Abstract
Introduction
Treatment of elevated blood pressure after acute intracerebral hemorrhage (ICH) is controversial. There is a risk of hematoma expansion with elevated blood pressure, and risk of ischemia with blood pressure control. This study was done to determine the effect of blood pressure control on outcome.
Methods
We retrospectively studied 122 patients with ICH. We collected 24-h blood pressure readings on all patients. The Glasgow Coma Score (GCS) at baseline and at 24 h was used to determine neurological deterioration (GCS decline ≥ 2). Baseline computerized tomography (CT) scans were reviewed for hematoma volume, intraventricular hemorrhage, and location of hemorrhage. Drops in systolic blood pressure and mean arterial pressures over 24 h were divided in quartiles to determine the risk of neurological deterioration among quartiles. A logistic regression model was used to determine the association between variables of interest and neurological deterioration.
Results
Neurological deterioration was observed in 12 patients (10%). Baseline blood pressure and GCS were only two variables significantly different among quartiles of blood pressure drop. Multivariable adjusted analysis for these variables demonstrated significant trend toward reduced neurological deterioration with maximum blood pressure drop (systolic or mean). The risk of neurological deterioration was significantly lower in the quartile of maximum drop of systolic (odds ratio [OR] 0.02, 95% confidence interval [CI] 0.0–0.68) or mean (OR 0.03, 95% CI 0.0–0.98) blood pressure when compared to the quartile with least drop.
Conclusion
This study supports that reduction of blood pressure in patients with acute ICH is safe and suggests that aggressive reduction might reduce the risk of neurological deterioration in first 24 h of admission.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients presenting to an emergency department with intracerebral hemorrhage (ICH), 27% have a systolic blood pressure (SBP) of 160 mmHg or greater [1]. The treatment of acute hypertension in patients with ICH is highly controversial [2]. There is concern for perihematomal ischemia with reduction of blood pressure (BP) [2] and persistently elevated BP may increase the risk of hematoma expansion after acute ICH [3–7]. No Phase III clinical trials have studied the differential safety or efficacy of treatment strategies for elevated blood pressure in acute ICH. American Heart Association guidelines recommend blood pressure control if SBP is more than 180 mmHg or mean arterial pressure (MAP) is more than 130 mmHg [8].
In Neurosciences Critical Care Unit (NSU) at University Hospitals of Cleveland, elevated BP is controlled in all patients with ICH. The goal is to bring the systolic BP to less than 160 mmHg, but there remains variability in achieving this goal. In addition, because of a wide spectrum of baseline BP in these patients, the amount of BP drop compared to baseline was even more variable. This provided us with the opportunity to study the effect of amount of BP drop on neurological deterioration.
Methods
Patient Selection
We used the International Classification of Diseases, 9th revision (ICD-9) code 431 to identify the patients with ICH admitted to University Hospitals Case Medical Center in Cleveland, OH from May 1997 to July 2001. We excluded patients with the following characteristics: Glasgow Coma Score (GCS) < 5, withdrawal of care on admission, surgical hematoma evacuation within 24 h of admission, onset of symptoms >24 h before arrival to the NSU, or insufficient BP readings. This study was approved by the local IRB.
Data Collection
We collected demographic factors including age, gender, and race; and baseline clinical risk factors including hypertension, diabetes mellitus, smoking status, alcohol use, and anticoagulation medication.
Two physicians (JIS and TR) retrieved and reviewed head computerized tomography (CT) scans (baseline only) for all patients. In addition to confirmation of the diagnosis of ICH, the parameters collected include hematoma volume (in cm3), intraventricular hemorrhage (as absent or present), hydrocephalus, location of hematoma (cerebral hemisphere, brainstem, or cerebellar), and midline shift (pineal in mm).
All patients with ICH were admitted to the NSU and had hourly BP recorded in the nursing flow sheet either from cuff or arterial line values. In addition, NSU protocol included hourly documentation of neurological examination, and control of BP (SBP < 160 mmHg). The first BP recording on arrival to the NSU was chosen as baseline BP for this study, because any treatment for BP before that was not according to any protocol and varied among the emergency medical service staff or emergency room physicians. For this study, arterial line readings were preferred over cuff pressure readings and were used if recordings were available for full 24 h. When arterial line readings were not available for full 24 h, cuff pressure readings were used as a substitution after establishment of concordance between the two methods. An arbitrary criterion of a difference of less than 10 mmHg of SBP on all simultaneous readings was used to establish concordance between the two methods. BP readings might be missing if the patient was off the floor (e.g., transport of patients to radiological studies). If the total number of BP readings was less than 12, then those patients were excluded from the analysis.
