Abstract
Background
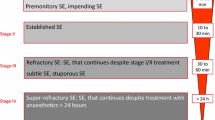
Management of refractory status epilepticus (SE) involves administration of intravenous γ-aminobutyric acid (GABAA) receptor agonists, such as benzodiazepines, barbiturates, or propofol. Animal models suggest that reductions in synaptic GABAA receptors may cause these drugs to become less effective as the duration of SE increases. This may explain the large doses that are commonly required to control seizures, which in turn contributes to a high incidence of complications, including hypotension and the need for vasopressors. In contrast, expression of excitatory N-methyl-d-aspartate (NMDA) receptors increases with prolonged SE and their stimulation by glutamate may propagate seizure activity. Ketamine is a NMDA-receptor antagonist that is considered promising as treatment for refractory SE. Compared with other anaesthetic drugs, ketamine produces less hypotension.
Methods
This report describes a patient who developed worsening hypotension with escalating doses of midazolam and propofol in the context of non-convulsive SE. He was therefore treated with ketamine within hours of being diagnosed.
Results
Ketamine was immediately efficacious at reducing the frequency, amplitude, and duration of seizures. The dose was rapidly titrated upwards using quantitative continuous EEG monitoring, until seizures were completely abolished. SE did not recur with weaning of sedatives and he went on to have an excellent recovery. A small number of previous reports have found ketamine to abort late SE. In most cases, ketamine was administered several days into the course, and outcomes were poor even though seizures were controlled.
Conclusion
Larger series and phase I clinical trial(s) of ketamine for treatment of refractory SE seem warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Status epilepticus (SE) is commonly defined as “refractory” when it fails to respond to conventional doses of benzodiazepines and at least one anti-epileptic drug (AED) [1]. Management of refractory SE involves endotracheal intubation and use of intravenous infusions of γ-aminobutyric acid (GABAA) receptor agonists, such as midazolam, propofol, or barbiturates [2]. Administration of deep sedation to suppress seizures is frequently complicated by hypotension, which commonly necessitates use of vasopressor agents.
Animal studies have reported that with prolonged SE, GABAA receptors become internalized within neurons, such that their concentration at synaptic membranes decreases and conventional doses of GABAA agonists become less effective [3]. In contrast, the concentration of synaptic N-methyl-d-aspartate (NMDA) receptors increases over time. Activation of these receptors by glutamate increases intracellular calcium, which may contribute to neuronal injury and promote further seizures. NMDA receptor antagonists appear to be especially effective in late SE [4, 5].
Ketamine is a unique anesthetic agent which blocks NMDA receptors and is therefore promising for the treatment of refractory SE [6]. An additional advantage is that it produces less hypotension than other anesthetic drugs. A small number of case reports have suggested that ketamine may be effective at aborting refractory SE [7–14].
Case Report
A 60-year-old man with cerebral palsy and epilepsy, managed as an outpatient with phenytoin (200 mg in the morning, 250 mg at bedtime) and clobazam (10 mg twice daily), was admitted to hospital with community-acquired pneumonia. His phenytoin level at admission was noted to be supra-therapeutic (112 μ mol/l; normal range 40–80 μ mol/l). On examination, he was found to be ataxic and have lateral gaze nystagmus. The phenytoin dose was temporarily reduced to 250 mg/day (100 mg in the morning, 150 mg at bedtime) and he was admitted to the hospitalist service. Over the subsequent week, levels were repeatedly documented to be sub-therapeutic, and the dose was again gradually increased to 450 mg/day (150 mg three times daily). His pneumonia responded well to therapy with levofloxacin (500 mg per day).
Ten days into the hospitalization, he developed a generalized seizure, after which he did not immediately regain consciousness. His complete blood count, electrolyte levels, glucose, urea, creatinine, and liver enzyme concentrations were all found to be within normal limits. The intensive care unit (ICU) service was consulted and he required endotracheal intubation because of coma and poor airway protection. A computed tomography scan revealed no acute abnormality. Because of a low clinical suspicion for a central nervous system infection, no lumbar puncture was performed.
