Abstract
In Kallmann syndrome (KS), congenital hypogonadism is associated with olfactory impairment. To evaluate flavor perception-related disability in KS patients, 30 patients with KS, 12 with normosmic hypogonadism (nIHH), 24 with acquired anosmia (AA), and 58 healthy controls entered the study. All participants completed questionnaires concerning dietary habits, olfaction-related quality of life (QoL), and self-determined olfactory, flavor, and taste abilities prior to undergoing standardized olfactometry and gustometry. Each subject underwent flavor testing, using orally administered aqueous aromatic solutions, identifying 21 different compounds by choosing each out of 5 alternative items. Flavor score (FS) was calculated as the sum of correct answers (range 0–21). Flavor perception by self-assessment was similar between KS, nIHH, and controls, and was mostly reduced only in AA. FS was similar between KS (5.4 ± 1.4) and AA (6.4 ± 1.9), and lower than in nIHH (16.2 ± 2.4, p < 0.001) and controls (16.8 ± 1.7, p < 0.0001). FS showed strong reproducibility, and correlated with olfactory scores in the overall population. KS and AA patients identified aromatics eliciting trigeminal stimulation better than pure odorants. Olfaction-related QoL was more impaired in AA than in KS. We report significant flavor impairment in KS. This contrasts with routine clinic evidence; KS patients, in contrast with AA, do not complain of flavor perception impairment, perhaps owing to the congenital nature of the dysfunction. Flavor perception impairment should be considered a specific KS disability, because of important detrimental effects on physical and mental health and on QoL. KS patients should also be advised of this impairment in order to prevent accidental and life-threatening events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Kallmann syndrome (KS; MIM 308700, 147950, 244200, 610628, 612370, 612702) is defined by the association between congenital hypogonadotropic hypogonadism (CHH) and olfactory impairment [1, 2].
Gustatory functions have been poorly evaluated in KS patients. Basic sense of taste, evaluated using electrogustometry, has been found to be normal in KS [3]. Flavor is a complex gustatory function, closely related to taste and to olfactory integrity, which ultimately enables food recognition, oral intake identification, and enjoyment of food. Patients experiencing olfactory loss, rather than lone olfactory impairment, mainly complain of flavor distortion and an inability to identify food, with serious repercussions on their global quality of life (QoL) [4]. In contrast, KS patients generally do not complain of gustatory or flavor dysfunctions [3].
The aim of this study was to explore the sense of taste in KS patients, in comparison with patients with congenital normosmic isolated hypogonadism (nIHH), those with acquired forms of anosmia, (AA), and normal healthy controls.
Materials and methods
Patients
The present study was approved by the Local Ethics Committee (Comitato Etico Università Federico II, reference number 253/13). All the participants were adults and gave their written informed consent, in keeping with Italian Bioethics Law and the Declaration of Helsinki.
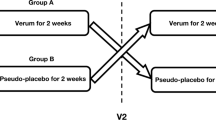
A total of 30 patients with KS, 12 with nIHH, 24 with AA, and 58 normal subjects entered the study. Criteria for inclusion of KS patients included (1) CHH, defined by clinical signs or symptoms of hypogonadism and the following: serum testosterone levels below 1 ng/mL in the presence of low or normal gonadotropins in men; primary amenorrhoea and oestradiol levels below 20 pg/mL in the presence of low or normal gonadotropins in women; (2) complete anosmia, as assessed by a previous olfactory test, or defined by self-report; and (3) further normal biochemical tests of anterior pituitary function and ferritin concentrations. nIHH was defined by the same criteria as KS, except for olfactory impairment. Almost all (28 KS and 11 nIHH) hypogonadic patients were correctly substituted for their hormonal deficiency either by sex steroids (24 KS and 8 nIHH) or gonadotropins (4 KS and 3 nIHH). AA was caused by trauma (n = 3), chronic nasal disease such as rhinosinusitis with or without polyps (n = 7), viral infections (n = 5), tumors (n = 2), previous surgery (n = 5), or unknown causes (n = 2). Subjects with neurodegenerative disorders were excluded.
