Abstract
Background
There is a paucity of reliable and recent data regarding epidemiology of non-aneurysmal subarachnoid hemorrhage (SAH) in population-based studies.
Objectives
To determine the incidence and case fatality of non-aneurysmal SAH using a population-based design.
Methods
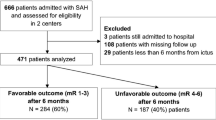
Medical records and angiographic data of all patients from Stearns and Benton Counties, Minnesota, admitted with SAH were reviewed to identify incident case of non-aneurysmal SAH. Patients with a first-time diagnosis of non-aneurysmal SAH (based on two negative cerebral angiograms performed ≥7 days apart) between June 1st, 2012 and June 30th, 2014 were considered incident cases. We calculated the incidences of non-aneurysmal and aneurysmal SAH adjusted for age and sex based on the 2010 US census.
Results
Of the 18 identified SAH among 189,093 resident populations, five were true incident cases of non-aneurysmal SAH in this population-based study. The age- and sex-adjusted incidence of non-aneurysmal SAH were 2.8 [95 % confidence interval (CI) 2.7–2·9] per 100,000 person-years which was lower than aneurysmal SAH incidence of 7.2 [95 % CI 7.1–7.4] per 100,000 person-years. The age-adjusted incidence of non-aneurysmal SAH was similar (compared with aneurysmal SAH) among men; 3.2 [95 % CI 3.1–3.3] per 100,000 person-years versus 2.2 [95 % CI 2.1–2.3] per 100,000 person-years, respectively. The age-adjusted case fatality rate at 3 months was 4.46 and 0.0 per 100,000 persons for aneurysmal and non-aneurysmal SAH, respectively.
Conclusions
The incidence of non-aneurysmal SAH was higher than previously reported particularly among men.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A review of 51 studies describing 58 study populations in 21 countries, reported a range of incidence of subarachnoid hemorrhage (SAH) from 22.7 (95 % confidence interval [CI] 21.9–23.5) in Japan, 19.7 (95 % CI 18.1–21.3) in Finland, 4.2 (95 % CI 3.1–5.7) in South and Central America, and 9.1 (95 % CI 8.8–9.5) in the other regions per 100,000 person-years [1]. The review did not differentiate between aneurysmal and non-aneurysmal SAH. Most studies have focused on aneurysmal SAH [2–4]. Estimation of incidence of non-aneurysmal SAH has been difficult because of inability to differentiate between SAH related to undiagnosed aneurysms and true non-aneurysmal SAH. In a nationwide study, 40 % of 77,352 patients admitted with non-traumatic SAH underwent either endovascular or surgical treatment for intracranial aneurysms [5]. The rates of any treatment (neurosurgical or endovascular) in population-based SAH-patient studies using case ascertainment by chart review have ranged from 38 to 70 % [6–8]. The relatively low rate of treatment is presumably attributable to relatively high rates of non-aneurysmal SAH [9] and early mortality (within 24 h) among non-traumatic SAH [6]. We performed this study to determine the actual incidence of non-aneurysmal SAH in a population-based cohort using a standard definition and associated case fatality.
Methods
Stearns and Benton Counties are situated in central Minnesota with a total area of 1,751 square miles or 1,120,915 acres. Both counties contain 38 cities and 46 townships. As of the US 2010 census, there were 189,093 people, 71,653 households, and 46,396 families residing in both counties. The population density was 108 people per square mile (67/km2). The racial/ethnic makeup of both counties was 92.34 % White, 2.85 % African American, 0.33 % Native American, 1.8 % Asian, 0.03 % Pacific Islander, 1.06 % from other races, and 1.56 % from two or more races; 2.55 % of the population were Hispanic of any race. The median age was 33.7 years and 23.48 % were under the age of 18 years, 14.59 % from 18 to 24, 25.46 % from 25 to 44, 24.40 % from 45 to 64, and 12.05 % who were 65 years of age or older. St. Cloud Hospital is the only acute care hospital and certified Primary Stroke Center with 489 licensed beds for both Stearns and Benton Counties. This hospital is the only hospital that provides endovascular and vascular neurosurgical services within Central Minnesota, and all patients with SAH within the catchment area are admitted to St. Cloud Hospital.
