Abstract
Purpose
The relationship between obstructive sleep apnea (OSA) and diabetic microvascular complications (DMC) are controversial. Whether low education is associated with increased risk of DMC independently of poor lifestyles are currently unknown. The aim of this study is to explore the independent associations of different PSG index and educational attainment with risks of DR, DKD, and DPN.
Methods
A cross-sectional study of 330 patients with T2DM who underwent overnight polysomnography (PSG) tests. Multivariable logistic regression analysis was performed to determine the associations of PSG index and educational attainments with DR, DKD, and DPN.
Results
The prevalence rates of DMC were 30.6% for DR, 24.9% for DKD, and 64.6% for DPN. All PSG index (AHI, REM-AHI, NREM-AHI, the severity of OSAS, ODI, MAI, and lowest SaO2) were not significantly associated with risks of DR, DKD, or DPN with adjustment for potential confounding factors. Subjects with increasing educational attainments showed significantly decreased prevalence rates of DR (42.6, 27.3, and 21.3%, p = 0.005), DKD (31.7, 25.3, and 14.7%, p = 0.035) and DPN (74.3, 63.6, and 53.3%, p = 0.015), respectively. Logistic regression analyses showed that educational attainment of primary or below showed significantly increased risks of DR (OR (95% CIs): 3.596 (1.453–8.899, p = 0.006)) and DKD (OR (95% CIs): 3.201 (1.244–8.242, p = 0.016)) as compared with that of college or above. There were significant trends of lower educational attainment with increased risks of DR and DKD (p values < 0.05).
Conclusion
PSG index were not significantly associated with DMC. But lower education was significantly associated with increased risks of DR and DKD, and strategies to prevent DMC for those with low education should be strengthened.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Around 10% of adults have diabetes mellitus and the prevalence rate has quadrupled in the past three decades globally. T2DM accounts for 90% of diabetes, which arouses a heavy public health burden worldwide [1, 2]. Most T2DM patients present or will develop at least one kind of diabetic complications, of which cardiovascular complications are the leading cause of morbidity and mortality for them [1, 2]. Longstanding or poorly controlled T2DM leads to the development of microvascular complications, which include retinopathy, nephropathy, and neuropathy [3]. Sleep disordered breathing (SDB) refers to a condition of repeated episodes of apnea and hypopnea during sleep due to several chronic conditions in which partial or complete cessation of breathing occurs many times throughout the night [4]. Obstructive sleep apnea (OSA), the most common form of SDB, is associated with many adverse health consequences [5]. Substantial evidence has shown that OSA is very common in T2DM patients [6]. Recent evidence has suggested a link between OSA and diabetic retinopathy (DR) [7], similar associations are also expanded to diabetic kidney disease (DKD) [8] and diabetic peripheral neuropathy (DPN) [9]. However, controversial results exit and there were significant heterogeneities regarding to OSA assessment in the evidence. For example, some studies have used polysomnography (PSG) to assess SDB while others were performed by using home sleep apnea testing which has been found to underestimate severity of OSA [10]. Therefore, further studies, especially using the more precise assessment of OSA, such as PSG, should be conducted to clarify these relationships between OSA and diabetic microvascular complications.
Educational attainment is an important indicator of socioeconomic status (SES). Education level has been found to be associated with diabetes prevalence [11], glycaemic control [12] as well as mortality in diabetes patients [13, 14]. Evidence on the association of education with diabetic microvascular complications is limited; and this is further complicated and controversial whether this relationship is independent of lifestyle habits, since lower education is related to smoking, drinking, physical inactivity and obesity [15]. Therefore, there is genuine need of more studies to clarify whether there are independent relations of education with diabetic microvascular complications.
In the present study, we firstly aimed to explore the independent association between different PSG index, such as the apnea hypopnea index (AHI), rapid eye movement AHI (REM-AHI), non-rapid eye movement AHI (NREM-AHI), the severity of obstructive sleep apnea syndrome (OSAS), oxygen desaturation index (ODI), microarousal index (MAI) as well as the lowest Oxygen saturation (SaO2), were significantly and independently associated with risks of diabetic microvascular complications (DR, DKD, or DPN) with adjustment for potential confounding factors. Secondly, we also aimed to clarify whether the associations of low education level with increased risks of diabetic microvascular complications were independent of unhealthy lifestyle habits.