Healthy controls had neither olfactory impairment nor reproductive disease on clinical enquiry, and were enrolled by participation in an educational and medical prevention program campaign (Campus Salute Onlus, Naples, Italy; www.campussalute.it). We excluded all controls having current or chronic sinusopathies, nasal polyps, or viral or seasonal rhinitis, and those suffering from either neurodegenerative or ascertained cognitive disorders. We also excluded individuals being administered drugs known to interfere with the ability to taste or smell (antithyroid drugs, antibiotics, griseofulvin, lithium, penicillamine, procarbazine, rifampin, anxiolytics, antipsychotics, antiepileptic drugs, antidepressants, amiodarone, digoxin, statins, and chemotherapeutic drugs). Characteristics of the sample population are summarized in Table 1.
Food or drink intake was restricted to water within 3 h before the tests, and smoking was prohibited within the same time period.
Questionnaires
Prior to the evaluation of chemosensory functions, patients and controls were invited to self-define their ability in sensorineural perception. Each participant was assessed for olfaction (ability to smell), flavor (food and oral intake identification ability), and sense of taste (basic taste ability) by means of a color-intuitive 10-grade arbitrary scale ranging from 0 (minimum) to 10 (maximum). In order to evaluate dietary habits, patients and controls were submitted to the PREDIMED questionnaire, in which scores range from 0 to 14 [5]. High scores mostly conformed to Mediterranean dietary style and related food preferences. All participants completed the questionnaire for olfactory disorders (QOD) that is particularly designed for anosmic populations. High QOD scores denote strong impairment of olfactory-related QoL [6].
Smell test
All the subjects were submitted to the Sniffin’ Sticks test (SS-Burghart Medical Technology, Wedel, Germany), in which odorants are presented in felt-tip pen-like sticks. The test consisted of 3 subtests for the study of odor threshold (T), odor discrimination (D), and odor identification (I), respectively, as described by Hummel et al. in 2007 [7].
Each subtest result was then added up to give a composite score, the “TDI” score. Anosmia has been defined as a TDI <16, while normosmia has been defined as a TDI >29 for subjects aged 18–53 years, and a TDI >28 for those aged >53 years.
Taste test
The basic gustatory test has been extensively described by Pingel et al. [8]. Four tastants were tested: (1) 10 g/L (29 mM) sucrose, for “sweet;” (2) 324 mg/L (1 mM) quinine hydrochloride, for “bitter;” and (3) 1.0 g/L (0.017 M) sodium chloride, for “salty;” (4) 0.2 g/L (1 mM) citric acid, for “sour.”
These substances were dissolved in distilled water and administered regionally. A drop of approximately 20 µL of each solution was applied on the upper surface of the tongue. Before application of each taste solution, the mouth was rinsed twice with distilled water. After presentation of the stimulus, each patient or control was invited to pick one of the five descriptors (“sweet,” “sour,” “salty,” “bitter,” or “water/no taste”). The Taste Score was calculated as the sum of correctly identified tastants and ranged from 0 to 16. Hypogeusia was defined as a TS <13 [8].
Flavor test
The flavor test was developed using aqueous solutions containing aromatic extracts, kindly provided by the manufacturer GIOTTI (Enrico Giotti spa, Scandicci, Firenze, Italy). Each compound had previously been tested and marketed for alimentary use in accordance with Italian and EU current regulations (European Food Safety Authority Regulation EC n. 178/2002; EC n. 854/2004; Italian G.U. n. 139/2004). A series of 20 extracts were selected, corresponding to routine dietary use. More details on aromatic bases employed for the current test are reported in Supplementary Table 1. Each tastant, originally stored in a 30 mL amber bottle, was diluted in distilled water according to the manufacturer’s instructions, stored at 4 °C in single-use aliquots after preparation, and kept at room temperature for 20 min before administration. An aliquot of approximately 1 mL of each tastant was administered in the oral cavity using a Pasteur pipette and left for approximately 5 s; the mouth was then rinsed twice with distilled water before the administration of the following tastant. At each administration, participants were invited to identify the aromatic by making a choice from 5 proposed items. A total of 21 aromatics (including one blank) were administered sequentially. The flavor score (FS) was calculated as the sum of correctly identified aromatics and ranged from 0 to 21. The flavor test has been deposited for patent license (application patent No. FI2014A000229). An abstract with partial data has already been reported as Oral Communication at the Congress of the French Society of Endocrinology [9].
