Abstract
Dermoid cysts are the most common teratomatous lesion; however, they infrequently arise in the head and neck region. Very rarely, dermoid cysts have been described in the thyrohyoid region, masquerading as a thyroid nodule. We describe the case of a 31-year-old woman with a lateral neck mass, associated with the thyroid gland inferiorly, which was excised and found to be a dermoid cyst. We then review the pathogenesis of dermoid cysts in this region, as well as review diagnosis and treatment of dermoid cysts of the head and neck.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dermoid cysts are teratomatous lesions comprised of both ectodermal and mesodermal elements, including epithelium and adnexal structures, such as hair follicles and sebaceous glands. Only 7 % of dermoid cysts arise in the head and neck region. In the neck, these lesions are typically midline and located in the floor of mouth or submandibular region. Lateral cervical dermoids have been reported, typically between the mylohyoid and hyoglossus muscles. Dermoid cysts arising in the thyrohyoid region are exceedingly rare. Ours is the case of a 31-year-old woman with a slowly enlarging lateral cervical cyst associated with the inferior thyroid gland, originally diagnosed as a thyroid nodule. On surgical excision, the patient was found to have a large cystic mass with inflammatory changes adherent to the inferior aspect of the right thyroid lobe. Histologic analysis confirmed a diagnosis of dermoid cyst. There is controversy surrounding the pathogenesis of thyrohyoid dermoid lesions; however, definitive treatment, as with other dermoids of the head and neck, remains surgical excision.
Case Report
A 31-year-old woman of Moroccan descent presented to our institution with a 3-year history of right-sided thyroid nodules. The largest thyroid nodule continued to grow in size and the patient became symptomatic, with increased right neck fullness and dysphagia. Real-time ultrasound of the neck demonstrated a markedly hypoechoic, avascular mass in the right thyroid lobe, measuring greater than 5 cm in length, which extended superiorly towards the cephalad portion of the lobe (Fig. 1). This nodule was not obviously cystic, in that there was no posterior rim enhancement, and the echotexture suggested a solid thyroid mass.
She underwent several ultrasound-guided fine needle aspiration biopsies (FNA) of the largest nodule (the other nodules were <1 cm) and fluid could not be aspirated on either occasion. The first biopsy was non-diagnostic and the second was suggestive of a branchial cleft cyst abnormality. MRI imaging was performed, which demonstrated a large cystic mass in the right neck associated with the inferior aspect of the thyroid gland, deep to the sternocleidomastoid and strap muscles, and anteromedial to the great vessels. The mass was bordered by the anterior belly of the digastric muscle superiorly and extended just past the cricoid cartilage inferiorly (Fig. 2). The mass was isointense to muscle on T1-weighted imaging, hyperintense on T2-weighted imaging, and no enhancement was noted with contrast administration. On fat suppressed images, the mass demonstrated a reduction in signal (Fig. 3).
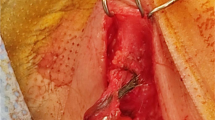
Due the patient’s symptoms and previously non-diagnostic FNA results, the patient was brought to the operating room for neck exploration and cyst excision with possible right hemithyroidectomy. The neck soft tissues and strap muscles were incised in the typical fashion in preparation for hemithyroidectomy. Lateral to the thyroid gland, a large, thin-walled cystic mass was encountered, roughly 8 × 3 cm in size. The mass appeared distinct from the thyroid gland and was carefully dissected from surrounding tissue. Inferiorly, there were inflammatory changes and adhesions between the mass and the inferior aspect of the right thyroid lobe, which was excised with the specimen. At several times the cyst wall was violated, yielding thick, white, waxy-appearing contents. The mass was removed completely and sent for pathologic analysis. The patient had an uneventful postoperative course and continues to do well without signs of recurrence or infection.
Grossly, the specimen was a 5.0 × 3.0 × 1.8-cm multi-lobulated aggregate of tan/white soft tissue with focal hemorrhage. On section, there was a 2.1-cm cystic mass with pasty contents and a smooth cyst wall. This cyst was located alongside unremarkable appearing thyroid tissue that was characteristically red/brown and heterogeneous.