To demonstrate safety in BP reduction, minimum BP was considered to be the point of maximum risk. Since the minimum blood pressure would have different impact based on the baseline pressure, we used maximum drop in BP as the marker of interest. There are no data to suggest either SBP or MAP as a better measure for management of BP after ICH. The American Heart Association guidelines [8] recommend management based on both parameters (SBP < 180, MAP < 130). We studied the association of both SBP and MAP with neurological deterioration. The drop in SBP and MAP was defined as the difference between the baseline pressure reading (on arrival to the NSU) and the minimum reading recorded in 24 h (after arrival to NSU). As there is no standard criterion for clinically significant drop of BP, to analyze the association between BP drop and neurological deterioration, we divided the BP into four quartiles. The use of multilevel classification also allows exploration of the shape of the association, and avoids the problem of non-linear association. It is also more robust to outliers when compared to linear trend.
The baseline GCS was retrieved from admission notes. Physician’s daily notes and nursing flow-sheets were used for 24-h GCS. Neurological deterioration was defined as a decrease in GCS of ≥2 points at 24 h compared to the baseline GCS. Our definition of neurological deterioration conforms with what has been previously reported [9]. Because a minimum drop of GCS of 2 points was used as a threshold, patients with GCS of 3 or 4 were excluded.
Statistical Analysis
The trajectory in BP during 24 h was analyzed with a linear mixed model using an autoregressive correlation structure [10] to identify the shape of the association and time to maximum decline and whether individual trajectories are significantly different from each other. The significance of maximum drop was analyzed using a paired sample t-test. We used analysis of variance (F-test) for comparison of means (continuous variables) and the chi-square method (categorical variables) for comparison of risk factors for neurological deterioration among different categories of BP drop. All values are expressed as means ± standard deviations. We used a generalized linear model with logit transformation and binomial distribution using the generalized estimating equation method [11] to account for multiple admissions per patient to study the effect of drop in BP as quartiles on neurological deterioration, unadjusted and adjusted for other neurological deterioration risk factors. Variables considered as risk factors were age, gender, intraventricular hemorrhage, volume of hematoma, baseline GCS, and baseline SBP or MAP. Adjusted models only included the most important predictors associated with levels of SBP/MAP drop because of the small number of patients with neurological deterioration. Associations of quartiles BP with neurological deterioration are expressed as odds ratios with the first quartile as reference. Tests for trends in quartiles are presented. A P-value of less than 0.05 was considered significant. All analyses were done using SAS (9.1.3 SAS Institute Inc., Cary, NC).
Results
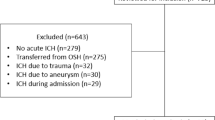
A total of 206 consecutive patients were admitted with ICH during the study period. We were unable to retrieve complete medical records for 13 patients (6%). Patients with GCS < 5 (n = 33), withdrawal of care on admission (n = 11), surgical hematoma evacuation within 24 h of admission (n = 18), onset of symptoms >24 h before arrival to the NSU (n = 4), or insufficient BP readings (n = 5) were excluded from this study. Characteristics of patients excluded from the analysis were similar to those analyzed (see Table 1).
A total of 122 patient-visits were included in the analysis. The patients’ mean age was 69.5 ± 13.2 years and 58 of them (48%) were men. Four patients were admitted with ICH on multiple occasions (3 patients on two occasions and 1 patient on three occasions). Neurological deterioration was seen in 12 patient-visits (10%). The most likely causes of neurological deterioration, as recorded in the medical records, were hydrocephalus in 2 patients; ICH growth in 4 patients; fever in 4 patients; and seizures in 2 patients. Mean baseline SBP and MAP were 169 ± 28 and 112 ± 20 mmHg, respectively. Median time to first BP recording from symptom onset for the entire cohort was 6 h (range 2–6). There was no difference in the median time to first BP recording among the 4 quartiles for either SBP or MAP analyses (Tables 2 and 3).
The trajectory of SBP and MAP followed a quadratic function, with a P-value for the quadratic term of <0.001 for SBP and MAP, and individual trajectories were significantly different from each other (P-value < 0.0001) (see Figs. 1 and 2). The minimum value, based on the quadratic function for SBP, was 148 mmHg, and for MAP it was 95 mmHg at 15.2 h and 14.9 h after admission, respectively. There was a significant absolute drop in both SBP and MAP from baseline (P < 0.05). Mean minimum values for SBP and MAP were 122 ± 18 and 78 ± 12 mmHg, respectively.
Clinical baseline characteristics of patients in relation to quartiles of SBP drop are shown in Table 2. There was no significant difference in these characteristics among SBP quartiles except for SBP at baseline (P < 0.0001). Similarly, Table 3 demonstrates the clinical characteristics of patients in relation to quartiles of MAP drop. Again, there was no significant difference in baseline characteristics among MAP quartiles, except for MAP at baseline (P < 0.0001).