Statistical analyses
Data are reported as mean ± standard deviation (SD) and as individual values in the figures. The non-parametric ANOVA Dunn’s test was used to compare quantitative data across the KS, nIHH, AA, and control groups. The χ 2 test and Fisher’s exact test were used to compare categorical data; Spearman’s rank test was applied to define correlations; and Bland–Altman plots and linear regression were used to assess reproducibility. Differences were considered statistically significant at p < 0.05. Univariate and multivariate analyses using logistic regression models were conducted to identify determinants of FS. Statistical analyses were performed and graphics were produced using Prism software, version 5.0f (GraphPad Software Inc., La Jolla,CA, USA) and the SPSS 16.0 package (SPSS, Inc., Chicago, IL, USA).
Results
Patients with AA were older than KS, nIHH, and controls (p < 0.01 vs. all) and had a higher body mass index (BMI) than controls and KS (p < 0.01 and p = 0.026, respectively). No difference in age and BMI was found across KS, nIHH, and controls. Population characteristics are shown in Table 1.
Sensorineural perception
Odor perception by self-assessment was impaired to a similar extent in KS and AA patients. It was consistently lower in anosmics (KS and AA) than in both nIHH (p < 0.0001) and controls (p < 0.0001, Fig. 1a). Taste perception by self-assessment was similar across the four groups (Fig. 1b). There was no difference in flavor perception among KS, nIHH, and controls. On the contrary, AA patients reported lower flavor perception than controls, nIHH, and KS (p < 0.001 for all, Fig. 1c).
Sensorineural perception and evaluation in healthy controls, and KS, nIHH, and AA patients. Data are reported as individual values in all panels. Details for each sensorineural test are provided in the “Materials and methods” section. AA acquired anosmia, KS Kallmann Syndrome, nIHH normosmic isolated hypogonadotropic hypogonadism; **p < 0.01; ***p < 0.001. a Olfactory perception by self-assessment (0–10 color-intuitive arbitrary scale). Higher values denote better perception. b Gustative perception by self-assessment (0–10 color-intuitive arbitrary scale). Patients and controls were instructed to indicate their subjective ability to perceive basic tastes (sweet, salty, sour, or bitter). c Flavor perception by self-assessment (0–10 color-intuitive arbitrary scale). Patients and controls were particularly instructed to indicate their subjective ability to perceive flavors and identification of different foods by ingestion. d Olfactory function evaluated by Sniffin’ Sticks® test (SS-Burghart Medical Technology, Wedel, Germany, see Methods section. The relative TDI Score (range 0–48) is reported on the y-axis. e Gustatory sensitivity evaluated by gustometry (see “Materials and methods” section). The Taste Score (range 0–16) is reported on the y-axis. f Flavor function evaluated by the flavor test (see “Materials and methods” section). The Flavor score (range 0–21) is reported on the y-axis
Chemosensory evaluation
KS and AA patients attained similar TDI scores on olfactometry (9.4 ± 2.1 vs 9.7 ± 2.7, respectively, p = 0.62). TDI scores in KS and AA were consistently lower than in either nIHH (36.3 ± 5.6, p < 0.001 for both) or controls (37.2 ± 4.3, p < 0.001 for both, Fig. 1d). Significance did not change after analysis of each subtest (threshold, discrimination, and identification) taken separately.
Taste Score by gustometry was not different across KS (15.1 ± 1.2), nIHH (15.8 ± 0.6), AA (15.1 ± 1.2), and controls (15.2 ± 1.3, Fig. 1e). Mild hypogeusia was found in 3 controls, 1 KS, and 1 AA [p = not significant (NS)].
