Abstract
The objective of the study is to investigate and analyze clinicopathological features of gastrointestinal stromal tumor (GIST) and relevant prognostic factors. Between September 2008 and April 2014, 168 patients who presented with pathologically confirmed GIST and underwent surgical resection of the tumors in our institution were included in this study. A retrospective study on clinicopathological features of the disease and follow-up study on 1-year, 3-year, and 5-year survival rates were performed. Of 168 patients, 113 were males and 55 females of age ranging from 18 to 78 years (mean age 52.6 ± 10.1 years). Seventy patients (41.7 %) presented abdominal distension, 74 (44.0 %) abdominal pain, and 82 (48.8 %) bloody stools. Of all patients, 115 (68.4 %) developed tumors in GI tract, 51 (30.4 %) presented multiple tumors, 88 (52.4 %) tumors displayed a maximal diameter >5 cm, mitotic count >5/50HPF were observed in 80 patients. Positive rate of CD117 was 92.9 % (156/12), DOG1 97.0 % (163/5), CD34 53.0 % (89/79) and S-100 25.6 % (43/125). Follow-up study achieved in 149 patients. Survival analysis and Cox regression analysis demonstrated that no significant prognostic effects were observed for gender, clinical presentations, tumor location, number of tumors, CD34 and S-100 expression (p > 0.05). However, tumor diameter and mitotic count were factors with significant effect on prognosis of GIST (p < 0.05). Tumors with diameter >5 cm and mitotic count ≥5/50HPF resulted in poor prognosis. Common symptoms of GIST include abdominal pain and blood stools. Tumor diameter and mitotic count are helpful for the evaluation of prognosis with favorable clinical value.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastrointestinal stromal tumors (GISTs) [1, 2] are mesenchymal tumors arising from the wall of the gastrointestinal (GI) tract, accounting for 1–3 % of malignancies of GI tract and majority of mesenchymal tumors of alimentary cannel. GISTs mainly affect middle aged to elderly adults, but are uncommonly seen in patients younger than 40 and with no significant gender predilection. GISTs rarely occur in the mesentery, omentum, and retroperitoneum. The majority of GISTs are seen in the stomach (50–70 %) as well as in the small intestine (20–30 %), and 0–6 % of GISTs are located in the esophagus and 10–20 % in the colon and the rectum. Currently, surgery still remains a radical treatment of GISTs [3]. Due to the fact that 20–30 % of GISTs are malignant and 11–47 % of patients show metastases at the first clinical visit, the study on prognostic factors has significant implications for GIST treatment. In the present study, a retrospective study and follow-up study are conducted on 168 patients with GISTs to investigate and analyze clinicopathological features and relevant prognostic factors of GISTs, aiming to provide evidence for guiding clinical treatment of GISTs.
Materials and Methods
Patients
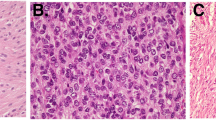
Between September 2008 and April 2014, 168 patients who presented with pathologically confirmed GIST and underwent surgical resection in our institution were included in this study. All patients were evaluated according to standard diagnostic criteria [4, 5]. Tumors primarily located in GI tract with spindle, pleomorphic or epithelioid tumor cells, and CD117 positivity was confirmed as GIST. Patients with other severe diseases or other epithelial, myogenic, and neurogenic tumors as well as lymphatic system tumors within the past 5 years were excluded.
Clinical Data and Parameters
(1) General conditions of patients including gender, age, and rate of abdominal distension, abdominal pain as well as bloody stool were recorded.
(2) Pathological data were documented, including location of tumor, number of tumors, tumor size, mitotic count (count in 50 randomly selected high power fields (HPF)), and positive rate of CD34, CD117, DOG1, S-100 (samples are considered positive when >10 % of cells display positive immunohistochemical staining).
(3) Survival parameters including time of death and survival time were obtained.
Data Collection
General conditions and pathological data were collected from clinical medial record and pathological examination record of patients. Surgically resected specimens were tested for CD34, CD117, DOG1, Ki67 and S-100 proteins using S-P immunohistochemical staining, and mitotic activity was recorded under microscopic observation. Survival data were obtained by telephoning with patients every 6 months during follow-up, which lasted over 5 years (range 6–64 months). Follow-up study was achieved in 149 patients with each receiving at least one follow-up study.
Statistical Study
Statistical analysis was performed using SPSS software version 17.0. Qualitative data were presented by number of cases or ratio of composition. Survival analysis and univariate analysis were performed using Kaplan–Meier method and Log-rank test. Multivariate analysis on factors affecting survival was carried out using Cox proportional hazards regression model. The best model was determined using stepwise regression. An α = 0.05 was considered as significant.