In univariable analysis, there was no association or trend between SBP or MAP drop-quartiles with neurological deterioration (see Tables 4 and 5 for crude odds ratios). In multivariable analysis, adjusting for baseline GCS and baseline SBP, there was a significant negative trend between SBP drop-quartiles and neurological deterioration (P = 0.047) and a significant decrease of risk in the quartile with maximum SBP drop (≥64 mmHg) compared to the quartile with minimum SBP drop (see Tables 4 and 5 for odds ratios). Similarly, there was a significant negative trend between MAP drop-quartiles and neurological deterioration (P = 0.04) and significant decrease of risk between the maximum and minimum MAP drop-quartiles.
Discussion
Our results suggest that there is trend toward reduced risk of neurological deterioration with higher drop in either SBP or MAP independent of baseline SBP or MAP. The risk of neurological deterioration after ICH is reduced in patients with a drop in SBP of ≥65 mmHg or a drop in MAP of ≥40 mmHg within 24 h of admission.
Previous studies have investigated the association between reduction of BP and hospital mortality. Two studies have reported improved mortality with reduction of elevated BP in patients with acute ICH. In 1962 Meyer and Bauer [12] published a prospective, nonrandomized, unblinded trial of reduction of BP with hypotensive drugs in 167 subjects with ICH. There was improved mortality in patients who received hypotensive drugs but the study was limited because of the fact that the treatment group was less severely affected as compared with the untreated group at presentation (93% of untreated patients were semicomatose or comatose as compared with 76% of the treated group). Dandapani et al. [13] retrospectively studied BP control within the first 2–6 h after presentation and reported improved mortality and morbidity with BP reduction. However, this study did not consider important variables such as hematoma volume, intraventricular hemorrhage, and initial GCS score. In a prospective study, Qureshi et al. [14] observed that a rapid decline in MAP within 24 h after acute ICH is associated with increased mortality. Recently, Qureshi et al. [15] prospectively studied the outcome in 27 patients with acute ICH when SBP and Diastolic BP were targeted below 160 and 100 mmHg, respectively. The rate of neurological deterioration at 24 h was not noted to be high (7.4%) compared to historical controls.
Although our study is similar to the prospective trial by Qureshi et al. [15], in terms of target BP control and outcome, since we collected retrospective data, our sample size is much larger. This study is different from other previous studies in that we investigated the deterioration in neurological status in the hyperacute setting rather than hospital mortality as an outcome. The effect of reduction in BP on hospital mortality may be confounded by other clinical factors during hospital stay. Using the 24-h GCS limits the possibility of other medical or neurological complications. Also, we speculate that the main risk of reduction in BP is ischemic injury and is more likely to be reflected in immediate GCS rather than in hospital mortality. Pilot phases of two major trials have been completed and preliminary results suggest no significant neurological deterioration with blood pressure control. Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT) [16] randomized 404 patients with SBP between 150 and 220 mmHg within 6 h of ICH into SBP of <180 mmHg and <140 mmHg goal groups. There was no difference in neurological deterioration at 72 h between the two groups. The Antihypertensive Treatment in Acute Cerebral Hemorrhage (ATACH) [17] trial enrolled 58 patients in 3 tiers. The target blood pressure for three tiers was SBP 170–200, 140–170, and 110–140 mmHg and neurological deterioration was seen in 1, 2, and 3 patients, respectively.
In the present study, we found no increased risk of neurological deterioration with marked reduction of BP, and observed better neurological outcome with such practice. These results suggest that the possible risk of ischemia, if present, may be clinically insignificant. The theory of perihematoma ischemia has been challenged by both human and animal studies measuring cerebral blood flow (CBF). Powers et al. [18] measured regional CBF with positron emission tomography (PET) using an [15] O tracer in 14 patients with acute ICH and demonstrated that reduction in MAP from 143 ± 10 to 119 ± 11 mmHg had no significant change in either global or periclot CBF. Powers et al. calculated that there is less than a 5% chance that global or periclot CBF will fall by more than −2.7 ml/100 g/min. Qureshi et al. [19] studied the effect of MAP reduction on periclot CBF after experimental introduction of ICH in a canine model. CBF was measured using radio-labeled microspheres and was repeated after MAP reduction. The reduction in MAP was not accompanied by any significant differences in regional CBF.
Hematoma enlargement is the main cause of neurological deterioration after ICH [20, 21]. Previous studies have associated high blood pressure with hematoma enlargement [3–7]. In the INTERACT pilot trial, the rate of substantial growth was reduced in patients whose blood pressure was more aggressively lowered (P = 0.05). We did not study hematoma enlargement, but a reduced rate of hematoma enlargement is a possible explanation of better outcomes observed in patients with maximum blood pressure drops in our study.
