Abstract
Highly active anti-retroviral therapy has proved successful in reducing morbidity and mortality associated with HIV infection though it has been linked to increased risk of cardiovascular disease. To date, the direct effects of the anti-retroviral drugs Efavirenz, Tenofovir and Emtricitabine on the vasculature relaxant response have not been elucidated, which impaired may predispose individuals to cardiovascular disease. Increased cellular oxidative stress and overactivation of the DNA repair enzyme poly (ADP-ribose) polymerase (PARP) have been identified as central mediators of vascular dysfunction. The aim of this study was to investigate whether exposure to Efavirenz, Tenofovir or Emtricitabine directly causes endothelial cell dysfunction via overactivation of PARP. Exposure of ex vivo male rat aortic rings or in vitro endothelial cells to Efavirenz but not Tenofovir or Emtricitabine impaired the acetylcholine-mediated relaxant response, increased cellular oxidative stress and PARP activity, decreased cell viability and increased apoptosis and necrosis. Pharmacological inhibition of PARP protected against the Efavirenz-mediated impairment of vascular relaxation and endothelial cell dysfunction. Oestrogen exposure also protected against the Efavirenz-mediated inhibition of the vascular relaxant response, cell dysfunction and increased PARP activation. In conclusion, Efavirenz directly impairs endothelial cell function, which may account for the increased risk of developing cardiovascular complications with anti-retroviral therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbidity and mortality associated with HIV infection and subsequent development of AIDS has been dramatically reduced since the introduction of Highly Active Anti-Retroviral Therapy (HAART) in 1993. Anti-retroviral drugs which inhibit HIV reverse transcriptase were not only the first to be developed but have also continued to be a key component in the effectiveness of HAART. The first anti-retroviral drugs to inhibit reverse transcriptase were nucleoside reverse transcriptase inhibitors (NRTI’s) such as the competitive inhibitor azidothymidine (AZT), and these were joined by nucleotide/nucleoside reverse transcriptase inhibitors (NtRTI’s) such as Tenofovir and Emtricitabine. These are analogues of the deoxynucleotides needed to synthesize the viral DNA competing with the naturally occurring deoxynucleotides, acting as substrates and being incorporated into the growing DNA chain, causing chain termination as they lack a 3′-hydroxy group. More recently, non-competitive inhibitors of reverse transcriptase have been developed the non-nucleoside reverse transcriptase inhibitors (NNRTIs) which directly bind to the viral reverse transcriptase enzyme at a site other than the active site to inhibit its function, one example of the first generation of these drugs is Efavirenz.
The success of HAART has been overshadowed by significant toxicities linked to anti-retroviral agents including increased risk of diabetes, atherosclerosis and cardiovascular complications. NRTI’s have been linked to endothelial cell dysfunction through mitochondrial toxicity and increased cellular oxidative stress proposed to be mediated inhibition of DNA polymerase-γ which is crucial for mitochondrial replication and repair [1]. Increased cellular oxidative stress and overactivation of the DNA repair enzyme poly (ADP-ribose) polymerase (PARP) with subsequent cell depletion of high-energy phosphates and NAD have been shown to be a central mediator of vascular dysfunction in a variety of cardiovascular diseases [2]. The NRTI AZT has been shown to increase oxidative stress in both cardiomyocytes [3] and endothelial cells [4] subsequently increasing PARP activation in cardiomyocytes [3]; likely to be the mechanism behind the increased risk of myocardial infarction (MI) found in the D:A:D study [5]. These cardiovascular side effects of NRTI’s was one of the driving factors to develop the newer NNRTI’s for HIV as they do not inhibit DNA polymerase-γ and were thought to have a reduced risk of mitochondrial toxicity.
In 2006, Atripla was introduced, a combination of Efavirenz, Tenofovir and Emtricitabine in a single pill, to be taken once-a-day improving patient compliance. However, some cardiovascular complications have been identified with this combination pill. In clinical studies, endothelial cell function of patients on this drug combination, Efavirenz/Tenofovir/Emtricitabine, as assessed by flow-mediated dilation of the brachial artery, was found to be reduced as compared to other anti-retroviral drug combinations [6] suggesting an increased risk of cardiovascular disease. Though the combination was found to increase the endothelial cell dysfunction as compared to Efavirenz alone [6], Tenofovir and Emtricitabine have not been found to affect endothelial cell function or cardiovascular disease risk in clinical studies [5]. Efavirenz-based regimens, however, have been shown to increase the risk of cardiovascular disease including an increased tendency to develop atherosclerotic lesions [7, 8]. However, there are conflicting data on Efavirenz increasing the risk of myocardial infarction (MI) with the D:A:D study finding no increased risk [5], while a study in Canada demonstrated a significant risk of MI in patients on Efavirenz [9].
