Abstract
Historically, eosinophils have been considered as end-stage cells involved in host protection against parasitic infection and in the mechanisms of hypersensitivity. However, later studies have shown that this multifunctional cell is also capable of producing immunoregulatory cytokines and soluble mediators and is involved in tissue homeostasis and modulation of innate and adaptive immune responses. In this review, we summarize the biology of eosinophils, including the function and molecular mechanisms of their granule proteins, cell surface markers, mediators, and pathways, and present comprehensive reviews of research updates on the genetics and epigenetics of eosinophils. We describe recent advances in the development of epigenetics of eosinophil-related diseases, especially in asthma. Likewise, recent studies have provided us with a more complete appreciation of how eosinophils contribute to the pathogenesis of various diseases, including hypereosinophilic syndrome (HES). Over the past decades, the definition and criteria of HES have been evolving with the progress of our understanding of the disease and some aspects of this disease still remain controversial. We also review recent updates on the genetic and molecular mechanisms of HES, which have spurred dramatic developments in the clinical strategies of diagnosis and treatment for this heterogeneous group of diseases. The conclusion from this review is that the biology of eosinophils provides significant insights as to their roles in health and disease and, furthermore, demonstrates that a better understanding of eosinophil will accelerate the development of new therapeutic strategies for patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eosinophils, a minority of the white blood cells, are classified as nonspecific destructive and cytotoxic cells. Our appreciation of certain basic characteristics of eosinophils is sturdy and unambiguous. It is clear that eosinophils are produced in the bone marrow from multipotent hematopoietic stem cells, which first differentiate into a progenitor, and then into a separate mature eosinophil lineage. Once mature, they are released into peripheral blood. Each of these steps is under the delicate regulation of transcription factors and (or) cytokines. Eosinophils are considered as end-stage cells which play essential roles in the immune response to parasitic infection, and in the mechanisms of hypersensitivity.
However, a comprehensive understanding of the role of this multifunctional cell in both health and disease is still in great need. In brief, eosinophils express an array of proinflammatory cytokines, chemokines, and lipid mediators, and express receptors for cytokines, immunoglobulins, and complement as well. Eosinophils can modify T cell activities through MHC class II and costimulatory molecules that allow eosinophils to act as antigen-presenting cells (APCs). In addition, advances in the field of eosinophil immunobiology have implicated eosinophils as important participants in the innate and adaptive immune responses [1–3].
In this review, we present a comprehensive perspective on the physiology and cellular biology of eosinophils, including the function and molecular mechanisms of their granule proteins and cell surface markers, and the genetic and epigenetic regulation of eosinophils, with special attention to the important roles of the transcription factor GATA-1 and interleukin (IL)-5 [4]. We also review the roles of eosinophils in eosinophilic human health and diseases, which include not only parasitic infection and allergic diseases [5] but also a variety of different syndromes that are identified to be associated with abnormalities of eosinophils. Examples of these syndromes include eosinophilic gastroenteritis and eosinophilic esophagitis, asthma, and hypereosinophilic syndrome. The recent updates on the genetic, molecular, and immunologic mechanisms of hypereosinophilic syndrome (HES) are also reviewed here and in more detail in another article in this issue.
The Significance of the Eosinophil Throughout History
The eosinophil granulocyte was first observed by Wharton Jones in 1846, and later described by Paul Ehrlich in 1879, who noted its uncommon capacity to be stained with the acidophilic dyes [2]. In spite of the fact that eosinophils have been discovered for over 130 years, our knowledge about their biochemistry and molecular biology remains quite limited, especially when compared to their highly studied sister cell, the neutrophil. This lack of research did not change until 1989, but with the development of separation and purification techniques, especially the use of “negative selection,” obtaining eosinophils in sufficient numbers and of high enough purity for research studies became possible [6, 7].
Over the years, in particular recently, research studies have shown that the activities of eosinophils are far more complex than previously appreciated in both health and disease. For example, Chu et al. [8] have suggested a role for eosinophils in plasma B cell survival in the bone marrow. Specifically, it has been observed that the number of antigen-specific plasma B cells is decreased in the bone marrow of eosinophil-deficient mice (PHIL or △dblGATA1) or mice depleted of eosinophils when immunized with anti-Siglec-F antibodies (Table 1). Studies have also highlighted a novel role of eosinophils in maintaining metabolic homeostasis through maintenance of adipose alternatively activated macrophages (AAMs) [9]. Eosinophils may also contribute potentially to the protumorigenic and/or antitumorigenic activities, despite the observation that the presence or absence of eosinophilia in cancer does not appear to have a major correlation with patient prognosis [10]. Currently, the presence of eosinophils has also been recognized as a marker for acute GVHD in transplant rejection (e.g., kidney [11] and heart [12]), although a thorough understanding of its mechanisms is lacking. In addition, the list of unexplained eosinophilic diseases has dramatically expanded in the past decades, whereas the exact roles and molecular mechanisms of eosinophilia in these diseases remain largely mysterious.
Cellular Biology of the Eosinophil: Granule Proteins and Cell Surface Markers
Eosinophil Granule Proteins
Human eosinophil granules contain four major proteins: major basic protein (MBP), eosinophil cationic protein (ECP), eosinophil peroxidase (EPO), and eosinophil-derived neurotoxin (EDN) [13] (Fig. 1), which are capable of inducing tissue damage and dysfunction [2].
Cellular features of eosinophils [25]. Mature eosinophils have minimal numbers of mitochondria, endoplasmic reticulum (ER), and Golgi, as well as a nucleus. Eosinophils express a large number of cell surface markers that support growth, adhesion, chemotaxis, and cell-to-cell interactions. CCR CC-chemokine receptor, CXCR CXC-chemokine receptor, CysLT cysteinyl leukotriene receptors, ECP eosinophil cationic protein, EDN eosinophil-derived neurotoxin, EPX eosinophil peroxidase, GM-CSF granulocyte-macrophage colony-stimulating factor, IFN interferon, IL interleukin, LFA lymphocyte function antigen, MBP major basic protein, NOD nucleotide-binding oligomerization domain, PRR pattern-recognition receptor, PSGL P-selectin glycoprotein ligand, RAGE receptor for advanced glycation end-products, RIG-I retinoic acid-inducible gene I, TGF transforming growth factor, TLR Toll-like receptor, TNF tumor necrosis factor, VLA very late activation antigen
ECP has been shown to possess antibacterial activity and promote degranulation of mast cells [14, 15]. The functional mechanism of ECP is thought to involve pore formation in target membranes [16]. Other noncytotoxic activities of ECP has also been demonstrated, such as suppression of T cell proliferative responses, immunoglobulin synthesis by B cells, induction of mast cell degranulation, and stimulation of airway mucus secretion [17]. Eosinophils play a role in protection against parasitic infections, a finding that was supported by the direct toxicity of MBP against helminthic worms [2, 15, 18]. The toxic effect of MBP is thought to result from increased membrane permeability through surface charge interactions leading to perturbation of the cell surface lipid bilayer [19].
EPO has been shown to catalyze the peroxidative oxidation of halides and pseudohalides (thiocyanate) together with hydrogen peroxide generated by dismutation of superoxide produced during the respiratory burst [20–22]. This reaction ends with the formation of bactericidal hypohalous acids, under physiologic conditions, promoting oxidative stress and subsequent cell death by apoptosis and necrosis.
EDN, also known as eosinophil peroxidase (EPX), is an eosinophil granule-derived secretory protein. EDN can exert some cytotoxic effects as a cationic toxin and is therefore able to put down parasites. For example, it is shown that EDN has the capability to kill newborn larvae of Trichinella spiralis [15].
Degranulation, the release of granule contents into the extracellular space, is a prominent eosinophil function in response to cytokines. It is accepted that piecemeal degranulation is the most commonly observed physiological form of eosinophil degranulation. Recent research has provided insights into the molecular mechanism of piecemeal degranulation. For example, IL-4 released from eotaxin-stimulated eosinophils first forms a complex with IL-4Rα within the granule membrane, and then mobilizes into secretory vesicles [23, 24]. Several granule- and vesicle-associated cytokine receptors have been identified in eosinophils to be in association with degranulation, including the receptors of IL-4, IL-6, and IL-13, as well as CCR3, although receptor-mediated trafficking pathways await further evaluation.
Cell Surface Markers
Eosinophils express a large number of cell surface markers that support growth, adhesion, chemotaxis, and cell-to-cell interactions (Fig. 1). Specfically, IL-5 receptor subunit-α (IL-5RA) is the most prominent cytokine receptor associated with eosinophils in human and mice (Table 1). Among the main receptors that define the unique biology of the eosinophil are sialic acid-binding immunoglobulin-like lectin 8 (SIGLEC-8) in humans and SIGLEC-F (or SIGLEC-5) in mice, as well as CC-chemokine receptor 3 (CCR3) [3, 25, 26].
Adhesion Receptors
Previous studies have demonstrated that eosinophils can express various cell surface markers associated with adhesion. For example, eosinophils constitutively express L-selectin, which regulates eosinophil rolling on the endothelium via CD34 and mucosal addressin cell adhesion molecule-1 (MAdCAM-1) in vivo [27, 28]. Eosinophils also express P-selectin glycoprotein ligand-1 (PSGL-1 or CD162) and sialyl-Lewis (CD15s), which interact with E-selectin and P-selectins [29].
