Abstract
Endogenous fibrinolysis is a protective mechanism against arterial thrombotic occlusion, which would otherwise lead to permanent tissue damage as acute myocardial infarction (AMI). We aimed to investigate the association of plasminogen activator inhibitor-1 (PAI-1) and tissue plasminogen activator (TPA) genes polymorphisms with myocardial infarction and its outcomes in Egyptian patients. 184 patients with AMI and 184 controls were included in the study. PAI-1 and TPA genes polymorphisms were analyzed by polymerase chain reaction. All patients were followed for AMI complications during their hospitalization. We found a significant association among TPA ID, II genotypes, and I allele and increased risk of AMI by 2.1, 3.2, and 1.9 fold, respectively. Also, the frequencies of PAI-1 4G/4G genotype and 4G allele were significantly increased in patients with AMI as compared to the control group. Furthermore, AMI patients with PAI-1 4G/4G genotype were significantly more likely to have morbidity and mortality complications as compared to AMI patients without complications (P = 0.00 and 0.048, respectively). We concluded that 4G/4G genotype and 4G allele of the PAI-1 gene are associated with risk of AMI and its morbidity. The PAI-1 4G/4G genotype is associated with mortality of AMI. There is also an association between TPA ID, II genotypes, and I allele with increased risk of AMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myocardial infarction (AMI) is one of the most important health problems in many nations around the world. It may be found in many age groups, but is predominant among elderly people [1]. It is a startling fact that upon a person has throughout his or her lifetime a 47 % chance of having a cardiac event [2]. The mortality from myocardial infarction has been reduced by more than 50 % over the past 30 years; nevertheless, a plateau has been reached [3]. AMI has devastating consequences include ischemic, mechanical, arrhythmic, embolic and inflammatory (pericarditis) disturbances. The ischemic and mechanical complications have the most prevalence and mortality rates among people with AMI [4]. Ischemic complications include infarct extension, recurrent infarction, and recurrent angina. Reocclusion of an infarct-related artery occurs in 5–30 % of patients following fibrinolytic therapy. These patients tend to have a poorer outcome [5].
Since AMI results as a direct consequence of the development of blockage in the coronary arteries due to clot formation (thrombosis), it has a direct relationship with the thrombosis–fibrinolysis system [6]. Tissue plasminogen activator (TPA) and plasminogen activator inhibitor-1 (PAI-1) are two important regulators of this pathway. TPA is a serine protease found in the endothelial cells and plays a role in the breakdown of the fibrin clot by converting plasminogen into plasmin, leading to fibrinolysis, and TPA action is inhibited by PAI-1 that acts by forming TPA–PAI-1 complex, resulting in impaired fibrinolytic function and thrombosis [7].
TPA is encoded by the PLAT (plasminogen activator tissue type) gene on chromosome 8p11.21 spanning 8 coding exons. Recently, one polymorphism, an Alu-repeat I/D polymorphism, was found in intron H of this gene. It was found that the heterozygous Insertion/Deletion (Ins/Del) is associated with an increased TPA activity [6].
Plasma PAI-1 levels are affected by many environmental and constitutive factors, including body mass, lipid metabolism, glucose concentration, renin-angiotensin-aldosterone system, and many others including genetic variability [8, 9].
One of the PAI-1 genetic polymorphisms, guanine insertion/deletion polymorphism known as (675 4G/5G) located within the promoter region of chromosome 7, is reported in many studies to be associated with the plasma concentration of PAI-1 [10].
Risk assessment and evaluation of predictors of AMI outcomes are an important part of the initial and ongoing evaluation of the patient. It can determine the patient’s prognosis, likely response to various treatments and guide decisions as to which therapeutic approach is most appropriate [11].
On the basis of these considerations, we designed this study to investigate the association of PAI-1 and TPA genes polymorphisms with myocardial infarction and its outcomes in Egyptian patients.