Shortly after admission to the ICU, continuous EEG (cEEG) monitoring was initiated. This demonstrated that he was having frequent non-convulsive seizures arising in his left temporal region and spreading across the corresponding cerebral hemisphere (Fig. 1). He received a further loading dose of phenytoin, as well as escalating doses of midazolam (repeated boluses of 5 mg and an infusion, which was progressively increased to 30 mg per hour). Because of persisting seizures, he subsequently received propofol (repeated boluses of 30 mg and an infusion increased to 50 μg/kg/min) and levetiracetam (1500 mg twice daily). These therapies were also unsuccessful at abolishing seizure activity. Arterial and central venous catheters were placed and he received fluid loading (2L) and norepinephrine (maximum 0.26 μg/kg/min) to maintain a mean arterial blood pressure greater than 70 mmHg. The central venous pressure was 11–13 mmHg and the central venous oxygen saturation was 85%.
Continuous EEG (top) and 12 h compressed density spectral array (CDSA) tracing (bottom T3-01 and T4-02). The CDSA x axis represents time, the y axis designates EEG frequencies between 0 and 30 Hz, and the color indicates the “power” (higher with increasing brightness). Nearly continuous seizure activity was seen over the left hemisphere during the initial 4 h (represented by the yellow bar), with corresponding peaks visualized using CDSA. During this time, the patient received escalating doses of midazolam and propofol (see text for details). He was also given levetiracetam and had previously already been loaded with phenytoin. The yellow asterisk indicates the time point corresponding to the 10 s raw EEG tracing, just prior to administration of 50 mg of ketamine, followed a 40 mg per hour infusion. Over the subsequent 8 h (represented by the red bar), with an incremental dose of ketamine, the frequency, amplitude, and duration of seizures gradually decreased (colour figure online)
To limit further hemodynamic compromise, it was decided to try ketamine to treat ongoing seizures, rather than further increasing the doses of midazolam or propofol. He initially received a 50 mg bolus, followed by an infusion of 40 mg per hour (0.6 mg/kg per hour). This immediately resulted in a reduction in the prevalence, duration, and amplitude of seizures (Fig. 1). With gradual dose-escalation over the subsequent hours, the seizure burden continued to decrease, until they were completely abolished approximately 12 h later, with ketamine infusing at a dose of 220 mg per hour (3.3 mg/kg per hour) (Fig. 2). Despite the increasing dose of ketamine, there was no further need to adjust the norepinephrine infusion rate to support his blood pressure (Fig. 3). After he had been seizure-free for approximately 48 h, sedative agents were gradually weaned off, with ongoing cEEG monitoring. Midazolam was discontinued first, since its active metabolites may cause prolonged sedation after cessation of a high-dose continuous infusion. Ketamine and propofol were subsequently gradually withdrawn, without any seizure recurrence. The patient regained consciousness approximately 24 h after discontinuation of all sedatives. He was extubated on the same day and was discharged from the ICU 24 h later. After 3 weeks of in-patient rehabilitation to overcome deconditioning and generalized weakness, he was discharged home, having returned to his baseline level of function.
Seizures eventually completely subsided with a ketamine dose of 220 mg per hour. Frequent, quasi-periodic left temporal epileptiform discharges can be seen on the raw EEG in between seizures. The yellow asterisk indicates the time point on the CDSA tracing corresponding to the 10 s EEG epoch (colour figure online)
Discussion
This case confirms previous reports suggesting that ketamine may, in selected cases, terminate refractory SE which has not responded to first-line therapy.
Unlike previous reports, the immediate and lasting efficacy of ketamine was clearly demonstrated using a quantitative compressed density spectral array (CDSA) EEG tracing. CDSA was useful in facilitating communication between the neurointensivist and bedside nurse. Indeed, characteristic CDSA “spikes” caused by recurrent seizures were used to titrate the ketamine dose upwards when expert interpretation of the raw EEG was not immediately available at the bedside, thereby facilitating more rapid and complete seizure control. Use of quantitative EEG displays has been found to have reasonable sensitivity and specificity when retrospectively interpreted by neurophysiologists [15]. Comparable studies involving neurointensivists, trainees or bedside nurses have not been performed. Nevertheless, in this patient, the consistent and characteristic appearance of the seizures could be used to guide therapy.