Integrins on the surface of immune cells integrate the extracellular and intracellular environments in the immune system. Integrin family members α7 (α4β7), β1 (α4β1 and α6β1), and β2 (αLβ2, αMβ2, αXβ2, and αDβ2) are expressed by eosinophils [30, 31].
Lymphocyte function antigen (LFA)-1 (αLβ2) is highly expressed by eosinophils. This molecule interacts with intercellular adhesion molecule-1 (ICAM-1) that is expressed on the surface of endothelial cells. The important role of ICAM-1 in ligand mediating T cell proliferation in response to antigen has been demonstrated by the fact that the shortage of ICAM-1 prevents eosinophils from entering the airways in ICAM-1-deficient mice [32]. In addition, the β2-integrin/ICAM-1-dependent pathways may play a role in the regulation of eosinophil accumulation in the colon [30].
The α4β7 integrin interacts with MAdCAM-1, which is mainly expressed by the vascular endothelium in the intestinal tract. Eotaxin-1-dependent eosinophil recruitment to the small intestine is MAdCAM-1/α4β7 integrin dependent [33]. Of note, in β7-integrin knockout (KO) mice, intestinal eosinophilia develops slowly following T. spiralis infection [34] (Table 1).
During their transit from the bloodstream into various tissues, eosinophils use integrins to interact with adhesion receptors on the surface of the vascular endothelium [3]. In mice, eosinophil recruitment to the site of allergic inflammation in the lung is dependent on very late activation antigen-4 (VLA-4, also known as α4β1 integrin, an integrin dimer composed of CD49d and CD29) [35]. The critical role of these integrin molecules in regulating eosinophil trafficking to the allergic lung has been demonstrated in anti-β1-treated mice and VLA-4-deficient mice [35, 36]. In a case series of three patients with multiple sclerosis, marked eosinophilia occurred after treatment with natalizumab, a humanized monoclonal inhibitory antibody against CD49 [37].
Receptors for Lipid Mediators
Eosinophils are equipped with multiple receptors for lipid recognition, including cysteinyl receptors (CysLT1R and CysLT2R), the high-affinity prostaglandin type 2 (PGD2) receptor, and platelet-activating factor (PAF) receptors [38–40]. CysLT1R is expressed on both mature eosinophils and immature eosinophil progenitors, while CysLT2R is only expressed on mature eosinophils. Expression of CysLT1R and CysLT2R is elevated during asthma exacerbations. It has been shown that CysLT1R antagonist is capable of stopping eosinophil from differentiation and/or maturation in vivo [39, 41].
The function of the PGD2 receptor (also known as chemoattractant receptor-homologous molecule expressed on Th2 cells (CRTH2)) on eosinophils has not yet been fully defined. However, it has been suggested that it may regulate eosinophil transmigration [42, 43], and mediate Th2 cell and eosinophil/basophil recruitment [42]. Thus, the CRTH2 receptor is currently being considered as a highly promising therapeutic target for the treatment of eosinophil-associated disorders. Preliminary data from a Phase II study of a CRTH2 antagonist to treat patients with moderate persistent asthma have shown a reduction in sputum eosinophil levels [44]. More clinical studies are needed to evaluate the effect of CRTH2 on reducing blood and tissue eosinophilia in human disease.
Chemokine Receptors
Eosinophils constitutively express the chemokine receptors CCR3 and CCR1 [45, 46]. With expression of CCR1, eosinophils respond to CCR1 ligands including macrophage inflammatory protein (MIP)-1a/CCL3. CCR3 is a promiscuous chemokine receptor that has up to 11 different ligands [47]. These ligands include the eotaxins [CCL11 (eotaxin-1), CCL24 (eotaxin-2), and CCL26 (eotaxin-3)]. CCR3 can also be activated by CCL5 (also known as “regulated upon activation, normal T cell expressed and secreted” (RANTES)), CCL7 (macrophage chemotactic protein-3, MCP3), CCL8 (MCP2), and CCL12 (MCP5). Eosinophils have also been shown to express a series of other chemokine receptors including CXCR3, CXCR4, CCR5, CCR6, and CCR8 [48–50].
Cytokine Receptors
Studies have shown that eosinophils express specific cytokine receptor subunits for IL-5, IL-3, and GM-CSF. These include IL-5 receptor α subunit (IL-5Rα, also known as CD125), IL-3 receptor α chain (IL-3Rα, also known as CD123), and the α subunit of the heterodimeric receptor for colony-stimulating factor 2 (CSF2Rα, also known as GM-CSFR or CD116) [51]. Eosinophils also express the c-kit receptor (CD117), IFNγ R α-chain (CDw119), TNF-α receptor types 1 and 2 (CD120a, CD120b), type 1 IL-4 receptor [IL-4R α-chain (CD124) and the common α-chain (CD132)], and the IL-9 receptor [CD129 and CD132] [3]. IL-5Rα is the most prominent cytokine receptor associated with eosinophils and is expressed by eosinophils and basophils in both humans and mice. IL-5 receptor signaling plays a significant role in promoting the development of eosinophils, as well as inducing eosinophil activation, and sustains eosinophil survival in peripheral blood and tissues [52]. Activation of CD120a and CD120b are thought to promote eosinophil apoptosis [53].
Pattern-Recognition Receptors (PRRs)
Human eosinophils express PRRs families, including several members of the Toll-like receptor (TLR) family, nucleotide-binding oligomerization domain (NOD)-like receptors and the receptor for advanced glycation end-products (RAGE) [54]. The expression of TLR1, TLR2, TLR3, TLR4, TLR5, TLR6, TLR7, and TLR9 has been reported on human eosinophils [54, 55], although at varying intensities. Of note, the presence or absence of TLR3, TLR4, and TLR6 has been unclear. Moreover, it has been suggested that human eosinophils do not express TLR2 and that peptidoglycan (ligand for TLR2) and Pam3CSK4 (ligand for TLR1/TLR2) cannot induce activation [56]. In contrast, mRNAs and proteins for TLR1, TLR2, and TLR6 have been found by Wong [55]. Moreover, they have shown that TLR2 can activate eosinophils by promoting cell surface expression of ICAM-1 and CD18.
Although the overall expression level of TLR on eosinophils is generally low compared with those in neutrophils, eosinophils expressed a relatively elevated level of TLR7. Of note, TLR7 may act as the most prominent TLR expressed by eosinophils. Functional analysis reveals that the synthetic ligand R-848 (also known as resiquimod), a TLR7 and TLR8 agonist, induces eosinophil secretion and prolongs eosinophil survival [56].
Complement Receptors and Fc Receptors
Recently, more and more studies have revealed that eosinophils express complement receptors such as CR1 (CD35), CR3 (CD11b/CD18), CR4 (CD11c), C3aR, C5aR, and receptors for C1q [57, 58]. CR1 can interact with a number of complement fragments including C3b, C4b, iC3b, and C1q. The expression of CR1 on eosinophil is regulated by a number of triggers, such as leukotriene B4 (LTB4). CR3 is recognized by the ligands iC3b and ICAM-1; both of which can induce eosinophil activation [59]. Moreover, eosinophils express Fc receptors for IgA, IgD, IgG, and IgM [58]. It appears that these receptors also have a role in stimulating eosinophil survival, degranulation, and generation of leukotrienes. The expression of the IgE receptor on eosinophils remains controversial [60], as more investigators tend to believe that eosinophils express few, if any, α or β chains of the high affinity IgE receptor or the low-affinity IgE receptor (CD23) [61–63].
Physiology of the Eosinophil
Eosinophils and Immune Regulation
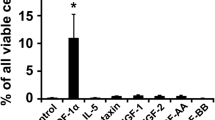
Classically, eosinophils have been considered to be end-stage effector cells. However, recent research has shown that eosinophils, which are equipped with an arsenal of cytokines and inflammatory mediators, possess numerous immune functions (Fig. 2).
Eosinophilic positioning in the immune system. Eosinophils are produced in the bone marrow from pluripotent stem cells. The stem cells first differentiate into a progenitor, and then into a separate eosinophil lineage. The development of eosinophils is determined by a body of interdependent regulatory events of transcription factors, especially GATA-1. IL-5 primarily controls the eosinophil migration from the bone marrow to the blood. Circulating eosinophils interact with the endothelium by processes involving rolling, adhesion, and diapedesis. Eosinophils also have a definitive impact on the actions of other leukocytes. Eosinophils can work as antigen-presenting cells (APCs), which have been described in the main text. Eosinophils also prime B cells for production of IgM and interact with dendritic cells (DCs), mast cells, and neutrophils. Eosinophils help the survival of plasma cells in the bone marrow
Antigen Presentation
For eosinophils to function as antigen-presenting cells (APCs), major histocompatibility complex II (MHC-II) proteins [human leukocyte antigen (HLA)-DR] must be expressed. Fresh blood eosinophils from most normal and eosinophilic donors are devoid of MHC class II expression [64], but when cultured in vitro with specific cytokines, e.g., GM-CSF, IL-3, or a combination of IL-3 and interferon-γ (IFN-γ), eosinophils can be uniformly induced to synthesize and express MHC class II [7, 64–66]. Similarly, it has been shown that airway or lymph node eosinophils constitutively express MHC class II in mice [67, 68]. Thus, eosinophils of human and mice have the capacity to express HLA-DR.