Materials and methods
Patients
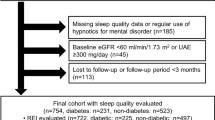
During the period from March 2013 to December 2017, a total of 346 patients with T2DM from the Department of Endocrinology and Diabetes, the First Affiliated Hospital of Xiamen University (Xiamen, China) had been recruited into the present cohort. Patients were diagnosed as diabetes based on American Diabetes Association (ADA) 2012 criteria: (1) a self-reported history of diabetes previously diagnosed by health care professionals; (2) fasting plasma glucose (FGP) ≥ 126 mg/dL (7.0 mmol/L); (3) 2-h plasma glucose (2-h PG, OGTT) ≥ 200 mg/dL (11.1 mmol/L); or (4) HbA1c ≥ 6.5% (48 mmol/mol) [16]. T2DM was identified for diabetes cases with the age of 20 years or older who are overweight or obese and/or have a family history of diabetes. Face-to-face interview was conducted for each patient to collect sociodemographic status, lifestyle habits, present and previous history of health, and medications. Patients were admitted for routine check-up evaluations and underwent detailed physical examinations and overnight PSG tests. Exclusion criteria included: the presence of hyperthyroidism or hypothyroidism; acute illnesses; heart diseases; uncontrolled hypertension; presence of cancer; craniofacial abnormalities; any respiratory disorder other than OSAS; current use of hypnotics or any treatment for breathing disorders; no diabetic microvascular complications assessments within 6 months. Of them, 330 patients who had complete data on clinical, PSG and diabetic microvascular complications measurements were left for the present analysis. This study was approved by the Human Research Ethics Committee of the First Affiliated Hospital of Xiamen University (Xiamen, China). Written informed consent was obtained from each participant.
Data collection
Subjects underwent weight, height and waist circumference measurements by using a calibrated scale after removing shoes and heavy clothes. Body mass index (BMI) was calculated as the weight in kilograms divided by the square of the height in meters. Waist circumference was measured at the midpoint between the inferior costal margin and the superior border of the iliac crest on the mid-axillary line. Arterial blood pressure (BP) was measured with OMRON electronic sphygmomanometer after sitting for at least 15 min. Three readings were taken at 5-min intervals and the mean of them was recorded.
Fasting blood samples after a 12-h overnight fasting were used to measure fasting plasma glucose (FPG), glycosylated hemoglobin A1c (HbA1c), and lipid profiles. All biochemical measurements were tested in the central laboratory of the First Affiliated Hospital, Xiamen University. Plasma glucose, liver enzyme levels, and serum lipid profiles, including triglyceride (TG), total cholesterol (TC), and high-density lipoprotein cholesterol (HDL-C) were determined on a HITACHI 7450 analyzer (HITACHI, Tokyo, Japan). Low-density lipoprotein cholesterol (LDL-C) was calculated by Friedewald’s formula. FPG concentration was measured by the hexokinase method and HbA1c by the Bio-Rad Variant Hemoglobin A1c assay.
Urinary albumin and creatinine were measured on a morning urine sample using an automatic analyser (COBAS INTEGRA 400 plus, Roche, Basel, Switzerland). Urinary albumin-to-creatinine ratio (ACR, milligram per gram) was calculated. The term of albuminuria was used to describe the increase in ACR of 30 mg/g or over. Estimated glomerular filtration rate (eGFR) was calculated using the following estimating equation, which was developed by modifying the Modification of Diet in Renal Disease equation based on the data from Chinese CKD patients [17], eGFR (mL/min/1.73 m2) = 175 × Scr (mg/dL)−1.234 × age(year)−0.179 [female × 0.79]. Reduced eGFR was defined as an eGFR < 60 mL/min/1.73 m2.
Assessments of microvascular complications
Diabetic microvascular complications were diagnosed by using the ADA diagnostic criteria. The presence of DR that encompassed simple, nonproliferative, or proliferative retinopathy was diagnosed by an experienced ophthalmologist who evaluated the optical fundi by using ophthalmoscopy or retinal photography. DKD was diagnosed based on the presence of albuminuria and/or reduced eGFR in the absence of signs or symptoms of other primary causes of kidney damage. Patients were asked for the symptoms or signs of motor, sensory, and autonomic nerves. Standard neurological examinations, including the foot sensation test using monofilament or vibration, the ankle reflex assessment and nerve conduction velocity (NCV) tests, were conducted by experienced clinicians. DPN was defined when at least two of the following symptoms presented: being insensible to 10-g Semmes–Weinstein monofilament at any of plantar sites on each foot, reduced vibration perception, absence of ankle reflex, or at least two abnormal NCV.