Case Ascertainment
Patients admitted with SAH from June 1st, 2012 through June 30th, 2014 were identified through several overlapping sources. Procedure notes for all diagnostic and interventional endovascular procedures were reviewed within a prospective database nested within EPIC electronic medical record system. A list of patients admitted with primary or secondary diagnoses of SAH (ICD-9-CM) code 430 was retrieved from data entered in the Get With The Guidelines®-Stroke registry. Cerebral angiography is performed for all patients with SAH documented by CT scan or identified in CSF analysis. Patients in whom an intracranial aneurysm was not documented underwent a repeat cerebral angiogram within 7–10 days. Patients who had primary residence within the 11 zip codes included in Stearns and Benton Counties were included in further analysis.
Data Collection
Patients admitted to St. Cloud Hospital with the diagnosis of SAH were identified using the above-mentioned methodology. Within EPIC electronic medical record system, patient charts were reviewed for information regarding demographic and clinical characteristics, preexisting risk factors, Hunt and Hess Scale at admission and Fisher grade based on initial CT scan findings. Details regarding aneurysm location, type of aneurism obliteration procedure, and details of medical treatment given were also extracted. Length of hospital stay and functional status defined by modified Rankin scale (mRS) at discharge was also ascertained. All vital status was ascertained by review of in-hospital and clinic records or by direct contact with patient or family by the treating physician to determine mortality at 1 and 3 months. In the event, the patient’s vital status could not be traced, we used the Social Security Administration Death Master File for ascertainment of vital status.
Sensitivity Analysis
A list of patients admitted with primary diagnoses of SAH (ICD-9-CM) code 430 and who had primary residence within the 11 zip codes included in Stearns and Benton Counties was retrieved from Minnesota Hospital Association data from June 1st, 2012 to December 31st, 2013. The methodology of data collection by Minnesota Hospital Association has been previously described [10, 11]. A total of 13 patients with the aforementioned ICD-9-CM codes were admitted from study population of which 12 were admitted to St. Cloud Hospital during the same period of time providing a yield of 92.3 %.
Data Analysis
We calculated age-adjusted incidence rates (age-adjusted to the 2010 US Standard Population) for all SAH, and aneurysmal and non-aneurysmal SAHs. The number of SAHs within each of the 11 age and gender groups were ascertained. We calculated crude rates using population data with the counts for each of the 11 age/gender groups expressed as the number of SAH events per 100,000 population at risk [12]. The age-adjusted rate was calculated by multiplying each crude rate by the appropriate weight and summing the products. We compared the incidence of aneurysmal and non-aneurysmal SAHs among men and women using standardized incidence ratio (SIR) with 95 % CI.
We also report the case fatality rate and mortality rate within 1 and 3 months of SAH onset for all SAH, and aneurysmal and non-aneurysmal SAHs. We calculated age-specific SAH-related death rate (ASDR) per 100,000 population for each age group as follows: ASDR = deaths in age group/estimated population of that age group × 100,000. Each ASDR was then multiplied by the proportion of the standard population for the same age group. The age-specific results were summed to get the age-adjusted death rate for SAH-related deaths as follows: AADR = Summation of (ASDR X standard proportion) [13].
Results
Of the 18 identified SAH, 5 were true incident cases of non-aneurysmal SAH, and one SAH was related to intracranial dissection, in this population-based study. Mean age (±SD) at diagnosis was 59.8 years (±18.8 years) compared with aneurysmal SAH 56.3 years (±11.3 years p = 0.6).The crude incidence of non-aneurysmal SAH was 2.7 [95 % CI 0.3–5.1] per 100,000 person-years which was lower than aneurysmal SAH incidence of 7.1 [95 % CI 3.3–10.9] per 100,000 person-years. The age-adjusted incidence of non-aneurysmal SAH was 2.8 [95 % CI 2.7–2·9] per 100,000 person-years which was lower than aneurysmal SAH incidence of 7.2 [95 % CI 7.1–7.4] per 100,000 person-years (SIR 0.38, 95 % CI 0.1–0.8, p = 0.1). There was a significantly higher age-adjusted incidence of aneurysmal SAH (compared with non-aneurysmal SAH) among women (12.1 [95 % CI 12.0–12.3] per 100,000 person-years vs. 2.3 [95 % CI 2.2–3.0] per 100,000 person-years; SIR 5.26, 95 % CI 3.3–8.5, p < 0.001). The age-adjusted incidence of aneurysmal SAH was similar (compared with non-aneurysmal SAH) among men (2.2 [95 % CI 2.1–2.3] per 100,000 person-years vs. 3.2 [95 % CI 3.1–3.3] per 100,000 person-years; SIR 0.66, 95 % CI 0.3–1.6, p = 0.5).