The direct effects of Tenofovir and Emtricitabine on in vitro endothelial cell function have not been investigated. Tenofovir has been found to cause nephrotoxicity but has no effect on inflammatory, apoptotic or oxidative stress gene expression in coronary endothelial cells [10]. Emtricitabine alone has not yet been investigated to determine any in vitro endothelial cell damaging effects though in combination with Tenofovir has been shown to have no effect on leucocyte–endothelial cell interaction, a combination proposed to have a better vascular profile than other anti-retroviral regimens [11].
Efavirenz has been shown to increase oxidative stress, MAPK and JNK phosphorylation and NF-κB activation in human coronary artery endothelial cells [12], effects proposed to be mediated by mitochondrial toxicity. Efavirenz was also found to decrease the expression of the tight junctional proteins claudin-1, occludin, zonula occluden-1 and junctional adhesion molecule-1 with a subsequent increase in monolayer permeability [12]. Efavirenz has been shown to increase cellular oxidative stress and cause cell dysfunction in a variety of other cell types including hepatocytes [13, 14]. Indeed, in HIV patients on Efavirenz increased levels of plasma F2 isoprostane concentrations which indicate increased oxidative stress have been observed [15]. These data suggest that Efavirenz may be the component of Atripla responsible for the endothelial cell dysfunction and subsequent increased risk of cardiovascular disease though the underlying pathology beyond increased oxidative stress has yet to be determined.
Therefore, the aim of this study was to examine the direct effects of the anti-retroviral drug components of Atripla, Efavirenz, Tenofovir and Emtricitabine, on endothelial cell function and investigate whether increased activation of PARP is responsible for any deleterious effects.
Methods
Reagents
Efavirenz, Tenofovir and Emtricitabine were obtained from Sequoia Research Products Ltd. (Pangbourne, UK). Acetylcholine chloride, bisbenzimide H 33342 trihydrochloride, digitonin, dimethyl sulphoxide (DMSO), 2,7-dichlorofluorescin diacetate, endothelial cell growth supplement, oestrogen, heparin, nitro blue tetrazolium (NBT), phenylephrine hydrochloride, propidium iodide, sodium dodecyl sulphate (SDS), sodium nitroprusside and thiazolyl blue tetrazolium bromide (MTT) were obtained from Sigma-Aldrich (Poole, UK). 3H-NAD was obtained from PerkinElmer Ltd. (Windsor, UK). PJ-34 was purchased from Calbiochem (Nottingham, UK). DMEM and Hams F12 culture media, non-essential amino acids, penicillin, streptomycin and foetal bovine serum (FBS) were obtained from GE Healthcare (Buckinghamshire, UK). Sprague–Dawley rats used in the ex vivo studies were obtained from Charles River Laboratories (Kent, UK). EA.hy926 cells used in the in vitro studies were obtained from the UK distributor of American Type Culture Collection LGC Standards (Middlesex, UK). All other chemicals were of reagent grade and obtained from Fisher Scientific (Loughborough, UK).
Ex Vivo
Thoracic aorta from male or female Sprague–Dawley rats (180–220 g) was dissected and cleared of periadventitial fat and connective tissue. Rings of 2–3 mm were cut and placed into Hams F12 medium supplemented with 3% FBS, endothelial cell growth supplement (0.03 mg/ml), heparin (50 U/ml) and 1% penicillin and streptomycin. For the initial experiments, male or female aortic rings were incubated with Hams F12 media alone (control) or with Efavirenz, Tenofovir or Emtricitabine 1, 3 or 10 µM, for 2, 4 or 6 h at 37 °C with 5% CO2. Subsequent to these experiments, male aortic rings were exposed to Efavirenz 10 µM in combination with either an inhibitor of PARP (PJ-34 3 µM) or oestrogen (10, 30 or 100 nM).
Subsequent to the relevant incubation, the aortic rings were mounted in organ baths filled with warmed (37 °C) and gas-equilibrated (95% O2, 5% CO2) Krebs solution containing (in mM) CaCl2 1.6, MgSO4 1.17, EDTA 0.026, NaCl 130, NaHCO3 14.9, KCl 4.7, KH2PO4 1.18, and glucose 5. Isometric tension of the rings was measured with force displacement transducers (Danish Myo Technology), digitized using PowerLab and displayed on a Macintosh computer. A preload tension of 1.5 g was applied and the rings were equilibrated for 60 min, followed by measurements of the concentration-dependent contraction to phenylephrine (10−9– 10−4 M) and in rings pre-contracted with phenylephrine (10−6M), relaxation to acetylcholine (10−9– 10−4M).