PSG measurements
PSG was performed using a digital polygraph on each patient (PSG, Compumedics, Abbotsford, Australia) from 11:00 pm to 7:00 am in the hospital. PSG was equipped with electroencephalogram, electrooculogram, submental electromyogram, chest and abdominal movement recording, body position monitoring, oronasal airflow monitoring, and Oxygen saturation (SaO2) and the PSG measurement was monitored by a technician [18]. Polysomnographic records were scored according to generally accepted scoring methods [19]. The recording duration > = 5 h was required for validation, and monitoring was repeated on a second night if subjective sleep latency exceeded 2 h on the first night or if respiratory parameters were missing. Lowest SaO2 was also computed. All sleep stages, arousals, and respiratory events were scored by trained technicians who were blinded to patients’ information. The reductions of airflow by more than 90 and 30% for at least 10 s were defined as apnea and hypopnea, accordingly; and the AHI was defined as the total number of apnea and hypopneas per hour of sleep [18, 19]. REM-AHI and NREM-AHI were calculated as the numbers of apneas and hypopneas during REM and NREM sleep divided by the REM and NREM sleep periods in hours, accordingly. Based on the AHI, the severity of OSAS was classified as follows: no (AHI < 5), mild (5 ≤ AHI < 15), moderate (15 ≤ AHI ≤ 30), or severe (AHI > 30). A microarousal was defined as an abrupt shift in the EEG frequency, including alpha, theta, and/or frequencies >16 Hz (but not spindles) that lasted at least 3 s, with at least 10 s of stable sleep preceding the change. The MAI was defined by the number of microarousal events per hour of recording. The ODI was defined as the number of times per sleep hour that oxygen saturation dropped by 3% or more.
Statistical analysis
Skewness and kurtosis tests for normality of AHI, REM-AHI, NREM-AHI, ODI, MAI, and sleep stages were conducted and found that these variables did not follow normal distributions. Data were presented as the mean ± standard deviation or as median (interquartile range) for continuous variable or number and percentage for categorical variable. Differences between subjects (categorized by educational attainments: primary or below, secondary, college, or above) were analyzed on continuous variables using one-way ANOVA for those with normal distribution and Kruskal–Wallis test for those with skewed distribution and on categorical variables using chi-square test.
Multivariable logistic regression was used to calculate adjusted odds ratios (OR) and 95% of educational attainment, AHI, REM-AHI, NREM-AHI, OSAS categories, ODI, MAI and lowest SaO2 for DR, DKD, and DPN separately with adjustment for age, sex, current smoking, regular drinking, BMI, systolic and diastolic BP, diabetes duration, OGLA use, Angiotensin-converting enzyme inhibitor/Angiotension receptor antagonist (ACEI/ARB) use, statin use, triglyceride, total cholesterol, HDL-cholesterol, and sleep time. AHI, REM-AHI, and NREM-AHI were presented as continuous and categorical variables (tertile 2 and tertile 3 vs. tertile 1) separately. Educational attainment was presented as categorical (secondary and primary or below vs. college or above). OSAS was also presented as categorical (mild, moderate and severe vs. no). Trend tests for educational attainment, AHI, REM-AHI, NREM-AHI, and OSAS were also conducted. All p values were two-sided and p value < 0.05 was considered statistically significant. All statistical analyses were performed using Stata14.0 (StatCorp, College Station, TX).
Results
Among the 330 patients with T2DM, 227 (68.8%) were men, and the mean ages (±SD) were 51.6 (±13.5) years for men and 55.1 (±15.4) years for women (p = 0.038). The total prevalence rates of diabetic microvascular complications were 30.6% for DR, 24.9% for DKD, and 64.6% for DPN.
Characteristics of patients stratified by educational attainment
For all subjects, the percentages of educational attainments were 30.6, 46.7, and 22.7% for primary or below, secondary, and college or above, respectively. Table 1 shows the differences of demographics and clinical characteristics stratified by educational attainments. Generally, with increasing educational attainments, patients were more likely to be male, younger, less likely to use statins, and had significantly decreased levels of systolic BP. Differences on lifestyle habits (current smoking and regular drinking), indices of obesity (BMI and waist circumference), diastolic BP, lipid profiles (triglyceride, total cholesterol, HDL-C, and LDL-C), FPG, glycosylated hemoglobin (HbA1c), disease duration, medication use (oral glucose-lowering agents (OGLA), insulin and ACEI/ARB) and PSG index (total sleep time, sleep stages, MAI, lowest SaO2, AHI, REM-AHI, NREM-AHI, OSAS categories and ODI) stratified by educational attainments were not statistically significant. As for prevalence of microvascular complications, subjects with increasing educational attainments (primary or below, secondary and college or above) showed significantly decreased prevalence rates of DR (42.6, 27.3, and 21.3%, p = 0.005), DKD (31.7, 25.3, and 14.7%, p = 0.035) and DPN (74.3, 63.6, and 53.3%, p = 0.015), respectively (Tables 2–4).