In addition to aborting refractory SE, clinicians must also strive to minimize the deleterious implications of deep sedation. In this patient, it would have been reasonable to further escalate doses of midazolam or propofol before resorting to ketamine. However, this approach would have undoubtedly resulted in more hypotension and the need for a higher vasopressor dose, which in turn would have increased the risk of other complications, such as arrhythmias or tissue hypoperfusion. The same concern would have been encountered with use of inhalational anesthetics or earlier administration of barbiturates. Hypotension should be carefully avoided in status epilepticus, since seizures are known to affect cerebral blood flow autoregulation, and may precipitate ischemia or metabolic crisis [16]. Our case demonstrates a “vasopressor-sparing” role for ketamine in the treatment of refractory SE, which has not been well described previously (Fig. 2) [10, 12].
We used a combination of propofol, midazolam, and (eventually) ketamine, rather than completely maximizing the dose of any one drug. There is little data to guide clinicians in transitioning from one sedative agent to another in caring for patients with refractory SE. Simultaneously targeting more than one receptor type (GABAA and NMDA) may be advantageous, but has not been well studied in humans [17, 18]. Furthermore, using a combination of drugs at lower doses could theoretically help minimize the harmful effects of any one agent. For example, the potentially lethal propofol-infusion syndrome has been described at doses exceeding 50–80 μg/kg/min, especially when used for several days and given in combination with vasopressors and benzodiazepines [19–21]. Midazolam metabolites may accumulate with high-dose infusions, resulting in a prolonged effect even after it has been discontinued. In our case, the risk of these sequelae may have been attenuated by the earlier administration of ketamine.
Review of the literature identified ten articles describing the use of ketamine to treat SE, three of which involved exclusively children (Table 1) [7–14, 22, 23]. There is one adult case series with seven patients, which has been published only as an abstract [10]. Some patients have been given ketamine boluses without an infusion, which may be effective at temporarily aborting electrographic seizures, but unlikely to achieve sustained control [8, 10]. Oral, rather than intravenous, ketamine has been used for patients not mechanically ventilated [11, 14]. The majority of patients treated with ketamine have either died or had poor neurological outcomes, even though SE was successfully aborted. This is probably largely related to the severity of patients’ underlying diagnoses. However, part of the reason may also be that ketamine infusions were generally used late in the course, in some cases after several weeks in the ICU [9, 10, 13]. In animal models, increased expression of NMDA receptors occurs over a period of hours rather than days or weeks, suggesting that earlier administration of antagonists may be advantageous [6].
It is conceivable that ketamine may be relatively more effective at treating refractory SE attributable to certain conditions. For example, the effect of glutamate on NMDA receptors is thought to be an important factor in the pathophysiology of cerebral ischemia [24]. Although the underlying cause of epilepsy in our patient was cerebral palsy, there was no evidence of acute cerebral ischemia. Ketamine has been reported to be efficacious in treating seizures caused by a variety of etiologies, including (but not limited to) anoxic encephalopathy (Table 1).
The maximum reported infusion dose and duration are 7.5 mg/kg per hour and 14 days, respectively [9, 10]. Adverse effects that have been described include acute hypertension [12] and possible cerebellar atrophy [11]. In the latter case, a very large dose of ketamine was used and alternative explanations for atrophy could not be confidently ruled out [11]. Despite being implicated in the pathophysiology of SE, synaptic NMDA receptors also have an important role in normal cognition and motor function. An encephalopathy caused by antibodies blocking NMDA receptors is now well recognized, with characteristic manifestations including abnormal movements, psychosis, and even seizures [25]. Although ketamine has been used successfully in the management of refractory SE, and has been widely administered in other settings, it remains possible that excessive, prolonged pharmacological NMDA receptor antagonism may have deleterious effects. Optimal therapy should block pathological NMDA receptor function without interfering with normal activity [26].
Our case differs from much of the published literature in that ketamine was used substantially earlier (within hours of the diagnosis of SE), had immediate and sustained efficacy, and was rapidly titrated upwards using quantitative cEEG technology. Potential adverse effects of other anesthetic agents were avoided, as demonstrated by the relatively stable blood pressure and awakening within 24 h of sedatives being discontinued.
Conclusion
Prospective studies are required to clarify optimal management of refractory SE. Specifically, future studies should assess the safety and efficacy of earlier co-administration of ketamine (or other novel agents) in comparison with a more standard strategy that simply involves escalating doses of midazolam, propofol, and/or barbiturates. Comparative trials should also assess the occurrence of relevant adverse drug effects, such as hemodynamic instability.
References
Rossetti AO, Lowenstein DH. Management of refractory status epilepticus in adults: still more questions than answers. Lancet Neurol. 2011;10:922–30.