In Vitro
EA.hy926 cells [16] were plated in a 12-, 24- or 96-well plates and grown in DMEM media supplemented with 3% FCS. Endothelial cells from PARP+/+ and PARP−/− mice were isolated and cultured as previously described [17]. The following measurements were then taken.
Oxidative Stress
Oxidative stress was quantified by using the dichlorofluorescein (DCF) assay. Following the treatment protocol, the experimental medium was removed and replaced with 100 µl DMEM medium without FCS containing 5 µM DCF and incubated for 30 min. The DCF containing medium was removed, cells were washed twice with 100 µL PBS buffer before a final 100 µl of PBS buffer was added to each well and the plate placed in a fluorescence plate reader (Biotek Synergy) for 30 min with the wavelength of excitation set at 485 nm and emission set at 528 nm and readings taken every 5 min. Data are expressed as % change in fluorescence at 30 min from time 0 before being compared to untreated cells and expressed as a % of control.
Poly (ADP-Ribose) Polymerase (PARP) Activity
PARP activity was measured as previously described [18]. Briefly, the medium was removed and replaced with 0.5 ml HEPES (pH 7.5) containing 0.01% digitonin and 3H-NAD (0.5 µCi ml−1) and the cells incubated for 20 min at 37 °C. The cells were then scraped from the wells and placed in an Eppendorf tubes containing 200 µl of ice-cold 50% TCA (w/v); the tubes were then placed at 4 °C. After 4 h the tubes were centrifuged at 1800 g for 10 min and the supernatant removed, the pellet was washed twice with 500 µl ice-cold 5% TCA. The pellet was solubilized in 250 µl NaOH (0.1 M) containing 2% SDS overnight at 37 °C; the PARP activity was then determined by measuring the radioactivity incorporated using a Wallac scintillation counter. The solubilized protein (250 µl) was mixed with 5 ml of scintillant (ScintiSafe Plus, Fisher) before being counted for 10 min. Results are expressed as a percentage of the PARP activity observed in untreated cells.
Cell Viability
Cell viability was determined by the reduction of yellow MTT into a purple formazan product by mitochondrial dehydrogenases of metabolically active cells. Following the treatment period, the experimental medium was removed and 100 µl MTT (1 mg/ml) added. After 1 h incubation, the MTT solution was carefully removed and the purple crystals were solubilized in 100 µl of DMSO. The DMSO was transferred to an ELISA plate and absorbance measured at 550 nm with a 620 nm Ref. [19]. Results were expressed as a percentage of the absorbance observed in untreated cells.
Apoptosis and Necrosis Levels
Apoptosis and necrosis were evaluated using Hoeschst/propidium iodide staining. Following 24 h exposure to the appropriate treatment protocol, the medium was removed and replaced with 100 µl of media containing 10 µg/ml of both Hoechst 33342 and propidium iodide. Cells were then visualized using an inverted Axiovert 25 (Zeiss) fluorescent microscope set at excitation and emission wavelengths of 365 and 397 nm, respectively. Apoptotic cells being distinguished with characteristic nuclear fragmentation and intense staining of condensed chromatin, while necrotic cells were identified by red propidium iodide staining of the cytoplasm in cells with damaged plasma membranes. Results were expressed as % of apoptotic, necrotic or live cells with 500 nuclei being randomly counted in each treatment per experiment.
Statistical Analysis
Results are presented as mean ± standard error of the mean (SEM). Repeated measures analysis of variance or Student’s t test was used to compare mean values as appropriate. Differences were considered significant when p < 0.05.
Results
Efavirenz But Not Tenofovir or Emtricitabine Exposure Results in Concentration- and Time-Dependent Endothelial Cell Dysfunction
The effect of short-term exposure to anti-retroviral drugs on male rat endothelial cell function was investigated by exposing aortic rings to Efavirenz, Tenofovir or Emtricitabine at 1, 3 or 10 µM for 2, 4 and 6 h. Endothelial cell function was assessed by the ability of the endothelial cell to produce nitric oxide in response to ACh and cause subsequent vascular smooth muscle cell relaxation.
Efavirenz exposure resulted in a time- and concentration-dependent impairment of ACh-mediated male rat aortic ring relaxation (Fig. 1). There was a significant increase in the EC50 concentration of acetylcholine following Efavirenz exposure as compared to untreated rings (Table 1a). Tenofovir and Emtricitabine exposure had no effect on acetylcholine-mediated aortic ring relaxation (data not shown) with no significant changes in the EC50 for acetylcholine (Table 1b, c).
Exposure of ex vivo aortic rings to Efavirenz for 2 h (a), 4 h (b) or 6 h (c) concentration-dependently impairs the ACh-relaxant response. Thoracic aortic rings obtained from male Sprague–Dawley rats were exposed to 1, 3 or 10 µM Efavirenz for 2, 4 or 6 h. Following Efavirenz exposure ACh-induced endothelium-dependent relaxation was determined. Data are expressed as mean ± SEM from 6–8 animals; **p < 0.01 versus untreated rings
Efavirenz, Tenofovir and Emtricitabine exposure had no effect on the phenylephrine-mediated contraction or relaxation to the nitric oxide donor S-nitroprusside of the aortic rings (data not shown).