Results
Clinical Characteristics of Patients with GIST
GIST is characterized by non-specific symptoms manifested by abdominal distension, abdominal pain, and bloody stools. Of 168 patients in this study, 113 were males and 55 females of age ranging from 18 to 78 years (mean age 52.6 ± 10.1 years). Seventy patients (41.7 %) presented abdominal distension, 74 (44.0 %) abdominal pain, and 82 (48.8 %) bloody stools (Table 1).
Pathological Features of Patients with GIST
Macroscopic observation revealed that 115 out of 168 patients (68.4 %) developed tumors in GI tract and 53 patients developed tumors at other sites. Multiple tumors were revealed in 51 patients (30.4 %) and single tumor in 117 patients. Eighty-eight (52.4 %) tumors demonstrated a maximal diameter >5 cm. Immunohistochemical staining showed that mitotic count >5/50HPF was observed in 80 patients. Positive rate of CD117 was 92.9 % (156/12), DOG1 97.0 % (163/5), CD34 53.0 % (89/79) and S-100 25.6 % (43/125). (Table 2).
Survival Analysis
Overall Survival (OS)
A follow-up study over 5 years was carried out in 168 patients and achieved in 149 patients. The results showed that 1-year, 3-year, and 5-year OS rates were 83.9, 56.1, and 36.9 %, respectively, with mean survival of 41.4 months and median survival of 42.1 months. Survival data and survival rate are presented in Table 3 and OS curve is presented in Fig. 1.
Univariate Analysis on Factors Affecting Survival
Univariate analysis was performed on more than ten factors affecting survival, including gender, abdominal distension and other factors. The result showed that the group of tumors with maximal diameter >5 cm and mitotic count ≥ 5/50HPF demonstrated poorer prognosis than controls (p < 0.05). However, gender, clinical presentations, tumor location, number of tumors, and expression of CD34 as well as S-100 proteins had no significant effect on prognosis of patients (p > 0.05) (Table 4).
Comprehensive Analysis on Factors Affecting Survival—Cox Model Analysis
Parameters/factors presented in Table 4 with smaller p values served as covariates and were included in the analysis using Cox proportional hazard model. Variable assignment: X1 = maximal tumor diameter (1 = >5, 0 = ≤5), X2 = mitotic count (1 = >5; 0 = ≤5), X3 = CD34 protein expression (1 = positive, 0 = negative), X4 = S-100 expression (1 = positive, 0 = negative), t = survival time (months), variable Y = patient outcome (1 = censored survival, 0 = death). Data were screened using multivariate stepwise regression analysis (entry level of 0.05, removal level of 0.10). Results are presented in Table 5.
The results in Table 5 demonstrate that mitotic count (increased count) was the most important factor associated patient survival (a risk factor for death) with relative risk reaching 8.381, followed by maximal tumor diameter. Tumor with larger size exhibits higher risk for death with relative risk reaching 3.881. CD34 protein expression displayed no significant impact, however, the p value was smaller and relative risk reached 2.812. S-100 protein expression was not a factor affecting survival and was removed by screening.
Discussion
GIST has no specific clinical manifestations and main symptoms are associated with tumor location and size. Clinical course of the disease can vary from several days to over 20 years. Patients with early stage tumor or benign tumor present no symptom, whereas those with malignancies experience short clinical course of several months mostly [6]. Common symptoms of GISTs include GI bleeding, dysphagia and discomfort with swallowing in patients with GIST at the gastric cardia. Some patients seek treatment due to perforation of ulcer, which may increase the risk for tumor cell seeding in peritoneal cavity and local recurrence of tumor. These patients usually present several common symptoms, including abdominal pain, masses, GI bleeding and GI obstruction, and subsequent development of the disease is difficult to predict. It has been reported in literature [7, 8] that tumor recurrence or metastasis still occurred several years after surgical resection of benign GISTs. Hence, accurate evaluation of prognosis is extremely crucial to guiding clinical treatment. In the present study, a retrospective study on clinicopathological features of the disease and follow-up survival analysis were conducted on 168 patients with GISTs, in an effort to investigate the relationship between clinicopathological features and survival rate the disease.
