Abstract
Systemic administration of kainic acid causes inflammation and apoptosis in the brain, resulting in neuronal loss. Dual cyclooxygenase/5-lipoxygenase (COX/5-LOX) inhibitors could represent a possible neuroprotective approach in preventing glutamate excitotoxicity. Consequently, we investigated the effects of a dual inhibitor of COX/5-LOX following intraperitoneal administration of kainic acid (KA, 10 mg/kg) in rats. Animals were randomized to receive either the dual inhibitor of COX/5-LOX (flavocoxid, 20 mg/kg i.p.) or its vehicle (1 ml/kg i.p.) 30 min after KA administration. Sham brain injury rats were used as controls. We evaluated protein expression of phosphorylated extracellular signal-regulated kinase (p-ERK1/2) and tumor necrosis factor alpha (TNF-α) as well as levels of malondialdehyde (MDA), prostaglandin E2 (PGE2) and leukotriene B4 (LTB4) in the hippocampus. Animals were also observed for monitoring behavioral changes according to Racine Scale. Finally, histological analysis and brain edema evaluation were carried out. Treatment with the dual inhibitor of COX/5-LOX decreased protein expression of p-ERK1/2 and TNF-α in hippocampus, markedly reduced MDA, LTB4 and PGE2 hippocampal levels, and also ameliorated brain edema. Histological analysis showed a reduction in cell damage in rats treated with the dual inhibitor of COX/5-LOX, particularly in hippocampal subregion CA3c. Moreover, flavocoxid significantly improved behavioral signs following kainic acid administration. Our results suggest that dual inhibition of COX/5-LOX by flavocoxid has neuroprotective effects during kainic acid-induced excitotoxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excitotoxicity is a central mechanism of neuronal death in a wide range of neurological disorders including epilepsy, stroke, trauma and neurodegenerative diseases (Mehta et al. 2013). Kainic acid (KA), a potent excitotoxic amino acid, stimulates KA receptors, which are members of non-N-methyl-d-aspartate ionotropic glutamate receptors, resulting in seizures, behavioral changes and neurodegeneration in susceptible brain regions such as the hippocampus (Ben-Ari 1985; Vincent and Mulle 2009; Zheng et al. 2011).
From a molecular point of view, activation of KA receptors produces membrane depolarization and causes alteration in intracellular calcium concentrations, generation of reactive oxygen species and mitochondrial dysfunction as well as an increased production of proinflammatory cytokines. All these cellular alterations lead to neuronal apoptosis and necrosis (Wang et al. 2005). Neuroinflammation and oxidative stress are thought to play an essential role in KA-induced excitotoxic brain damage (Marini et al. 2004a, b; Farooqui et al. 2006; Zhang and Zhu 2011).
Cyclooxygenase (COX) is the rate-limiting enzyme in the synthesis of prostanoids, including prostaglandins (PGs), prostacyclin and thromboxanes, which are crucial mediators in neuroinflammation (Takemiya et al. 2007). Accordingly, prostaglandin E2 (PGE2) is pathologically increased in the brain after KA treatment and has been proven to be closely associated with brain damage (Takemiya et al. 2006; Takemiya and Yamagata 2013).
5-Lipoxygenase (5-LOX) is also expressed in neurons, and it represents the key enzyme in the synthesis of the inflammatory eicosanoids, leukotrienes (LTC4, LTD4, LTE4 and LTF4) from arachidonic acid, that following KA receptor activation promote neurodegeneration and brain damage (Chu and Praticò 2009; Farooqui 2011).
Recent findings on this topic indicate the potential therapeutic role of dual COX/5-LOX inhibitors in KA-induced excitotoxicity and oxidative damage due their antioxidant/anti-inflammatory effect, also suggesting the need for the development of new neuroprotective agents (Manev et al. 2000; Bishnoi et al. 2007; Kumar et al. 2012). A dual inhibitor of COX/5-LOX, namely flavocoxid, is a mixed extract containing the naturally occurring flavonoids, baicalin from Scutellaria baicalensis and catechin from Acacia catechu (Burnett et al. 2007a). Specifically, this association showed a balanced inhibition of both COX-1 and COX-2 enzyme activities and a significant inhibition of 5-LOX enzyme activity (COX-1 enzyme, IC50 = 12.3 μg/ml and COX-2 enzyme, IC50 = 11.3 μg/ml and only a weak COX-1 activity, IC50 = 25 μg/ml; 5-LOX enzyme, IC50 = 110 μg/ml) (Burnett et al. 2007a, 2011; Burnett and Levy 2012). Through the inhibition of the peroxidase moieties of these enzymes, flavocoxid significantly reduces oxidative stress/lipid peroxidation, blunting IkB-α loss from the cytoplasm and the consequent NF-kB activation in LPS-stimulated macrophages (Altavilla et al. 2009). These anti-inflammatory activities have been tested and confirmed in several experimental in vivo models (Messina et al. 2009; Polito et al. 2010; Altavilla et al. 2012; Bitto et al. 2012). Pharmacokinetic and toxicological safety studies in animals and humans have also shown the efficacy and safety of this flavonoid combination (Burnett et al. 2007b; Burnett and Levy 2012). In addition, this dual inhibitor of COX/5-LOX is effective in ameliorating the signs and symptoms of moderate osteoarthritis of the knee, in humans, with a good safety profile (Levy et al. 2010; Burnett and Levy 2012).