Efavirenz But not Tenofovir or Emtricitabine Exposure Results in Loss of Endothelial Cell Viability, Increase in Cellular Oxidative Stress and Increase in Apoptosis and Necrosis Levels
Efavirenz caused a dose-dependent decrease in EA.hy926 endothelial cell viability following 24 h exposure as measured by the MTT assay (Fig. 2). Exposure of endothelial cells to Efavirenz for 24 h also caused a dose-dependent increase in both apoptosis and necrosis levels (Table 2a). Neither Tenofovir nor Emtricitabine had any effect on endothelial cell viability (Fig. 2) or on apoptosis and necrosis levels (Table 2b, c).
Exposure of EA.hy926 cells for 24 h to Efavirenz increased levels of oxidative stress by 30 ± 7, 28 ± 6 and 32 ± 12% for 3, 10 and 30 µM, respectively (p < 0.05 vs. untreated cells). There was no increase in EA.hy926 cellular oxidative stress following exposure to Tenofovir or Emtricitabine even up to 100 µM (data not shown).
Inhibition of PARP Protects Against Efavirenz-Mediated Endothelial Cell Dysfunction
To determine whether Efavirenz-mediated activation of PARP mediates the observed endothelial cell dysfunction and loss of cell viability, we pharmacologically inhibited PARP with PJ-34 [20].
Exposure to 10 µM Efavirenz for 4 h significantly impaired endothelial cell function as assessed by acetylcholine-mediated vascular ring relaxation (Fig. 3) and increased the EC50 for acetylcholine from 3.2 ± 0.4 (× 10−8 M) to 10.7 ± 3.2 (× 10−8 M) (p < 0.05). Inhibition of PARP with PJ-34 (3 µM) significantly protected against the Efavirenz-mediated endothelial cell dysfunction (Fig. 3) and partially reduced the EC50 for acetylcholine reducing it to 7.5 ± 0.1 (× 10−8 M) (p < 0.05 vs. Efavirenz 10 µM). PJ-34 alone had no effect on vascular ring contraction induced by phenylephrine or relaxation by acetylcholine (data not shown).
Efavirenz-mediated impairment of endothelium-dependent aortic ring relaxation is prevented by pharmacological inhibition of PARP. Exposure of thoracic aortic rings to 10 µM Efavirenz for 4 h significantly impaired acetylcholine-induced endothelium-dependent relaxation, an effect prevented by simultaneous incubation of the rings with the PARP inhibitor PJ-34 (3 µM). Data are expressed as mean ± SEM from 10 animals; **p < 0.01 versus untreated rings, †† p < 0.01 versus Efavirenz-treated rings
To confirm that Efavirenz was affecting the cellular activity of PARP, we carried out in vitro experiments exposing both the endothelial cell line EA.hy926 and primary mouse endothelial cells isolated from PARP+/+ and PARP−/− mice to Efavirenz and measured PARP activity.
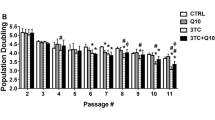
Efavirenz exposure dose- and time- dependently increased PARP activity in EA.hy926 cells (Fig. 4), while Tenofovir and Emtricitabine had no effect on PARP activity (Table 3). Exposure of EA.hy926 cells to 10 µM Efavirenz for 4 h increased PARP activity by almost fourfold (Fig. 5a), an effect significantly attenuated by simultaneous application of the PARP inhibitor PJ-34 (Fig. 5a). In addition, 10 µM Efavirenz increased PARP activity sixfold in PARP+/+ mouse endothelial cells (Fig. 5b), an effect which was attenuated both by pharmacological inhibition with PJ-34 (3 µM) and in gene knockout PARP−/− mouse endothelial cells (Fig. 5b). Basal PARP activity in PARP−/− mouse endothelial cells was found to be 58.6 ± 2% of that observed in PARP+/+ mouse endothelial cells.