Associations of AHI and educational attainment with DR
For unadjusted ORs, compared with educational attainment of college or above, those with primary or below showed significantly increased risk of DR with OR (95% CI) of 2.734 (1.387–5.390, p = 0.004). Although educational attainment of secondary did not show significantly increased risk (OR (95% CI)) of 1.383 (0.717–2.666, p = 0.333), there was a significant trend between educational attainments and risk of DR (trend test, p = 0.002). All PSG index (AHI, REM-AHI, NREM-AHI, OSAS categories, ODI, MAI, and lowest SaO2) were not significantly associated with risk of DR. With adjustment for potential confounding factors (age, sex, current smoking, regular drinking, BMI, systolic and diastolic BP, diabetes duration, OGLA use, ACEI/ARB use, statin use, triglyceride, total cholesterol, HDL-cholesterol, and sleep time), educational attainment of primary or below was still significantly associated with increased risk of DR compared with that of college or above; and the negative association trend of educational attainment with risk of DR was still statistically significant. However, PSG index (AHI, REM-AHI, NREM-AHI, OSAS categories, ODI, MAI, and lowest SaO2) were still not significantly associated with risk of DR.
Associations of AHI and educational attainment with DKD
Similar to risk of DR, educational attainment of primary or below showed significantly increased risk of DKD as compared with that of college or above both without and with adjustment for potential confounding factors, and the unadjusted and adjusted ORs (95% CI) were 2.698 (1.256–5.798, p = 0.011) and 3.201 (1.244–8.242, p = 0.016), respectively. And there was a significantly negative trend between educational attainment and risk of DKD even after adjustment. However, there was no significant association between PSG index (AHI, REM-AHI, NREM-AHI, OSAS categories, ODI, MAI, and lowest SaO2) and risk of DKD.
Associations of AHI and educational attainment with DPN
As for risk of DPN, educational attainment of primary or below showed significantly increased risk of DPN as compared with that of college or above with the unadjusted OR (95% CI) of 2.524 (1.336–4.769, p = 0.004); however, this association became statistically non-significant with further adjustment for potential confounding factors (the adjusted OR (95% CI) of 1.489 (0.666–3.330, p = 0.332)). When compared with tertile 1 of NREM-AHI, the tertile 2 group showed significantly increased risk of DPN with the unadjusted OR (95% CI) of 2.523 (1.415–4.498, p = 0.002), but this significant association disappeared after adjustment for confoundings (the adjusted OR (95% CI) of 1.316 (0.652–2.655, p = 0.444)). The tertile 3 group did not show significant association with DPN; and there was no significant trend between increasing tertiles of NREM-AHI and risk of DPN. Although moderate OSAS, compared with no OSAS, showed increased risk of DPN (unadjusted OR (95% CI) of 2.118 (1.061–4.228, p = 0.033)), this association became statistically non-significant with adjustment for potential confounding (the adjusted OR (95% CI) of 0.772 (0.322–1.852, p = 0.563)). Neither REM-AHI nor other PSG index (AHI, ODI, MAI, and lowest SaO2) show any significant association with risk of DPN.
Discussion
In the present study of 330 patients with T2DM, we did not find any of PSG index (AHI, REM-AHI, NREM-AHI, the severity of OSAS, ODI, MAI, or lowest SaO2) was significantly and independently associated with risks of diabetic microvascular complications (DR, DKD, or DPN) with adjustment for potential confounding factors. However, we did find that educational attainment of primary or below showed significantly increased risks of DR and DKD as compared with that of college or above, although educational attainment was not independently associated with risk of DPN. Furthermore, we found there were significant trends of lower educational attainment with increased risks of DR and DKD.
Most patients with T2DM suffered from SDB, such as OSA [20]. And available evidence has shown SDB was associated with not only glycemic control but also development of microangiopathies, such as DR, in T2DM [21,22,23]. However, results of accumulating studies on the association between SDB and DR are controversial with some studies showing significant association [7, 24] while others showing no independent association [25, 26]. Moreover, not all of the previous studies have used PSG to assess SDB, and some even were performed by using home sleep apnea testing, which has been found to underestimate severity of OSA [10]. Therefore, there is increasing interest to examine associations of PSG index with DR. Nishimura et al. recently found that REM-AHI, but not NREM-AHI, was significantly and independently associated with DR based on 131 patients with T2DM [23]. They proposed that REM sleep-related OSA, rather than NREM sleep, may stimulate increased sympathetic activity during REM sleep, more oxidative stress, nitrosative stress and chronic inflammation and therefore could be a potential risk factor for DR. Meanwhile conflicting results of non-significant association between AHI and DR are increasing. Banerjee et al. found that the presence of OSA, determined by AHI, was not associated with diabetic retinal complications [25]. In the present study, we found that none of the PSG index (AHI, REM-AHI, NREM-AHI, the severity of OSAS, ODI, MAI, or lowest SaO2) was significantly and independently associated with risk of DR.