Microscopically, the cyst (C) was located immediately adjacent to normal follicular thyroid tissue (T), separated by a thin rim of fibrous tissue (Fig. 4a). The cyst lining was comprised of stratified squamous epithelium (arrows, Fig. 4a, b), variably attenuated or hyperkeratotic, with abundant, centrally desquamated keratin debris (C). Additionally, the cyst wall (Fig. 4b) showed mature skin elements, including developing hair follicles (asterisk) and abundant sebaceous glands (S). As the lesion was surrounded by perithyroidal connective tissue unaffiliated with the overlying skin surface, these elements appear inherent to the lesion. A diagnosis of dermoid cyst was made.
a In this image (×20, H&E), the hyperkeratotic stratified squamous cyst lining (arrow) shows keratotic cyst contents (c). The cyst is adherent to adjacent normofollicular thyroid tissue (T) with no diagnostic abnormality. b This H&E (×100) image shows the epithelial and stromal components of the cyst, with the surface hyperkeratotic squamous epithelium (arrows), cyst contents (c), and adnexal sebaceous glands (S), and hair follicle bud (asterisk)
Discussion
Epidermoid and dermoid cysts, as well as teratomas, arise from primordial germ cell tissue (mesoderm, ectoderm, and/or endoderm). Epidermoid cysts contain only ectodermally derived elements, while dermoid cysts and teratomas are derived from more than one germ cell layer. Dermoid cysts contain both mesodermal and ectodermal components, and teratomas contain derivatives from all three germ cell tissues. Dermoid cysts contain skin and adnexal structures, such as sebaceous and nonsebaceous sweat glands, hair follicles, hair and connective tissue [1]. They may be cystic, containing keratinized debris, or arise in solid form.
Dermoid cysts are the most common teratomatous lesion, arising in up to 1 in 4,000 births; however, only 7 % of these lesions occur within the head and neck [2]. The most common sites in the head and neck include the periorbital region, nose, scalp, and submental region. When dermoids do appear in the neck, they are typically midline involving the floor of mouth. Lateral neck dermoid cysts rarely occur and usually are found in the submandibular region between the hyoglossus and mylohyoid muscles [3]. These lesions displace the submandibular gland anterolaterally and may appear dumbbell shaped as they pass through or behind the mylohyoid sling [3].
The incidence of lateral dermoid cysts arising in the thyrohyoid region of the neck is exceedingly rare [4]. These cysts may be confused with a cold thyroid nodule or a thyroglossal duct cyst [1, 4, 5]. This is the first report of a dermoid cyst presenting as a thyroid nodule in an adult.
Controversy exists regarding the origin of lateral cervical dermoid cysts. It is unclear if lateral cervical dermoids represent true lateral cysts or midline cysts that have migrated laterally as they expand [3, 6]. Several theories have been proposed to explain the pathogenesis of dermoid cysts in the thyrohyoid region. (1) Sequestral variant: In 1937, New and Erich proposed that dermoid cysts may arise congenitally, as germinal cell layers become entrapped within embryonic fusion planes. Dermoids within the thyrohyoid region may result from germinal cell layers that become included in mid-ventral and mid-dorsal fusion planes in the thyroidal or suprasternal regions [1]. (2) Thyroglossal duct variant: In 1987, deMello et al. examined 75 cases of presumed thyroglossal duct cyst abnormalities and found that 11 of these cases were actually dermoid cysts, containing only skin and its appendages. Six cases were “mixed” lesions, containing both adnexal structures as well as an epithelial tract associated with follicular thyroid tissue. Based on these histologic findings, deMello proposed that dermoid cysts in the thyrohyoid region arise from totipotent progenitor cells that become entrapped as the thyroglossal duct descends inferiorly from the base of tongue during embryogenesis [7]. However, unlike in our patient, these lesions were located in the midline, and 9 out of 11 of them were associated with the hyoid bone. Finally, (3) Acquired variant: it has been proposed that ectopic dermoid cysts result from traumatic implantation of skin into deeper tissues during a traumatic event [1] or, perhaps, when a hematoma stimulates adjacent sweat glands to proliferate [8]. Our patient had no history of cervical lacerations or trauma, making this theory unlikely in her case.
