Because of the substantial risk of delayed cerebral ischemia (DCI), this physiological effect has particular relevance in SAH [12, 13]. To our knowledge, no prior studies have examined the incidence and impact of spontaneous hyperventilation in patients with SAH. Therefore, this study was conducted to determine the frequency of spontaneous hyperventilation in SAH and investigate its association with DCI and neurological outcome. We hypothesized that spontaneous hyperventilation is associated with greater illness severity, DCI, and poor neurological outcome at the time of hospital discharge.
Methods
Study Design
We conducted a retrospective analysis of data from a prospectively collected cohort of patients with SAH. Data were collected by the investigators and extracted from the electronic medical record. Approval for this study was provided by the University of Michigan Institutional Review Board.
Patient Population
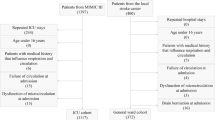
All patients with spontaneous SAH admitted to the University of Michigan Neurological Intensive Care Unit (NICU) between January 2010 and March 2014 were identified from a patient registry. The registry was created by active surveillance of all patients admitted to the NICU. SAH was diagnosed by computed tomography (CT) scan and/or the presence of xanthochromia on lumbar puncture. Exclusion criteria included etiology from trauma or arteriovenous malformation and age <18 years.
Clinical Management
All patients were treated in accordance with current guidelines from the Neurocritical Care Society and American Heart Association [14, 15]. Care was provided by a multidisciplinary team of neurosurgeons and neurointensivists in a dedicated neurological ICU, typically for 14 days. Twenty-four hour access to CT angiography, CT perfusion, and digital subtraction angiography (DSA) was available. All stable patients underwent emergent angiography and, if identified, aneurysms were secured within 24 h by surgical clipping or endovascular coiling. Any signs of hydrocephalus were treated by placement of an external ventricular drain. All patients were treated with nimodipine 60 mg every 4 h unless it was not tolerated due to hypotension despite adjustments in dose and frequency. Transcranial Doppler ultrasounds were performed on all patients for 14 days following the initial hemorrhage. Intravenous fluids were administered to maintain euvolemia. Fever was treated aggressively with antipyretics and surface cooling devices. Daily spontaneous breathing trials were performed on all ventilated patients with fraction of inspired oxygen (FiO2) ≤50 % and positive end expiratory pressure (PEEP) <10. The minimum amount of sedation necessary to prevent ventilator dyssynchrony and patient discomfort was provided. DCI, when present, was treated with additional intravenous fluids and hemodynamic augmentation with vasopressors. If not responsive to initial medical management or if deficits were deemed sufficiently severe, patients underwent emergent angiography and were treated with the intraarterial administration of nicardipine or balloon angioplasty at the discretion of the treating interventionalist.
Clinical Data
Arterial blood gas (ABG) results were reviewed for all subjects. Study subjects had to have at least one ABG that was obtained while not mechanically ventilated, or if mechanically ventilated, the patient had to be breathing above the set respiratory rate or on a pressure support (PS) mode. This was done to exclude instances of iatrogenic hyperventilation. Spontaneous hyperventilation was defined by the presence of at least one ABG with both PaCO2 <35 mmHg (4.67 kPa) and pH >7.45. Patients were further defined as having severe hyperventilation if they had both PaCO2 ≤30 mmHg (4.00 kPa) and pH ≥7.50. Patients with hyperventilation not meeting the requirement for severe hyperventilation were considered to have moderate hyperventilation.
Demographic data (age, sex) as well as social and medical history [tobacco use, alcohol abuse, diabetes, hypertension, coronary artery disease (CAD)] were obtained by interview with the patient and/or family on admission. The World Federation of Neurosurgical Societies (WFNS) and Hunt–Hess (HH) scores, both measures of clinical severity ranging from 1 to 5 with 5 indicating the most severe neurological deficits, were determined by initial clinical examination [16, 17]. Two measures of radiographic severity, the modified Fisher scale (0–4; 0 = no visible hemorrhage, 4 = thick SAH with intraventricular hemorrhage) and Hjidra’s SAH sum score (0–42; 0 = no visible hemorrhage, 42 = complete filling of 10 cisterns and fissures and all 4 ventricles) were calculated by the investigators based on the admission head CT [18, 19].