B7 molecules CD80 (B7-1) and CD86 (B7-2) are especially significant on APCs and serve to deliver the requisite costimulatory signals to lymphocytes. The function of B7 on eosinophils has been well studied by Celestin and colleagues [66]. The populations of highly purified eosinophils (>98 %), isolated from the blood of human, express no detectable CD80, CD86, or HLA-DR molecules on their surface, as shown by FACS analysis. Surface CD86 expression becomes consistently detectable at 48 h and further increases at 72 h following culture with IL-3 at a concentration of 20 ng/ml. In contrast to its induction of CD86, IL-3 failed to induce expression of CD80 on eosinophils. Peritoneal eosinophils of IL-5-transgenic mice express CD80 and CD86 without cytokine treatment, and their expression on the eosinophils is increased by incubation with GM-CSF [69].
Evidence supporting a role of eosinophils in antigen presentation in vivo shows that eosinophils following antigen challenge migrate from endobronchial areas to the draining mediastinal lymph nodes [67]. These eosinophils localize to the T cell regions of the draining lymph nodes, like classical APCs, and they form clusters with antigen-specific T cells [67, 70]. Lymph node eosinophils, expressing MHC class II, CD80, and CD86, can restimulate memory T cells from antigen-challenged mice [67, 71]. Using mice that have received adoptive transfer of antigen-specific naive T cell receptor (TCR)-transgenic T cells, eosinophils have been shown to have the capacity to activate naive T cells [70].
The capacity of eosinophils to present protein antigen has been debated in some publications. It has been reported that mouse eosinophils are in fact efficient APCs for naive antigen-specific T cells both in vitro and in vivo [72]. Contradictorily, whole protein-pulsed mouse eosinophils do not seem to be able to stimulate antigen-specific naive T cells and antigen-specific primed T cells, although some proliferation of T cells can be observed [66, 73]. It is interesting to note that the ability of eosinophils to present antigen may be related to the extraction methodology. The use of ammonium chloride (chemical formula NH4Cl), an inhibitor of lysosome acidification (needed for antigen presentation), negatively correlates with eosinophil antigen presentation activity [67, 73], providing a possible explanation for the discrepancy of results between different studies.
Mast Cell Regulation
A substantial body of literature has emerged demonstrating that eosinophils have the propensity to regulate mast cell functions. Both MBP and ECP, but not EDN, stimulated concentration-dependent histamine release from purified rat peritoneal mast cells [74]. Besides, human umbilical cord blood-derived mast cells can be activated by MBP to release histamine, PGD-2, GM-CSF, TNF-α, and IL-8 [75]. Several studies have indicated that MBP induces mast cell activation in a pattern similar to that of other polybasic compounds, such as substance P, compound 48/80, and bradykinin [75].
An “eosinophil-mast cell axis” has been proposed whereby the two innate immune leukocytes interact to enhance their respective capabilities. Chymase, a mast cell-specific protease, enhances eosinophil survival, recruits eosinophils into tissue sites, and promotes the release of eosinophil-derived cytokines and chemokines [76]. It is suggested that mediator exchange between mast cells and eosinophils might occur through direct cell-cell contacts [77]. Nerve growth factor (NGF) [78] is preformed in eosinophils and acts in an autocrine fashion following activation by EPO. Meanwhile, NGF promotes mast cell survival and activation [79, 80]. In conclusion, eosinophils and mast cells communicate in a symbiotic fashion.
Thymic Eosinophils
Thymic eosinophils, localizing to the corticomedullary region, are preferentially recruited during the neonatal period. In mice, the absolute number of eosinophils in the thymus increases 10-fold between 7 and 14 days of age to reach parity with dendritic cells. Thereafter, the absolute number of eosinophils declines, with a marked fall at the age of 28 days. Subsequently, a second influx of eosinophils is observed at 16 weeks of age, corresponding to the commencement of thymic involution. Eosinophils at this stage localize to the medullary region [81].
Detectable mRNA levels of TGF-β and IL-16 are present in thymic eosinophils, consistent with their wide distribution among leukocytes. Thymic eosinophils of mice also express proinflammatory cytokines TNF-α, IL-1α, and the Th2-cytokines IL-4 and IL-13 [81]. Recently, it has also been shown that thymic eosinophils in humans at the neonatal stage and in childhood, express indoleamine 2,3-dioxygenase (IDO), IL-4, and IL-13 [82]. Eotaxin-1, which is constitutively expressed in the thymus, is capable of regulating the recruitment of eosinophils into the thymus [83]. In animal experiments, eosinophilia is completely deficient in eotaxin-knockout mice [84].
It has also been postulated that eosinophils may participate directly in the selection of T cells or may aid in the scavenging of dead cells that fail in negative selection. Consistent with this speculation, the recruitment of eosinophils and their anatomical localization within discrete compartments of the thymus coincide with negative selection of double-positive thymocytes [81]. Using a model of acute negative selection, injection of the cognate peptide into MHC class I-restricted male (HY) TCR transgenic mice increases the proportion of thymic eosinophils. Eosinophils have been associated with clusters of apoptotic bodies, suggesting eosinophil-mediated MHC class I-restricted thymocyte deletion.
Eosinophils also express costimulatory molecules that are related to clonal deletion, such as CD30 ligand (CD153) and CD66 [81]. In a recent study, the IDO-positive eosinophils have the capacity to promote the Th2 character of the developing thymus in normal humans by inducing apoptosis of Th1 cells through depletion of tryptophan [82]. Another function of thymic eosinophils is that eosinophils aid macrophages in the phagocytosis of apoptotic thymocytes induced by γ-irradiation [85].
Eosinophils and Reproduction
In the uterus, eosinophils are predominantly localized to the endometrial stroma and at the endometrial-myometrium junction, where they may contribute to regulation of development and maintenance of epithelial integrity [86]. Eosinophil recruitment into the uterus is regulated by IL-5, but their presence in the subepithelial stroma is not affected by IL-5 deficiency, suggesting redundant pathways [87]. Accordingly, in response to ovarian steroid hormones, the infiltration of eosinophils in the uterus correlates with the expression of eotaxin-1, RANTES, and MIP-1α [88, 89].
Eotaxin-1-deficient mice have a 2-week delay in the onset of estrus, along with a delay in the first age of parturition. These suggest a role for eosinophils in preparing the mature uterus for pregnancy [90]. In addition, the infiltration and degranulation of eosinophils in the cervixes of pregnant women have been observed by Knudsen and colleagues [91]. Timmons et al. [92] have suggested that the increased presence of eosinophils in the cervix is involved in dilation for birth and postpartum remodeling. On the other hand, the effect of eosinophils during blastocyst implantation and pregnancy has yet to be proven [93, 94]. Interestingly, the MBP of eosinophils is ectopically expressed by placental X cells and giant cells in the uterus during pregnancy [95], although this is not directly related to eosinophils [96].
Deletion of the eotaxin-1 gene in mice results in reduction in terminal end bud formation and reduces branching complexity of the ductal tree [97]. Eosinophils participate in mammary gland development through local secretion of eosinophil-derived TGF-β [97]. The importance of eosinophils in the mammary gland development has also been demonstrated in animal models, which shows less well-developed branching of the mammary ducts, fewer terminal end buds and lower overall density of mammary gland structures in IL-5-deficient mice [98] (Table 1). Unexpectedly, overabundance of eosinophils in hypereosinophilic mice that express IL-5 retards mammary gland development [86], although the exact mechanisms remain to be elucidated.
Genetic Regulation of the Eosinophil
Eosinophils are produced in the bone marrow from pluripotent stem cells. The stem cells first differentiate into progenitors, which share properties of basophils and eosinophils, and then into a separate eosinophil lineage [99] (Fig. 2).
The development of eosinophils is determined by many interdependent regulatory events and transcription factors, including GATA-binding protein family (such as GATA1 and GATA2), CCAAT/enhancer-binding proteins (such as C/EBPα and C/EBPε), and PU.1 (a member of the E26-transformation-specific (ETS) family of transcription factors) [100, 101] (Fig. 2). Of above transcription factors, GATA-1 appears to be the most significant for the eosinophil lineage. GATA-1, a zinc finger family member, is named for its ability to bind the promoter sequence composed of the bases GATA. Mice with a targeted deletion of the double GATA-binding site of GATA-1 gene show a specific loss of eosinophil lineage [102]. The essential and instructive roles of GATA-1 in eosinophil development have also been confirmed by in vitro experiments [103, 104]. This double GATA site is present in numerous eosinophil-specific genes such as CC-chemokine receptor 3, granule protein genes, and IL-5 receptor alpha, and in the downstream GATA-1 promoter [102, 105, 106].
C/EBP-induced eosinophil differentiation can be separated into two distinct events, lineage commitment and maturation [100, 107]. Recently, it has been shown that both activator and repressor isoforms of C/EBPε can regulate the differentiation of human CD34+ progenitor cells into eosinophils in vitro [108]. PU.1 is generally considered as essential for the differentiation of monocytes/macrophages, dendritic cells, and neutrophils [105, 109, 110]. It has also been shown that graded expression of PU.1 determines distinct cell lineage fates, with low levels inducing lymphocytic and high levels myeloid differentiation. Functional interactions between GATA1 and PU.1 have been reported in eosinophil cell lines. GATA-1 and PU.1 synergistically regulate eosinophil lineage specification and eosinophil granule protein transcription [105].
