Abstract
There is little information on whether past use of oral contraceptives (OCs) at child-bearing age influences the incidences of diabetes and insulin resistance (IR) after menopause. This study aimed to evaluate the association of past use of OCs with the development of diabetes and IR in post-menopausal women. This cross-sectional study was based on data from the Korea National Health and Nutrition Examination Survey carried out from 2007 to 2012. Of the 50405 participants, 6554 post-menopausal women were included in the analysis. The associations of OC use with the prevalence of diabetes in post-menopausal women were examined using multivariate logistic analysis. In addition, fasting glucose and insulin levels were measured in 3338 nondiabetic post-menopausal women, and the association between IR and OCs was examined by the analysis of covariance. The prevalence of diabetes was significantly higher in post-menopausal participants who had taken OCs for more than 6 months than in those who had never taken OCs. The association remained significant after adjusting for multiple confounding factors (odd ratio 1.379; 95 % CI 1.115–1.707; P = 0.003). The duration of OC use was also positively associated with the prevalence of diabetes. Furthermore, taking OCs for more than 6 months led to a significant increase in fasting insulin levels and HOMA-IR in nondiabetic participants. Past use of OCs for more than 6 months led to a significant increase in the prevalence of diabetes in post-menopausal women, and increased IR in nondiabetic participants. These results suggested that the prolonged use of OCs at reproductive age may be an important risk factor for developing diabetes in post-menopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes is an increasing health burden in elderly populations worldwide due to poor glycemic control and multiple comorbidities [1–3]. In addition, the prevalence of diabetes in women is steadily increasing, and it is now a major public health concern [4, 5]. The risk of diabetes increases when women reach menopause, a critical time during which women undergo hormonal transitions [6, 7]. An epidemiological study showed that the prevalence of diabetes during young adulthood is higher in males than in females, whereas the prevalence in women increases markedly after menopause [8]. Therefore, it is necessary to identify factors that influence the development of diabetes in post-menopausal women. Although reproductive factors including the number of pregnancies, age at the time of first childbirth, and age at menopause are known to be associated with the risk of developing diabetes in later life [9–11], no study has examined the association between OC use at childbearing age and the incidence of diabetes in later life.
Worldwide, the prevalence of OC use was steadily increased in women of reproductive age [12]. These drugs alter lipid metabolism, and are associated with an increased risk of coronary heart disease [13, 14]. However, the effects of OCs on carbohydrate metabolism and insulin sensitivity have not been clearly elucidated. Many studies report that OCs do not influence glucose tolerance and insulin resistance (IR) [15, 16], and some show that OCs improve glucose control [17]. On the other hand, other studies suggest that OCs increase glucose intolerance and IR [18, 19]. However, there is no consistent evidence showing that OC use increases the incidence of diabetes. Two large-scale prospective studies evaluated whether OC use is associated with an increased incidence of diabetes [20, 21]. Chasan-Taber et al. reported no association between diabetes and current or past OC use [20]. The study by Rimm et al. had a 12-year follow-up period, and found no association between current OC use and the risk of diabetes; however, past OC use led to a marginal increase in the risk (relative risk 1.10; CI 1.01–1.21) [21]. One case–control study reported no association between OC use and the prevalence of diabetes among post-menopausal women [22], but only a small number of incident cases were examined. Therefore, there is little concrete information to show that the OC use results in the development of diabetes in later life.
Here, we examined data from the Korea National Health and Nutrition Examination Survey (KNHANES) conducted from 2007 to 2012 and investigated the association between past use of OCs at child-bearing age and the prevalence of diabetes at post-menopause. In addition, we examined the association between OC use and IR in nondiabetic post-menopausal women.