Subjects and Methods
Subjects
Unrelated 184 Egyptian patients (mean age 57.1 ± 10.8 years) with documented acute myocardial infarction (AMI group) were recruited from the patients admitted to the cardiology department of Zagazig University Hospital (Zagazig, Egypt). AMI was diagnosed according to WHO criteria, which are based on the complaint of chest pain for more than 20 min, higher than normal levels of cardiac-specific markers and ST changes on electrocardiography (ECG). Exclusion criteria included patients with unstable angina, congenital, rheumatic heart disease, cardiomyopathy, malignant tumor, inflammatory or connective tissue diseases.
Myocardial infarction group was divided into four subgroups: group I includes 82 patients who were not revascularized, did not have complications or died; group II (morbidity group) includes 45 patients who had complications in the form of heart failure, arrhythmia [AF, VT and heart block], LV thrombus, myocardial aneurysm, cardiogenic shock, cardiac arrest, and reinfarction; group III (mortality group) includes 28 patients who were died; and group IV (revascularization group) includes 29 patients who had undergone revascularization (percutaneous coronary intervention PCI or coronary artery bypass graft CABG) and did not have any complications. All the participants were subjected to the following at the time of admission: thorough history taking, clinical examination, Standard 12-lead surface electrocardiogram, and Echocardiographic examination. All patients were followed for complications during their hospitalization.
The control group comprised 184 healthy subjects with no family history of CAD, MI or stroke. The ethical committee of Zagazig University approved this study, and a written informed consent was obtained from all subjects prior to their inclusion in this work.
Biochemical Measurement
Blood samples were drawn from all subjects after an overnight fast and divided into two portions. One portion of blood (2 ml) was added to EDTA, second portion of 2 ml blood was left for 10 min to clot and then was centrifuged at 1,000×g for 5 min. The serum and plasma were then separated and stored at −20 °C for the following procedures:
A-Analyses of lipid
Total cholesterol and triglycerides were measured by routine enzymatic methods (Spinreact). HDLc was determined after precipitation of the apoB-containing lipoproteins. LDLc was calculated using Friedewald formula [12].
B-Estimation
of serum level of cardiac markers (CKMB and troponin).
C-Genomic DNA Extraction
Genomic DNA was extracted from EDTA whole blood sample using a spin column method according to the protocol (QIAamp Blood Kit; Qiagen GmbH, Hilden, Germany). DNA was stored at −20 °C till the time of use.
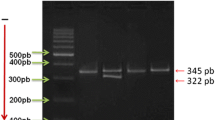
Amplification of Plasminogen Activator Inhibitor-1 (675 4G/5G) Polymorphism
PAI-1 genotypes were identified by polymerase chain reaction–restriction fragment length polymorphism (PCR–RFLP) method of the promoter region containing 4G/5G polymorphism as described by Mansfield et al. [13] using the following primers: PAI-1: 5′ AAG CTT TTA CCA TGG TAA CCCCTG GT 3′, PAI-2: 5′ TGC AGC CAG CCA CGT GAT TGTCTA 3′, PAI-4G: 5′ GTC TGG ACA CGT GGG GA 3′, and PAI-5G: 5′ GTC TGG ACA CGT GGG GG 3′. Both PAI-1 and PAI-2 amplify a 257-bp (base pair) product from either allele. The PAI-4G specifically amplifies the 4G allele, and PAI-5G specifically amplifies the 5G allele. PCR cycling conditions were: 95 °C for 2 min followed by 45 cycles at 94 °C for 35 s, at 65 °C for 45 s, and 72 °C for 75 s. A final extension step was carried out at 72 °C for 5 min. The PCR product was separated on 2 % agarose gel stained with ethidium bromide and visualized under UV light. Both PAI-1 and PAI-2 amplify a 257-bp product from either allele. The PAI-4G specifically amplifies the 4G allele, and PAI-5G specifically amplifies the 5G allele (139 or 140 bp).