Our study has several potential limitations. It is retrospective and may not be free from bias in data collection or patient selection. The baseline BP was taken on admission to the NSU rather than on arrival to the emergency room. Since most of the patients with ICH have hematoma expansion within the first 24 h [3, 21] we tried to limit this group by eliminating patients who did not reach NSU within 24 h of symptom onset. However, there is the possibility that a number of patients may have had hematoma expansion and neurological deterioration before the baseline examination. This will limit the patients’ benefiting from BP reduction. Additionally, due to the lack of serial exams, the neurological deterioration was established from a 24-h exam and not correlated to the time of maximum drop in BP.
This study supports that reduction of blood pressure in patients with acute ICH is safe and suggests that aggressive reduction might reduce the risk of neurological deterioration in first 24 h of admission.
References
Qureshi AI, Ezzeddine MA, Nasar A, et al. Prevalence of elevated blood pressure in 563704 adult patients with stroke presenting to the ED in the United States. Am J Emerg Med. 2007;25:32–8.
Powers WJ. Acute hypertension after stroke: the scientific basis for treatment decisions. Neurology. 1993;43:461–7.
Broderick JP, Brott TG, Tomsick T, Barsan W, Spilker J. Ultra-early evaluation of intracerebral hemorrhage. J Neurosurg. 1990;72:195–9.
Chen ST, Chen SD, Hsu CY, Hogan EL. Progression of hypertensive intracerebral hemorrhage. Neurology. 1989;39:1509–14.
Kazui S, Naritomi H, Yamamoto H, Sawada T, Yamaguchi T. Enlargement of spontaneous intracerebral hemorrhage. Incidence and time course. Stroke. 1996;27:1783–7.
Ohwaki K, Yano E, Nagashima H, Hirata M, Nakagomi T, Tamura A. Blood pressure management in acute intracerebral hemorrhage: relationship between elevated blood pressure and hematoma enlargement. Stroke. 2004;35:1364–7.
Maruishi M, Shima T, Okada Y, Nishida M, Yamane K. Involvement of fluctuating high blood pressure in the enlargement of spontaneous intracerebral hematoma. Neurol Med Chir. 2001;41:300–5.
Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American heart association/American stroke association stroke council, high blood pressure research council, and the quality of care and outcomes in research interdisciplinary working group: the American academy of neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38:2001–23.
Mayer SA, Sacco RL, Shi T, Mohr JP. Neurological deterioration in noncomatose patients with intracerebral hemorrhage. Neurology. 1994;44:1379–84.
Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer; 2000.
Diggle P. Analysis of longitudinal data. 2nd ed. Oxford/New York: Oxford University Press; 2002.
Meyer JS, Bauer RB. Medical treatment of spontaneous intracranial hemorrhage by the use of hypotensive drugs. Neurology. 1962;12:36–47.
Dandapani BK, Suzuki S, Kelley RE, Reyes-Iglesias Y, Duncan RC. Relation between blood pressure and outcome in intracerebral hemorrhage. Stroke. 1995;26:21–4.
Qureshi AI, Bliwise DL, Bliwise NG, Akbar MS, Uzen G, Frankel MR. Rate of 24-hour blood pressure decline and mortality after spontaneous intracerebral hemorrhage: a retrospective analysis with a random effects regression model. Crit Care Med. 1999;27:480–5.
Qureshi AI, Mohammad YM, Yahia AM, et al. A Prospective multicenter study to evaluate the feasibility and safety of aggressive antihypertensive treatment in patients with acute intracerebral hemorrhage. J Intensive Care Med. 2005;20:34.
Anderson C. The Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT): results of the Vanguard Phase. In: International stroke conference. New Orleans, Louisiana; 2008.
Qureshi AI. Acute blood pressure management—the North American perspective: insights from the ATACH trial. In: International stroke conference. New Orleans, Louisiana; 2008.
Powers WJ, Zazulia AR, Videen TO, et al. Autoregulation of cerebral blood flow surrounding acute (6 to 22 hours) intracerebral hemorrhage. Neurology. 2001;57:18–24.
Qureshi AI, Wilson DA, Hanley DF, Traystman RJ. Pharmacologic reduction of mean arterial pressure does not adversely affect regional cerebral blood flow and intracranial pressure in experimental intracerebral hemorrhage. Crit Care Med. 1999;27:965–71.
Leira R, Davalos A, Silva Y, et al. Early neurologic deterioration in intracerebral hemorrhage. Predictors and associated factors. Neurology. 2004;63:461–7.
Brott T, Broderick J, Kothari R, et al. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997;28:1–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suri, M.F.K., Suarez, J.I., Rodrigue, T.C. et al. Effect of Treatment of Elevated Blood Pressure on Neurological Deterioration in Patients with Acute Intracerebral Hemorrhage. Neurocrit Care 9, 177–182 (2008). https://doi.org/10.1007/s12028-008-9106-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-008-9106-7