Methods
Subjects
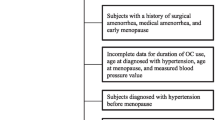
This cross-sectional study was based on data collected by KNHANES IV (2007–2009) and V (2010–2012). KNHANES is a large-scale population-based nationwide survey conducted by the Korea Centers for Disease Control and Prevention. Of the 50405 participants, 8475 were post-menopausal women. Participants with a history of early menopause (under age 40), post-surgical or medical amenorrhea (e.g., due to hysterectomy or use of intrauterine devices), or hormone replacement therapy were excluded. Participants with incomplete data regarding duration of OC use, age at the time of diabetes diagnosis, and age at menopause were also excluded. To assess the association between OC use and the incidence of diabetes after menopause, participants diagnosed with diabetes prior to menopause were excluded. This left 6554 post-menopausal women in whom the association between OC use and prevalence of diabetes was evaluated. In addition, when examining the association between IR and OC use, participants lacking data regarding fasting glucose and insulin levels were excluded from the analysis. Fasting glucose, fasting insulin, β-cell function, and IR (assessed by homeostatic model assessment (HOMA)) were measured cross-sectionally in 3338 post-menopausal women who had never used anti-diabetic medications. A flow chart showing the subject selection process is presented in Fig. 1. The KNHANES data are publicly available, and ethics approval was obtained from the Korean Centers for Disease Control & Prevention.
Measurement of biochemical and clinical variables
Blood and urine samples were collected after an 8 h fast and transported to the Neodin Medical Institute (Seoul, Korea). Serum glucose and insulin levels were measured using a Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan). HOMA-IR was calculated as follows: fasting glucose (mmol/L) × fasting insulin (µIU/L)/22.5. HOMA-β was calculated as follows: [20 × fasting insulin (µIU/L)]/[fasting glucose (mmol/L) − 3.5]. Body weight and height were measured by trained staff during the health examination, and body mass index (BMI) was calculated as weight divided by height (m2). Blood pressure (BP) was measured three times with the subject seated and using a cuff on the right arm attached to a mercury sphygmomanometer (Baumanometer; W. A. Baum, Copiague, NY, USA). The final BP was calculated as the average of the second and third readings. The glomerular filtration rate was estimated using the Modification of Diet in Renal Disease equation. Demographic and personal medical data were collected using standardized health questionnaires. These data included age at menopause, history of OC use, hormone replacement therapy, and history of diabetes, hypertension (HTN), hyperlipidemia, smoking, alcohol consumption, and physical activity.
Statistical analyses
All continuous data were expressed as the mean ± standard deviation, and all categorical data were expressed as numbers and percentages. Statistical analysis was performed using SPSS 18.0 software (SPSS Inc., Chicago, IL, USA). Demographic and clinical variables were compared using the Student’s t test and Chi-square test. Participants were divided into groups according to the duration of OC use, and the groups were compared in terms of baseline characteristics using the Student’s t- and Chi-square tests. Trends across groups were tested for significance using analysis of variance. Multivariable logistic regression models were used to estimate the prevalence of diabetes in each group. The models were adjusted for age, BMI, physical activity, heavy alcohol usage, smoking status, systolic BP, HTN, treatment of hyperlipidemia, age at menopause, and number of pregnancies. Analysis of covariance was used to estimate the mean fasting- glucose, insulin, and HOMA-IR values for each group after adjustment for multiple variables. For all statistical tests, a P value < 0.05 was considered statistically significant.
Results
General characteristics of the participants
The general characteristics of the participants are presented in Table 1. Overall, 5296 post-menopausal women had no history of OC use, whereas 1258 had used OCs in the past; 849 of these had a past history of OC use for longer than 6 months. The mean duration of OC use in this latter group was 32.1 months. Participants who used OCs were younger, taller, and heavier, and had a slightly higher BMI than participants who did not. There was no significant difference between the groups in terms of lipid profiles (total cholesterol, HDL, and triglycerides). However, significantly more participants in the OCs group had hyperlipidemia than in the non-OCs group. There was no difference in estimated glomerular filtration rate among the groups. Systolic BP was higher in women with a longer history of OC use, although there was no difference in mean diastolic BP among the groups. HTN was significantly more prevalent in the group with a longer history of OC use. The number of women with diabetes was 755 in the nonuser group, 59 in the less than 6-month user group, and 165 in the more than 6-month user group. The number of new participants diagnosed with diabetes on the basis of fasting glucose levels during surveys was 137 in non-user, ten in the less than 6-month user group, and 26 in the more than 6-month user group. Women who used OCs for longer than 6 months had a significantly higher prevalence of diabetes, and were diagnosed at a younger age. There was no significant difference in lifestyle behaviors (smoking, alcohol consumption, and physical activity) or a difference in age at menarche among groups; however, women who used OCs reached menopause at an older age and had a shorter post-menopausal period. OC users also had a greater number of pregnancies.