Eosinophil development is modulated by the aforementioned transcription factors; subsequently, permissive differentiation and proliferation are regulated by IL-3, IL-5, and granulocyte-macrophage colony-stimulating factor (GM-CSF) [1]. Located on chromosome 5 in position q31, these three cytokines bind to receptor that shares the common beta chain, in addition to the unique alpha chains [111]. Of these three cytokines, IL-5 is the most specific and potent for selective differentiation of eosinophils [112]. Specifically, the critical function of IL-5 in eosinophil development has been demonstrated by genetic manipulation of mice [33, 113, 114]. IL-5 also stimulates the migration of eosinophils from the bone marrow to the circulation [115]. Several clinical trials with humanized anti-IL-5 antibody in humans have targeted the pivotal function of IL-5 in regulating eosinophils [116, 117]. Mepolizumab, a humanized monoclonal antibody (mAb) with potent IL-5 neutralizing effects, cause a substantial reduction in blood and sputum eosinophil numbers in the treatment of patients with asthma [118, 119]. Reslizumab, another monoclonal antibody directed against IL-5, has been in clinical trials for eosinophilic asthma and eosinophilic esophagitis. A monoclonal antibody directed against the IL-5 receptor, benralizumab, has also shown promise in the treatment of eosinophilic asthma [120]. Another approach directed at eosinophil-related genes has been to use antisense oligonucleotides to inhibit the expression of the common β-chain and of the chemokine receptor CCR3 in patients with eosinophilic asthma [121].
Epigenetic Regulation of the Eosinophil
Epigenetic mechanisms of gene regulation are important factors to orchestrate a tightly regulated pattern of gene expression. Epigenetics refers to stable and heritable changes in gene expression that do not involve changes in DNA sequence. The major mechanisms of epigenetic gene regulation include DNA methylation, histone modifications, and microRNA.
It was not until recently that epigenetics has been considered to be involved in eosinophil biology, but our understanding of the possible mechanisms remains limited. It has been shown that the development of eosinophils can be regulated by miR-21 and miR-223 [122, 123]. C/EBPα, highly expressed in granulocyte and monocyte progenitor cells, is a key transcription factor for eosinophils. Besides genetics, C/EBPα is subjected to regulation by a multifaceted molecular system. C/EBPα mRNA is a target of oncogenic miR-124a, which decreases expression level of C/EBPα in a posttranscriptional manner [124]. BCR-ABL suppresses C/EBPα expression through interaction with Poly(rC)-binding protein E2 (hnRNPE2) [125]. Inversely, this mechanism is counteracted by miR-328, which increases C/EBPα translation [126]. Another example is that deregulated expression levels of fms-liketyrosinekinase (FLT3) affects the phosphorylation of Ser21, which is needed for the transformation of the functional C/EBPα protein [127]. It is believed that the different mechanisms are highly interactive with each other.
The important roles of epigenetic dysregulation in complex diseases such as cancer, autoimmune diseases have been well documented. However, research into the epigenetic mechanisms of eosinophilic diseases is still at an early stage. Among these, asthma is a representative eosinophilic disease associated, at least partly, with epigenetic mechanisms, including DNA methylation and histone modifications. In BALB/c mice sensitized with chicken ovalbumin (OVA), airway hyperreactivity and pulmonary eosinophilia both diminished after treated with 5-azacytidine (Aza) [128]. Sun and colleagues [129] have identified that protein arginine methyltransferase-1 (PRMT1) plays an important role in asthma pathogenesis. In E3 rats sensitized with OVA, inhibition of PRMT1 ameliorates pulmonary inflammation and eosinophil infiltration in the Ag-induced pulmonary inflammation (AIPI).
Epigenetics is also implicated in the mechanisms of resistance to imatinib in patients with chronic eosinophilic leukemia (CEL) that initially responds to treatment with imatinib, which has been a conspicuous clinical problem. An imatinib-resistant EOL-1R cell line (EOL-1R) has been successfully established by Nishioka and colleagues [130] by culturing with increasing concentrations of sunitinib for 6 months. Treatment with antiepigenetic agents restores the expression of phosphatase and tensin homolog deleted on chromosome 10 (PTEN) in EOL-1R, resulting in the sensitization of this imatinib-resistant cell line to imatinib [130].
Hypereosinophilia and Human Diseases
Hypereosinophilia is a common disorder characterized by marked hypereosinophilia (>1500/mm3) with or without tissue damage, resulting in a variety of clinical manifestations. Hypereosinophilia can be divided into two categories clinically: blood hypereosinophilia and tissue hypereosinophilia, which can exist either alone or coincidently [131]. The most common diseases with hypereosinophilia are parasitic infections and allergic diseases such as drug allergy, food allergy, asthma, and atopic dermatitis. Hypereosinophilia can also be observed in some patients with HIV infection, and in some patients with coccidiomyocosis or aspergillosis, two types of fungal infectious diseases. Tissue hypereosinophilia in skin lesions may be identified in various eosinophilic dermatoses, and can occasionally be observed in cutaneous T cell lymphoma [132].
A series of clinical syndromes characterized by marked blood hypereosinophilia and (or) tissue hypereosinophilia with unknown cause have been documented. Among these entities, tissue hypereosinophilia may be observed in specific organs or systems, including the skin (eosinophilic cellulitis, eosinophilic fasciitis, eosinophilic pustular folliculitis, etc. [132]), gastrointestinal tract (eosinophilic esophagitis, eosinophilic gastroenteritis, and colitis), respiratory tract (eosinophilic asthma, eosinophilic pneumonia), and hematologic system (eosinophilic leukemia). Another rare group of eosinophilic diseases, featured by unexplained, persistent blood hypereosinophilia with or without tissue involvement in multiple organs or systems, are referred to as HES. The etiology and pathogenesis of these entities are still largely mysterious. Other chapters in this special issue will present detailed and comprehensive reviews on these clinical syndromes separately. Here, we only discuss the etiology and pathogenesis of hypereosinophilic syndrome as an example to facilitate a better understanding of how research progress has updated our knowledge into these rare eosinophilic disorders.
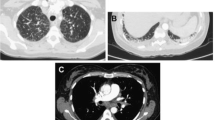
Hypereosinophilic Syndrome: a Collection of Eosinophilic Disorders with Distinct Molecular Bases
The term “hypereosinophilic syndrome” was first introduced in 1968 by Hardy and Anderson [133] to describe a rare condition characterized by unexplained, persistent peripheral hypereosinophilia associated with multiple organ involvement [134, 135]. It actually referred to a highly heterogeneous group of disorders with unknown cause at that time. This heterogeneity has been further validated by both clinical investigations and translational research into the etiology, which uncovered diverse genetic and cytological abnormalities associated with distinct subsets of hypereosinophilic syndrome.
Definition and Classification of HES
The definition and criteria of HES have been evolving with the progress of our understanding of the disease over the past decades, and details of the disease are still controversial with regard to certain aspects due to the complexity in nomenclature, criteria, and classification.
The original criteria was proposed by Chusid et al. [136] in 1975, which defines HES as a condition characterized by persistent blood eosinophilia (eosinophil count exceeding 1500/mm3) for at least 6 months with presumptive signs and symptoms of organ involvement, with parasitic, allergic, or other known causes of eosinophilia excluded.
An updated term, hypereosinophilic syndromes (HESs), was later thought to be a more relevant term for this group of rare diseases, because research advances have led to a brand new concept that HESs refer to a group of different entities with distinct etiologies and pathologies, instead of just a single disease with different clinical variants [137]. HESs can be subdivided into six different groups, which are myeloproliferative variants of HES, lymphocytic variants of HES, familial eosinophilia, overlap HES (referring to eosinophilic disease restricted to a single organ system), associated HES (eosinophilia ≥1.5 × 10/L in the setting of another diagnosis, such as sarcoidosis, Churg-Strauss syndrome, or inflammatory bowel disease), and undefined HES (referring to idiopathic HES with or without symptoms, including episodic variants), as proposed by the Hypereosinophilic Syndromes Working Group in 2006 [137].
In the past decade, several versions of criteria and classification algorithms for HES have been successively proposed by different groups; however, the taxonomy and definition of HES remain unstandardized among various fields of medicine. Thus, a recent, comprehensive, multidisciplinary consensus was achieved in the Year 2011 Working Conference on Eosinophil Disorders and Syndromes [138]. According to this consensus, HES is defined by the following three criteria: (1) blood eosinophil counts >1.5 × 109/L on two examinations (interval ≥1 month); and (2) organ damage and/or dysfunction attributable to tissue hypereosinophilia; and (3) exclusion of other disorders or conditions as the major reason for organ damage [138]. HES is further subdivided into three categories: idiopathic HES, primary or neoplastic HES (HESN), and secondary or reactive HES (HESR), each including a series of conditions. Specially, myeloproliferative HES and chronic eosinophilic leukemia (CEL) can be attributable to the HESN category, and lymphoid variant HES, for which clonal T cells is identified as the only potential cause, is deemed as a subvariant of HESR. Thus, the concept of HES has been largely updated and standardized [138]. However, challenges still remain because the etiologies and pathogenic mechanisms of many subsets of HES remain unclear.