FS was dramatically lower in KS (5.4 ± 1.4) than in nIHH (16.2 ± 2.4, p < 0.001) and in controls (16.8 ± 1.7, p < 0.0001). No difference was found between KS and AA (6.4 ± 1.9, p = NS) (Fig. 1f). Differences in FS did not change after adjustment for age and BMI. A strong correlation was found between TDI and FS scores in the entire population (r = 0.89, p < 0.0001, Supplemental Fig. 1A). Nonetheless, correlation was invalidated when considering the anosmic (AA + KS, Supplemental Fig. 1B) and the normosmic (controls and nIHH, Supplemental Fig. 1C) populations separately.
Univariate analysis in the overall population showed that FS score correlated with gender (r = 0.4, p < 0.0001), and odor self-assessment (r = 0.86, p < 0.0001), QOD–QoL (r = 0.77, p < 0.0001) and TDI (r = 0.94, p < 0.0001) scores. Correlations remained significant after adjustment for gender. After adjustment for TDI score, only the odor self-assessment score still remained significant (r = 0.52, p = 0.039).
Univariate analysis in the KS population showed that FS score was inversely related to QOD–QoL scores (r = −0.78, p 0.013), whereas TDI scores did not correlate with QOD items.
KS and AA patients, unlike controls and nIHH, were better able to identify aromatics that elicit a trigeminal response than those with a pure olfactory action (p < 0.0001 and p < 0.01, respectively. Supplemental Fig. 2). Nevertheless, the ability to identify compounds that elicit a trigeminal response was weaker in KS and AA than in controls (p = 0.028).
Test/re-test analyses showed strong reproducibility at both normosmic and anosmic ranges (Supplemental Fig. 3).
All populations attained similar PREDIMED scores (Table 1). When analyzing food preference details, however, AA seemed to more frequently consume legumes and nuts than controls (Supplemental Table 2).
QOD–QoL score was higher in AA than in controls (p < 0.0001), nIHH (p < 0.0001), and KS (p < 0.05). It was also higher in KS than in controls and in nIHH (p < 0.05 for both).
Discussion
KS is a developmental disorder in which congenital hypogonadism is associated with anosmia, because of the common ontogenesis of GnRH neurons within the olfactory placode. Olfactory impairment, though variable, is a well-recognized disability in KS patients [2]. In contrast, gustatory function has been poorly evaluated in this group. Functional evaluations exploring the basic sense of taste were not abnormal in a small series of KS patients [3]. In the same work, an intact sense of taste was reported in KS, which prompted the Authors to hypothesize that congenital anosmics might learn to concentrate on other aspects of foods to compensate for this dysfunction [3]. Another clinical entity comprising congenital hypogonadism with different degrees of eye and nasal malformations has been described and is actually known as Bosma sequence [10]. The involvement of nasal region, palate and maxilla, as well as ophthalmologic and central nervous system malformations (mainly at forebrain and corpus callosum) might be part of placodal multisystemic diseases featuring the «holoprosencephaly sequence». It is of interest, in this setting, that some of the related putative genes, like FGF8, CHD7, and FGFR1, are also mutated in KS patients [11]. Along with smell loss, basic taste was also impaired in these subjects (hypogeusia) [10].
Flavor is a complex sense, deriving from a combination of odorant and gustatory inputs, and is variously influenced by aspect, texture, and temperature [12, 13]. In our series, KS patients reported intact flavor perception by self-assessment, in contrast with individuals with AA, who also complained of difficulties in oral intake identification.
Analysis of olfactory and gustative functions through standard chemosensory tests revealed similar anosmic scores for KS and AA by the Sniffin’ Sticks test, and normogeusic scores for all groups by the taste test. This indicates that the degree of olfactory impairment is similar in the anosmic populations, and thus differences in FS might not be due to subtle weakening of the ability to smell.