Regarding to association of OSA with DKD, another common microvascular complication of diabetes, available evidence was inconsistent. Buyukaydin et al. found that there was no significant relationship between respiratory obstructive parameters and microalbuminuria in patients with diabetes [27]. Leong et al. reported that there was a significant inverse relationship between AHI and eGFR in obese DM patients [8]. And they recently conducted a systematic review and meta-analysis and found that there was moderate evidence showing OSA was associated with DKD in DM patients, but concluded that more future studies are needed to assess the possible mechanisms between OSA and DKD [8]. The present study found that neither AHI, including REM-AHI, NREM-AHI, and the severity of OSAS, nor other PSG index (ODI, MAI, or lowest SaO2) was significantly associated with DKD, defined as the presence of albuminuria and/or eGFR <60 mL/min/1.73 m2. The only available evidence by now from prospective study showed a significant decline of eGFR in patients with T2DM and OSA [28]. We therefore suggested future studies, especially the prospective cohort studies are warranted to clarify the potential relationship and mechanisms between OSA and DKD.
DPN is characterized by pain, paraesthesia, and sensory loss, and it is estimated that around 50% of diabetes patients may develop DPN [29]. Although a few risk factors of DPN have been known, including metabolic factors such as high fat, high glucose, and low insulin, autoimmune factors producing neurotoxic inflammation, neurovascular factors resulting in damage to vessels carrying nutrients and oxygen to the nerves, and lifestyle factors such as alcohol use and smoking [30], the pathological progression and molecular mechanisms of DPN are still unclear and worthy of exploring. OSA may increase nitrosative and oxidative stress as well as insulin resistance, and may impair microvascular regulation in T2DM patients [31], which in turn could elevate inflammatory markers and contribute to microvascular complications [6]. Existing evidence suggests a possible relationship between OSA and DPN [31, 32]. Tahrani et al. found a fourfold increase of peripheral neuropathy in T2DM patients with OSA compared with those without [31]. Gu et al. recently conducted a meta-analysis based on 11 studies and found OSA was significantly associated with diabetic neuropathy with OR (95% CI) of 1.84 (1.18–2.87) [33]. However, this positive relationship was constricted only in type 1 diabetes but not in T2DM, and there was a significant heterogeneity in this meta-analysis with different assessment and classification of OSA [33]. We found the tertile 2 group of NREM-AHI, compared with the tertile 1 group, showed significantly increased risk of DPN, but this significant association disappeared after adjustment for potential confounding factors. And neither REM-AHI nor other PSG index (AHI, the severity of OSAS, ODI, MAI, and lowest SaO2) show significant association with risk of DPN.
Reasons for the null significant association between PSG index and microvascular complications of T2DM, including DR, DKD and DPN, in the present study are not clear. One possible reason was that most of our T2DM patients were obese with relatively higher AHI levels, with the prevalence of OSA in the present study of around 66%; and we may therefore underestimate the true associations of AHI with DR. But future studies, especially from the designed prospective cohort study with larger sample size, are needed to clarify the relationship and mechanisms between OSA and diabetic microvascular complications.
Substantial evidence has demonstrated that lower educational attainment is associated with higher diabetes prevalence [11] and poorer glycaemic control [12] as well as increased mortality and hospitalization [13, 14, 34] in diabetes patients. This is suggested to be due to unhealthy lifestyle, in particular a higher prevalence of obesity and physical inactivity, in those with lower level of education [15]. However, the association between educational attainment and microvascular complications in T2DM patients has been less described. Based on The Action in Diabetes and Vascular Disease: Preterax and Diamicron modified release Controlled Evaluation study, Blomster et al. found that low education was associated with increased risk of not only all-cause mortality and major cardiovascular events (defined as death from cardiovascular disease, non-fatal stroke, or non-fatal myocardial infarction) but also microvascular events (defined as new or worsening renal disease or diabetic eye disease). And these relationships consisted even with adjustment for lifestyle variables of smoking, physical activity, and alcohol use [13]. But the combined microvascular events were treated as the surrogate outcome, diabetic microvascular complications, actually including retinopathy, nephropathy, and neuropathy, have not been tested individually in the study [13]. In the present study, we found educational attainment of primary or below was significantly associated with increased risks of DR and DKD as compared with that of college or above with adjustment for all the potential confounding factors, although educational attainment was not independently associated with risk of DPN. Furthermore, we found there were significant trends of lower educational attainment with increased risks of DR and DKD. Unhealthy lifestyles, such as physical inactivity and alcohol drinking, have consistently shown to be associated with increased risks of diabetic microvascular complications [35, 36]. But this cannot be used to fully explain the associations of lower education with increased risks of diabetic microvascular complications, since lifestyle habits, such as smoking, drinking, and obesity, have been adjusted for by using multivariable logistic regression analyses in the present study. In the general clinical practice on T2DM patients in China, treatment and health education to prevent diabetic complications are commonly applied to each T2DM patients, even to their families or care-givers. Our results imply that this strategy should be strengthened especially for those with educational level of primary or below.