Genetic and Molecular Basis of HES: Diverse Variants, Distinct Etiologies
The heterogeneity of HES was not appreciated until the distinct molecular mechanisms of certain subgroups of HES were uncovered in the past 15 years. Among these developments, identification of the etiologies underlying the myeloproliferative variant of HES and the lymphocytic variant of HES has been a milestone in the research history of HES [139].
One of the breakthroughs was the discovery of Fip1-like 1 (FIP1L1)/platelet-derived growth factor receptor alpha (PDGFRA), a novel fusion tyrosine kinase caused by a complex chromosomal abnormality, as the etiology of an HES subgroup that is now designated as the myeloproliferative variant of HES (M-HES) [140]. The inspiration of this investigation originated from the interesting observation that a subgroup of patients with HES showed amazingly good response to the treatment with imatinib mesylate [141], a tyrosine kinase inhibitor proven to be successful in treating chronic myeloid leukemia by targeting its oncogenic BCR-ABL tyrosine kinase. This prompted the hypothesis that an activated tyrosine kinase that can be targeted by imatinib, such as platelet-derived growth factor receptor (PDGFR), ABL, or KIT, might be the etiological cause in this subgroup of patients with HES. This inferred molecular basis was soon validated. In a series of patients with HES responsive to imatinib treatment, expression of the FIP1L1-PDGFRA fusion gene (shortly as F/P fusion), caused by a fusion of the FIP1L1 gene to the PDGFRA gene due to an interstitial deletion on chromosome 4q12, was detected in white blood cells [142]. As a constitutively activated tyrosine kinase, FIP1L1-PDGFRA was demonstrated to transform hematopoietic cells and contribute to the hypereosinophilia in HES [142, 143], which can be inhibited by imatinib.
FIP1L1-PDGFRA has been found to be present in the majority of patients with M-HES [144, 145]. However, M-HES also includes patients carrying some rare chromosomal abnormalities other than the FIP1L1-PDGFRA fusion gene [146], and those exhibiting clinical and biological signs of myeloproliferative disorders (e.g., hepatomegaly, splenomegaly, and cytopenia) without any identified genetic defect [134]. It should also be noted that many M-HES patients with detectable FIP1LI-PDGFRA fusion genes fulfill the current World Health Organization criteria for chronic eosinophilic leukemia (CEL) [147]. A considerable overlap between M-HES and CEL exists, and thus, these two entities are preferred to be classified into the same subtype of HES [137].
The other important advance has been the progress made in better understanding the lymphocytic variant of HES (L-HES) [148, 149]. Since the first reports of clonal expansion of CD3-CD4+ T cells in some patients with HES, evidence has shown that these phenotypically abnormal T cells produce large amounts of interleukin-5 (IL-5) [150, 151], a cytokine regulating the growth, differentiation, and activation of eosinophils [112, 152, 153]. It was later reported that clonal populations of T cells with aberrant immunophenotypes producing excessive amount of IL-5 occur in a proportion of patients with idiopathic eosinophilia [154]. The sustained overproduction of eosinophilopoietic cytokines, mainly IL-5, by clonal populations of activated T cell subsets with abnormal immunophenotypes, has become generally believed to be the driving cause of the secondary polyclonal eosinophilia in the lymphocytic variant of HES [155, 156].
Beyond that, chromosomal abnormalities have also been identified in familial eosinophilia [157], an autosomal dominant disorder characterized by marked eosinophilia and progression to end organ damage in some, but not all, affected family members [158]. The genetic defects have been mapped to chromosome 5q31-33. Familial eosinophilia is considered as a rare variant of HES [137].
Conclusion
These findings in the recent years have greatly refreshed the interpretation of the etiologies and pathogenic mechanisms of HES and have therefore lead to a brand-new concept of this group of rare disorders in terms of taxonomy, diagnostic methods, and therapeutic strategies. Identification of new genetic, molecular and immunologic mechanisms in those less studied subsets of HES is still in great need in order to better understand the role of eosinophils in health and disease.
The field of eosinophil biology has been hallmarked by revolutionized perspectives and emerging challenges. It has been increasingly acknowledged that eosinophils serve as pleiotropic multifunctional leukocytes. Eosinophil-related cytokines, chemokines, and growth factors may contribute to augment inflammatory responses in antiparasitic infection, allergy, and various other conditions, most of which calls for further studies to elucidate their mechanisms. A better understanding of eosinophil will aid in the development of new therapeutic strategies for diseases characterized by eosinophil dysregulation [159].
References
Rothenberg ME, Hogan SP (2006) The eosinophil. Annu Rev Immunol 24:147–174
Gleich GJ, Adolphson CR (1986) The eosinophilic leukocyte: structure and function. Adv Immunol 39:177–253
Hogan SP, Rosenberg HF, Moqbel R et al (2008) Eosinophils: biological properties and role in health and disease. Clin Exp Allergy 38:709–750
Yang YH, Chiang BL (2014) Novel approaches to food allergy. Clin Rev Allergy Immunol 46:250–257
Weinstock JV (2014) Do we need worms to promote immune health? Clin Rev Allergy Immunol 1–5. doi:10.1007/s12016-014-8458-3
Hansel TT, De Vries IJ, Iff T et al (1991) An improved immunomagnetic procedure for the isolation of highly purified human blood eosinophils. J Immunol Methods 145:105–110
Hansel TT, De Vries IJ, Carballido JM et al (1992) Induction and function of eosinophil intercellular adhesion molecule-1 and HLA-DR. J Immunol 149:2130–2136
Chu VT, Frohlich A, Steinhauser G et al (2011) Eosinophils are required for the maintenance of plasma cells in the bone marrow. Nat Immunol 12:151–159
Wu D, Molofsky AB, Liang HE et al (2011) Eosinophils sustain adipose alternatively activated macrophages associated with glucose homeostasis. Science 332:243–247
Samoszuk M (1997) Eosinophils and human cancer. Histol Histopathol 12:807–812
Meleg-Smith S, Gauthier PM (2005) Abundance of interstitial eosinophils in renal allografts is associated with vascular rejection. Transplantation 79:444–450
Trull AK, Akhlaghi F, Charman SC et al (2004) Immunosuppression, eotaxin and the diagnostic changes in eosinophils that precede early acute heart allograft rejection. Transpl Immunol 12:159–166
Hamann KJ, Barker RL, Ten RM, Gleich GJ (1991) The molecular biology of eosinophil granule proteins. Int Arch Allergy Appl Immunol 94:202–209
Lehrer RI, Szklarek D, Barton A, Ganz T, Hamann KJ, Gleich GJ (1989) Antibacterial properties of eosinophil major basic protein and eosinophil cationic protein. J Immunol 142:4428–4434
Gleich GJ, Loegering DA, Bell MP, Checkel JL, Ackerman SJ, McKean DJ (1986) Biochemical and functional similarities between human eosinophil-derived neurotoxin and eosinophil cationic protein: homology with ribonuclease. Proc Natl Acad Sci U S A 83:3146–3150
Young JD, Peterson CG, Venge P, Cohn ZA (1986) Mechanism of membrane damage mediated by human eosinophil cationic protein. Nature 321:613–616
Venge P, Bystrom J, Carlson M et al (1999) Eosinophil cationic protein (ECP): molecular and biological properties and the use of ECP as a marker of eosinophil activation in disease. Clin Exp Allergy 29:1172–1186
O’Donnell MC, Ackerman SJ, Gleich GJ, Thomas LL (1983) Activation of basophil and mast cell histamine release by eosinophil granule major basic protein. J Exp Med 157:1981–1991
Wasmoen TL, Bell MP, Loegering DA, Gleich GJ, Prendergast FG, McKean DJ (1988) Biochemical and amino acid sequence analysis of human eosinophil granule major basic protein. J Biol Chem 263:12559–12563
Agosti JM, Altman LC, Ayars GH, Loegering DA, Gleich GJ, Klebanoff SJ (1987) The injurious effect of eosinophil peroxidase, hydrogen peroxide, and halides on pneumocytes in vitro. J Allergy Clin Immunol 79:496–504
MacPherson JC, Comhair SA, Erzurum SC et al (2001) Eosinophils are a major source of nitric oxide-derived oxidants in severe asthma: characterization of pathways available to eosinophils for generating reactive nitrogen species. J Immunol 166:5763–5772