Patient complications including pneumonia, neurogenic myocardial injury, systemic inflammatory response syndrome (SIRS), radiographic vasospasm, DCI, and discharge neurological outcome were adjudicated by the investigators. Pneumonia was defined by the decision of the treating physician to complete a full course of antibiotic treatment based on chest X-ray, culture results, and clinical symptoms. Neurogenic myocardial injury was defined by abnormal elevation of troponin and/or the presence of newly impaired ejection fraction (EF <40 %) on echocardiogram [20]. SIRS was identified by the presence of at least 2 of 4 criteria: (1) temperature >38 or <36 °C; (2) pulse >90 beats/min; (3) respiratory rate >20 breaths/min; (4) WBC count >12,000 cells/mm3 or <4000 cells/mm3 [21].
Radiographic vasospasm was defined as the presence of vascular luminal narrowing on angiographic images as determined by the interpreting neuroradiologist. DCI was defined using previously published criteria as either (1) the development of new focal neurological signs or decline in the level of consciousness thought to be due to the presence of ischemia after other etiologies (hydrocephalus, toxic-metabolic abnormality, seizure) had been excluded or (2) the presence of new infarcts on CT or MRI [22]. Outcome at hospital discharge was determined by study staff via direct interview and review of therapy service notes using the modified Rankin scale (mRs) [23]. The mRs ranges from 0 to 6, with 0 representing no neurological deficits and 6 equaling death. A poor discharge outcome was considered to be mRs >3, indicating severe disability or death. Demographic and clinical data were prospectively entered into a database using research electronic data capture (REDCap) tools hosted at the University of Michigan [24].
Statistical Analysis
To compare differences in baseline demographic and clinical characteristics between the groups of patients with and without spontaneous hyperventilation, we used χ 2 test or t test, as appropriate. Similar testing was used to compare the groups with and without complete ABG data. We then examined associations between hyperventilation severity and two outcomes—DCI and poor functional outcome (mRs >3)—using bivariate logistic regression. In addition to demographic factors (age, gender), factors with statistically significant associations in bivariate analysis were included in multivariable logistic regression analysis, and results were expressed as adjusted odds ratios. We used the same multivariable models adjusting for demographic characteristics, SAH severity, etiology, and complications to obtain adjusted predicted probabilities of both DCI and poor functional outcome at different severities of hyperventilation (none, moderate, and severe). To assess final model fit, we used the area under the curve method (C statistic = 0.75 for model with outcome of DCI; C statistic = 0.88 for model with outcome of poor discharge mRs) and the Hosmer–Lemeshow goodness of fit test (both models had p > 0.05, suggesting good model fit). We considered a two-sided p < 0.05 statistically significant. All analyses were performed using STATA version 13 (Stata Corp, College Station, TX).
Results
Of 317 patients, 207 were included in the final analysis and 110 patients were excluded for not having an eligible ABG. Of the 110 excluded patients, 109 were excluded because they did not have an ABG checked during their hospitalization. None of these patients had required mechanical ventilation. One mechanically ventilated patient did not have an ABG obtained while overbreathing the ventilator, and was also excluded. Overall, 32 of 207 (15.5 %) patients in the study group were mechanically ventilated versus 1 of 110 patients (0.9 %) in the excluded group. Study patients were also older and had greater severity of illness (Supplemental Table 1).
Of the 207 patients eligible for the study, 113 (55 %) had an ABG with both PaCO2 <35 mmHg and pH >7.45 and were classified as having spontaneous hyperventilation. Forty-nine of the 113 with spontaneous hyperventilation (43.4 %) had an ABG with PaCO2 ≤30 mmHg and pH ≥7.5 and were determined to have severe spontaneous hyperventilation. The remaining 64 (56.6 %) were considered to have moderate spontaneous hyperventilation.
Clinical characteristics of patients with spontaneous hyperventilation are compared to those without spontaneous hyperventilation in Table 1. Those with spontaneous hyperventilation had significantly higher incidence of both DCI (43.4 vs. 18.1 %, p < 0.001) and poor discharge outcome (68.5 vs. 41.8 %, p < 0.001). There were no significant differences in age, gender, medical comorbidities, method of aneurysm treatment, and aneurysm location. However, spontaneously hyperventilating patients were significantly more likely to have an aneurysmal etiology (86.7 vs. 75.5 %, p = 0.03), higher mean WFNS (3.2 vs. 2.5, p = 0.007), and HH (3.5 vs. 2.9, p = 0.001) scores, and were more likely to experience radiographic vasospasm (34.6 vs. 10.5 %, p < 0.001), pneumonia (38.1 vs. 14.9 %, p < 0.001), neurogenic myocardial injury (38.9 vs. 22.3 %, p = 0.01), and SIRS (66.4 vs. 42.6 %, p = 0.001).