Claassen J, Hiersch LJ, Emerson RG, Mayer SA. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002;43:146–53.
Goodkin HP, Yeh JL, Kapur J. Status epilepticus increases the intracellular accumulation of GABAA receptors. J Neurol. 2005;25:5511–20.
Mazarati AM, Wasterlain CG. N-methyl-d-aspartate receptor antagonists abolish the maintenance phase of self-sustaining status epilepticus in rat. Neurosci Lett. 1999;265:187–90.
Kapur J, Lothman EW. NMDA receptor activation mediates the loss of GABAergic inhibition induced by recurrent seizures. Epilepsy Res. 1990;5:103–11.
Borris DJ, Bertram EH, Kapur J. Ketamine controls prolonged status epilepticus. Epilepsy Res. 2000;42:117–42.
Walker MC, Howard RS, Smith SJ, et al. Diagnosis and treatment of status epilepticus on a neurological intensive care unit. Q J Med. 1996;89:913–20.
Kofke WA, Bloom MJ, Van Cott A, Brenner RP. Electrographic tachyphylaxis to etomidate and ketamine used for refractory status epilepticus controlled with isoflurane. J Neurosurg Anesthesiol. 1997;9:269–72.
Sheth RD, Gidal BE. Refractory status epilepticus: response to ketamine. Neurology. 1998;51:1765–6.
Nathan B, Smith TL, Bleck TB. The use of ketamine in the treatment of refractory status epilepticus. Neurology. 2002;3:A197.
Ubogu EE, Sagar SM, Lerner AJ, et al. Ketamine for refractory status epilepticus: a case of possible ketamine-induced neurotoxicity. Epilepsy Behav. 2003;4:70–5.
Pruss H, Holtkamp M. Ketamine successfully terminates malignant status epilepticus. Epilepsy Res. 2008;82:219–22.
Hsieh CY, Sung PS, Tsai JJ, Huang CW. Terminating prolonged refractory status epilepticus using ketamine. Clin Neuropharm. 2010;33:165–7.
Yeh PS, Shen HN, Chen TY. Oral ketamine controlled refractory nonconvulsive status epilepticus in an elderly patient. Seizure. 2011;20:723–6.
Stewart CP, Otsubo H, Ochi A, et al. Seizure identification in the ICU using quantitative EEG displays. Neurology. 2010;75:1501–8.
Ko SB, Ortega-Gutierrez S, Choi HA, et al. Status epilepticus-induced hyperemia and brain tissue hypoxia after cardiac arrest. Arch Neurol. 2011;68:1323–6.
Stewart LS, Persinger MA. Ketamine prevents learning impairment when administered immediately after status epilepticus onset. Epilepsy Behav. 2001;2:585–91.
Martin BS, Kapur J. A combination of ketamine and diazepam synergistically controls refractory status epilepticus induced by cholinergic stimulation. Epilepsia. 2008;49:248–55.
Iyer VN, Hoel R, Rabinstein AA. Propofol infusion syndrome in patients with refractory status epilepticus: an 11-year clinical experience. Crit Care Med. 2009;37:3024–30.
Rossetti AO, Reichhart MD, Schaller MD, et al. Propofol treatment of refractory status epilepticus: a study of 31 episodes. Epilepsia. 2004;45:757–63.
Vasile B, Rasulo F, Candiani A, Latronico N. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med. 2003;29:1417–25.
Mewasingh LD, Skhara T, Aeby A, et al. Oral ketamine in paediatric non-convulsive status epilepticus. Seizure. 2003;12:483–9.
Kramer U, Shorer Z, Ben-Zeev B, et al. Severe refractory status epilepticus owing to presumed encephalitis. J Child Neurol. 2005;20:184–7.
Rossi DJ, Oshima T, Attwell D. Glutamate release in severe brain ischaemia is mainly be reversed uptake. Nature. 2000;403:316–21.
Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7:1091–8.
Benarroch EE. NMDA receptors: recent insights and clinical correlations. Neurology. 2011;76:1750–7.
Acknowledgment
The author acknowledges Dr. Neelan Pillay, who assisted with timely cEEG interpretation in this patient.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kramer, A.H. Early Ketamine to Treat Refractory Status Epilepticus. Neurocrit Care 16, 299–305 (2012). https://doi.org/10.1007/s12028-011-9668-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9668-7