However, no study has examined, to date, whether a dual inhibitor of COX/5-LOX might also have neuroprotective effects in the KA-induced acute brain damage, which still represents a valuable model in rodents for exploring the pathogenesis of excitotoxicity and testing new neuroprotective compounds. In light of this background, the aim of the present study was to investigate in KA-administered rats the protective effects of flavocoxid.
Materials and Methods
Animals
All animal procedures were carried out in accordance with EU Directive 2010/63/EU on the protection of animals used for scientific experiments. Male Sprague–Dawley rats (250–300 g) fed on a standard diet and with tap water ad libitum and were allocated in our animal facility with a 12-h light–dark cycle. The temperature of the animals was maintained at approximately 37 °C using an overhead lamp.
Experimental Protocol
After general anesthesia with sodium pentobarbital (50 mg/kg i.p.), the animals (n = 96) were divided into the following groups: sham + vehicle (1 ml/kg i.p.); sham + flavocoxid (20 mg/kg i.p.); KA (10 mg/kg i.p.) + vehicle; and KA + flavocoxid (20 mg/kg i.p.). Flavocoxid was administered 30 min after KA injection. The dose was chosen in agreement with previously published in vivo experiments (Altavilla et al. 2009, 2012; Messina et al. 2009; Polito et al. 2010). A first set of animals (n = 6 in each experimental group) was killed 2 h after KA injection to measure the concentration of phosphorylated extracellular signal-regulated kinase (p-ERK1/2) and tumor necrosis factor-α (TNF-α) in hippocampal region. A second set of animals (n = 6 in each experimental group) was killed 6 h after kainic acid to assess the hippocampal levels of malondialdehyde (MDA), prostaglandin E2 (PGE2) and leukotriene B4 (LTB4). A third set of animals (n = 12 in each experimental group) was killed 48 h after KA for histological analysis (n = 6) and brain edema evaluation (n = 6). This latter set of animals was also observed over the total period of 6 h after KA acid injection for monitoring behavioral signs.
Determination of Phosphorylated Extracellular Signal-Regulated Kinase (p-ERK1/2) and Tumor Necrosis Factor Alpha (TNF-α) by Western Blot Analysis
Protein samples (30 µg) from hippocampus were separated by electrophoresis and transferred on to a nitrocellulose membrane using the transfer buffer (39 mM glycine, 48 mM Tris pH 8.3, 20 % methanol) at 200 mA for 1 h. The membranes were blocked with 5 % nonfat dry milk in TBS-0.1 % Tween for 1 h at room temperature to block nonspecific binding, washed three times for 10 min each in TBS-0.1 % Tween and incubated with a primary antibody for phosphorylation level of ERK1/2 or TNF-α (Cell Signaling, Beverly, MA) in TBS-0.1 % Tween overnight at 4 °C. The day after, membranes were washed three times for 10 min each in TBS-0.1 % Tween and incubated with a specific peroxidase-conjugated secondary antibody (Pierce, UK) for 1 h at room temperature. After washing, the membranes were analyzed by the enhanced chemiluminescence system according to the manufacturer’s protocol (Amersham, UK). The results from each experimental group were expressed as relative integrated intensity compared with those of sham rats measured with the same batch. Beta-actin (Cell Signaling, Beverly, MA) was used to confirm protein equal loading.
Evaluation of Lipid Peroxidation
Lipid peroxidation was measured by malondialdehyde (MDA) assay. The assay was carried out by using a colorimetric commercial kit (Lipid Peroxidation Assay kit, cat No. 437634; Calbiochem-Novabiochem Corp., Darmstadt, Germany). Briefly, 0.65 mL 10.3 nM N-methyl-2-phenylindole in acetonitrile was added to 0.2 mL of brain tissue. After vortexing for 3–4 s and adding 0.15 mL of 37 % (v/v) HCl, the samples were mixed and closed with a tight stopper and incubated at 45 °C for 60 min. The samples were then cooled on ice, and the absorbance was measured spectrophotometrically at 586 nm.
A calibration curve of an accurately prepared standard MDA solution (from 2 to 128 nM/mL) was also drawn for comparison.
Measurement of Prostaglandin E2 (PGE2) and Leukotriene B4 (LTB4) Hippocampal Levels
PGE2 was directly assayed on hippocampus samples without purification by using the Cayman EIA kit (Cayman, Arcore, Milan, Italy). Samples were run in duplicate, and the absorbance was spectrophotometrically read at 412 nm. Signal intensity was directly proportional to the content of PGE2 in samples. Hippocampal tissue samples were homogenized and assayed for LTB4 using a commercially available ELISA kit (R&D Systems, Milan, Italy) based on the forward sequential competitive binding technique in which LTB4 present in samples competes with a fixed amount of horseradish peroxidase-labeled LTB4 for sites on a chicken polyclonal antibody. The absorbance was read at 450 nm. The intensity of the color was proportional to the concentration of LTB4 in the sample.