In bivariate analysis, we found that patients with moderate hyperventilation had almost three times the odds of DCI [odds ratio (OR) 2.9, 95 % confidence interval (CI) 1.40–6.00], and patients with severe hyperventilation had over 4 times the odds of DCI (OR 4.35, CI 2.02–9.37), compared to patients without spontaneous hyperventilation (Table 2). Other factors significantly associated with DCI were WFNS (OR 1.31, CI 1.10–1.56), SAH sum score (OR 1.07, CI 1.04–1.10), neurogenic myocardial injury (OR 2.17, CI 1.27–3.70), SIRS (OR 6.01, CI 3.37–10.72), and pneumonia (OR 4.14, CI 2.28–7.50). Relative to aneurysmal etiology, perimesencephalic SAH had a significant inverse association with DCI (OR 0.05, CI 0.01–0.40).
Additionally, severe hyperventilation was strongly associated with poor discharge outcome (OR 9.30, CI 3.58–24.14), while the association with moderate hyperventilation was not statistically significant (OR 1.69, CI 0.88–3.25). Other factors significantly associated with poor discharge outcome were age (OR 1.04, CI 1.02–1.06), WFNS (OR 3.32, CI 2.60–4.24), SAH sum score (OR 1.09, CI 1.06–1.12), SIRS (OR 9.96, CI 5.84–16.98), pneumonia (OR 6.32, CI 3.32–12.04), and DCI (OR 3.96, CI 2.27–6.92). Relative to aneurysmal etiology, perimesencephalic SAH was less likely to be associated with poor discharge outcome (OR 0.09, CI 0.03–0.29).
In addition to age and gender, all factors significantly associated with DCI in the bivariate analysis were included in a multivariable logistic regression model (Table 3). After adjusting for WFNS, SAH sum score, etiology, pneumonia, and SIRS, only moderate (OR 2.49, CI 1.10–5.62) and severe (OR 3.12, CI 1.30–7.49) spontaneous hyperventilation remained significantly associated with DCI. Similarly, in addition to age and gender, all factors significantly associated with poor discharge outcome in bivariate analysis were included in a multivariable logistic regression model of poor discharge outcome (Table 4). After adjusting for WFNS, SAH sum score, pneumonia, and DCI, severe spontaneous hyperventilation remained significantly associated with poor discharge outcome (OR 4.52, CI 1.37–14.89). Other covariates with significant associations include age (OR 1.05, CI 1.02–1.08), WFNS (OR 2.47, CI 1.78–3.42), and SIRS (OR 2.76, CI 1.10–6.89).
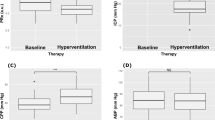
Figure 1 shows the predicted probability of DCI for patients with different hyperventilation status, after controlling for age, gender, WFNS, SAH sum score, etiology, pneumonia, and SIRS. The adjusted predicted probability of DCI was 18.5 % for patients with no hyperventilation, 39.1 % for those with moderate hyperventilation, and 50.0 % when severe hyperventilation was present. Compared to patients with no hyperventilation, patients with moderate and severe spontaneous hyperventilation were significantly more likely to experience DCI (p = 0.003 and p < 0.001, respectively). Figure 2 shows the adjusted predicted probability of poor discharge outcome for patients by hyperventilation status, after adjusting for age, sex, WFNS, SAH sum score, pneumonia, and DCI. The adjusted predicted probability of poor discharge outcome was 42.2 % for patients with no hyperventilation, 54.8 % for those with moderate hyperventilation, and 86.4 % when severe hyperventilation was present. Compared to patients with severe hyperventilation, patients with no and moderate spontaneous hyperventilation were significantly less likely to experience a poor discharge outcome (p < 0.001 for both comparisons). The difference in adjusted predicted probability for patients with moderate compared to no spontaneous hyperventilation did not reach the pre-specified threshold of statistical significance (p = 0.05).