Association between past use of OCs and diabetes post-menopause
The odds ratios (OR) for the prevalence of diabetes in post-menopausal women according to OC use are shown in Table 2. In the unadjusted model, the odds ratio for diabetes was significantly higher for women who used OCs for more than 6 months than for women who did not use OCs. After adjusting for age, BMI, and various confounding factors (physical activity, heavy drinking, smoking status, systolic BP, HTN, hyperlipidemia, age at menopause, and number of pregnancies), the association between past use of OCs and diabetes in post-menopausal women still remained significant (model 5: OR 1.340; 95 % CI 1.099–1.634; P = 0.004). The ORs of participants who used OCs for less than 6 months were not statistically different from those of non-users. (model 5: OR, 1.041; 95 % CI, 0.771–1.405; P = 0.793).
Association between duration of OC use and prevalence of diabetes post-menopause
The association between duration of OC use and the prevalence of diabetes is shown in Table 3. In the unadjusted model, duration of OC use was positively associated with the risk of diabetes post-menopause. This association remained significant after adjusting for age, BMI, lifestyle behaviors, current medical status, and reproductive factors (model 5: OR, 1.005; 95 % CI, 1.002–1.009; P = 0.003). Thus, the risk of diabetes in post-menopausal women showed a significant increasing trend of 0.5 % per 1 month of OC use.
Association between OC use and IR in nondiabetic post-menopausal subjects
Additionally, after excluding participants for whom data regarding fasting glucose and fasting insulin levels were unavailable, we examined the association between past use of OCs and IR in nondiabetic post-menopausal women (Fig. 2; n = 3338). Fasting insulin levels in women who used OCs for more than 6 months were significantly higher than those in the other groups (Fig. 2a); however, there was no significant difference in fasting glucose levels between groups (Fig. 2b). The HOMA-IR for women who used OCs for more than 6 months was significantly higher than that for the other women (Fig. 2c). These associations were true for both the unadjusted and adjusted models.
Association between past use of oral contraceptives (OCs) and insulin resistance in nondiabetic post-menopausal women (n = 3338). Levels of fasting insulin (a), fasting glucose (b), and HOMA-IR (c). Model is adjusted for age, BMI, lifestyle behaviors (physical activity, alcohol consumption, and smoking status), current medical status (systolic BP, HTN, and hyperlipidemia), and reproductive factors (age at menopause and number of pregnancies). *P < 0.05 and † P < 0.01
Association between parity and post-menopausal diabetes
Given the increase in parity in the more than 6-month user group (Table 1), the association between number of pregnancies and the prevalence of diabetes was also estimated (Table 4). Women who had a larger number of pregnancies had significantly higher ORs for diabetes. After adjustment for multiple confounding factors including duration of OC use, the number of pregnancies was still positively associated with the prevalence of diabetes (OR = 1.046 per 1 pregnancy, CI 1.015–1.078, P = 0.003).
Discussion
Despite conflicting studies, it is generally accepted that OCs do not have a deleterious effect on glucose metabolism in healthy women. However, previous studies were conducted in relatively young women and had limited follow-up periods; therefore, the effects of OCs in later life have not been investigated. In this study, we found that the prevalence of diabetes in post-menopausal women who had used OCs for more than 6 months was significantly higher than that in women who did not use OCs. In addition, increased prevalence of diabetes was also associated with the duration of OC use. To the best of our knowledge, the present study is the first to examine the long-term effects of OC use at childbearing age on the development of diabetes after menopause.
Estrogen has been suggested to suppress gluconeogenesis in the liver which leads to lower fasting blood glucose levels [23]. In line with this, hormone replacement in post-menopausal women improves fasting glucose and insulin levels [24, 25]. The association between current OC use in premenopausal women and glucose intolerance has been investigated; however, most studies reported no association between OC use and fasting glucose and insulin levels [14–16]. Nevertheless, several studies suggest that OC use may impair glucose regulation by altering insulin sensitivity [13, 19, 26]. Intravenous glucose tolerance tests showed an increase in IR in women who had used OCs, which appeared to be primarily an effect of estrogen [18]. Another study showed that the use of OCs was associated with an increased IR, independently of the estrogen dose [27]. On the other hand, the CARDIA study, which enrolled 1940 young women, revealed that current use of OCs was associated with lower fasting glucose levels [17]. It remains to be clarified whether OC use disturbs glucose homeostasis. In addition, no study has investigated the long-term effect of OC use on glucose intolerance and IR in later life. In this study, we showed that past use of OCs for more than 6 months was significantly associated with higher fasting insulin levels and HOMA-IR in nondiabetic women. It is possible that prolonged use of OCs may lead to a higher risk of developing diabetes by increasing IR post-menopause.