Evaluation of Brain Edema
To evaluate the extent of brain edema following KA acid administration, tissue sections from each group of animals were assayed for water content at 48 h after injury, using wet weight/dry weight. Freshly dissected tissue samples of hippocampus were weighed on aluminum foil, dried for 24 h at 105 °C and reweighed as previously described (Calapai et al. 1995). The percentage of water was calculated as follows: water content (%) = (wet weight − dry weight)/wet weight × 100.
Histology
Forty-eight hours after KA challenge, six animals in each group were killed under anesthesia, as before described. After perfusion with cold saline solution to remove red blood cells, whole brain was immediately removed, dissected and preserved in a solution of paraformaldehyde 4 % in 0.1 M phosphate buffer (PB) and stored at 4 °C. Fixed brains were embedded in paraffin and cut in coronal sections (7 μm) and then stained with Nissl method to observe morphologic changes. Histological identification of nervous structures was made by analogies with the brain of the rat, according to the atlas of Paxinos and Watson (1986). Morphologic analysis was performed using an Axiophot photomicroscope (Carl Zeiss, Berlin, Germany), and evaluation of viable neurons was done in the hippocampal regions using an image system (Soft Imaging System, GmbH, Hamburg, Germany). The slides were analyzed double-blinded by two observers independently. Hippocampus neuron counts were made in three adjacent microscope fields in the region of a given section. Criteria for a neuron to be counted were a well-defined cytoplasm and a clearly visible nucleolus with a nuclear outline. Neuron morphology was observed in areas of the CA1 and CA3 regions and in hippocampal subregion CA3c. Corresponding topographical areas were selected in each animal of the specific groups. Three sections per animal were normally analyzed.
Behavioral Signs
Animals were observed for behavioral changes (grooming, rearing, hind limb scratching, wet dog shakes, jaw movements, salivation, urination, defecation, head nodding), incidence and latency of convulsions over the total period of 6 h. Seizure activity was rated during a 6-h period following the KA challenge according to the scale devised by Racine (1972): stage 1, facial clonus; stage 2, nodding; stage 3, forelimb clonus; stage 4, forelimb clonus with rearing; stage 5, rearing, jumping and falling. Animals were scored after having had three consecutive seizures at each stages.
Data Analysis and Statistical Procedures
The statistical significance of the differences between control and treatment groups was analyzed with one-way ANOVA using Tukey’s test as post hoc procedure. Moreover, repeated measures two-way ANOVA was used to analyze behavioral scores in experimental groups. In all cases, a probability error of less than 0.05 was selected as criterion for statistical significance.
Compounds
Flavocoxid (Limbrel®), a dual inhibitor of COX/5-LOX, was a kind gift of Primus Pharmaceuticals, Inc. (Scottsdale, Arizona, USA), and is a mixture of naturally occurring flavonoids baicalin and catechin. The compound was administered intraperitoneally in 0.9 % NaCl solution. Kainic acid (Nanocs Inc., Cambridge Pharma-Chem) was dissolved in distilled water. Rats were administered kainic acid at a dose of 10 mg/kg i.p., with pH adjusted to 7.1 ± 0.1. All substances were prepared fresh daily.
Results
Effects of a Dual Inhibitor of COX/5-LOX on Hippocampal Protein Expression of p-ERK1/2 and TNF-α
Figure 1a, b shows representative gels and quantitative data, highlighting hippocampal protein expression of p-ERK1/2 and TNF-α in rats subjected to kainic acid-induced neurotoxicity and treated with vehicle or flavocoxid (20 mg/kg i.p.). Very low protein levels for both p-ERK1/2 and TNF-α were observed in the hippocampus of sham rats. In contrast, the hippocampus of animals challenged with kainic acid had a marked increase in the protein levels for p-ERK1/2 and TNF- α. The dual inhibitor of COX/5-LOX blunted the increase in hippocampal p-ERK1/2 and TNF-α protein expression of kainic acid-induced rats (Fig. 1a, b).
Representative Western blot analysis of p-ERK1/2 (a) and TNF-α (b) in hippocampus samples collected from sham and kainate-lesioned rats treated with vehicle or flavocoxid (20 mg/kg i.p.). Autoradiography highlights p-ERK1/2 (a) and TNF-α (b) expression and relative quantitative data (mean ± SD of six animals) that were evaluated 2 h after the administration of kainate, respectively. #P < 0.001 versus sham + vehicle; *P < 0.001 versus kainate + vehicle
Effects of a Dual Inhibitor of COX/5-LOX on PGE2 and LTB4 Hippocampal Levels
Inflammatory eicosanoids derived from arachidonic acid (PGE2 and LTB4) have been shown to be involved in brain damage induced in rats by systemic administration of kainic acid. Our results confirm that kainic acid causes a profound increase in both PGE2 and LTB4 hippocampal levels (Fig. 2a, b). Conversely, the dual inhibitor of COX/5-LOX significantly reduced PGE2 and LTB4 in the treated group.