It is important to consider that no routine clinic test is available for assessing flavor. We developed a test to assess this function, based on the identification of oral liquid intakes. This test explores the capacity to identify different aromatics dissolved in aqueous solutions, thus allowing standardization and eliminating putative confounding factors, such as consistency, temperature, and appearance (color and shape). The flavor test has shown high reproducibility in both normal individuals and anosmic populations (see Supplemental Fig. 3).
We clearly show a dramatic impairment of flavor ability in KS, which is similar to that observed in AA subjects. Flavor perception impairment does not seem to be due to peculiar dietary habits, as all populations tested attained similar scores and expressed similar food choices, consistent with medium adherence to Mediterranean diet regimens. A more detailed evaluation of the flavor test shows that the distribution of correct answers is not widely scattered, but some compounds are more frequently perceived correctly than others. In particular, KS and AA are more able to identify compounds with trigeminal action than those already known as pure odorants. Hummel et al. found hypersensitivity of trigeminal nerve in three patients with KS by means of chemosensory evoked potentials [14]. Despite these findings, in our larger series, aromatics with a trigeminal component are less repeatedly perceived in KS and AA than in normosmics, in line with more recent evidence reporting an overall reduction of trigeminal stimulation in anosmic populations [15, 16].
AA patients were older and had a higher BMI than KS, nIHH, and controls. FS, however, does not correlate with age or BMI. On the contrary, gender represents a stronger determinant for FS, in the same way as is known for olfactometry, in which better performances are registered in young women [17]. FS completely correlates with olfactometric scores, thus representing an optimal tool to detect clear-cut anosmic from normosmic individuals. Correlation is abolished when anosmic or normosmic populations are considered separately. Although the TDI score is not designed specifically to detect patients with a better or worse sense of smell among normosmics or anosmics, the FS might provide different information from that provided by simple olfactory volatile impressions; this could possibly derive from various combinatory inputs during oral intake. This should be more appropriately evaluated, and should also be investigated in specific subpopulations, e.g., those involved in the perfume, culinary, or gastronomic fields. Mild hypogeusia was found in only a few subjects, and was not related to a particular subpopulation. Furthermore, taste scores in these individuals were just below the lower limits of normality, reflecting a mild impairment likely not affecting results. Taste scores did not correlate with flavor scores. We did not include the “umami” flavor among tastants because it is hardly recognizable or distinguishable from “salty.”
Sex steroid deficiency per se does not seem to have a role in flavor perception. The FS is strictly normal in patients with nIHH, who share the same steroidogenic defect as KS. Similarly, hormonal treatment does not have a role in determining FS. In the overall CHH population, there were three patients who were not, or were insufficiently, supplemented with hormonal treatments, and they attained similar scores. Treatment with HRT or gonadotropins did not affect FS results either. No difference in FS was registered on the basis of the different mutations in either the KS or the nIHH genes tested.
Consistent with what is routinely observed in clinics and in previous reports, we confirm that KS patients are hardly aware of their taste disabilities. Patients were asked specifically about their ability to perceive flavors and aromatics and to recognize foods and oral intake in their daily life. In our experience, only a few KS subjects reported a clear consciousness of this inadequacy, and the vast majority was not aware of it. In line with this finding, detriment to QoL related to the sensorineural inabilities in KS is less critical than in AA, probably reflecting the congenital nature of the disorder in the former.
It is of interest that, in anosmic population, FS negatively correlated with the QOD–QoL scores, whereas TDI did not. This may reflect a major importance of taste dysfunction in determining the QoL detriment. The importance of using validated questionnaires in this setting is underlined by the difficulties in producing a reproducible olfactory ability self-evaluation by simply asking the patient about the presence or the degree of hyposmia on a visual analogic scale [6, 18]. The scores deriving from the QOD, particularly designed for anosmic populations, revealed higher impairment in AA than in KS.
AA patients, who attained the highest QOD–QoL scores, also scored the lowest sincerity statements, indicating a particular tendency to give socially desirable answers in this population. This may be due to the older age of AA, since it is known that age may affect QOD results [6]. Alternatively, higher QOD scores in AA may more properly reflect a global detriment in general wellbeing, which is more strongly perceived in the acquired form of this dysfunction. Although other QoL questionnaires have not been specifically tested in this study, QOD items were designed to explore the complaints about disosmic patients’ problems in daily life, and have been shown to well correlate with established tests for QoL and mood states, such as the Beck’s Depression Inventory or the Mood Inventory tests [6].