In addition, several studies showed that parity is a risk factor for diabetes [11, 28]. A study of 1186 women aged 40 years or more showed that parity was positively associated with the risk of diabetes and impaired glucose tolerance [28]. However, another large prospective cohort study showed that parity was not associated with the risk of diabetes after adjustment for age and BMI [29]. Interestingly, this study showed that women with a larger number of pregnancies had significantly higher ORs of diabetes. Given that the association between OC use and diabetes was more significant after removing parity from the adjusted variables (OR, 1.340 ≥ 1.391; P value, 0.004 ≥ 0.001, data not shown), it would appear that influence of OC use on diabetes interacted with parity. In addition, parity was also positively associated with the prevalence of diabetes after adjusting for multiple variables. This association was independent of the duration of OC use.
The study has several limitations. First, the cross-sectional design meant that we were unable to identify a causal relationship between OC use and diabetes. Second, data regarding OC use and age at the time of diabetes diagnosis were collected retrospectively, which may have led to memory bias. Third, the effects of several variables (e.g., the types of OCs, age at the time of OC use, and time since ceasing OC use) that may affect glucose metabolism [30] were not examined. Fourth, although type 1 diabetes in post-menopausal women is very rare, we could not exclude latent autoimmune diabetes in adults. Fifth, several diseases that influence glucose metabolism (e.g., polycystic ovarian syndrome) [31] were not assessed as variables. Sixth, the number of OC users was smaller than that of non-users. This baseline imbalance in populations may have caused a potential bias.
In conclusion, the present study identified an association between past use of OCs and an increased prevalence of diabetes in post-menopausal women. The results suggest that the prolonged use of OCs at child-bearing age may be an important risk factor for developing diabetes in later life. Further investigation is necessary to determine the long-term effect of OCs on the risk of diabetes.
References
K.M. Narayan, J.P. Boyle, L.S. Geiss, J.B. Saaddine, T.J. Thompson, Impact of recent increase in incidence on future diabetes burden: U.S., 2005–2050. Diabetes Care 29(9), 2114–2116 (2006). doi:10.2337/dc06-1136
M.S. Kirkman, V.J. Briscoe, N. Clark, H. Florez, L.B. Haas, J.B. Halter, E.S. Huang, M.T. Korytkowski, M.N. Munshi, P.S. Odegard, R.E. Pratley, C.S. Swift, Diabetes older adults. Diabetes Care 35(12), 2650–2664 (2012). doi:10.2337/dc12-1801
E. Selvin, J. Coresh, F.L. Brancati, The burden and treatment of diabetes in elderly individuals in the U.S. Diabetes Care 29(11), 2415–2419 (2006). doi:10.2337/dc06-1058
J.E. Shaw, R.A. Sicree, P.Z. Zimmet, Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 87(1), 4–14 (2010). doi:10.1016/j.diabres.2009.10.007
E.A. Spencer, K.L. Pirie, R.J. Stevens, V. Beral, A. Brown, B. Liu, J. Green, G.K. Reeves, Diabetes and modifiable risk factors for cardiovascular disease: the prospective Million Women Study. Eur. J. Epidemiol. 23(12), 793–799 (2008). doi:10.1007/s10654-008-9298-3
H.M. Kim, J. Park, S.Y. Ryu, J. Kim, The effect of menopause on the metabolic syndrome among Korean women: the Korean National Health and Nutrition Examination Survey, 2001. Diabetes Care 30(3), 701–706 (2007). doi:10.2337/dc06-1400