The results of this study showed that symptoms including abdominal distension, abdominal pain, and bloody stools, despite its non-specificity, were common clinical manifestations of GIST. In the present study, 68.4 % of patients developed tumors in GI tract, 30.4 % were multiple tumors and 52.4 % of patients developed tumors with maximal diameter >5 cm, indicating that GISTs mostly occurred in the stomach and small intestine and majorities were single tumor with maximal diameter >5 cm [9]. Diagnosis of GIST relies on clinicopathological features of the disease. CD117, product of C-kit gene, shows good sensitivity and specificity for the diagnosis of GIST. DOG1, known also as TMEM16A and ANO1, is currently considered the most specific and sensitive marker of GIST, partly because its expression does not depend on mutations in the c-kit or PDGFRA genes, and partly because of its expression in CD117-negative cases. In addition, CD34 and S-100 can serve as ancillary studies for differential diagnosis [10, 11]. CD34, known as an antigen marker for stem cells, presents on hematopoietic stem cells in bone marrow. CD34 expression in GIST can reach over 80 % and its presence suggests that GIST is originated from and closely related to primitive and undifferentiated mesenchymal stem cells. S-100 expression is weak in GIST, displaying scattered and focal expression. The results of this study confirmed that CD34 positivity reached 53.0 %, CD117 92.9 %, DOG1 97.0 % and S-100 25.6 %. During over 5-year follow-up study, survival analysis was performed by determining 1-year, 3-year, and 5-year survival rates and assessing the relationship between clinicopathological features of the disease and survival rate. The results demonstrated that prognostic effect of immunohistochemical parameters, such as CD34, CD117, DOG1 and S-100, is uncertain and they can only serve as ancillary parameters for diagnosis. However, maximal tumor diameter and mitotic count are factors affecting prognosis of GIST. Tumors with longer tumor diameter and higher mitotic count, especially the latter, resulted in poorer prognosis, which is consistent with the results of most studies [11, 12].
In conclusion, clinicopathological features including abdominal distension, abdominal pain, bloody stools, tumor location, and number of tumors, tumor diameter, and results of immunohistochemical studies help with the diagnosis of GIST. In addition, tumor diameter and mitotic count are factors affecting GIST prognosis. In clinical practice, precautions should be taken when treating patients with abdominal discomfort and bloody stools, to achieve early detection, early treatment, and improve post therapeutic survival.
References
Zhao, X., & Yue, C. (2012). Gastrointestinal stromal tumor. Journal of Gastrointestinal Oncology, 3(3), 189–208.
Minarik, G., Plank, L., Lasabova, Z., et al. (2013). Spectrum of mutations in gastrointestinal stromal tumor patients—a population-based study from Slovakia. APMIS, 121(6), 539–548.
Lu, Z. H., Wu, X. J., Fang, Y. J., et al. (2011). Surgical treatment and prognosis of gastrointestinal stromal tumor. Zhonghua Wei Chang Wai Ke Za Zhi, 14(10), 778–780.
Chou, Y. H., Tu, C. C., Huang, C. C., et al. (2011). A clinically-occult gastrointestinal stromal tumor in a Meckel’s diverticulum presenting as hollow organ perforation. Chang Gung Medical Journal, 34(6 Suppl), 56–61.
Pera, M., Iglesias, M., Puig, S., et al. (2011). A sporadic multiple gastrointestinal stromal tumor with unique clinical and molecular features. Human Pathology, 42(8), 1194–1199.
Joensuu, H., Eriksson, M., Sundby, H. K., et al. (2012). One vs three years of adjuvant imatinib for operable gastrointestinal stromal tumor: A randomized trial. Journal of the American Medical Association, 307(12), 1265–1272.
Rutkowski, P., Wozniak, A., Debiec-Rychter, M., et al. (2011). Clinical utility of the new American Joint Committee on Cancer staging system for gastrointestinal stromal tumors: Current overall survival after primary tumor resection. Cancer, 117(21), 4916–4924.
Wang, C. Z., Hou, Y. Y., Shen, K. T., et al. (2011). Clinicopathological features and prognosis of cystic gastrointestinal stromal tumor. Zhonghua Wei Chang Wai Ke Za Zhi, 14(8), 599–602.
Seshadri, R. A., Singh, S. S., & Ratnagiri, R. (2012). Synchronous jejunal gastrointestinal stromal tumor and primary adenocarcinoma of the colon. Indian Journal of Surgery, 74(2), 196–198.
Miettinen, M., & Lasota, J. (2011). Histopathology of gastrointestinal stromal tumor. Journal of Surgical Oncology, 104(8), 865–873.
Riddle, N. D., Gonzalez, R. J., Bridge, J. A., et al. (2011). A CD117 and CD34 immunoreactive sarcoma masquerading as a gastrointestinal stromal tumor: Diagnostic pitfalls of ancillary studies in sarcoma. Cancer Control, 18(3), 152–159.
Pelz, A. F., Agaimy, A., Daniels, M., et al. (2011). Gastrointestinal stromal tumor presenting as a rectovaginal mass. Clinicopathologic and molecular-genetic characterization of a rare tumor with a literature review. Human Pathology, 42(4), 586–593.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, Q., Wang, Y., Kong, L. et al. Study on Clinicopathological Features of Gastrointestinal Stromal Tumor and Relevant Prognostic Factors. Cell Biochem Biophys 73, 743–747 (2015). https://doi.org/10.1007/s12013-015-0678-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0678-5