The adjusted predicted probability of DCI was 18.5 % for patients with no hyperventilation, 39.1 % for those with moderate hyperventilation, and 50.0 % when severe hyperventilation was present. Error bars show 95 % confidence intervals. Compared to those with no hyperventilation, the probability of DCI was significantly increased in patients with moderate (p = 0.003) and severe (p < 0.001) hyperventilation. There was no significant difference between patients with moderate and severe hyperventilation (p = 0.23)
The adjusted predicted probability of poor discharge outcome was 42.2 % for patients with no hyperventilation, 54.8 % for those with moderate hyperventilation, and 86.4 % when severe hyperventilation was present. Error bars show 95 % confidence intervals. Compared to those with severe hyperventilation, the probability of poor discharge outcome was significantly lower in patients with no (p < 0.001) and moderate (p < 0.001) hyperventilation. The difference between patients with no and moderate hyperventilation was not statistically significant (p = 0.05)
Discussion
In this retrospective analysis of a prospectively collected database of SAH patients admitted to an academic neurological ICU, we found that spontaneous hyperventilation was common and independently associated with DCI and poor discharge outcome. These results suggest a novel and potentially clinically relevant relationship between spontaneous hyperventilation, DCI, and functional outcome. To our knowledge, this is the first study to detect an association between spontaneous hyperventilation and DCI. It is also the first study to demonstrate a relationship between spontaneous hyperventilation and neurological outcome in a dedicated population of SAH patients. Our results are consistent with previous studies that have shown increased mortality in TBI patients treated with induced hyperventilation [1].
The exact mechanism of the association between spontaneous hyperventilation and DCI is unclear. It may be explained by the marked decrease in CBF that is triggered by hypocapnia. However, the observational nature of this study limits inferences about causality. Another important potential mediator of hyperventilation after SAH is the SIRS. SIRS is common after SAH, and our data and other studies suggest that it is associated with poor neurological outcome and may have an association with DCI [25, 26]. However, inclusion of SIRS in both multivariable logistic regression models did not affect the strength of the associations with spontaneous hyperventilation.
It is also possible that severe brain injury and/or DCI directly induce hyperventilation, similar to the phenomenon of central neurogenic hyperventilation. Although case reports of central neurogenic hyperventilation are largely restricted to patients with infiltrating brain tumors [27–29], it has been described in a variety of other disease entities [30–32]. There is extensive cortical inhibitory input into the brainstem respiratory centers [33]. This has led some to hypothesize that severe brain injury may induce hyperventilation by disrupting this cortical inhibition, thereby “releasing” brainstem respiratory centers and triggering hyperventilation [34]. Theoretically, in the case of DCI this process could become self-reinforcing because hyperventilation would further decrease CBF, consequently triggering more hyperventilation.
Although the causal nature of the association between spontaneous hyperventilation, DCI, and neurological outcome is uncertain, some may consider therapeutic interventions to minimize hyperventilation. In fact, induced hypercapnia has recently been proposed as an acute treatment for DCI [35]. Unfortunately, in spontaneously breathing patients, therapeutic options are limited. Hypocarbia-induced cerebral vasoconstriction is mediated by nitric oxide [36]. Consequently, nitric oxide donors currently being tested for treatment of SAH-induced vasospasm may also mitigate the effects of hyperventilation, but this has not been tested [37]. Adding dead space to the ventilator circuit can sometimes reduce hypocapnia. Sedation with opioids can also be effective, but may interfere with monitoring of the patient’s neurological status [38, 39]. The use of neuromuscular blockade is typically discouraged in critically ill neurological patients because it further compromises the ability to assess neurological status, and neuromuscular blockers significantly increase the risk of adverse effects such as ICU-acquired weakness [40, 41]. Additional study is needed before either modality should be recommended to treat severe spontaneous hyperventilation in SAH. Previous studies have used cerebral oxygenation monitors to show decreased brain oxygen during spontaneous hyperventilation [11]. Invasive or non-invasive cerebral oxygen or blood flow monitors may be particularly useful for measuring treatment efficacy in future studies. At present, a reasonable treatment approach is to consider low-risk interventions to reduce common triggers of hyperventilation, such as pain and inflammation.