We should acknowledge the following limitations in the present study. The first major limitation was that most of our T2DM patients were obese with relatively higher prevalence of OSA. Around 66% of our subjects were OSA (AHI > = 5 events/h) and we may therefore underestimate the true associations of AHI with DR. Another major limitation was that our sample size might not have sufficient power to find significant associations between PSG index and diabetic microvascular complications. Therefore, a cohort with larger sample size, especially from a prospective cohort study design, should be conducted to clarify our findings in future. Third, the present study was designed as a cross-sectional study, therefore we cannot preclude the possibility of reverse causality between PSG measurements and diabetic microvascular complications.
Conclusions
Available evidence on the association of OSA and diabetic microvascular complications are limited and controversial and worthy of exploring further, especially with PSG assessment in different populations. We found that all the PSG index (AHI, REM-AHI, NREM-AHI, the severity of OSAS, ODI, MAI, and lowest SaO2) were not significantly and independently associated with risks of DR, DKD, or DPN. But more studies, especially from the designed prospective cohort study with larger sample size, are needed to clarify in future. Educational attainment of primary or below was significantly associated with increased risks of DR and DKD as compared with that of college or above and there were significant trends of lower educational attainment with increased risks of DR and DKD. These findings were not fully explained by unhealthy lifestyle habits for those with lower education attainments, and strategies to prevent incidence and progression of diabetic microvascular complications for them, beyond the general clinical practices, should be developed and strengthened.
References
Y. Zheng, S.H. Ley, F.B. Hu, Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14(2), 88–98 (2018)
A. Menke, S. Casagrande, L. Geiss, C.C. Cowie, Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 314(10), 1021–1029 (2015)
W.M. Valencia, H. Florez, How to prevent the microvascular complications of type 2 diabetes beyond glucose control. BMJ 356, i6505 (2017)
T. Young, M. Palta, J. Dempsey, J. Skatrud, S. Weber, S. Badr, The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med 328(17), 1230–1235 (1993)
T. Young, L. Finn, P.E. Peppard, M. Szklo-Coxe, D. Austin, F.J. Nieto, R. Stubbs, K.M. Hla, Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31(8), 1071–1078 (2008)
S. Nannapaneni, K. Ramar, S. Surani, Effect of obstructive sleep apnea on type 2 diabetes mellitus: a comprehensive literature review. World J. Diabetes 4(6), 238–244 (2013)
Q.A. Altaf, P. Dodson, A. Ali, N.T. Raymond, H. Wharton, H. Fellows, R. Hampshire-Bancroft, M. Shah, E. Shepherd, J. Miah, A.H. Barnett, A.A. Tahrani, Obstructive sleep apnea and retinopathy in patients with type 2 diabetes. A longitudinal study. Am. J. Respir. Crit. Care Med 196(7), 892–900 (2017)
W.B. Leong, F. Jadhakhan, S. Taheri, G.N. Thomas, P. Adab, The association between obstructive sleep apnea on diabetic kidney disease: a systematic review and meta-analysis. Sleep 39(2), 301–308 (2016)
H. Shen, J. Zhao, Y. Liu, G. Sun, Interactions between and shared molecular mechanisms of diabetic peripheral neuropathy and obstructive sleep apnea in type 2 diabetes patients. J. Diabetes Res 2018, 3458615 (2018)
M.T. Bianchi, B. Goparaju, Potential underestimation of sleep apnea severity by At-home kits: rescoring in-laboratory polysomnography without sleep staging. J. Clin. Sleep. Med 13(4), 551–555 (2017)