The differential diagnosis for cervical dermoid cyst includes other cystic neck masses, such as thyroglossal duct cyst and ectopic thyroid tissue, multinodular goiter, epidermal cyst, sebaceous cyst, cystic hygroma, branchial cleft cyst, lymphangioma, bronchogenic cyst, lipoma, and ranula. These can often be distinguished on the basis of location; however, infrahyoid dermoids may be incorrectly diagnosed as thyroglossal duct cyst or a thyroid nodule [1, 4, 5, 7]. Malignant lesions, such cystic squamous cell carcinoma or papillary carcinoma, are included in the differential diagnosis [2, 9].
Radiographically, dermoid cysts appear as well-defined unilocular, thin-walled cysts. Fat globules within the lesion may produce a characteristic “sac of marbles” appearance on CT imaging and fat fluid levels may also be apparent on both CT and MRI [9]. MRI allows for important soft tissue detail that may aid in diagnosis as well as perioperative and surgical planning. On MRI fat saturation technique, the fatty elements of a dermoid cyst lose their signal, as demonstrated in our patient, which is 100 % specific for diagnosis of a dermoid cyst [10].
Dermoid cysts are typically slow growing, becoming larger as sebaceous contents accumulate. There is no gender predilection. Treatment involves surgical excision along with any tract visualized leading towards the midline to prevent infection or rare malignant transformation, as well as reduce the risk of recurrence and relieve symptoms caused by expansion [6]. In the thyrohyoid region, if a tract is identified in association with or approaching the hyoid bone, a Sistrunk procedure should be considered [7]. In this case, the cyst was lateral without extension to the midline and no tract was identified, therefore the hyoid bone was left intact.
Conclusion
Dermoid cysts are the most common teratomatous lesion but rarely occur within locations of the head and neck. Infrequently, dermoid cysts may arise in association with the thyroid gland and may be misdiagnosed as a thyroid nodule or thyroglossal duct abnormality. As with dermoids in other regions of the head and neck, lesions in the thyrohyoid region should be excised completely, along with any associated tissue track to prevent recurrence.
References
McAvoy JM, Zuckerbraun L. Dermoid Cysts of the Head and Neck in Children. Arch Otolaryngol 1976; 102: 529–531.
Holt GR, Holt JE, Weaver RG. Dermoids and teratomas of the head and neck. Ear, Nose Throat J 1979; 58: 520–31.
Rosen D, Wirtschafter A, Rao VM, Wilcox TO. Dermoid cyst of the lateral neck: A case report and literature review. Ear, Nose Throat J 1998; 77(2): 129–32.
Singh N, Hollan AJA, Arbuckle S, et al. Intrathyroid dermoid cyst presenting as a unilateral “cold” nodule. Pediatr Surg In 2005; 21: 761–763.
Cox CA, Nguyen DL, Medina J et al. Dermoid cyst presenting as a “cold” thyroid nodule. Clinical Nuclear Medicine 1996; 21(5): 395.
Leveque H, Saraceno CA, Tang C et al. Dermoid cysts of the floor of the mouth and lateral neck. The Laryngoscope 1979; 89(2): 296–305.
deMello DE, Lima JA, Liapis H. Midline cervical cysts in children: thyroglossal anomalies. Arch Otolaryngol Head Neck Surg 1987; 113: 418–20.
Soni NK, Chatterji P. A massive sublingual-cervical dermoid. J Laryngol Otol 1978; 92(12): 1115–19.
Lev S, Lev MH. Imaging of cystic lesions. Radiologic Clinics of North America 2000; 38(5): 1013–1027.
Ro EY, Thomas RM, Isaacson GC. Giant dermoid cyst of the neck can mimic a cystic hygroma: Using MRI to differentiate cystic neck lesions. Int J of Pediatr Otorhinolaryngol 2007; 71: 653–658.
Conflict of Interest
There are no financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Diercks, G.R., Iannuzzi, R.A., McCowen, K. et al. Dermoid Cyst of the Lateral Neck Associated with the Thyroid Gland: a Case Report and Review of the Literature. Endocr Pathol 24, 45–48 (2013). https://doi.org/10.1007/s12022-013-9234-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-013-9234-2