At admission, 6 of 13 patients with aneurysmal SAH and 0 of 5 patients with non-aneurysmal SAH were categorized as poor grade (Hunt and Hess grade of 4 and 5), respectively. Eleven of 13 patients with aneurysmal SAH and 2 of 5 patients with non-aneurysmal SAH were categorized as Fisher grade of 3 or 4, respectively, based on initial CT scan. The distribution of blood was categorized as perimesencephalic in all of 5 patients with non-aneurysmal SAH versus diffuse in 13 patients with aneurysmal SAH. Angiographic cerebral vasospasm was documented in 4 patients and required endovascular treatment in 3 patients with aneurysmal SAH. No cerebral vasospasm in patients with non-aneurysmal SAH. Among survivors was identified with non-aneurysmal SAH, mild (mRS 1–2) and moderate (mRS 3–5) disability was seen in 3 and 2 patients, respectively, Among survivors with aneurysmal SAH, mild (mRS 1–2) and moderate (mRS 3–5) disability was seen in 5 and 4 patients, respectively. The 1-month case fatality rate of non-aneurysmal SAH was significantly lower compared with aneurysmal SAH (0.00 vs. 23.0 %, p = 0.2). The 3-month case fatality rate of non-aneurysmal SAH was significantly lower compared with aneurysmal SAH (0.0 vs. 30.8 %, p = 0.2). The 3-month mortality rate was higher among patients with aneurysmal SAH (4.3 per 100,000 persons) compared with non-aneurysmal SAH (0 per 100,000 persons). The age-adjusted case fatality rate at 3 months 4.4 and 0.0 per 100,000 persons for aneurysmal and non-aneurysmal SAH, respectively.
Discussion
The incidence of non-aneurysmal SAH was relatively high with the incidence of aneurysmal and non-aneurysmal SAH being similar among men. Although, the case fatality was quite low, the rate of disability of any severity was considerable. The frequency of non-aneurysmal SAH in recent studies is low and ranges from 11 to 19 % in data derived from tertiary care specialized centers [14–16]. The incidence estimates from such reports are often artifactually lower because of transferred patients and selective triages based on presence of aneurysms on noninvasive imaging results. Incidence studies pertaining to SAH are particularly prone to such biases because of high rates of transfer for aneurysm treatment [17, 18]. At tertiary care centers, approximately 50–70 % of the SAH patients are transferred from other hospitals [19, 20]. Therefore, the impact of skewed estimates can be considerable. We used a population-based design to avoid the biases introduced by selective triages and admission patterns. We also used serial angiographic criteria for confirmation of absence of intracranial aneurysm or other underlying etiology. Such methodology avoids lack of detection of small intracranial aneurysms seen with CT angiography [21] and delayed appearance of aneurysms [14]. There is a possibility that the relatively higher than expected incidence ratio of non-aneurysmal SAH maybe related to decreasing rates of SAH related to aneurysmal rupture because of increasing treatments provided at an unruptured state [22]. The incidence of aneurysmal and non-aneurysmal SAH was similar among men but the incidence of aneurysmal SAH was prominently higher than non-aneurysmal SAH among women. Although the incidence of non-aneurysmal SAH appeared similar among men and women, the higher incidence of aneurysmal SAH explained the higher incidence of all SAHs in women seen in our and other studies [1].
Our current understanding of management of SAH patients is based upon data generated from aneurysmal SAH patients [14]. Non-aneurysmal SAH patients have been excluded from several large clinical trials including randomized clinical trials of nimodipine [23–25], nicardipine [26], magnesium sulfate [27, 28], tirilazad mesylate [29–31], and clazosentan [32, 33]. We found no case fatality but 2 of 5 patients (40 %) had severe disability following non-aneurysmal SAH. The absence of any case fatality in our study maybe attributable to perimesencephalic location of SAH and/or absence of angiographic vasospasm requiring treatment in non-aneurysmal SAH patients. Death or severe disability can be seen in 20 % of the patients with non-aneurysmal SAH [15] with high incidence of in-hospital adverse events [14]. In a combined analysis of case series and 18 previous reports [34], the overall rate of vasospasm was 16.3 % (95 % CI 12.3–21.1) and cerebral ischemia was 6.8 % (95 % CI 5.0–9.1) in non-aneurysmal SAH patients. In patients with diffuse SAH, the rates of vasospasm and cerebral ischemia were 31.3 % (95 % CI 21.6–43.9) and 9.7 % (95 % CI 7.0–13.0), respectively, Therefore, exclusion of such patients from clinical trials and studies of therapeutic interventions prevents adequate reduction in death and disability associated with SAH [5].