Exposure of EA.hy926 cells to Efavirenz for 2 h (a), 4 h (b) or 6 h (c) concentration-dependently increased PARP activation. EA.hy926 cells were exposed to Efavirenz (1, 3, or 10 µM) for 2, 4 or 6 h prior to the measurements being taken. Data are expressed as mean ± SEM from four separate experiments with two replicates per experiment; *p < 0.05, **p < 0.01 versus untreated cells
Exposure of EA.hy926 cells (a) or mouse endothelial cells (b) to Efavirenz increased PARP activation, an effect attenuated by inhibition PARP either pharmacologically or through gene deletion. Inhibition of PARP pharmacologically with PJ-34 (3 µM) blocked the increase in PARP activity in EA.hy926 cells and mouse endothelial cells exposed to Efavirenz (EFV, 10 µM). Additionally, increased PARP activation was blocked in endothelial cells isolated from PARP-1 gene knockout mice exposed to Efavirenz (10 µM). Data are expressed as mean ± SEM from four separate experiments with 3–6 replicates per experiment; **p < 0.01 versus untreated cells †† p < 0.01 versus Efavirenz-treated cells
Efavirenz-Mediated loss of EA.hy926 Cell Viability and Increase in Apoptosis and Necrosis are Reversed by Inhibition of PARP
Inhibition of PARP with PJ-34 dose-dependently reversed the Efavirenz (30 µM)-mediated loss of endothelial cell viability (Fig. 6). PJ-34 (3 µM) also fully protected against the increased levels of apoptosis and necrosis observed following 24 h exposure to 30 µM Efavirenz (Table 4).
Efavirenz (30 µM)-mediated loss of EA.hy926 cell viability following 24 h exposure is attenuated by PARP inhibition. Data are expressed as mean ± SEM from four separate experiments with 3–6 replicates per experiment; * p < 0.05; ** p < 0.01 versus untreated cells †† p < 0.01 versus Efavirenz-treated cells
Effects of Oestrogen on Efavirenz-Mediated Endothelial Cell Dysfunction
Aortic rings isolated from female rats exposed to Efavirenz for 4 (Fig. 7a) or 6 h (Fig. 7b) showed no endothelial cell dysfunction. With the EC50 for untreated rings being 1.2 ± 0.1 (× 10−7 M) and for rings exposed to 10 µM Efavirenz for 4 and 6 h being 1.3 ± 0.2 (× 10−7 M) and 1.1 ± 0.7 (× 10−7 M), respectively (p > 0.05 vs. untreated rings).
Exposure of ex vivo aortic rings from female rats to Efavirenz for 4 h (a), or 6 h (b) had no effect on the acetylcholine-relaxant response. Efavirenz-mediated impairment of the ACh-relaxant response in ex vivo aortic rings from male rats (c) and increased PARP activity in EA.hy926 (d) was attenuated by oestrogen. Thoracic aortic rings obtained from female Sprague–Dawley rats were exposed to 1, 3 or 10 µM Efavirenz for 4 or 6 h following which acetylcholine-induced endothelium-dependent relaxation was determined (a, b). Thoracic aortic rings obtained from male Sprague–Dawley rats were exposed to 10 µM Efavirenz for 4 h ± oestrogen (10, 30 or 100 nM) before acetylcholine-induced endothelium-dependent relaxation was determined (c). Mouse endothelial cells were exposed to Efavirenz (10 µM) ± oestrogen (100 nM) for 4 h before PARP activity was measured (d). Aortic ring data are expressed as mean ± SEM from 6–8 animals; *p < 0.05; **p < 0.01 versus untreated rings; † p < 0.05; †† p < 0.01 versus Efavirenz-treated rings. Endothelial cell data are expressed as mean ± SEM from four separate experiments with 3–6 replicates per experiment; **p < 0.01 versus untreated cells †† p < 0.01 versus Efavirenz-treated cells
Simultaneous addition of oestrogen (10–100 nM) dose-dependently protected against the endothelial cell dysfunction observed in male rat aortic rings following 4 h exposure to Efavirenz (10 µM) (Fig. 7c). Oestrogen alone had no effect on vascular ring contraction induced by phenylephrine or relaxation by acetylcholine (data not shown). Oestrogen significantly reduced the increased PARP activity observed in mouse endothelial cells exposed to 10 µM Efavirenz for 4 h (Fig. 7d).
Discussion
The data presented here demonstrates for the first time that exposure of endothelial cells to the Efavirenz component of Atripla but not the Tenofovir or Emtricitabine causes direct cellular dysfunction associated with and mediated by an increased level of oxidative stress and activity of the DNA repair enzyme PARP. Additionally, oestrogen was found to protect against Efavirenz-mediated endothelial cell dysfunction likely through its inhibitory effects on PARP activation which may explain why aortic rings isolated from female rats were found to be resistant to Efavirenz-mediated dysfunction.