PGE2 (a) and LTB4 (b) levels studied by ELISA in hippocampus samples collected from sham and kainate-lesioned rats treated with vehicle or flavocoxid (20 mg/kg i.p.) 6 h after the administration of kainate. Each point represents the mean ± SD of six experiments. #P < 0.001 versus sham + vehicle; *P < 0.001 versus kainate + vehicle
Effects of a Dual Inhibitor of COX/5-LOX on MDA Hippocampal Levels
Kainic acid caused a significantly increase in MDA hippocampal levels (Fig. 3). In contrast, the dual inhibitor of COX/5-LOX, administered following kainate injury, reduced the tissues levels of MDA as compared to vehicle-treated group (Fig. 3).
MDA levels studied by ELISA in hippocampus samples collected from sham and kainate-lesioned rats treated with vehicle or flavocoxid (20 mg/kg i.p.) 6 h after the administration of kainate. Each point represents the mean ± SD of six experiments. #P < 0.001 versus sham + vehicle; *P < 0.001 versus kainate + vehicle
Administration of a Dual Inhibitor of COX/5-LOX Reduces Brain Edema
KA injection caused brain edema, particularly in susceptible brain regions (hippocampal CA1 and CA3 regions). Assessment of water content revealed that flavocoxid-treated animals had a significant reduction in brain edema compared with vehicle-treated animals (Fig. 4).
Effects of flavocoxid (20 mg/kg i.p.), a dual inhibitor of COX/5-LOX or vehicle, on brain edema evaluated through water content in the hippocampus of rats challenged with kainic acid or sham rats. Each point represents the mean ± SD of six animals. #P < 0.001 versus sham + vehicle; *P < 0.001 versus kainate + vehicle
Administration of a Dual Inhibitor of COX/5-LOX Counteracts Kainic Acid-Induced Neuronal Loss in the Rat Hippocampus
Sham rats treated with either vehicle or flavocoxid demonstrated normal neuronal density in the CA1 and CA3 regions and CA3c subregion (Fig. 5a, b and e). In contrast, CA1 and CA3 regions and the hippocampal subregion CA3c of rats administered with kainic acid + vehicle showed evident neuronal loss with degenerating pyramidal cells and edema. Neuronal damage was particularly evident in the hippocampal subregion CA3c (Fig. 5c, e). Administration of the dual inhibitor of COX/5-LOX (20 mg/kg i.p.) significantly reduced the neuronal loss and preserved neuronal architecture in the CA1, CA3 regions and in the subregion CA3c (Fig. 5d, e).
a Representative Nissl-stained sections of a sham hippocampus. b Representative Nissl-stained sections of a sham + flavocoxid (20 mg/kg i.p.) hippocampus. c Representative KA-injected hippocampus. We observed that the damaged areas induced by KA are characterized by evident neuronal loss and edema. Arrows indicate degenerating pyramidal cells, in particular in CA3c. d Representative KA-injected hippocampus treated with flavocoxid (20 mg/kg i.p.), a dual inhibitor of COX/5-LOX. A well-preserved neuronal architecture in the CA1 and CA3 regions and in hippocampal subregion CA3c was observed in KA-injected rats treated with flavocoxid. Original magnification 10× and 40×. e Effects of flavocoxid (20 mg/kg i.p.), a dual inhibitor of COX/5-LOX, or vehicle on neuronal density in the CA1 and CA3 regions and in hippocampal subregion CA3c of rats challenged with kainic acid or sham rats. Each point represents the mean ± SD of six animals. #P < 0.001 versus sham + vehicle; *P < 0.001 versus kainate + vehicle
A Dual Inhibitor of COX/5-LOX Improves Kainic Acid-Induced Behavioral Signs
Rats treated with vehicle and administered with 10 mg/kg of kainic acid had marked abnormal behavioral signs lasting 5–6 h. The administration of the dual inhibitor of COX/5-LOX, at 20 mg/kg i.p., significantly reduced the frequency and the intensity of the behavioral signs 120 and 240 min following kainic acid administration (Fig. 6a, b).
Discussion
The injection of kainic acid, an analog of glutamic acid, has been used as an useful experimental tool for acute and chronic brain disorders characterized by a strong excitotoxic damage (Ben-Ari 1985; Marini et al. 2004a, b; Vincent and Mulle 2009; Zheng et al. 2011). Although each disease has distinctive morphological and biochemical features, the pathophysiology is outlined by an exaggerated inflammatory response, including the up-regulation of inflammatory cytokines expression, overproduction of the proinflammatory eicosanoids, edema formation, and it is usually related to the evolution of brain damage triggered by this neurotoxic cascade (Farooqui 2011).