Amplification of tissue Plasminogen Activator (I/D) Polymorphism
The subjects were genotyped for TPA (I/D) polymorphism by PCR–RFLP as previously described [14]. The region surrounding the polymorphism was amplified with the forward primer 5′ TCCGTAACAGGACAGCTCA-3′ and reverse primer 5′-ACCGTG GCTTCAGTCATGGA-3′. PCR cycling conditions were: 95 °C for 2 min followed by 30 cycles at 94 °C for 35 s, at 58 °C for 1 min, and 72 °C for 75 s. A final extension step was carried out at 72 °C for 1 min. The PCR product was separated on 2 % agarose gel stained with ethidium bromide and visualized under UV light. The PCR produced a band of 656 bp for D allele and a band of 976 bp for I allele or both for I and D alleles.
Statistical Analysis
Data were analyzed with SPSS version 15.0 (statistical package for the Social Science, Chicago, IL). The results of continuous variables were expressed as mean ± SD. The means of genotypes groups were compared by one-way analysis of variance (ANOVA). The TPA and PAI-1 genes variants under investigation were evaluated for deviation from Hardy–Weinberg equilibrium analyses by comparing observed and expected genotype frequencies by means of chi2 (χ 2) test in cases and control groups. The statistical difference in genotype distribution and allele frequencies in both control and case subjects was assessed by using χ 2 test. Odds ratios (ORs) and confidence intervals (CIs) were calculated.
Results
Clinical Data and Biochemical Characteristics of Study Subjects (Table 1)
The prevalence of atherogenic risk factors (including diabetes, hypertension, and smoking) was significantly higher in the patient group as compared to that of the control group. We observed significantly higher levels of TC, TG, and LDLc and significantly lower levels of HDL in patients group as compared to control and in group II, III and IV as compared to group I. Also, CPK and troponin levels were significantly increased in group III and IV as compared to group I.
Distribution of TPA and PAI-1 Genotypes and Alleles in the Study Population (Table 2)
The frequencies of TPA and PAI-1 genotypes and alleles were all in accordance with the Hardy–Weinberg equilibrium in all groups. In AMI patients, the frequencies of TPA ID, II genotypes, and I allele were significantly increased compared to control group. Also, the frequencies of PAI-1 4G/4G genotypes and 4G allele were significantly increased in AMI patients compared to control group. Carriers of TPA II genotype and PAI-1 4G/4G genotype were significantly more likely to develop AMI (OR = 3.2 95 % CI 1.48–7.3 and P = 0.002 and OR = 3.33 95 % CI 1.5–7.5 and P = 0.003, respectively).
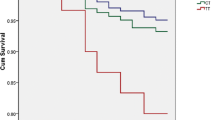
Distribution of TPA and PAI-1 Genotypes and Alleles in AMI Patients with Morbidity Versus Those without Complications (Table 3)
The frequencies of PAI-1 4G/4G genotype and 4G allele were significantly increased in AMI patients with morbidity compared to AMI patients without complications. AMI patients with PAI-1 4G/4G genotype and 4G allele were significantly more likely to have morbidity (OR = 4.6, 95 % CI 1.9–10.8 and P = 0.000 and OR = 2.6, 95 % CI 1.45–4.76 and P = 0.002, respectively). On the contrary, the genotypes and I allele frequencies of TPA were not significantly different between AMI patients with morbidity and those without complications.
Distribution of TPA and PAI-1 Genotypes and Alleles in AMI Patients with Mortality Versus Those Without Complications (Table 4)
The frequency of PAI-1 4G/4G genotype was significantly increased in AMI patients with mortality compared to AMI patients without complications. The incidence of death was significantly more likely to occur after the incidence of AMI in subjects carrying PAI-1 4G/4G genotype (OR = 2.25, 95 % CI 1.02–4.9 and P = 0.048). On the contrary, the genotypes and allele I frequencies of TPA were not significantly different between AMI patients with mortality and those without complications.