Our largest limitation was small number of events which was a consequence of restricting the denominator population to two counties and one hospital. Such a restriction resulted in high accuracy of the diagnosis of non-aneurysmal SAH and avoidance of variations in management between hospitals. However, the precision of estimates is lower than that seen with a larger number of events. The relatively low precision of estimate due to large contribution of single events in the analysis can exaggerate the incidence and disability estimates associated with non-aneurysmal SAH. The small number of events also reduced our ability to detect differences in incidences between men and women and other subgroups. There was a difference in time periods between US census and case ascertainment but the estimated 1.0 and 2.0 % population increases between April 1, 2010 and July 1, 2013 in Stearns and Benton counties was too small to affect calculation of incidences [35]. Nonetheless, the high incidence and burden of non-aneurysmal SAH were highlighted by the results of our study. The unique predisposition of men to non-aneurysmal SAH requires further study.
References
de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78:1365–72.
Lindekleiv HM, Njolstad I, Ingebrigtsen T, Mathiesen EB. Incidence of aneurysmal subarachnoid hemorrhage in Norway, 1999–2007. Acta Neurol Scand. 2011;123:34–40.
ACROSS Group. Epidemiology of aneurysmal subarachnoid hemorrhage in Australia and New Zealand: incidence and case fatality from the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS). Stroke. 2000;31:1843–50.
Ishihara H, Kunitsugu I, Nomura S, et al. Seasonal variation in the incidence of aneurysmal subarachnoid hemorrhage associated with age and gender: 20-year results from the Yamaguchi cerebral aneurysm registry. Neuroepidemiology. 2013;41:7–12.
Qureshi AI, Vazquez G, Tariq N, Suri MF, Lakshminarayan K, Lanzino G. Impact of International Subarachnoid Aneurysm Trial results on treatment of ruptured intracranial aneurysms in the United States. Clinical article. J Neurosurg. 2011;114:834–41.
Inagawa T. Trends in surgical and management outcomes in patients with aneurysmal subarachnoid hemorrhage in Izumo city, Japan, between 1980–1989 and 1990–1998. Cerebrovasc Dis. 2005;19:39–48.
Pobereskin LH. Incidence and outcome of subarachnoid haemorrhage: a retrospective population based study. J Neurol Neurosurg Psychiatry. 2001;70:340–3.
Ronne-Engstrom E, Enblad P, Gal G, et al. Patients with spontaneous subarachnoid haemorrhage—presentation of a 10-year hospital series. Br J Neurosurg. 2009;23:499–506.
Sacco S, Totaro R, Toni D, Marini C, Cerone D, Carolei A. Incidence, case-fatalities and 10-year survival of subarachnoid hemorrhage in a population-based registry. Eur Neurol. 2009;62:155–60.
Qureshi AI, Chaudhry SA, Rodriguez GJ, Suri MF, Lakshminarayan K, Ezzeddine MA. Outcome of the ‘Drip-and-Ship’ paradigm among patients with acute ischemic stroke: results of a statewide study. Cerebrovasc Dis Extra. 2012;2:1–8.
Qureshi AI, Chaudhry SA, Majidi S, Grigoryan M, Rodriguez GJ, Suri MF. Population-based estimates of neuroendovascular procedures: results of a state-wide study. Neuroepidemiology. 2012;39:125–30.
Surveillance, epidemiology, and end results program-turning cancer data into discovery. National Institutes of Health: Bethesda.
Missouri Department of Health adn Seniour Services. Missouri 1999. NIH publication 99–4564.
Khan AA, Smith JD, Kirkman MA, et al. Angiogram negative subarachnoid haemorrhage: outcomes and the role of repeat angiography. Clin Neurol Neurosurg. 2013;115:1470–5.
Lin N, Zenonos G, Kim AH, et al. Angiogram-negative subarachnoid hemorrhage: relationship between bleeding pattern and clinical outcome. Neurocrit Care. 2012;16:389–98.
Andaluz N, Zuccarello M. Yield of further diagnostic work-up of cryptogenic subarachnoid hemorrhage based on bleeding patterns on computed tomographic scans. Neurosurgery. 2008;62:1040–6 discussion 7.
Rosner J, Nuno M, Miller C, et al. Subarachnoid hemorrhage patients: to transfer or not to transfer? Neurosurgery. 2013;60(Suppl 1):98–101.
Samuels O, Webb A, Culler S, Martin K, Barrow D. Impact of a dedicated neurocritical care team in treating patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2011;14:334–40.