G.R. Dagenais, H.C. Gerstein, X. Zhang, M. McQueen, S. Lear, P. Lopez-Jaramillo, V. Mohan, P. Mony, R. Gupta, V.R. Kutty, R. Kumar, O. Rahman, K. Yusoff, K. Zatonska, A. Oguz, A. Rosengren, R. Kelishadi, A. Yusufali, R. Diaz, A. Avezum, F. Lanas, A. Kruger, N. Peer, J. Chifamba, R. Iqbal, N. Ismail, B. Xiulin, L. Jiankang, D. Wenqing, Y. Gejie, S. Rangarajan, K. Teo, S. Yusuf, Variations in diabetes prevalence in low-, middle-, andhigh-income countries: results from the prospective urban and rural epidemiological study. Diabetes Care. 39(5), 780–787 (2016)
M.L. Tan, J.A. Manski-Nankervis, S. Thuraisingam, A. Jenkins, D. O’Neal, J. Furler, Socioeconomic status and time in glucose target range in people with type 2 diabetes: a baseline analysis of the GP-OSMOTIC study. BMC Endocr. Disord. 18(1), 47 (2018)
J.I. Blomster, S. Zoungas, M. Woodward, B. Neal, S. Harrap, N. Poulter, M. Marre, B. Williams, J. Chalmers, G.S. Hillis, The impact of level of education on vascular events and mortality in patients with type 2 diabetes mellitus: Results from the ADVANCE study. Diabetes Res Clin. Pr. 127, 212–217 (2017)
H. Vandenheede, P. Deboosere, A. Espelt, M. Bopp, C. Borrell, G. Costa, T.A. Eikemo, R. Gnavi, R. Hoffmann, I. Kulhanova, M. Kulik, M. Leinsalu, P. Martikainen, G. Menvielle, M. Rodriguez-Sanz, J. Rychtarikova, J.P. Mackenbach, Educational inequalities in diabetes mortality across Europe in the 2000s: the interaction with gender. Int J. Public Health 60(4), 401–410 (2015)
T.A. Lakka, J. Kauhanen, J.T. Salonen, Conditioning leisure time physical activity and cardiorespiratory fitness in sociodemographic groups of middle-ages men in eastern Finland. Int J. Epidemiol. 25(1), 86–93 (1996)
American Diabetes Association. Stand. Med. Care Diabetes - 2012 Diabetes Care 35(Suppl 1), S11–S63 (2012)
Y.C. Ma, L. Zuo, J.H. Chen, Q. Luo, X.Q. Yu, Y. Li, J.S. Xu, S.M. Huang, L.N. Wang, W. Huang, M. Wang, G.B. Xu, H.Y. Wang, Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J. Am. Soc. Nephrol. 17, 2937–2944 (2006)
R.B. Berry, R. Budhiraja, D.J. Gottlieb, D. Gozal, C. Iber, V.K. Kapur, C.L. Marcus, R. Mehra, S. Parthasarathy, S.F. Quan, S. Redline, K.P. Strohl, S.L. Davidson Ward, M.M. Tangredi; American Academy of Sleep Medicine., Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J. Clin. Sleep. Med 8(5), 597–619 (2012)
Y. Ikeda, T. Kasai, F. Kawana, S. Kasagi, H. Takaya, S. Ishiwata, K. Narui, Comparison between the apnea-hypopnea indices determined by the REMstar Auto M series and those determined by standard in-laboratory polysomnography in patients with obstructive sleep apnea. Intern Med. 51(20), 2877–2885 (2012)
G.D. Foster, M.H. Sanders, R. Millman, G. Zammit, K.E. Borradaile, A.B. Newman, T.A. Wadden, D. Kelley, R.R. Wing, F.X. Sunyer, V. Darcey, S.T. Kuna; Sleep AHEAD Research Group., Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 32(6), 1017–1019 (2009)
S. Reutrakul, B. Mokhlesi, Obstructive sleep apnea and diabetes: a state of the art review. Chest 152(5), 1070–1086 (2017)
B. Mokhlesi, D. Grimaldi, G. Beccuti, E. Van Cauter, Effect of one week of CPAP treatment of obstructive sleep apnoea on 24-hour profiles of glucose, insulin and counter-regulatory hormones in type 2 diabetes. Diabetes Obes. Metab. 19(3), 452–456 (2017)
A. Nishimura, T. Kasai, S. Kikuno, K. Nagasawa, M. Okubo, K. Narui, Y. Mori, Apnea hypopnea index during rapid eye movement sleep with diabetic retinopathy in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 104(6), 2075–2082 (2019)
A. Nishimura, T. Kasai, H. Tamura, A. Yamato, D. Yasuda, K. Nagasawa, M. Okubo, K. Narui, Y. Mori, Relationship between sleep disordered breathing and diabetic retinopathy: analysis of 136 patients with diabetes. Diabetes Res Clin. Pr. 109(2), 306–311 (2015)