Distribution of TPA and PAI-1 Genotypes and Alleles in AMI Patients with Revascularization Versus Without Revascularization (Table 5)
The frequencies of PAI-1 and TPA genotypes and alleles were not significantly different between AMI patients with revascularization and those without complications.
Comparison of the type of complication between group II (morbidity) and group III (mortality) (Table 6)
There was no significant difference between the two groups regarding the type of complication (arrhythmia, heart failure, reinfarction, and shock).
Discussion
To our knowledge, this is the first study conducted in Egyptian AMI patients to investigate the relationship between TPA and PAI-1 genes polymorphisms and susceptibility to AMI and its outcome. Over the last decade, increasing evidence has emerged to support the assumption that AMI is a failure of timely spontaneous thrombolysis [15]. Previous studies examined the association of polymorphisms in TPA and PA-I genes with AMI [14, 16–18], however, their data are conflicting. Also, there is a lack of studies investigating the genetic determinants of the different outcomes in AMI patients. Therefore, further studies in different populations are essential.
Our study showed a significant association between TPA ID, II genotypes, and I allele and increased risk of AMI. This finding is consistent with that of Van der Bom et al. [14] who reported that TPA genotypes characterized by either one or two insertion alleles (I/D and I/I) were associated with an excessive number of cases of AMI compared with the D/D genotype. Moreover, Voetsch and Loscalzo [6] concluded that there was a two-fold increase in the risk of MI for homozygous insertions, while the heterozygous (Ins/Del) was associated with a 50 % increased risk of MI. The contrast was found in a study of Waqas et al. [16] who found no significant association of this polymorphism in the Pakistanian population. Also, Ridker et al. [19] documented that in the cohort of middle-aged US men, the presence of the insertion allele of TPA gene was not associated with future risks of myocardial infarction. Furthermore, our data disagree with those of Steeds et al. [20] who observed that TPA I/D polymorphism is not a major independent risk factor for myocardial infarction in UK population.
In this study, we demonstrated that AMI patients showed a significant increase in the frequencies of PAI-1 4G/4G genotype and 4G allele as compared to the control group. These results are consistent with Onalan et al. [21] who reported that the PAI-1 4G4G genotype was an independent predictor of AMI (OR: 2.7, P = 0.002). Also, Kholer and Grant [22] showed an association between this polymorphism and ST elevation acute myocardial infarction (STEMI) in young patients. This agrees with several other studies [16, 23, 24] that confirmed a significantly increased risk of MI with the presence of PAI-1 4G/4G genotype in different populations. On the contrary, our data disagree with those [25, 26] who found no significant association of this polymorphism with the risk of MI.
Differences in the population genetic backgrounds, lifestyle, diet as well as study design, and recruitment of the cases in each study could explain the variation in the results. Also, it is difficult to identify a single gene polymorphism as a risk factor for a polygenic and multifactorial disease as AMI.
This is the first study that investigates the association of TPA and PAI-1 genes with the different outcomes in AMI patients and found that the frequencies of PAI-1 4G/4G genotype were significantly increased in AMI patients with morbidity or mortality complications as compared to AMI patients without complications.
The association of PAI-1 gene polymorphism (675 4G/5G) with circulating PAI-1 levels in healthy subjects, young MI patients, and non-insulin-dependent diabetes, with subjects homozygous for the 4G (deletion) allele having the highest PAI-I levels [27–30], could explain the association of this polymorphism with the risk of AMI and its adverse outcomes. In vitro studies have identified the differential binding of transcription-regulating proteins at the site of this polymorphism, with increased gene transcription associated with the 4G allele [27, 28].
In agreement with these findings, a prospective study of 249 angina patients found that those with higher PAI-1 activity had a 4.2-fold increased risk of subsequent coronary events [31]. Moreover, Akkus et al. [32] reported that raised levels of PAI-1 in 180 AMI patients on admission were associated with greatly increased risk of cardiogenic shock and in-hospital and 1-year mortality (OR: 6.0). Also, in a study done on 520 patients with acute coronary syndrome, increased PAI-1 was a significant and independent risk factor for the occurrence of major adverse cardiovascular events (OR: 5.3) [33].