Wu W, Chen Y, Hazen SL (1999) Eosinophil peroxidase nitrates protein tyrosyl residues. Implications for oxidative damage by nitrating intermediates in eosinophilic inflammatory disorders. J Biol Chem 274:25933–25944
Lacy P, Stow JL (2011) Cytokine release from innate immune cells: association with diverse membrane trafficking pathways. Blood 118:9–18
Spencer LA, Melo RC, Perez SA, Bafford SP, Dvorak AM, Weller PF (2006) Cytokine receptor-mediated trafficking of preformed IL-4 in eosinophils identifies an innate immune mechanism of cytokine secretion. Proc Natl Acad Sci U S A 103:3333–3338
Rosenberg HF, Dyer KD, Foster PS (2013) Eosinophils: changing perspectives in health and disease. Nat Rev Immunol 13:9–22
Shamri R, Xenakis JJ, Spencer LA (2011) Eosinophils in innate immunity: an evolving story. Cell Tissue Res 343:57–83
Sriramarao P, von Andrian UH, Butcher EC, Bourdon MA, Broide DH (1994) L-selectin and very late antigen-4 integrin promote eosinophil rolling at physiological shear rates in vivo. J Immunol 153:4238–4246
Berg EL, McEvoy LM, Berlin C, Bargatze RF, Butcher EC (1993) L-selectin-mediated lymphocyte rolling on MAdCAM-1. Nature 366:695–698
Symon FA, Lawrence MB, Williamson ML, Walsh GM, Watson SR, Wardlaw AJ (1996) Functional and structural characterization of the eosinophil P-selectin ligand. J Immunol 157:1711–1719
Forbes E, Hulett M, Ahrens R et al (2006) ICAM-1-dependent pathways regulate colonic eosinophilic inflammation. J Leukoc Biol 80:330–341
Bochner BS, Schleimer RP (2001) Mast cells, basophils, and eosinophils: distinct but overlapping pathways for recruitment. Immunol Rev 179:5–15
Wang H, Rudd CE (2008) SKAP-55, SKAP-55-related and ADAP adaptors modulate integrin-mediated immune-cell adhesion. Trends Cell Biol 18:486–493
Mishra A, Hogan SP, Brandt EB et al (2002) Enterocyte expression of the eotaxin and interleukin-5 transgenes induces compartmentalized dysregulation of eosinophil trafficking. J Biol Chem 277:4406–4412
Artis D, Humphreys NE, Potten CS et al (2000) Beta7 integrin-deficient mice: delayed leukocyte recruitment and attenuated protective immunity in the small intestine during enteric helminth infection. Eur J Immunol 30:1656–1664
Nakajima H, Sano H, Nishimura T, Yoshida S, Iwamoto I (1994) Role of vascular cell adhesion molecule 1/very late activation antigen 4 and intercellular adhesion molecule 1/lymphocyte function-associated antigen 1 interactions in antigen-induced eosinophil and T cell recruitment into the tissue. J Exp Med 179:1145–1154
Pretolani M, Ruffie C, Lapa e Silva JR, Joseph D, Lobb RR, Vargaftig BB (1994) Antibody to very late activation antigen 4 prevents antigen-induced bronchial hyperreactivity and cellular infiltration in the guinea pig airways. J Exp Med 180:795–805
Okigami H, Takeshita K, Tajimi M et al (2007) Inhibition of eosinophilia in vivo by a small molecule inhibitor of very late antigen (VLA)-4. Eur J Pharmacol 559:202–209
Wang H, Tan X, Chang H, Huang W, Gonzalez-Crussi F, Hsueh W (1999) Platelet-activating factor receptor mRNA is localized in eosinophils and epithelial cells in rat small intestine: regulation by dexamethasone and gut flora. Immunology 97:447–454
Fujii M, Tanaka H, Abe S (2005) Interferon-gamma up-regulates expression of cysteinyl leukotriene type 2 receptors on eosinophils in asthmatic patients. Chest 128:3148–3155
Zinchuk O, Fukushima A, Zinchuk V, Fukata K, Ueno H (2005) Direct action of platelet activating factor (PAF) induces eosinophil accumulation and enhances expression of PAF receptors in conjunctivitis. Mol Vis 11:114–123
Thivierge M, Doty M, Johnson J, Stankova J, Rola-Pleszczynski M (2000) IL-5 up-regulates cysteinyl leukotriene 1 receptor expression in HL-60 cells differentiated into eosinophils. J Immunol 165:5221–5226
Hirai H, Tanaka K, Yoshie O et al (2001) Prostaglandin D2 selectively induces chemotaxis in T helper type 2 cells, eosinophils, and basophils via seven-transmembrane receptor CRTH2. J Exp Med 193:255–261
Sugimoto H, Shichijo M, Iino T et al (2003) An orally bioavailable small molecule antagonist of CRTH2, ramatroban (BAY u3405), inhibits prostaglandin D2-induced eosinophil migration in vitro. J Pharmacol Exp Ther 305:347–352
Barnes N, Pavord I, Chuchalin A et al (2012) A randomized, double-blind, placebo-controlled study of the CRTH2 antagonist OC000459 in moderate persistent asthma. Clin Exp Allergy 42:38–48
Elsner J, Dulkys Y, Gupta S et al (2005) Differential pattern of CCR1 internalization in human eosinophils: prolonged internalization by CCL5 in contrast to CCL3. Allergy 60:1386–1393
Phillips RM, Stubbs VE, Henson MR, Williams TJ, Pease JE, Sabroe I (2003) Variations in eosinophil chemokine responses: an investigation of CCR1 and CCR3 function, expression in atopy, and identification of a functional CCR1 promoter. J Immunol 170:6190–6201
Gong L, Wilhelm RS (2009) CCR3 antagonists: a survey of the patent literature. Expert Opin Ther Pat 19:1109–1132
Sullivan SK, McGrath DA, Liao F, Boehme SA, Farber JM, Bacon KB (1999) MIP-3alpha induces human eosinophil migration and activation of the mitogen-activated protein kinases (p42/p44 MAPK). J Leukoc Biol 66:674–682
Nagase H, Miyamasu M, Yamaguchi M et al (2000) Glucocorticoids preferentially upregulate functional CXCR4 expression in eosinophils. J Allergy Clin Immunol 106:1132–1139
Oliveira SH, Lira S, Martinez AC, Wiekowski M, Sullivan L, Lukacs NW (2002) Increased responsiveness of murine eosinophils to MIP-1beta (CCL4) and TCA-3 (CCL1) is mediated by their specific receptors, CCR5 and CCR8. J Leukoc Biol 71:1019–1025
Rothenberg ME, Pomerantz JL, Owen WF Jr et al (1988) Characterization of a human eosinophil proteoglycan, and augmentation of its biosynthesis and size by interleukin 3, interleukin 5, and granulocyte/macrophage colony stimulating factor. J Biol Chem 263:13901–13908
Wechsler ME, Fulkerson PC, Bochner BS et al (2012) Novel targeted therapies for eosinophilic disorders. J Allergy Clin Immunol 130:563–571
Zeck-Kapp G, Czech W, Kapp A (1994) TNF alpha-induced activation of eosinophil oxidative metabolism and morphology—comparison with IL-5. Exp Dermatol 3:176–188
Kvarnhammar AM, Cardell LO (2012) Pattern-recognition receptors in human eosinophils. Immunology 136:11–20
Wong CK, Cheung PF, Ip WK, Lam CW (2007) Intracellular signaling mechanisms regulating toll-like receptor-mediated activation of eosinophils. Am J Respir Cell Mol Biol 37:85–96
Nagase H, Okugawa S, Ota Y et al (2003) Expression and function of Toll-like receptors in eosinophils: activation by Toll-like receptor 7 ligand. J Immunol 171:3977–3982
Walsh GM, Hartnell A, Moqbel R et al (1990) Receptor expression and functional status of cultured human eosinophils derived from umbilical cord blood mononuclear cells. Blood 76:105–111
Giembycz MA, Lindsay MA (1999) Pharmacology of the eosinophil. Pharmacol Rev 51:213–340
Koenderman L, Kuijpers TW, Blom M, Tool AT, Roos D, Verhoeven AJ (1991) Characteristics of CR3-mediated aggregation in human eosinophils: effect of priming by platelet-activating factor. J Allergy Clin Immunol 87:947–954
Kita H, Gleich GJ (1997) Eosinophils and IgE receptors: a continuing controversy. Blood 89:3497–3501
Seminario MC, Saini SS, MacGlashan DW Jr, Bochner BS (1999) Intracellular expression and release of Fc epsilon RI alpha by human eosinophils. J Immunol 162:6893–6900
Kita H, Kaneko M, Bartemes KR et al (1999) Does IgE bind to and activate eosinophils from patients with allergy? J Immunol 162:6901–6911
Ying S, Barata LT, Meng Q et al (1998) High-affinity immunoglobulin E receptor (Fc epsilon RI)-bearing eosinophils, mast cells, macrophages and Langerhans’ cells in allergen-induced late-phase cutaneous reactions in atopic subjects. Immunology 93:281–288
Lucey DR, Nicholson-Weller A, Weller PF (1989) Mature human eosinophils have the capacity to express HLA-DR. Proc Natl Acad Sci U S A 86:1348–1351
Mawhorter SD, Kazura JW, Boom WH (1994) Human eosinophils as antigen-presenting cells: relative efficiency for superantigen- and antigen-induced CD4+ T-cell proliferation. Immunology 81:584–591
Celestin J, Rotschke O, Falk K et al (2001) IL-3 induces B7.2 (CD86) expression and costimulatory activity in human eosinophils. J Immunol 167:6097–6104
Shi HZ, Humbles A, Gerard C, Jin Z, Weller PF (2000) Lymph node trafficking and antigen presentation by endobronchial eosinophils. J Clin Invest 105:945–953