Efavirenz is a first-generation NNRTI designed not only to be more effective against HIV replication but also to reduce the mitochondrial toxicity associated with NRTI’s such as AZT and Stavudine cause endothelial cell dysfunction via inhibition of DNA polymerase-γ and subsequent oxidative stress [4]. Since NNRTIs such as Efavirenz are non-competitive inhibitors of HIV reverse transcriptase and do not inhibit DNA polymerase-γ, they are proposed to be less likely to have mitochondrial toxicity increasing cellular oxidative stress. However, Efavirenz has been found to in vitro to increase cellular oxidative stress in a variety of cell types including hepatocytes where it was found to have mitochondrial toxic effects and inhibit mitochondrial complex I [14]. Efavirenz also increased cellular oxidative stress in endothelial cells [12], an effect we were able to confirm, again with mitochondrial toxicity likely to be responsible as there was a disruption of endothelial mitochondrial membrane potential following Efavirenz exposure [12].
Endothelial cell-mediated control of blood pressure is exerted via production of NO due to activation of eNOS, an NADPH-dependent enzyme [2]. Increased cellular oxidative stress in endothelial cells can significantly disrupt this primary function by impairing the availability of nitric oxide either directly by reacting with nitric oxide to produce peroxynitrite, or indirectly by affecting nitric oxide synthesis [2]. Efavirenz caused a dose- and time-dependent impairment of acetylcholine-induced nitric oxide-mediated relaxation of isolated aortic rings from male rats, an effect prevented by inhibition of the DNA repair enzyme PARP. Direct measurement of PARP activity demonstrated a dose- and time-dependent increase in enzyme activity in endothelial cells exposed to Efavirenz, which could be inhibited pharmacologically or by gene disruption. Increased single-strand DNA breaks, often caused by increased oxidative or nitrosative stress [2], result in an overactivation of PARP that, using NAD+ as a substrate, catalyses the building of homopolymers of adenosine diphosphate ribose units (PAR polymers). Though PARP activation has been linked to loss of cell viability and increased levels of necrosis and apoptosis [21], observed here in endothelial cells treated with Efavirenz, we do not believe that this can explain the observed cellular dysfunction due to the timescale involved. The loss of endothelial cell function is observed following only 4 h exposure to Efavirenz suggesting that the underlying pathological effect is being mediated through interference in the cellular pathways involved in vasorelaxation. Previously, overactivation of PARP in endothelial cells has been shown to impair relaxation of the blood vessel [17] by suppression of eNOS activity through cellular depletion of NAD and NADPH levels [22]. It is therefore likely that Efavirenz-mediated oxidative stress and subsequent PARP activation are responsible for impairing the activity of eNOS and hence vascular relaxation.
The endothelial cell damaging effects of Efavirenz observed in vitro are at concentrations comparable to those seen clinically where the C max of Efavirenz has been reported to be 12.4 ± 3.7 µM, and in as many as 20% of patients the C max reaching up to 50 µM [23, 24]. The C min of Efavirenz has been reported to be 4.9 ± 2 µM (with a range between 1.6 and 8.7 µM) [25]; therefore, it may be Efavirenz-mediated endothelial cell dysfunction that accounts for the significantly increased risk of MI observed in patients [9].
Endothelial cells exposed to Efavirenz showed decreased cell viability and increased levels of necrosis and apoptosis, effects which appear to be linked to PARP overactivation as indicated by the protection provided by pharmacological inhibition of PARP. Though as indicated earlier, it seems unlikely Efavirenz-mediated loss of endothelial cell viability and increase in cell death are responsible for the Efavirenz-mediated impairment of vasorelaxation due to the timescale of the deleterious effects; however, PARP overactivation appears to be the common mediator of Efavirenz-mediated endothelial cell damage. PARP activation has been shown to cause disruption of mitochondrial membrane potential and ultimately destruction of the mitochondria as demonstrated by broken cristae and swelling [21]. This Efavirenz-mediated increase in cellular PARP activation may also explain the loss of mitochondrial function in endothelial cells reported following Efavirenz exposure [12].
PARP activation has been shown to mediate both necrosis and apoptosis [21]. Depletion of cellular levels of NAD and high-energy phosphates by overactivation of PARP has been shown to result in cellular necrosis [26], with inhibitors of PARP maintaining cellular pools of NAD, ATP, etc. cellular necrosis can be prevented. PARP activation via the production of the PAR polymer has also been shown to regulate apoptosis [26], the PAR polymer mediates the release of apoptotic proteins such as apoptosis inducing factor (AIF) [27] and cytochrome C [28] from the mitochondria. Inhibition of PARP blocks both the AIF- and cytochrome C-mediated apoptotic pathways [21]. In hepatic cells, Efavirenz was shown to reduce the mitochondrial levels of both cytochrome C and AIF [13], suggesting both PARP-regulated pathways are involved in Efavirenz-mediated cellular apoptosis; hence, this may be the reason PARP inhibition was so protective in endothelial cells. Inhibition of PARP has also been linked to cellular protection from autophagy [29] through maintaining the activation of the AKT/mTOR pathway, Efavirenz increases autophagy in endothelial cells leading to apoptosis [30] and this pathway may also be blocked by PARP inhibition.