Only one study done by Marcucci et al. [34] investigated the association of 37 atherosclerosis-associated genetic polymorphisms and 17 blood marker variables with the risk for only recurrent coronary outcomes in nonhyperlipidemic postinfarction patients and found that only the PAI-1 4G/5G polymorphism was associated with recurrent risk (HR = 4.02, P = 0.00039, for 4G/4G versus 4G/5G plus 5G/5G patients).
On the contrary, the frequency of PAI-1 genotypes and alleles were not significantly different between AMI patients with and without revascularization. This finding agrees with those of a study done by Fernandez-Cadenas et al. [35] who reported no association between PAI-1 4 G/5 G polymorphism and recanalization rate.
Our study revealed that the frequencies of TPA genotypes and allele I were not significantly different between AMI patients with and without morbidity, mortality complications or with revascularization.
Previous studies investigated the association between TPA level and the coronary disease outcomes and reported that high TPA levels predict future cardiovascular events (especially recurrent events) in patients with established CAD and AMI [36–38]. Paradoxically, increased plasma TPA indicates inhibited endogenous fibrinolysis. This is because free TPA released into blood from endothelial cells immediately forms a complex with circulating PAI-1 [39, 40]. Because PAI-1 concentration in plasma is much higher than TPA antigen concentration, the TPA antigen assay measures both free and complexed TPA, and increased concentration of TPA antigen is supposed to indicate a reduced rather than enhanced fibrinolytic activity [41].
The nature of I/D polymorphism, an insertion of an Alu repeat in an intron, a nontranslated region, makes a direct functional effect of I allele on the TPA protein unlikely [42]. Different studies showed that the Alu polymorphism in the TPA gene was not associated with TPA plasma levels [14, 43]. Furthermore, the basal endothelial TPA synthesis was reported not to be influenced by this polymorphism [44].
The association of TPA (I/D) polymorphism with the risk of myocardial infarction could be explained by the presence of linkage disequilibrium with other genes that produce a functional effect (impaired fibrinolytic capacity?) and may cause an increased risk for MI.
Conclusion
The 4G/4G genotype and 4G allele of the PAI-1 gene are associated with the risk of AMI and its morbidity. The PAI-1 4G/4G genotype is associated with mortality of AMI. There is also an association among TPA ID, II genotypes and I allele with an increased risk of AMI. Finally, as MI is a polygenic disease, it remains important to assess different single nucleotide polymorphisms (SNPs) by linkage studies and haplotype analysis to identify genes that might have a significant influence on the risk of MI and its outcomes.
Ethical Approval
The study protocol was approved by the ethical committee of Faculty of Medicine, Zagazig University.
References
Hansson, G. K. (2005). Inflammation, atherosclerosis, and coronary artery disease. New England Journal of Medicine, 352, 1685–1695.
Chaer, R. A., Billeh, R., & Massad, M. G. (2004). Genetics and gene manipulation therapy of premature coronary artery disease. Cardiology, 101, 122–130.
American Heart Association: Heart and Stroke Statistical Update. American Heart Association. 2000 ed. Dallas: 2000.
McKay, R. G., Pfeffer, M. A., Pasternak, R. C., Markis, J. E., Come, P. C., Nakao, S., et al. (1986). Left ventricular remodeling after myocardial infarction: A corollary to infarct expansion. Circulation, 74, 693–702.
Brouwer, M. A., van den Bergh, P. J. P. C., Aengevaeren, W. R. M., Veen, G., Luijten, H. E., Hertzberger, D. P., et al. (2002). Aspirin plus coumarin versus aspirin alone in the prevention of reocclusion after fibrinolysis for acute myocardial infarction: Results of the Antithrombotics in the Prevention of Reocclusion In Coronary Thrombolysis (APRICOT)-2 Trial. Circulation, 106, 659–665.