Duez C, Dakhama A, Tomkinson A et al (2004) Migration and accumulation of eosinophils toward regional lymph nodes after airway allergen challenge. J Allergy Clin Immunol 114:820–825
Tamura N, Ishii N, Nakazawa M et al (1996) Requirement of CD80 and CD86 molecules for antigen presentation by eosinophils. Scand J Immunol 44:229–238
Wang HB, Ghiran I, Matthaei K, Weller PF (2007) Airway eosinophils: allergic inflammation recruited professional antigen-presenting cells. J Immunol 179:7585–7592
MacKenzie JR, Mattes J, Dent LA, Foster PS (2001) Eosinophils promote allergic disease of the lung by regulating CD4(+) Th2 lymphocyte function. J Immunol 167:3146–3155
Padigel UM, Hess JA, Lee JJ et al (2007) Eosinophils act as antigen-presenting cells to induce immunity to Strongyloides stercoralis in mice. J Infect Dis 196:1844–1851
van Rijt LS, Vos N, Hijdra D, de Vries VC, Hoogsteden HC, Lambrecht BN (2003) Airway eosinophils accumulate in the mediastinal lymph nodes but lack antigen-presenting potential for naive T cells. J Immunol 171:3372–3378
Zheutlin LM, Ackerman SJ, Gleich GJ, Thomas LL (1984) Stimulation of basophil and rat mast cell histamine release by eosinophil granule-derived cationic proteins. J Immunol 133:2180–2185
Piliponsky AM, Gleich GJ, Bar I, Levi-Schaffer F (2002) Effects of eosinophils on mast cells: a new pathway for the perpetuation of allergic inflammation. Mol Immunol 38:1369
Wong CK, Ng SS, Lun SW, Cao J, Lam CW (2009) Signalling mechanisms regulating the activation of human eosinophils by mast-cell-derived chymase: implications for mast cell-eosinophil interaction in allergic inflammation. Immunology 126:579–587
Matsuba-Kitamura S, Yoshimoto T, Yasuda K et al (2010) Contribution of IL-33 to induction and augmentation of experimental allergic conjunctivitis. Int Immunol 22:479–489
Solomon A, Aloe L, Pe’er J et al (1998) Nerve growth factor is preformed in and activates human peripheral blood eosinophils. J Allergy Clin Immunol 102:454–460
Bullock ED, Johnson EM Jr (1996) Nerve growth factor induces the expression of certain cytokine genes and bcl-2 in mast cells. Potential role in survival promotion. J Biol Chem 271:27500–27508
Horigome K, Bullock ED, Johnson EM Jr (1994) Effects of nerve growth factor on rat peritoneal mast cells. Survival promotion and immediate-early gene induction. J Biol Chem 269:2695–2702
Throsby M, Herbelin A, Pleau JM, Dardenne M (2000) CD11c + eosinophils in the murine thymus: developmental regulation and recruitment upon MHC class I-restricted thymocyte deletion. J Immunol 165:1965–1975
Tulic MK, Sly PD, Andrews D et al (2009) Thymic indoleamine 2,3-dioxygenase-positive eosinophils in young children: potential role in maturation of the naive immune system. Am J Pathol 175:2043–2052
Matthews AN, Friend DS, Zimmermann N et al (1998) Eotaxin is required for the baseline level of tissue eosinophils. Proc Natl Acad Sci U S A 95:6273–6278
Fulkerson PC, Fischetti CA, McBride ML, Hassman LM, Hogan SP, Rothenberg ME (2006) A central regulatory role for eosinophils and the eotaxin/CCR3 axis in chronic experimental allergic airway inflammation. Proc Natl Acad Sci U S A 103:16418–16423
Kim HJ, Alonzo ES, Dorothee G, Pollard JW, Sant’Angelo DB (2010) Selective depletion of eosinophils or neutrophils in mice impacts the efficiency of apoptotic cell clearance in the thymus. PLoS One 5, e11439
Sferruzzi-Perri AN, Robertson SA, Dent LA (2003) Interleukin-5 transgene expression and eosinophilia are associated with retarded mammary gland development in mice. Biol Reprod 69:224–233
Robertson SA, Mau VJ, Young IG, Matthaei KI (2000) Uterine eosinophils and reproductive performance in interleukin 5-deficient mice. J Reprod Fertil 120:423–432
Zhang J, Lathbury LJ, Salamonsen LA (2000) Expression of the chemokine eotaxin and its receptor, CCR3, in human endometrium. Biol Reprod 62:404–411
Gouon-Evans V, Pollard JW (2001) Eotaxin is required for eosinophil homing into the stroma of the pubertal and cycling uterus. Endocrinology 142:4515–4521
Gouon-Evans V, Lin EY, Pollard JW (2002) Requirement of macrophages and eosinophils and their cytokines/chemokines for mammary gland development. Breast Cancer Res 4:155–164
Knudsen UB, Uldbjerg N, Rechberger T, Fredens K (1997) Eosinophils in human cervical ripening. Eur J Obstet Gynecol Reprod Biol 72:165–168
Timmons BC, Fairhurst AM, Mahendroo MS (2009) Temporal changes in myeloid cells in the cervix during pregnancy and parturition. J Immunol 182:2700–2707
Robertson SA, Mau VJ, Hudson SN, Tremellen KP (1997) Cytokine-leukocyte networks and the establishment of pregnancy. Am J Reprod Immunol 37:438–442
De M, Choudhuri R, Wood GW (1991) Determination of the number and distribution of macrophages, lymphocytes, and granulocytes in the mouse uterus from mating through implantation. J Leukoc Biol 50:252–262
Maddox DE, Kephart GM, Coulam CB, Butterfield JH, Benirschke K, Gleich GJ (1984) Localization of a molecule immunochemically similar to eosinophil major basic protein in human placenta. J Exp Med 160:29–41
Wagner JM, Hustin J, Bonno M, Kephart GM, Gurian KV, Gleich GJ (1994) Pregnancy-associated major basic protein: deposition of protein and expression of mRNA at the maternal-fetal junction in early and late gestation. Placenta 15:625–640
Gouon-Evans V, Rothenberg ME, Pollard JW (2000) Postnatal mammary gland development requires macrophages and eosinophils. Development 127:2269–2282
Colbert DC, McGarry MP, O’Neill K, Lee NA, Lee JJ (2005) Decreased size and survival of weanling mice in litters of IL-5-/ -mice are a consequence of the IL-5 deficiency in nursing dams. Contemp Top Lab Anim Sci 44:53–55
Boyce JA, Friend D, Matsumoto R, Austen KF, Owen WF (1995) Differentiation in vitro of hybrid eosinophil/basophil granulocytes: autocrine function of an eosinophil developmental intermediate. J Exp Med 182:49–57
Nerlov C, Graf T (1998) PU.1 induces myeloid lineage commitment in multipotent hematopoietic progenitors. Genes Dev 12:2403–2412
McNagny K, Graf T (2002) Making eosinophils through subtle shifts in transcription factor expression. J Exp Med 195:F43–F47
Yu C, Cantor AB, Yang H et al (2002) Targeted deletion of a high-affinity GATA-binding site in the GATA-1 promoter leads to selective loss of the eosinophil lineage in vivo. J Exp Med 195:1387–1395
Hirasawa R, Shimizu R, Takahashi S et al (2002) Essential and instructive roles of GATA factors in eosinophil development. J Exp Med 195:1379–1386
Iwasaki H, Mizuno S, Mayfield R et al (2005) Identification of eosinophil lineage-committed progenitors in the murine bone marrow. J Exp Med 201:1891–1897
Du J, Stankiewicz MJ, Liu Y et al (2002) Novel combinatorial interactions of GATA-1, PU.1, and C/EBPepsilon isoforms regulate transcription of the gene encoding eosinophil granule major basic protein. J Biol Chem 277:43481–43494
Zimmermann N, Daugherty BL, Kavanaugh JL, El-Awar FY, Moulton EA, Rothenberg ME (2000) Analysis of the CC chemokine receptor 3 gene reveals a complex 5′ exon organization, a functional role for untranslated exon 1, and a broadly active promoter with eosinophil-selective elements. Blood 96:2346–2354
Nerlov C, McNagny KM, Doderlein G, Kowenz-Leutz E, Graf T (1998) Distinct C/EBP functions are required for eosinophil lineage commitment and maturation. Genes Dev 12:2413–2423
Bedi R, Du J, Sharma AK, Gomes I, Ackerman SJ (2009) Human C/EBP-epsilon activator and repressor isoforms differentially reprogram myeloid lineage commitment and differentiation. Blood 113:317–327
DeKoter RP, Singh H (2000) Regulation of B lymphocyte and macrophage development by graded expression of PU.1. Science 288:1439–1441
Walsh JC, DeKoter RP, Lee HJ et al (2002) Cooperative and antagonistic interplay between PU.1 and GATA-2 in the specification of myeloid cell fates. Immunity 17:665–676
Vadas M, Lopez A, Gamble J et al (1994) Cytokines and allergy. J Allergy Clin Immunol 94:1289–1293
Sanderson CJ (1992) Interleukin-5, eosinophils, and disease. Blood 79:3101–3109
Lee JJ, McGarry MP, Farmer SC et al (1997) Interleukin-5 expression in the lung epithelium of transgenic mice leads to pulmonary changes pathognomonic of asthma. J Exp Med 185:2143–2156
Owen WF, Rothenberg ME, Petersen J et al (1989) Interleukin 5 and phenotypically altered eosinophils in the blood of patients with the idiopathic hypereosinophilic syndrome. J Exp Med 170:343–348