This study has several limitations that should be considered when interpreting the results. First, several patients were excluded from analysis because they did not have an ABG. This selected for a population of patients with greater illness severity, so it is likely that our analysis overestimates the true prevalence of hyperventilation in SAH patients. However, the final cohort was relatively evenly matched between patients with and without hyperventilation, and it is unlikely that excluding these patients had a significant impact on the associations that were identified. Additionally, inclusion in the hyperventilation group only required a single ABG obtained at any time point showing a respiratory alkalosis. Both timing and duration of hyperventilation could influence DCI and neurological outcome, but the current study limits analysis to presence or absence of hyperventilation, rather than timing of onset or cumulative duration.
As this study was conducted at a single academic center, it is possible that these results are not generalizable to all patient populations. However, our institution is a referral center for a wide geographic region, and all care was provided in accordance with standard guidelines. Further, since the study was observational, it may not be possible to account for all confounders mediating an association between hyperventilation, DCI, and poor neurological outcome. Nonetheless, our final regression models include well-established markers of clinical (WFNS) and radiographic (SAH sum score) severity, along with all other factors that were significant in bivariate analysis. Important potential confounders such as infectious and non-infectious triggers of inflammation were accounted for by including pneumonia and SIRS in the final models.
Conclusion
Spontaneous hyperventilation is common in patients with SAH and is significantly associated with DCI and poor neurological outcome at hospital discharge. Further study is needed to determine the pathophysiological underpinnings of this association. Interventions to minimize hyperventilation in SAH patients may be considered, though at present further investigations are needed to determine if they have any beneficial effect on outcome.
References
Muizellar JP, Marmarou A, Ward JD, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75:731–9.
Curley G, Kavanagh BP, Laffey JG. Hypocapnia and the injured brain: more harm than benefit. Crit Care Med. 2010;38:1348–59.
Huang CT, Cook AW, Lyons HA. Severe craniocerebral trauma and respiratory abnormalities. Arch Neurol. 1963;9:545–54.
Lee MC, Klassen AC, Resch JA. Respiratory pattern disturbances in ischemic cerebral vascular disease. Stroke. 1971;5:612–6.
Rout MW, Lane DJ, Wollner L. Prognosis in acute cerebrovascular accidents in relation to respiratory pattern and blood gas tensions. BMJ. 1971;3:7–9.
Vapalahti M, Troupp H. Prognosis for patients with severe brain injuries. BMJ. 1971;3:404–7.
North BJ, Jennet S. Abnormal breathing patterns associated with acute brain damage. Arch Neurol. 1974;31:338–44.
Raichle ME, Plum F. Hyperventilation and cerebral blood flow. Stroke. 1972;3:566–75.
Coles JP, Minhas PS, Fryer TD, et al. Effect of hyperventilation on cerebral blood flow in traumatic head injury: clinical relevance and monitoring correlates. Crit Care Med. 2002;30:1950–9.
Coles JP, Fryer TD, Coleman MR, et al. Hyperventilation following head injury: effect on ischemic burden and cerebral oxidative metabolism. Crit Care Med. 2007;35:568–78.
Carrera E, Schmidt JM, Fernandez L, et al. Spontaneous hyperventilation and brain tissue hypoxia in patients with severe brain injury. J Neurol Neurosurg Psychiatry. 2010;81:793–7.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–96.
Van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid hemorrhage. Lancet. 2007;369:306–18.
Diringer MN, Bleck TP, Hemphill JC, et al. Critical care management of patient’s following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit Care. 2011;15:211–40.
Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2012;43:1711–37.
Hunt WE, Hess RM. Surgical risk as related to the time of intervention in the repair of cerebral aneurysms. J Neurosurg. 1968;28:14–20.
Drake CG. Report of World Federation of Neurosurgeons committee on a universal subarachnoid hemorrhage grading system. J Neurosurg. 1988;68:985–6.
Hjidra A, van Gijn J, Nagelkerke NJD, Vermeulen M, van Cevel H. Prediction of delayed cerebral ischemia, rebleeding, and outcome after aneurysmal subarachnoid hemorrhage. Stroke. 1988;19:1250–6.
Frontera JA, Claassen J, Schmidt JM, et al. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified Fisher scale. Neurosurgery. 2007;59:21–7.
Mayer SA, Lin J, Homma S, et al. Myocardial injury and left ventricular performance after subarachnoid hemorrhage. Stroke. 1999;30:780–6.
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101:1644–55.