Apart from overt anosmics, it will be interesting to evaluate taste in hyposmic patients, who may experience partially distorted impressions of odor. The main question to explore, using this completely qualitative test, is whether these patients may achieve a full recognition of food, even if only intermediate scores are recorded on olfactometry. Although it is beyond the scope of this study, it will be also intriguing to assess taste function and food identification tasks in patients suffering from dys- or ageusia, as their main complaint seems to solely affect the basic taste ability.
One limitation of our study lies in the subjective nature of the test. A further development with chemosensory evoked potentials or functional brain MRI under different aromatics administration could be useful to support and expand our findings [19].
Flavor perception disability is both a social and a medical concern. This function is closely associated with the enjoyment and social function of mealtimes, and invariably influences relationships and social behaviors [4, 20–22]. From a medical point of view, recognition of nutrients may prevent ingestion of spoilt or contaminated foods. Thus, taste alteration is not merely an inconvenience but can also impact on physical and mental health. Abnormal flavor perception in KS might have serious health consequences by elevating the risk of foodborne illness and by altering food choices, with potential repercussions on nutritional status. Moreover, flavor and taste dysfunction may lead to an increased risk of allergic reactions in people with food sensitivities and even have an impact on survival [23].
In conclusion, in agreement with previous reports, we show that, along with impairment of sense of smell, KS patients also fail to identify oral intake. The deficiency in flavor perception has to be considered a specific sensorineural impairment in KS, a condition for which spectrum of associated disabilities is expanding. KS patients should be made aware of their gustative disability in order to prevent nutritional imbalance and accidental life-threatening events.
References
J. Young, Approach to the male patient with congenital hypogonadotropic hypogonadism. J. Clin. Endocrinol. Metab. (2012). doi:10.1210/jc.2011-1664
H.M. Lewkowitz-Shpuntoff, V.A. Hughes, L. Plummer, M.G. Au, R.L. Doty, S.B. Seminara, Y.M. Chan, N. Pitteloud, W.F. Crowley, R. Balasubramanian, Olfactory phenotypic spectrum in idiopathic hypogonadotropic hypogonadism: pathophysiological and genetic implications. J. Clin. Endocrinol. Metab. (2012). doi:10.1210/jc.2011-2041
K.S. Hasan, S.S. Reddy, N. Barsony, Taste perception in kallmann syndrome, a model of congenital anosmia. Endocr. Pract. (2007). doi:10.4158/EP.13.7.716
S.S. Schiffman, Taste and smell losses in normal aging and disease. JAMA 278, 1357–1362 (1997)
M.A. Martinez-Gonzalez, A. Garcia-Arellano, E. Toledo, J. Salas-Salvado, P. Buil-Cosiales, D. Corella, M.I. Covas, H. Schroder, F. Aros, E. Gomez-Gracia, M. Fiol, V. Ruiz-Gutierrez, J. Lapetra, R.M. Lamuela-Raventos, L. Serra-Majem, X. Pinto, M.A. Munoz, J. Warnberg, E. Ros, R. Estruch, A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One (2012). doi:10.1371/journal.pone.0043134
J. Frasnelli, T. Hummel, Olfactory dysfunction and daily life. Eur. Arch. Otorhinolaryngol. (2005). doi:10.1007/s00405-004-0796-y
T. Hummel, G. Kobal, H. Gudziol, A. Mackay-Sim, Normative data for the “Sniffin’ Sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: an upgrade based on a group of more than 3,000 subjects. Eur. Arch. Otorhinolaryngol. (2007). doi:10.1007/s00405-006-0173-0