Voetsch, B., & Loscalzo, J. (2004). Genetic determinants of arterial thrombosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 24, 216–229.
Robinson, S. D., Ludlam, C. A., Boon, N. A., & Newby, D. E. (2006). Tissue plasminogen activator genetic polymorphisms do not influence tissue plasminogen activator release in patients with coronary heart disease. Journal of Thrombosis and Haemostasis, 4, 2262–2269.
Mansfield, M. W., Stickland, M. H., & Grant, P. J. (1995). Environmental and genetic factors in relation to elevated circulating levels of plasminogen activator inhibitor-1 in Caucasian patients with non-insulin-dependent diabetes mellitus. Thrombosis and Haemostasis, 74, 842–847.
Dawson, S., Hamsten, A., Wiman, B., Henney, A., & Humphries, S. (1991). Genetic variation at the plasminogen activator inhibitor-1 locus is associated with altered levels of plasma plasminogen activator inhibitor-1 activity. Arteriosclerosis and Thrombosis, 11, 183–190.
Humphries, S. E., Panahloo, A., Montgomery, H. E., Green, F., & Yudkin, J. (1997). Gene-environment interaction in the determination of levels of haemostatic variables involved in thrombosis and fibrinolysis. Thrombosis and Haemostasis, 78, 457–461.
Boersma, E., Pieper, K. S., Steyerberg, E. W., Wilcox, R. G., Chang, W. C., Lee, K. L., et al. (2000). Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation: Results from an international trial of 9461 patients. Circulation, 101, 2557–2567.
Frieldewald, W. T., Levy, R. I., & Fredrickson, D. S. (1972). Estimation of the concentration of low density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry, 18(6), 499–502.
Mansfield, M. W., Strickland, M. H., & Grant, P. J. (1995). Plasminogen activator inhibitor-1 promoter polymorphism and coronary artery disease in non–insulin-dependent diabetes. Thrombosis and Haemostasis, 74, 1032–1034.
Van der Bom, J. G., de Knijff, P., Haverkate, F., Bots, M. L., Meijer, P., de Jong, P. T., et al. (1997). Tissue plasminogen activator and risk of myocardial infarction. The Rotterdam Study. Circulation, 95, 2623–2627.
Swan, H. J. (1989). Acute myocardial infarction: A failure of timely, spontaneous thrombolysis. Journal of the American College of Cardiology, 13, 1435–1437.
Waqas, A., Meera, M., Imran, S., Amina, A. K., Ahmed, S., Umar, K., et al. (2011). Role of tissue plasminogen activator and plasminogen activator inhibitor polymorphism in myocardial infarction. Molecular Biology Reports, 38, 2541–2548.
Hoekstra, T., Geleijnse, J. M., Schouten, E. G., & Kluft, C. (2004). Plasminogen activator inhibitor-type 1: Its plasma determinants and relation with cardiovascular risk. Thrombosis and Haemostasis, 91, 861–862.
Ding, J., Nicklas, B. J., Fallin, M. D., de Rekeneire, N., Kritchevsky, S. B., Pahor, M., et al. (2006). Plasminogen activator inhibitor type 1 gene polymorphisms and haplotypes are associated with plasma plasminogen activator inhibitor type 1 levels but not with myocardial infarction or stroke. American Heart Journal, 152, 1109–1115.
Ridker, P. M., Baker, M. T., Hennekens, C. H., Stampfer, M. J., & Vaughan, D. E. (1997). Alu-repeat polymorphism in the gene coding for tissue- type plasminogen activator (t-PA) and risks of myocardial infarction among middle-aged men. Arteriosclerosis, Thrombosis, and Vascular Biology, 17, 1687–16890.
Steeds, R., Adams, M., Smith, P., Channer, K., & Samani, N. J. (1998). Distribution of tissue plasminogen activator insertion/deletion polymorphism in myocardial infarction and control subjects. Thrombosis and Haemostasis, 79, 980–984.