Drazin D, Rosner J, Nuno M, et al. Type of admission is associated with outcome of spontaneous subarachnoid hemorrhage. Int J Stroke. 2013;. doi:10.1111/ijs.12005.
Catalano AR, Winn HR, Gordon E, Frontera JA. Impact of interhospital transfer on complications and outcome after intracranial hemorrhage. Neurocrit Care. 2012;17:324–33.
Anderson GB, Steinke DE, Petruk KC, Ashforth R, Findlay JM. Computed tomographic angiography versus digital subtraction angiography for the diagnosis and early treatment of ruptured intracranial aneurysms. Neurosurgery. 1999;45:1315–20 discussion 20-2.
Siddiq F, Adil MM, Kainth D, Moen S, Qureshi AI. The emergence of endovascular treatment-only centers for treatment of intracranial aneurysms in the United States. J Stroke Cerebrovasc Dis. 2013;22:e504–10.
Allen GS, Ahn HS, Preziosi TJ, et al. Cerebral arterial spasm–a controlled trial of nimodipine in patients with subarachnoid hemorrhage. New Engl J Med. 1983;308:619–24.
Philippon J, Grob R, Dagreou F, Guggiari M, Rivierez M, Viars P. Prevention of vasospasm in subarachnoid haemorrhage. A controlled study with nimodipine. Acta Neurochir. 1986;82:110–4.
Petruk KC, West M, Mohr G, et al. Nimodipine treatment in poor-grade aneurysm patients. Results of a multicenter double-blind placebo-controlled trial. J Neurosurg. 1988;68:505–17.
Haley EC Jr, Kassell NF, Torner JC, Truskowski LL, Germanson TP. A randomized trial of two doses of nicardipine in aneurysmal subarachnoid hemorrhage. A report of the Cooperative Aneurysm Study. J Neurosurg. 1994;80:788–96.
Bradford CM, Finfer S, O’Connor A, et al. A randomised controlled trial of induced hypermagnesaemia following aneurysmal subarachnoid haemorrhage. Crit Care Resusc. 2013;15:119–25.
Dorhout Mees SM, Algra A, Vandertop WP, et al. Magnesium for aneurysmal subarachnoid haemorrhage (MASH-2): a randomised placebo-controlled trial. Lancet. 2012;380:44–9.
Lanzino G, Kassell NF. Double-blind, randomized, vehicle-controlled study of high-dose tirilazad mesylate in women with aneurysmal subarachnoid hemorrhage. Part II. A cooperative study in North America. J Neurosurg. 1999;90:1018–24.
Haley EC Jr, Kassell NF, Apperson-Hansen C, Maile MH, Alves WM. A randomized, double-blind, vehicle-controlled trial of tirilazad mesylate in patients with aneurysmal subarachnoid hemorrhage: a cooperative study in North America. J Neurosurg. 1997;86:467–74.
Haley EC Jr, Kassell NF, Torner JC. A randomized controlled trial of high-dose intravenous nicardipine in aneurysmal subarachnoid hemorrhage. A report of the Cooperative Aneurysm Study. J Neurosurg. 1993;78:537–47.
Shen J, Pan JW, Fan ZX, Xiong XX, Zhan RY. Dissociation of vasospasm-related morbidity and outcomes in patients with aneurysmal subarachnoid hemorrhage treated with clazosentan: a meta-analysis of randomized controlled trials. J Neurosurg. 2013;119:180–9.
Macdonald RL, Higashida RT, Keller E, et al. Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haemorrhage undergoing surgical clipping: a randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol. 2011;10:618–25.
Gross BA, Lin N, Frerichs KU, Du R. Vasospasm after spontaneous angiographically negative subarachnoid hemorrhage. Acta Neurochir. 2012;154:1127–33.
Commerce USDo. State & County Quick Facts. United States Census Bureau. Online: Census Bureau; 2014.
Conflict of interest
The authors declare that they have no conflict of interest.
Financial Disclosure
Dr. Qureshi has received funding from the National Institutes of Health RO1-NS44976-01A2 (medication provided by ESP Parma), American Heart Association Established Investigator Award 0840053N, National Institute of Health U01-NS062091-01A2, and the Minnesota Medical Foundation, Minneapolis, MN.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qureshi, A.I., Jahangir, N., Qureshi, M.H. et al. A Population-Based Study of the Incidence and Case Fatality of Non-aneurysmal Subarachnoid Hemorrhage. Neurocrit Care 22, 409–413 (2015). https://doi.org/10.1007/s12028-014-0084-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0084-7