J. Pingel, J. Ostwald, H.W. Pau, T. Hummel, T. Just, Normative data for a solution-based taste test. Eur. Arch. Otorhinolaryngol. (2010). doi:10.1007/s00405-010-1276-1
L. Maione, I.C. Nettore, A. Colao, R. Pivonello, E. Cantone, N. Maione, C. Eloit, Y. Young, Altération de la perception des goûts chez des patients avec syndrome de Kallmann : une atteinte neurosensorielle méconnue. Ann. Endocrinol. (2014). doi:10.1016/j.ando.2014.07.067
J.F. Bosma, R.I. Henkin, R.L. Christiansen, J.R. Herdt, Hypoplasia of the nose and eyes, hyposmia, hypogeusia, and hypogonadotrophic hypogonadism in two males. J. Craniofac. Genet. Dev. Biol. 1, 153–184 (1981)
J.M. Graham Jr, J. Lee, Bosma arhinia microphthalmia syndrome. Am. J. Med. Genet. A 140, 189–193 (2006)
S.C. Kinnamon, R.F. Margolskee, Mechanisms of taste transduction. Curr. Opin. Neurobiol. 6, 506–513 (1996)
D.M. Small, J. Prescott, Odor/taste integration and the perception of flavor. Exp. Brain Res. (2005). doi:10.1007/s00221-005-2376-9
T. Hummel, H. Pietsch, G. Kobal, Kallmann’s syndrome and chemosensory evoked potentials. Eur. Arch. Otorhinolaryngol. 248, 311–312 (1991)
J. Frasnelli, B. Schuster, T. Hummel, Interactions between olfaction and the trigeminal system: what can be learned from olfactory loss. Cereb. Cortex (2007). doi:10.1093/cercor/bhl135
T. Hummel, S. Barz, J. Lotsch, S. Roscher, B. Kettenmann, G. Kobal, Loss of olfactory function leads to a decrease of trigeminal sensitivity. Chem. Senses 21, 75–79 (1996)
R.L. Doty, E.L. Cameron, Sex differences and reproductive hormone influences on human odor perception. Physiol. Behav. (2009). doi:10.1016/j.physbeh.2009.02.032
S. Nordin, A.U. Monsch, C. Murphy, Unawareness of smell loss in normal aging and Alzheimer’s disease: discrepancy between self-reported and diagnosed smell sensitivity. J. Gerontol. B Psychol. Sci. Soc. Sci. 50, P187–P192 (1995)
R.I. Henkin, L.M. Levy, Functional MRI of congenital hyposmia: brain activation to odors and imagination of odors and tastes. J. Comput. Assist. Tomogr. 26, 39–61 (2002)
B.S. Naik, N. Shetty, E.V. Maben, Drug-induced taste disorders. Eur. J. Intern. Med. (2010). doi:10.1016/j.ejim.2010.01.017
S.S. Schiffman, B.G. Graham, Taste and smell perception affect appetite and immunity in the elderly. Eur. J. Clin. Nutr. 54(Suppl 3), S54–S63 (2000)
S.S. Schiffman, J. Zervakis, Taste and smell perception in the elderly: effect of medications and disease. Adv. Food Nutr. Res. 44, 247–346 (2002)
S.S. Schiffman, Effects of aging on the human taste system. Ann. N. Y. Acad. Sci. (2009). doi:10.1111/j.1749-6632.2009.03924.x
Acknowledgments
We thank the Campus Salute Onlus for collaborating with Federico II University, and for allowing the enrolment of a sample population drawn from educational and preventive medical programs particularly addressed to the general population. We are grateful to Dr Corinne Eloit for her competence and expertise in the domain of sensorineural abilities, and for her inspiring insights. We are indebted to Donato Creti, Francesca Trapani, and the entire team at Enrico GIOTTI spa for their commitment and for providing facilities to prepare and distribute the aromatic bases used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the Authors of this study declare they have no conflict of interest.
Additional information
Luigi Maione and Elena Cantone have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Maione, L., Cantone, E., Nettore, I.C. et al. Flavor perception test: evaluation in patients with Kallmann syndrome. Endocrine 52, 236–243 (2016). https://doi.org/10.1007/s12020-015-0690-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0690-y