A neuroprotective approach with anti-inflammatory treatments may attenuate or prevent KA-mediated neurodegeneration. Regarding this latter, the potential role of NSAIDs and/or selective COX-2 inhibitors including celecoxib, NS398, rofecoxib and SC58125 has been extensively studied (Gobbo and O’Mara 2004; Takemiya et al. 2006; Takemiya and Yamagata 2013). Although the selective COX-2 inhibitors can suppress an elevation of PGE2 and block hippocampal cell death (Takemiya et al. 2007), inhibition of COX-2 with selective drugs in experimental models of adult rodents has resulted in contrasting findings. In fact, some studies reported that these drugs could ameliorate seizure-induced neuronal damage (Kunz and Oliw 2001; Kawaguchi et al. 2005; Jung et al. 2006), while in others no clear neuroprotection has been observed (Holtman et al. 2009), or they have even enhanced neurodegeneration (Baik et al. 1999). However, taking into account that PG synthesis is only one part of the arachidonic acid pathway, it has been suggested that a better anti-inflammatory action could be obtained by a dual inhibition of COX and 5-LOX enzymes in target organs (Leone et al. 2007).
Indeed, neuroprotection represents an important and multifaceted problem into clinical setting taking into account the different molecular pathways activated during the development of brain damage. For instance, glial activation involving astrocytes, microglial cells, lymphocyte infiltration and/or reactive mediators, such as reactive oxygen species, are further hallmarks of inflammatory reactions. This justifies the research strategy focusing on some novel neuroprotective compounds that rely on multiple mechanisms, including anti-inflammatory mechanisms associated with indirect anti-radical activity.
Flavonoids have been used in traditional remedies for the treatment of a variety of diseases, including inflammatory conditions (Van Loon 1997; Chou et al. 2003; De Clerq 2005; Huang et al. 2005). Flavocoxid, marketed as Limbrel®, is an FDA-regulated prescription, medical food, for the clinical dietary management of osteoarthritis in the USA, which contains the flavonoids baicalin and catechin (Burnett et al. 2007a; Levy et al. 2010). Pharmacokinetic data obtained in healthy individuals justify both timing and route of administration of a dual inhibitor of COX/5-LOX in the present experimental model (Flavocoxid, 500 mg per os; AUC: 7007 μg/ml/h, C max: 0.93 μg/ml, T max: 5.8 h, T½: 11–12 h for baicalin; half-life range from 2 to 3 h, plasma levels peak ~3 h with levels still detectable 120 h later, probably due to reabsorption and enterohepatic circulation for catechin) (Burnett and Levy 2012).
Our data showed that flavocoxid, acting as a dual inhibitor of COX/5-LOX, exerts beneficial effects after KA administration in rats. Flavocoxid significantly reduced LTB4 and PGE2 levels and decreased the protein expression of TNF-α in hippocampus following KA injection, suggesting that blocking both leukotrienes and prostaglandins production might have synergistic effects and achieve optimal anti-inflammatory activity (Farooqui et al. 2006; Bishnoi et al. 2007). Moreover, our data are in agreement with experimental evidences showing that the prostaglandin signal is strongly connected with cytokines production (i.e., TNF-α), also indicating a key role of MAP kinase family members in the biosynthesis of eicosanoids in brain (Chen et al. 2004; Jeong et al. 2011).
Indeed, elevated p-ERK1/2 protein expression in hippocampal samples of rats treated with KA confirmed a crucial role of MAP kinase family members in the early phase of neuroinflammation and in the progression of brain injury following KA injection (Lubin et al. 2005; Wang et al. 2011). Flavocoxid reduced hippocampal p-ERK1/2 and TNF-α protein expression in KA-challenged rats and markedly attenuated the severity of inflammatory process. More specifically, flavocoxid caused a decrease in ERK and TNF-α signaling at 2 h following KA injection, while the reduction in eicosanoids occurred later. This confirms that the compound has an effect on the early steps of the inflammatory cascade, as previously shown (Altavilla et al. 2009).
In our study, the elevated MDA levels 6 h after KA administration suggest an increased lipid peroxidation/oxidative stress during the early phase of the excitotoxic damage. Indeed, administration of the dual inhibitor of COX/5-LOX reduced MDA levels in KA-challenged rats and markedly attenuated the severity of brain injury. These data confirm our previous results obtained in vitro in endotoxin-stimulated macrophages (Altavilla et al. 2009).
Also, in agreement with our results, it has been recently demonstrated that the pre-treatment with flavocoxid was protective in an experimental model of cerebral ischemia in rats, suggesting that this medical food may represent a potential therapy for stroke patients to reduce neuroinflammation and lipid peroxidation (Singh and Chopra 2014).
Our results showed that a dual inhibition of COX/5-LOX by flavocoxid was able to blunt brain edema. These effects are likely strictly linked because it has been suggested that overproduction of cytokines, proinflammatory eicosanoids and reactive oxygen species is strongly related to brain edema formation induced by KA (Marini et al. 2004a, b; Wang et al. 2011).