Frontera JA, Fernandez A, Schmidt JM. Defining vasospasm after subarachnoid hemorrhage. What is the most clinically relevant definition? Stroke. 2009;40:1963–8.
Sulter G, Steen C, De Keyser J. Use of the Barthel index and modified Rankin scale in acute stroke trials. Stroke. 1999;30:1538–41.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Dhar R, Diringer MN. The burden of the systemic inflammatory response syndrome predicts vasospasm and outcome after subarachnoid hemorrhage. Neurocrit Care. 2008;8:404–12.
Tam AKH, Ilodigwe D, Mocco J, et al. Impact of systemic inflammatory response syndrome on vasospasm, cerebral infarction, and outcome after subarachnoid hemorrhage: exploratory analysis of CONSCIOUS-1 data. Neurocrit Care. 2013;13:182–9.
Plum F, Swanson AG. Central neurogenic hyperventilation in man. AMA Arch Neurol Psychiatry. 1959;81:535–49.
Tarulli AW, Lim C, Bui JD, et al. Central neurogenic hyperventilation: a case report and discussion of pathophysiology. Arch Neurol. 2005;62:1632–4.
Ledet D, Delos NM, Khan R, et al. Central neurogenic hyperventilation and renal tubular acidosis in children with pontine gliomas. Neurology. 2014;82:1099–100.
Johnston SC, Singh V, Ralston HJ, Gold WM. Chronic dyspnea and hyperventilation in an awake patient with small subcortical infarcts. Neurology. 2001;47:2131–3.
Nystad D, Salvesen R, Nielsen EW. Brainstem encephalitis with central neurogenic hyperventilation. J Neurol Neurosurg Psychiatry. 2007;78:107–8.
Takahashi M, Tsunemi T, Miyayosi T, Mizusawa H. Reversible central neurogenic hyperventilation in an awake patient with multiple sclerosis. J Neurol. 2007;254:1763–4.
Plum F. Neurological integration of behavioral and metabolic control of breathing. In: Porter R, editor. Breathing: Hering–Breur Centenary Symposium: CIBA Foundation. London: Churchill; 1970. p. 159–75.
Leitch AG, McLennan JE, Balkenhol RG, et al. Mechanisms of hyperventilation in head injury: case report and review. Neurosurgery. 1979;5:701–7.
Westermaier T, Stetter C, Kunze E, et al. Controlled transient hypercapnia: a novel approach for the treatment of delayed cerebral ischemia after subarachnoid hemorrhage? J Neurosurg. 2014;121:1056–62.
Thompson BG, Pluta RM, Girton ME, Oldfield EH. Nitric oxide mediation of chemoregulation but not autoregulation of cerebral blood flow in primates. J Neurosurg. 1994;84:71–8.
Fathi AR, Bakhtian KD, Pluta RM. The role of nitric oxide donors in treating cerebral vasospasm after subarachnoid hemorrhage. In: Feng H, et al., editors. Early brain injury or cerebral vasospasm, vol. 110., Acta Neurochirugica SupplementVienna: Springer; 2011. p. 93–7.
Jaeckle KA, Digre KB, Jones CR, Bailey PL, McMahill PC. Central neurogenic hyperventilation: pharmacologic intervention with morphine sulfate and correlative analysis of respiratory, sleep, and oculomotor dysfunction. Neurology. 1990;40:1715–20.
Adashi YU, Sano H, Doi M, Santo S. Central neurogenic hyperventilation treated with intravenous fentanyl followed by transdermal application. J Anes. 2007;21:417–9.
Greenberg SB, Vender J. The use of neuromuscular blocking agents in the ICU: where are we now? Crit Care Med. 2014;41:1332–44.
Sanfilippo F, Santonocito C, Veenith T, Astuto M, Maybauer MO. The role of neuromuscular blockade in patients with traumatic brain injury: a systematic review. Neurocrit Care. 2014;. doi:10.1007/s12028-014-0061-1.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding support
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Williamson, C.A., Sheehan, K.M., Tipirneni, R. et al. The Association Between Spontaneous Hyperventilation, Delayed Cerebral Ischemia, and Poor Neurological Outcome in Patients with Subarachnoid Hemorrhage. Neurocrit Care 23, 330–338 (2015). https://doi.org/10.1007/s12028-015-0138-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-015-0138-5