Onalan, O., Balta, G., Oto, A., Kabakci, G., Tokgozoglu, L., Aytemir, K., et al. (2008). Plasminogen activator inhibitor-1 4G4G genotype is associated with myocardial infarction but not with stable coronary artery disease. Journal of Thrombosis and Thrombolysis, 26, 211–217.
Kholer, H. P., & Grant, P. J. (2000). Plasminogen-activator inhibitor type 1 and coronary artery disease. New England Journal of Medicine, 342, 1792–1801.
Margaglione, M., Cappucci, G., Colaizzo, D., Giuliani, N., Vecchione, G., Grandone, E., et al. (1998). The PAI-1 gene locus 4G/5G polymorphism is associated with a family history of coronary artery disease. Arteriosclerosis, Thrombosis, and Vascular Biology, 18, 152–156.
Iacoviello, L., Burzotta, F., Di Castelnuovo, A., Zito, F., Marchioli, R., & Donati, M. B. (1998). The 4G/5G polymorphism of PAI-1 promoter gene and the risk of myocardial infarction: A meta-analysis. Thrombosis and Haemostasis, 80, 1029–1030.
Crainich, P., Jenny, N. S., Tang, Z., Arnold, A. M., Kuller, L. H., Manolio, T., et al. (2003). Lack of association of the plasminogen activator inhibitor-1 4G/5G promoter polymorphism with cardiovascular disease in the elderly. Journal of Thrombosis and Haemostasis, 1, 1799–1804.
Anderson, J. L., Muhlestein, J. B., Habashi, J., Carlquist, J. F., Bair, T. L., Elmer, S. P., et al. (1999). Lack of association of a common polymorphism of the plasminogen activator inhibitor-1 gene with coronary artery disease and myocardial infarction. Journal of the American College of Cardiology, 34, 1778–1783.
Dawson, S. J., Wiman, B., Hamsten, A., Green, F., Humphries, S., & Henney, A. M. (1993). The two allele sequences of a common polymorphism in the promoter of the plasminogen activator inhibitor-1 (PAI-1) gene respond differently to interleukin-1 in HepG2 cells. Journal of Biological Chemistry, 268, 10739–10745.
Eriksson, P., Kallin, B., van’t Hooft, F. M., Bavenholm, P., & Hamsten, A. (1995). Allele-specific increase in basal transcription of the plasminogen-activator inhibitor 1 gene is associated with myocardial infarction. Proceedings of the National Academy of Sciences USA, 92, 1851–1855.
Panahloo, A., Mohamed-Ali, V., Lane, A., Green, F., Humphries, S. E., & Yudkin, J. S. (1995). Determinants of plasminogen activator inhibitor 1 activity in treated NIDDM and its relation to a polymorphism in the plasminogen activator inhibitor 1 gene. Diabetes, 44, 37–42.
Ye, S., Green, F. R., Scarabin, P. Y., Nicaud, V., Bara, L., Dawson, S. J., et al. (1995). The 4G/5G genetic polymorphism in the promoter of the plasminogen activator inhibitor-1 (PAI-1) gene is associated with differences in plasma PAI-1 activity but not with risk of myocardial infarction in the ECTIM study. Thrombosis and Haemostasis, 74, 837–841.
Takazoe, K., Ogawa, H., Yasue, H., Sakamoto, T., Soejima, H., Miyao, Y., et al. (2001). Increased plasminogen activator inhibitor activity and diabetes predict subsequent coronary events in patients with angina pectoris. Annals of Medicine, 33, 206–212.
Akkus, M. N., Polat, G., Yurtdas, M., Akcay, B., Ercetin, N., Cicek, D., et al. (2009). Admission levels of C-reactive protein and plasminogen activator inhibitor-1 in patients with acute myocardial infarction with and without cardiogenic shock or heart failure on admission. International Heart Journal, 50, 33–45.