Collins PD, Marleau S, Griffiths-Johnson DA, Jose PJ, Williams TJ (1995) Cooperation between interleukin-5 and the chemokine eotaxin to induce eosinophil accumulation in vivo. J Exp Med 182:1169–1174
Leckie MJ, ten Brinke A, Khan J et al (2000) Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet 356:2144–2148
Kips JC, O’Connor BJ, Langley SJ et al (2003) Effect of SCH55700, a humanized anti-human interleukin-5 antibody, in severe persistent asthma: a pilot study. Am J Respir Crit Care Med 167:1655–1659
Iikura M, Hojo M, Sugiyama H (2014) Glucocorticoids and mepolizumab in eosinophilic asthma. N Engl J Med 371:2433–2434
Walsh GM (2009) Mepolizumab and eosinophil-mediated disease. Curr Med Chem 16:4774–4778
Castro M, Wenzel SE, Bleecker ER et al (2014) Benralizumab, an anti-interleukin 5 receptor alpha monoclonal antibody, versus placebo for uncontrolled eosinophilic asthma: a phase 2b randomised dose-ranging study. Lancet Respir Med 2:879–890
Allakhverdi Z, Allam M, Guimond A et al (2006) Multitargeted approach using antisense oligonucleotides for the treatment of asthma. Ann N Y Acad Sci 1082:62–73
Wong CK, Lau KM, Chan IH et al (2013) MicroRNA-21* regulates the prosurvival effect of GM-CSF on human eosinophils. Immunobiology 218:255–262
Lu TX, Lim EJ, Besse JA et al (2013) MiR-223 deficiency increases eosinophil progenitor proliferation. J Immunol 190:1576–1582
Hackanson B, Bennett KL, Brena RM et al (2008) Epigenetic modification of CCAAT/enhancer binding protein alpha expression in acute myeloid leukemia. Cancer Res 68:3142–3151
Perrotti D, Cesi V, Trotta R et al (2002) BCR-ABL suppresses C/EBPalpha expression through inhibitory action of hnRNP E2. Nat Genet 30:48–58
Eiring AM, Harb JG, Neviani P et al (2010) miR-328 functions as an RNA decoy to modulate hnRNP E2 regulation of mRNA translation in leukemic blasts. Cell 140:652–665
Radomska HS, Basseres DS, Zheng R et al (2006) Block of C/EBP alpha function by phosphorylation in acute myeloid leukemia with FLT3 activating mutations. J Exp Med 203:371–381
Wu CJ, Yang CY, Chen YH, Chen CM, Chen LC, Kuo ML (2013) The DNA methylation inhibitor 5-azacytidine increases regulatory T cells and alleviates airway inflammation in ovalbumin-sensitized mice. Int Arch Allergy Immunol 160:356–364
Sun Q, Yang X, Zhong B et al (2012) Upregulated protein arginine methyltransferase 1 by IL-4 increases eotaxin-1 expression in airway epithelial cells and participates in antigen-induced pulmonary inflammation in rats. J Immunol 188:3506–3512
Nishioka C, Ikezoe T, Yang J, Yokoyama A (2010) Long-term exposure of leukemia cells to multi-targeted tyrosine kinase inhibitor induces activations of AKT, ERK and STAT5 signaling via epigenetic silencing of the PTEN gene. Leukemia 24:1631–1640
Gotlib J (2014) World Health Organization-defined eosinophilic disorders: 2014 update on diagnosis, risk stratification, and management. Am J Hematol 89:325–337
Long H, Zhang G, Wang L, Lu Q (2015) Eosinophilic skin diseases: a comprehensive review. Clin Rev Allergy Immunol 1–25. doi:10.1007/s12016-015-8485-8
Hardy WR, Anderson RE (1968) The hypereosinophilic syndromes. Ann Intern Med 68:1220–1229
Simon HU, Rothenberg ME, Bochner BS et al (2010) Refining the definition of hypereosinophilic syndrome. J Allergy Clin Immunol 126:45–49
Cogan E, Roufosse F (2012) Clinical management of the hypereosinophilic syndromes. Expert Rev Hematol 5:275–289
Chusid MJ, Dale DC, West BC, Wolff SM (1975) The hypereosinophilic syndrome: analysis of fourteen cases with review of the literature. Medicine (Baltimore) 54:1–27
Klion AD, Bochner BS, Gleich GJ et al (2006) Approaches to the treatment of hypereosinophilic syndromes: a workshop summary report. J Allergy Clin Immunol 117:1292–1302
Valent P, Klion AD, Horny HP et al (2012) Contemporary consensus proposal on criteria and classification of eosinophilic disorders and related syndromes. J Allergy Clin Immunol 130:607–612
Roufosse F, Goldman M, Cogan E (2006) Hypereosinophilic syndrome: lymphoproliferative and myeloproliferative variants. Semin Respir Crit Care Med 27:158–170
Klion AD (2005) Recent advances in the diagnosis and treatment of hypereosinophilic syndromes. Hematol Am Soc Hematol Educ Prog 1:209–214
Gleich GJ, Leiferman KM, Pardanani A, Tefferi A, Butterfield JH (2002) Treatment of hypereosinophilic syndrome with imatinib mesilate. Lancet 359:1577–1578
Cools J, DeAngelo DJ, Gotlib J et al (2003) A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med 348:1201–1214
Stone RM, Gilliland DG, Klion AD (2004) Platelet-derived growth factor receptor inhibition to treat idiopathic hypereosinophilic syndrome. Semin Oncol 31:12–17
Pardanani A, Ketterling RP, Li CY et al (2006) FIP1L1-PDGFRA in eosinophilic disorders: prevalence in routine clinical practice, long-term experience with imatinib therapy, and a critical review of the literature. Leuk Res 30:965–970
Ogbogu PU, Bochner BS, Butterfield JH et al (2009) Hypereosinophilic syndrome: a multicenter, retrospective analysis of clinical characteristics and response to therapy. J Allergy Clin Immunol 124:1319–1325, e1313
Curtis CE, Grand FH, Musto P et al (2007) Two novel imatinib-responsive PDGFRA fusion genes in chronic eosinophilic leukaemia. Br J Haematol 138:77–81
Bain BJ (2004) Relationship between idiopathic hypereosinophilic syndrome, eosinophilic leukemia, and systemic mastocytosis. Am J Hematol 77:82–85
Roufosse F, Cogan E, Goldman M (2007) Lymphocytic variant hypereosinophilic syndromes. Immunol Allergy Clin North Am 27:389–413
Kahn JE, Bletry O, Guillevin L (2008) Hypereosinophilic syndromes. Best Pract Res Clin Rheumatol 22:863–882
Brugnoni D, Airo P, Rossi G et al (1996) A case of hypereosinophilic syndrome is associated with the expansion of a CD3-CD4+ T-cell population able to secrete large amounts of interleukin-5. Blood 87:1416–1422
Cogan E, Schandene L, Crusiaux A, Cochaux P, Velu T, Goldman M (1994) Brief report: clonal proliferation of type 2 helper T cells in a man with the hypereosinophilic syndrome. N Engl J Med 330:535–538
Lopez AF, Sanderson CJ, Gamble JR, Campbell HD, Young IG, Vadas MA (1988) Recombinant human interleukin 5 is a selective activator of human eosinophil function. J Exp Med 167:219–224
Corren J (2012) Inhibition of interleukin-5 for the treatment of eosinophilic diseases. Discov Med 13:305–312
Simon HU, Plotz SG, Dummer R, Blaser K (1999) Abnormal clones of T cells producing interleukin-5 in idiopathic eosinophilia. N Engl J Med 341:1112–1120
Vassina EM, Yousefi S, Simon D, Zwicky C, Conus S, Simon HU (2006) cIAP-2 and survivin contribute to cytokine-mediated delayed eosinophil apoptosis. Eur J Immunol 36:1975–1984
Klion A (2009) Hypereosinophilic syndrome: current approach to diagnosis and treatment. Annu Rev Med 60:293–306
Rioux JD, Stone VA, Daly MJ et al (1998) Familial eosinophilia maps to the cytokine gene cluster on human chromosomal region 5q31-q33. Am J Hum Genet 63:1086–1094
Klion AD, Law MA, Riemenschneider W et al (2004) Familial eosinophilia: a benign disorder? Blood 103:4050–4055
Sriaroon P, Ballow M (2014) Biological modulators in eosinophilic diseases. Clin Rev Allergy Immunol 1–21. doi:10.1007/s12016-014-8444-9
Kopf M, Brombacher F, Hodgkin PD et al (1996) IL-5-deficient mice have a developmental defect in CD5+ B-1 cells and lack eosinophilia but have normal antibody and cytotoxic T cell responses. Immunity 4:15–24
Yoshida T, Ikuta K, Sugaya H et al (1996) Defective B-1 cell development and impaired immunity against Angiostrongylus cantonensis in IL-5R alpha-deficient mice. Immunity 4:483–494
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 81220108017, No. 81430074, No. 81301357, and No. 81270024), the Ph.D. Programs Foundation of Ministry of Education of China (No. 20120162130003), the Natural Science Foundation of Hunan Province of China (13JJ4025), and the National Key Clinical Speciality Construction Project of National Health and Family Planning Commission of the People’s Republic of China.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Wei Liao and Hai Long contributed equally to this work.
Rights and permissions
About this article
Cite this article
Liao, W., Long, H., Chang, C.CC. et al. The Eosinophil in Health and Disease: from Bench to Bedside and Back. Clinic Rev Allerg Immunol 50, 125–139 (2016). https://doi.org/10.1007/s12016-015-8507-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-015-8507-6