The other two components of the Atripla HAART medication Emtricitabine and Tenofovir showed no direct damaging effects on endothelial cell function, viability or levels of apoptosis and necrosis. This is likely to be because whereas Efavirenz increased cellular oxidative stress and PARP activation, we observed no such increase with either Tenofovir or Emtricitabine. The concentrations of Emtricitabine and Tenofovir used in this study are relatable to the C max observed clinically being 7.28 and 1.03 µM [31, 32], respectively, so our data do support the clinical evidence that Tenofovir and Emtricitabine have a good cardiovascular safety profile. However, due to the combination of Efavirenz, Emtricitabine and Tenofovir being found to have increased endothelial damaging effects than Efavirenz alone [6], the possibility of metabolites of Emtricitabine or Tenofovir having endothelial cell damaging effects or if these drugs affect the bioavailability and plasma concentration of Efavirenz cannot be ruled out.
There seems to be a gender difference with regard to the incidence of cardiovascular side effects suffered by HIV patients on HAART, with women being less affected than men [33], however, this is reversed in post-menopausal female subjects on HAART who display an increased cardiovascular risk than their male counterparts due to the loss of their natural oestrogen protection [34]. Oestrogen has shown to be protective to the cardiovascular system against a wide variety of disease, and mechanistic studies have linked this protection to modulating injury-induced inflammation, growth factor expression and oxidative stress. Oestrogen has also been shown to affect PARP activation not directly inhibiting the enzyme but indirectly where PARP and the oestrogen receptor-α (ERα) interact when oestrogen is bound to the receptor [35]. Male mice treated with oestrogen have lower liver levels of PARP activation following lipopolysaccharide (LPS) treatment as compared to control [35], and castrated males have lower PARP activity in peripheral blood monocytes [36]. This interaction between PARP and ERα has been shown to have a physiological role with PARP being a key regulator of ERα in controlling ERα transactivation and gene transcription [37]. Oestrogen has also been shown to protect against hydrogen peroxide-mediated necrosis and reduce PARP activity in bone marrow-derived macrophages from male mice [38].
Acetylcholine-induced nitric oxide-mediated relaxation of female aortic rings was unaffected by exposure to Efavirenz suggesting a protective effect of oestrogen exposure. Gender differences in the vascular effects of LPS exposure for 3 h have been observed previously with LPS causing a significant impairment of endothelial cell function of aortic rings isolated from male rats but had no effect on the endothelial cell function of aortic rings isolated from female rats [35]. Simultaneous application of oestrogen protected male aortic rings from Efavirenz-mediated dysfunction, as well as inhibiting Efavirenz-mediated PARP activation in endothelial cells. Due to the short exposure time required for oestrogen to exert its endothelial cell protective effect against Efavirenz, it is unlikely that this is a gene transcription-dependent effect or increased levels of cellular protective anti-oxidant enzymes which oestrogen has been reported to induce [39]. It is very likely that the oestrogen-mediated inhibition of Efavirenz-induced PARP activation is via an interaction between ERα and PARP. However, oestrogen and selective oestrogen receptor modulators such as raloxifene have been shown to protect against oxidative stress-induced endothelial cell dysfunction by increasing the activity of eNOS by phosphorylation of the enzyme [40] and this cannot be ruled out as mediating part of the observed oestrogen protective effect. Similarly, though endothelial cell function in aortic rings from female rats may be protected from Efavirenz-mediated dysfunction because of an oestrogen-mediated reduction in PARP activation, these endothelial cells may also have higher levels of anti-oxidant defences and/or eNOS activity. However, it is clear that the effects of oestrogen on a cellular level protect endothelial cells from HAART drug-induced damage, and this may explain the clinical observations that female HIV patients, at least pre-menopause, have less cardiovascular side effects [34].
Based on the data presented here, we conclude that exposure to Efavirenz but not the other components of Atripla, Tenofovir and Emtricitabine leads to increased oxidative stress, activation of PARP and impaired function of vascular endothelial cells. This impairment of vasorelaxation may predispose HIV patients on Efavirenz-based HAART regimens to the development of cardiovascular complications including hypertension and increased risk of MI. Indeed, overactivation of PARP may account for the impaired brachial artery flow-mediated dilation, an indicator of endothelial cell dysfunction, observed in HIV-infected patients on Efavirenz therapy [8]. We also propose that the observed gender differences in risk of developing cardiovascular complications in HIV patients on HAART may be a result of oestrogen-induced impairment of PARP activation protecting endothelial cell function. With HIV infection becoming a chronic disease due to effective HAART understanding, the underlying mechanisms of HAART-mediated cardiovascular complications as well as the impact of any physiological changes such as menopause on HAART side effects are essential. Though Efavirenz as a first-generation NNRTI has significantly less cardiovascular damaging effects than the original NRTIs, there is still more research needed to improve the cardiovascular safety profile of this class of anti-retrovirals either by direct modification of the drugs or development of protective adjuvant therapies.