The biochemical and molecular picture is also correlated with histological findings. In fact, 2 days following KA administration, we observed a significant neuronal loss in both CA1 and CA3 areas, particularly in hippocampal subregion CA3c, which is more susceptible to excitotoxic injury and has a pivotal role in limbic epileptogenesis. In contrast, flavocoxid caused significant neuroprotective effects with an improvement in the histological picture, preserving neuronal architecture.
Indeed, cell death in epilepsy is a function of both severity and frequency of seizures. Accordingly, our treatment significantly improved behavioral changes that accompanied KA administration in rats. In fact, flavocoxid, at 20 mg/kg i.p., reduced the number of seizures as well as their intensity 120 and 240 min following KA administration.
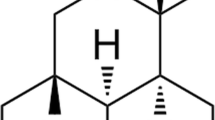
So far, the present findings, taken together, could be the result of a reduced seizure severity/frequency than the consequence of targeting molecular pathways examined, then unmasking a novel and interesting anti-epileptic effect of flavocoxid. However, flavocoxid is not primarily a compound directly targeting cellular excitability, but it is a nutraceutical combination that acts on COX and 5-LOX enzymes activity and on early steps of the inflammatory cascade. Consequently, we hypothesize, in light of the actual data, that the neuroprotective effect of flavocoxid is likely related to an attenuation of kainate-triggered excitotoxic cascade (see Fig. 7). Of course, further experiments will be needed to better clarify this latter intriguing issue.
Conclusions
Collectively, we demonstrated for the first time that a naturally derived dual inhibitor of COX and 5-LOX displays neuroprotective effects against excitotoxicity induced by kainic acid. Such combined inhibition could counteract many deleterious effects of excitotoxicity, avoiding some of the harmful side effects of NSAIDs and/or selective COX-2 inhibitors in clinical setting.
In addition, these findings suggest that flavocoxid might also offer a structural model for the design of new analog compounds and/or for new nutritional approaches that can provide novel therapeutic options in the management of neurological disorders.
References
Altavilla, D., Minutoli, L., Polito, F., Irrera, N., Arena, S., Magno, C., et al. (2012). Effects of flavocoxid, a dual inhibitor of COX and 5-lipoxygenase enzymes, on benign prostatic hyperplasia. British Journal Pharmacology, 167, 95–108.
Altavilla, D., Squadrito, F., Bitto, A., Polito, F., Burnett, B. P., Di Stefano, V., et al. (2009). Flavocoxid, a dual inhibitor of cyclooxygenase and 5-lipoxygenase, blunts pro-inflammatory phenotype activation in endotoxin-stimulated macrophages. British Journal Pharmacology, 157, 1410–1418.
Baik, E. J., Kim, E. J., Lee, S. H., & Moon, C. (1999). Cyclooxygenase-2 selective inhibitors aggravate kainic acid induced seizure and neuronal cell death in the hippocampus. Brain Research, 843, 118–129.
Ben-Ari, Y. (1985). Limbic seizure and brain damage produced by kainic acid: Mechanisms and relevance to human temporal lobe epilepsy. Neuroscience, 14, 375–403.
Bishnoi, M., Patil, C. S., Kumar, A., & Kulkarni, S. K. (2007). Co-administration of acetyl-11-keto-beta-boswellic acid, a specific 5-lipoxygenase inhibitor, potentiates the protective effect of COX-2 inhibitors in kainic acid-induced neurotoxicity in mice. Pharmacology, 79, 34–41.
Bitto, A., Minutoli, L., David, A., Irrera, N., Rinaldi, M., et al. (2012). Flavocoxid, a dual inhibitor of COX-2 and 5-LOX of natural origin, attenuates the inflammatory response and protects mice from sepsis. Critical Care, 16, R32.
Burnett, B. P., Bitto, A., Altavilla, D., Squadrito, F., Levy, R. M., & Pillai, L. (2011). Flavocoxid inhibits phospholipase A2, peroxidase moieties of the cyclooxygenases (COX), and 5-lipoxygenase, modifies COX-2 gene expression, and acts as an antioxidant. Mediators of Inflammation, 2011, 385780.
Burnett, B. P., Jia, Q., Zhao, Y., & Levy, R. M. (2007a). A medicinal extract of Scutellaria baicalensis and Acacia catechu acts as a dual inhibitor of cyclooxygenase and 5-lipoxygenase to reduce inflammation. Journal of Medicinal Food, 10, 442–451.
Burnett, B. P., & Levy, R. M. (2012). Flavocoxid (Limbrel®) manages osteoarthritis through modification of multiple inflammatory pathways: A review. Functional Foods in Health and Disease, 2, 379–413.
Burnett, B. P., Silva, S., Mesches, M. H., Wilson, S., & Jia, Q. (2007b). Safety evaluation of a combination, defined extract of Scutellaria baicalensis and Acacia catechu. Journal of Food Biochemistry, 31, 797–825.