C.R. Gracia, M.D. Sammel, E.W. Freeman, H. Lin, E. Langan, S. Kapoor, D.B. Nelson, Defining menopause status: creation of a new definition to identify the early changes of the menopausal transition. Menopause (New York) 12(2), 128–135 (2005)
W. Yang, J. Lu, J. Weng, W. Jia, L. Ji, J. Xiao, Z. Shan, J. Liu, H. Tian, Q. Ji, D. Zhu, J. Ge, L. Lin, L. Chen, X. Guo, Z. Zhao, Q. Li, Z. Zhou, G. Shan, J. He, Prevalence of diabetes among men and women in China. N. Engl. J. Med. 362(12), 1090–1101 (2010). doi:10.1056/NEJMoa0908292
J.S. Brand, Y.T. van der Schouw, N.C. Onland-Moret, S.J. Sharp, K.K. Ong, K.T. Khaw, E. Ardanaz, P. Amiano, H. Boeing, M.D. Chirlaque, F. Clavel-Chapelon, F.L. Crowe, B. de Lauzon-Guillain, E.J. Duell, G. Fagherazzi, P.W. Franks, S. Grioni, L.C. Groop, R. Kaaks, T.J. Key, P.M. Nilsson, K. Overvad, D. Palli, S. Panico, J.R. Quiros, O. Rolandsson, C. Sacerdote, M.J. Sanchez, N. Slimani, B. Teucher, A. Tjonneland, R. Tumino, A.D. van der, E.J. Feskens, C. Langenberg, N.G. Forouhi, E. Riboli, N.J. Wareham, Age at menopause, reproductive life span, and type 2 diabetes risk: results from the EPIC-InterAct study. Diabetes care 36(4), 1012–1019 (2013). doi:10.2337/dc12-1020
J.H. Kim, Y. Jung, S.Y. Kim, H.Y. Bae, Impact of age at first childbirth on glucose tolerance status in postmenopausal women: the 2008–2011 Korean National Health and Nutrition Examination Survey. Diabetes Care 37(3), 671–677 (2014). doi:10.2337/dc13-1784
A.G. Fowler-Brown, I.H. de Boer, J.M. Catov, M.R. Carnethon, A. Kamineni, L.H. Kuller, D.S. Siscovick, K.J. Mukamal, Parity and the association with diabetes in older women. Diabetes Care 33(8), 1778–1782 (2010). doi:10.2337/dc10-0015
L. Alkema, V. Kantorova, C. Menozzi, A. Biddlecom, National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet (London, England) 381(9878), 1642–1652 (2013). doi:10.1016/s0140-6736(12)62204-1
I.F. Godsland, D. Crook, R. Simpson, T. Proudler, C. Felton, B. Lees, V. Anyaoku, M. Devenport, V. Wynn, The effects of different formulations of oral contraceptive agents on lipid and carbohydrate metabolism. N. Engl. J. Med. 323(20), 1375–1381 (1990). doi:10.1056/nejm199011153232003
J.B. Croft, D.S. Freedman, J.L. Cresanta, S.R. Srinivasan, G.L. Burke, S.M. Hunter, L.S. Webber, C.G. Smoak, G.S. Berenson, Adverse influences of alcohol, tobacco, and oral contraceptive use on cardiovascular risk factors during transition to adulthood. Am. J. Epidemiol. 126(2), 202–213 (1987)
K.V. Porkka, R. Erkkola, S. Taimela, O.T. Raitakari, G.H. Dahlen, J.S. Viikari, Influence of oral contraceptive use on lipoprotein (a) and other coronary heart disease risk factors. Ann. Med. 27(2), 193–198 (1995)
J.A. Goldman, Intravenous glucose tolerance after 18 months on progestogen or combination-type oral contraceptive. Isr. J. Med. Sci. 14(3), 324–327 (1978)
C. Kim, D.S. Siscovick, S. Sidney, C.E. Lewis, C.I. Kiefe, T.D. Koepsell, Oral contraceptive use and association with glucose, insulin, and diabetes in young adult women: the CARDIA Study. Coronary Artery Risk Development in Young Adults. Diabetes Care 25(6), 1027–1032 (2002)
D. Crook, I. Godsland, Safety evaluation of modern oral contraceptives. Effects on lipoprotein and carbohydrate metabolism. Contraception 57(3), 189–201 (1998)
D. Simon, C. Senan, P. Garnier, M. Saint-Paul, E. Garat, N. Thibult, L. Papoz, Effects of oral contraceptives on carbohydrate and lipid metabolisms in a healthy population: the Telecom study. Am. J. Obstet. Gynecol. 163(1 Pt 2), 382–387 (1990)
L. Chasan-Taber, W.C. Willett, M.J. Stampfer, D.J. Hunter, G.A. Colditz, D. Spiegelman, J.E. Manson, A prospective study of oral contraceptives and NIDDM among U.S. women. Diabetes Care 20(3), 330–335 (1997)