Marcucci, R., Brogi, D., Sofi, F., Giglioli, C., Valente, S., Liotta, A. A., et al. (2006). PAI-1 and homocysteine, but not lipoprotein (a) and thrombophilic polymorphisms, are independently associated with the occurrence of major adverse cardiac events after successful coronary stenting. Heart, 92, 377–381.
Corsetti, J. P., Ryan, D., Moss, A. J., Rainwater, D. L., Zareba, W., & Sparks, E. C. (2008). Plasminogen activator inhibitor-1 polymorphism (4G/5G) predicts recurrence in nonhyperlipidemic postinfarction patients. Arteriosclerosis, Thrombosis, and Vascular Biology, 28, 548–554.
Fernandez-Cadenas, I., Alvarez-Sabin, J., Ribo, M., Rubiera, M., Mendioroz, M., Molina, C. A., et al. (2007). Influence of thrombin-activatable fibrinolysis inhibitor and plasminogen activator inhibitor-1 gene polymorphisms on tissue-type plasminogen activator-induced recanalization in ischemic stroke patients. Journal of Thrombosis and Haemostasis, 5, 1862–1868.
Kinlay, S., Schwartz, G. G., Olsson, A. G., Rifai, N., Bao, W., Libby, P., et al. (2009). Endogenous tissue plasminogen activator and risk of recurrent cardiac events after an acute coronary syndrome in the MIRACL study. Atherosclerosis, 206, 551–555.
Lee, C. W., Ahn, J. M., Park, D. W., Kim, Y. H., Hong, M. K., Song, J. K., et al. (2008). Tissue plasminogen activator on admission is an important predictor of 30-day mortality in patients with acute myocardial infarction undergoing primary angioplasty. Atherosclerosis, 196, 327–332.
Soeki, T., Tamura, Y., Shinohara, H., Sakabe, K., Onose, Y., & Fukuda, N. (2002). Plasma concentrations of fibrinolytic factors in the subacute phase of myocardial infarction predict recurrent myocardial infarction or sudden cardiac death. International Journal of Cardiology, 85, 277–283.
Nordenhem, A., & Wiman, B. (1998). Tissue plasminogen activator (tPA) antigenin plasma: Correlation with different tPA/inhibitor complexes. Scandinavian Journal of Clinical and Laboratory Investigation, 58, 475–483.
Wiman, B. (1999). Predictive value of fibrinolytic factors in coronary heart disease. Scandinavian Journal of Clinical and Laboratory Investigation. Supplement, 230, 23–31.
Kluft, C. (1994). Constitutive synthesis of tissue type plasminogen activator and plasminogen activator inhibitor type 1: Conditions and therapeutic targets. Fibrinolysis, 8(Suppl 2), 1–7.
Makalowski, W., Mitchell, G. A., & Labuda, D. (1994). Alu sequences in the coding regions of mRNA: A source of protein variability. Trends in Genetics, 10, 188–193.
Robinson, S. D., Ludlam, C., Boon, N. A., & Newby, D. E. (2005). Tissue plasminogen activator genetic polymorphisms do not influence tissue plasminogen activator releasein patients with coronary artery disease. Journal of Thrombosis and Hemostasis, 4, 2262–2269.
van den Eijnden-Schrauwen, Y., Lakenberg, N., Emeis, J. J., & de Knijff, P. (1995). Alu-repeat polymorphism in the tissue type plasminogen activator gene does not affect basal endothelial t-PA synthesis. Thrombosis and Haemostasis, 74, 1202.
Acknowledgments
This study was funded with the support of Academic Research in Zagazig University Projects, Zagazig University Post Graduate & Research Affairs.
Conflict of interest
No conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Aziz, T.A.A., Rezk, N.A. Relation of PAI-1 and TPA Genes Polymorphisms to Acute Myocardial Infarction and its Outcomes in Egyptian Patients. Cell Biochem Biophys 71, 227–234 (2015). https://doi.org/10.1007/s12013-014-0188-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-014-0188-x