Calapai, G., Squadrito, F., Rizzo, A., Marciano, M. C., Campo, G. M., & Caputi, A. P. (1995). Multiple actions of the coumarine derivative cloricromene and its protective effects on ischemic brain injury. Naunyn-Schmiedeberg’s archives of pharmacology, 351, 209–215.
Chen, B. C., Chang, Y. S., Kang, J. C., Hsu, M. J., Sheu, J. R., Chen, T. L., et al. (2004). Peptidoglycan induces nuclear factor-kappaB activation and cyclooxygenase-2 expression via Ras, Raf-1, and ERK in RAW 264.7 macrophages. The Journal of biological chemistry, 279, 20889–20897.
Chou, T. C., Chang, L. P., Li, C. Y., Wong, C. S., & Yang, S. P. (2003). The antiinflammatory and analgesic effects of baicalin in carrageenan evoked thermal hyperalgesia. Anesthesia & Analgesia Journal, 97, 1724–1729.
Chu, J., & Praticò, D. (2009). The 5-lipoxygenase as a common pathway for pathological brain and vascular aging. Cardiovascular Psychiatry and Neurology, 2009, 174657.
De Clerq, E. (2005). Current lead natural products for the chemotherapy of human immunodeficiency virus (HIV) infection. Medicinal Research Reviews, 20, 323–349.
Farooqui, A. A. (2011). Neurochemical aspects of inflammation in brain. In A. A. Farooqui & T. Farooqui (Eds.), Molecular aspects of neurodegeneration and neuroprotection. Bentham Science.
Farooqui, A. A., Ong, W. Y., & Horrocks, L. A. (2006). Inhibitors of brain phospholipase A2 activity: Their neuropharmacological effects and therapeutic importance for the treatment of neurologic disorders. Pharmacological Reviews, 58, 591–620.
Gobbo, O. L., & O’Mara, S. M. (2004). Post-treatment, but not pre-treatment, with the selective cyclooxygenase-2 inhibitor celecoxib markedly enhances functional recovery from kainic acid-induced neurodegeneration. Neuroscience, 125, 317–327.
Holtman, L., van Vliet, E. A., van Schaik, R., Queiroz, C. M., Aronica, E., & Gorter, J. A. (2009). Effects of SC58236, a selective COX-2 inhibitor, on epileptogenesis and spontaneous seizures in a rat model for temporal lobe epilepsy. Epilepsy Research, 84, 56–66.
Huang, Y., Tsang, S. Y., Tao, X., & Chen, Z. Y. (2005). Biological properties of baicalein in cardiovascular system. Current Drug Targets - Cardiovascular & Hematological Disorders, 5, 177–184.
Jeong, E. A., Jeon, B. T., Shin, H. J., Kim, N., Lee, D. H., Kim, H. J., et al. (2011). Ketogenic diet-induced peroxisome proliferator-activated receptor-γ activation decreases neuroinflammation in the mouse hippocampus after kainic acid-induced seizures. Experimental Neurology, 232, 195–202.
Jung, K. H., Chu, K., Lee, S. T., Kim, J., Sinn, D. I., Kim, J. M., et al. (2006). Cyclooxygenase-2 inhibitor, celecoxib, inhibits the altered hippocampal neurogenesis with attenuation of spontaneous recurrent seizures following pilocarpine-induced status epilepticus. Neurobiology of Disease, 23, 237–246.
Kawaguchi, K., Hickey, R. W., Rose, M. E., Zhu, L., Chen, J., & Graham, S. H. (2005). Cyclooxygenase-2 expression is induced in rat brain after kainate-induced seizures and promotes neuronal death in CA3 hippocampus. Brain Research, 1050, 130–137.
Kumar, A., Prakash, A., Pahwa, D., & Mishra, J. (2012). Montelukast potentiates the protective effect of rofecoxib against kainic acid-induced cognitive dysfunction in rats. Pharmacology, Biochemistry and Behavior, 103, 43–52.
Kunz, T., & Oliw, E. H. (2001). The selective cyclooxygenase-2 inhibitor rofecoxib reduces kainate-induced cell death in the rat hippocampus. European Journal of Neuroscience, 13, 569–575.
Leone, S., Ottani, A., & Bertolini, A. (2007). Dual acting anti-inflammatory drugs. Current Topics in Medicinal Chemistry, 7, 265–275.
Levy, R. M., Khokhlov, A., Kopenkin, S., Bart, B., Ermolova, T., Kantemirova, R., et al. (2010). Efficacy and safety of flavocoxid, a novel therapeutic, compared with naproxen: A randomized multicenter controlled trial in subjects with osteoarthritis of the knee. Advances in Therapy, 27, 731–742.
Lubin, F. D., Johnston, L. D., Sweatt, J. D., & Anderson, A. E. (2005). Kainate mediates nuclear factor-kappa B activation in hippocampus via phosphatidylinositol-3 kinase and extracellular signal-regulated protein kinase. Neuroscience, 133, 969–981.