D. Banerjee, W.B. Leong, T. Arora, M. Nolen, V. Punamiya, R. Grunstein, S. Taheri, The potential association between obstructive sleep apnea and diabetic retinopathy in severe obesity-the role of hypoxemia. PLoS ONE 8(11), e79521 (2013)
R. Zhang, P. Zhang, F. Zhao, X. Han, L. Ji, Association of diabetic microvascular complications and parameters of obstructive sleep apnea in patients with Type 2 diabetes. Diabetes Technol. Ther. 18(7), 415–420 (2016)
B. Buyukaydin, M.E. Akkoyunlu, R. Kazancioglu, F. Karakose, H.K. Ozcelik, R. Erkoc, L. Kart, The effect of sleep apnea syndrome on the development of diabetic nephropathy in patients with type 2 diabetes. Diabetes Res Clin. Pr. 98(1), 140–143 (2012)
A.A. Tahrani, A. Ali, N.T. Raymond, S. Begum, K. Dubb, Q.A. Altaf, M.K. Piya, A.H. Barnett, M.J. Stevens, Obstructive sleep apnea and diabetic nephropathy: a cohort study. Diabetes Care. 36(11), 3718–3725 (2013)
S. Tesfaye, D. Selvarajah, R. Gandhi, M. Greig, P. Shillo, F. Fang, I.D. Wilkinson, Diabetic peripheral neuropathy may not be as its name suggests: evidence from magnetic resonance imaging. Pain 157(Suppl 1), S72–S80 (2016)
V. Rosenfeld, Sleep dysfunction, diabetes, and pain: a troublesome triad. J. Fam. Pr. 63(6 Suppl), S18–S24 (2014)
A.A. Tahrani, A. Ali, N.T. Raymond, S. Begum, K. Dubb, S. Mughal, B. Jose, M.K. Piya, A.H. Barnett, M.J. Stevens, Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am. J. Respir. Crit. Care Med 186(5), 434–441 (2012)
Q.A. Altaf, A. Ali, M.K. Piya, N.T. Raymond, A.A. Tahrani, The relationship between obstructive sleep apnea and intra-epidermal nerve fiber density, PARP activation and foot ulceration in patients with type 2 diabetes. J. Diabetes Complicat. 30(7), 1315–1320 (2016)
X. Gu, X. Luo, X. Wang, J. Tang, W. Yang, Z. Cai, The correlation between obstructive sleep apnea and diabetic neuropathy: a meta-analysis. Prim. Care Diabetes 12(5), 460–466 (2018)
K.I. Birkeland, M.E. Jørgensen, B. Carstensen, F. Persson, H.L. Gulseth, M. Thuresson, P. Fenici, D. Nathanson, T. Nyström, J.W. Eriksson, J. Bodegård, A. Norhammar, Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. Lancet Diabetes Endocrinol. 5(9), 709–717 (2017)
J.I. Blomster, C.K. Chow, S. Zoungas, M. Woodward, A. Patel, N.R. Poulter, M. Marre, S. Harrap, J. Chalmers, G.S. Hillis, The influence of physical activity on vascular complications and mortality in patients with type 2 diabetes mellitus. Diabetes Obes. Metab. 15(11), 1008–1012 (2013)
J.I. Blomster, S. Zoungas, J. Chalmers, Q. Li, C.K. Chow, M. Woodward, G. Mancia, N. Poulter, B. Williams, S. Harrap, B. Neal, A. Patel, G.S. Hillis, The relationship between alcohol consumption and vascular complications and mortality in individuals with type 2 diabetes. Diabetes Care. 37(5), 1353–1359 (2014)
Acknowledgements
We are grateful to all the patients for their participation.
Funding
C.L. was founded by Natural Science Foundation of China grant no: 81870611. Z.L. was founded by the National Key R&D Program of China grant no: 2017YFC0907100.ML was founded by Natural Science Foundation of Fujian Province grant no: 2017J01365.
Author contributions
The study concept and design were framed by C.D., Z.L., and C.L., C.D., C.H., S.Z., L.D., W.W., C.Z., and S.W. collected data. C.D., C.H., Z.L., and C.L. conducted the statistical data analysis and drafted the manuscript. M.L., X.J., and S.Y., contributed to discussion and revision. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Chunmin Du, Chunmei He
Rights and permissions
About this article
Cite this article
Du, C., He, C., Dong, L. et al. Associations of apnea hypopnea index and educational attainments with microvascular complications in patients with T2DM. Endocrine 67, 363–373 (2020). https://doi.org/10.1007/s12020-020-02192-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02192-w