E.B. Rimm, J.E. Manson, M.J. Stampfer, G.A. Colditz, W.C. Willett, B. Rosner, C.H. Hennekens, F.E. Speizer, Oral contraceptive use and the risk of type 2 (non-insulin-dependent) diabetes mellitus in a large prospective study of women. Diabetologia 35(10), 967–972 (1992)
A.D. Rosenthal, X.O. Shu, F. Jin, G. Yang, T.A. Elasy, Q. Li, H.X. Xu, Y.T. Gao, W. Zheng, Oral contraceptive use and risk of diabetes among Chinese women. Contraception 69(3), 251–257 (2004). doi:10.1016/j.contraception.2003.10.015
I.F. Godsland, The influence of female sex steroids on glucose metabolism and insulin action. J. Intern. Med. Suppl. 738, 1–60 (1996)
A. Ferrara, A.J. Karter, L.M. Ackerson, J.Y. Liu, J.V. Selby, Hormone replacement therapy is associated with better glycemic control in women with type 2 diabetes: The Northern California Kaiser Permanente Diabetes Registry. Diabetes Care 24(7), 1144–1150 (2001)
H.E. Brussaard, Gevers Leuven, J.A., Frolich, M., Kluft, C., Krans, H.M.: short-term oestrogen replacement therapy improves insulin resistance, lipids and fibrinolysis in postmenopausal women with NIDDM. Diabetologia 40(7), 843–849 (1997)
W. Oelkers, J.M. Foidart, N. Dombrovicz, A. Welter, R. Heithecker, Effects of a new oral contraceptive containing an antimineralocorticoid progestogen, drospirenone, on the renin–aldosterone system, body weight, blood pressure, glucose tolerance, and lipid metabolism. J. Clin. Endocrinol. Metabol. 80(6), 1816–1821 (1995). doi:10.1210/jcem.80.6.7775629
A. Cagnacci, S. Ferrari, A. Tirelli, R. Zanin, A. Volpe, Route of administration of contraceptives containing desogestrel/etonorgestrel and insulin sensitivity: a prospective randomized study. Contraception 80(1), 34–39 (2009). doi:10.1016/j.contraception.2009.01.012
D. Kritz-Silverstein, E. Barrett-Connor, D.L. Wingard, The effect of parity on the later development of non-insulin-dependent diabetes mellitus or impaired glucose tolerance. N. Engl. J. Med. 321(18), 1214–1219 (1989). doi:10.1056/nejm198911023211802
J.E. Manson, E.B. Rimm, G.A. Colditz, M.J. Stampfer, W.C. Willett, R.A. Arky, B. Rosner, C.H. Hennekens, F.E. Speizer, Parity and incidence of non-insulin-dependent diabetes mellitus. Am. J. Med. 93(1), 13–18 (1992)
I.F. Godsland, C. Walton, C. Felton, A. Proudler, A. Patel, V. Wynn, Insulin resistance, secretion, and metabolism in users of oral contraceptives. J. Clin. Endocrinol. Metabol. 74(1), 64–70 (1992). doi:10.1210/jcem.74.1.1530790
D.A. Ehrmann, R.B. Barnes, R.L. Rosenfield, M.K. Cavaghan, J. Imperial, Prevalence of impaired glucose tolerance and diabetes in women with polycystic ovary syndrome. Diabetes Care 22(1), 141–146 (1999)
Acknowledgments
We thank all participants for enthusiastically participating in this study. This work was supported by grants (NRF-2015R1A2A1A15053422 and NRF-2015R1A2A1A10052745) from the National Research Foundation of Korea funded by the Ministry of Science, ICT and Future Planning, and grants (HI16C1501 and HI15C0001) from the Korea Health technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No potential conflicts of interest relevant to this article are reported.
Rights and permissions
About this article
Cite this article
Kim, SW., Jeon, JH., Lee, WK. et al. Long-term effects of oral contraceptives on the prevalence of diabetes in post-menopausal women: 2007–2012 KNHANES. Endocrine 53, 816–822 (2016). https://doi.org/10.1007/s12020-016-0972-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-0972-z