Manev, H., Uz, T., & Qu, T. (2000). 5-Lipoxygenase and cyclooxygenase mRNA expression in rat hippocampus: Early response to glutamate receptor activation by kainate. Experimental Gerontology, 35, 1201–1209.
Marini, H., Altavilla, D., Bellomo, M., Adamo, E. B., Marini, R., Laureanti, F., et al. (2004a). Modulation of IL-1 beta gene expression by lipid peroxidation inhibition after kainic acid-induced rat brain injury. Experimental Neurology, 188, 178–186.
Marini, H., Costa, C., Passaniti, M., Esposito, M., Campo, G. M., Ientile, R., et al. (2004b). Levetiracetam protects against kainic acid-induced toxicity. Life Sciences, 74, 1253–1264.
Mehta, A., Prabhakar, M., Kumar, P., Deshmukh, R., & Sharma, P. L. (2013). Excitotoxicity: Bridge to various triggers in neurodegenerative disorders. European Journal of Pharmacology, 698, 6–18.
Messina, S., Bitto, A., Aguennouz, M., Mazzeo, A., Migliorato, A., Polito, F., et al. (2009). Flavocoxid counteracts muscle necrosis and improves functional properties in MDX mice: A comparison study with methylprednisolone. Experimental Neurology, 220, 349–358.
Paxinos, G., & Watson, C. (1986). The rat brain in stereotaxic coordinates. Sydney: Academic Press.
Polito, F., Bitto, A., Irrera, N., Squadrito, F., Fazzari, C., Minutoli, L., et al. (2010). Flavocoxid, a dual inhibitor of cyclooxygenase-2 and 5-lipoxygenase, reduces pancreatic damage in an experimental model of acute pancreatitis. British Journal of Pharmacology, 161, 1002–1011.
Racine, R. J. (1972). Modification of seizure activity by electrical stimulation: Motor seizure. EEG. Clinical Neurophysiology, 32, 281–294.
Rojas, A., & Dingledine, R. (2013). Ionotropic glutamate receptors: Regulation by G-protein-coupled receptors. Molecular Pharmacology, 83, 746–752.
Singh, D. P., & Chopra, K. (2014). Flavocoxid, dual inhibitor of cyclooxygenase-2 and 5-lipoxygenase, exhibits neuroprotection in rat model of ischaemic stroke. Pharmacology, Biochemistry and Behavior, 120, 33–42.
Takemiya, T., Maehara, M., Matsumura, K., Yasuda, S., Sugiura, H., & Yamagata, K. (2006). Prostaglandin E2 produced by late induced COX-2 stimulates hippocampal neuron loss after seizure in the CA3 region. Neuroscience Research, 56, 103–110.
Takemiya, T., Matsumura, K., & Yamagata, K. (2007). Roles of prostaglandin synthesis in excitotoxic brain diseases. Neurochemistry International, 51, 112–120.
Takemiya, T., & Yamagata, K. (2013). Intercellular signaling pathway among endothelia, astrocytes and neurons in excitatory neuronal damage. International Journal of Molecular Sciences, 14, 8345–8357.
Van Loon, I. M. (1997). The golden root: Clinical applications of Scutellaria baicalensis GEORGI flavonoids as modulators of the inflammatory response. Alternative Medicine Review, 2, 472–480.
Vincent, P., & Mulle, C. (2009). Kainate receptors in epilepsy and excitotoxicity. Neuroscience, 158, 309–323.
Wang, Y., Liu, P. P., Li, L. Y., Zhang, H. M., & Li, T. (2011). Hypothermia reduces brain edema, spontaneous recurrent seizure attack, and learning memory deficits in the kainic acid treated rats. CNS Neuroscience & Therapeutics, 17, 271–280.
Wang, Q., Yu, S., Simonyi, A., Sun, G. Y., & Sun, A. Y. (2005). Kainic acid-mediated excitotoxicity as a model for neurodegeneration. Molecular Neurobiology, 31, 3–16.
Zhang, X. M., & Zhu, J. (2011). Kainic Acid-induced neurotoxicity: Targeting glial responses and glia-derived cytokines. Current Neuropharmacology, 9, 388–398.
Zheng, X. Y., Zhang, H. L., Luo, Q., & Zhu, J. (2011). Kainic acid-induced neurodegenerative model: Potentials and limitations. Journal of Biomedicine and Biotechnology, 2011, 457079.
Acknowledgments
This study was granted by a departmental funding.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national and/or institutional guidelines for the care and use of animals were followed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Letteria Minutoli and Herbert Marini have equally contributed to this paper.
Rights and permissions
About this article
Cite this article
Minutoli, L., Marini, H., Rinaldi, M. et al. A Dual Inhibitor of Cyclooxygenase and 5-Lipoxygenase Protects Against Kainic Acid-Induced Brain Injury. Neuromol Med 17, 192–201 (2015). https://doi.org/10.1007/s12017-015-8351-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12017-015-8351-0