References
Apostolova, N., Blas-Garcia, A., & Esplugues, J. V. (2011). Mitochondrial interference by anti-HIV drugs: mechanisms beyond Pol-gamma inhibition. Trends in Pharmacological Sciences, 32, 715–725.
Pacher, P., Beckman, J. S., & Liaudet, L. (2007). Nitric oxide and peroxynitrite in health and disease. Physiological Reviews, 87, 315–424.
Gao, R. Y., Mukhopadhyay, P., Mohanraj, R., Wang, H., Horvath, B., Yin, S., et al. (2011). Resveratrol attenuates azidothymidine-induced cardiotoxicity by decreasing mitochondrial reactive oxygen species generation in human cardiomyocytes. Molecular Medicine Reports, 4, 151–155.
Jiang, B., Hebert, V. Y., Li, Y., Mathis, J. M., Alexander, J. S., & Dugas, T. R. (2007). HIV antiretroviral drug combination induces endothelial mitochondrial dysfunction and reactive oxygen species production, but not apoptosis. Toxicology and Applied Pharmacology, 224, 60–71.
Worm, S. W., Sabin, C., Weber, R., Reiss, P., El-Sadr, W., Dabis, F., et al. (2010). Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the data collection on adverse events of anti-HIV drugs (D:A:D) study. Journal of Infectious Diseases, 201, 318–330.
Gupta, S. K., Shen, C., Moe, S. M., Kamendulis, L. M., Goldman, M., & Dube, M. P. (2012). Worsening endothelial function with efavirenz compared to protease inhibitors: a 12-month prospective study. PLoS ONE, 7, e45716.
Maggi, P., Bellacosa, C., Carito, V., Perilli, F., Lillo, A., Volpe, A., et al. (2011). Cardiovascular risk factors in patients on long-term treatment with nevirapine- or efavirenz-based regimens. Journal of Antimicrobial Chemotherapy, 66, 896–900.
Gleason, R. L., Jr., Caulk, A. W., Seifu, D., Rosebush, J. C., Shapiro, A. M., Schwartz, M. H., et al. (2016). Efavirenz and ritonavir-boosted lopinavir use exhibited elevated markers of atherosclerosis across age groups in people living with HIV in Ethiopia. Journal of Biomechanics, 49, 2584–2592.
Durand, M., Sheehy, O., Baril, J. G., Lelorier, J., & Tremblay, C. L. (2011). Association between HIV infection, antiretroviral therapy, and risk of acute myocardial infarction: a cohort and nested case-control study using Quebec’s public health insurance database. Journal of Acquired Immune Deficiency Syndromes, 57, 245–253.
Kim, C., Gupta, S. K., Green, L., Taylor, B. M., Deuter-Reinhard, M., Desta, Z., et al. (2011). Abacavir, didanosine and tenofovir do not induce inflammatory, apoptotic or oxidative stress genes in coronary endothelial cells. Antiviral Therapy, 16, 1335–1339.
De Pablo, C., Orden, S., Calatayud, S., Marti-Cabrera, M., Esplugues, J. V., & Alvarez, A. (2012). Differential effects of tenofovir/emtricitabine and abacavir/lamivudine on human leukocyte recruitment. Antiviral Therapy, 17, 1615–1619.
Jamaluddin, M. S., Lin, P. H., Yao, Q., & Chen, C. (2010). Non-nucleoside reverse transcriptase inhibitor efavirenz increases monolayer permeability of human coronary artery endothelial cells. Atherosclerosis, 208, 104–111.
Apostolova, N., Gomez-Sucerquia, L. J., Moran, A., Alvarez, A., Blas-Garcia, A., & Esplugues, J. V. (2010). Enhanced oxidative stress and increased mitochondrial mass during Efavirenz-induced apoptosis in human hepatic cells. British Journal of Pharmacology, 160, 2069–2084.
Blas-Garcia, A., Apostolova, N., Ballesteros, D., Monleon, D., Morales, J. M., Rocha, M., et al. (2010). Inhibition of mitochondrial function by efavirenz increases lipid content in hepatic cells. Hepatology, 52, 115–125.
Hulgan, T., Morrow, J., D’Aquila, R. T., Raffanti, S., Morgan, M., Rebeiro, P., et al. (2003). Oxidant stress is increased during treatment of human immunodeficiency virus infection. Clinical Infectious Diseases, 37, 1711–1717.
Edgell, C. J., McDonald, C. C., & Graham, J. B. (1983). Permanent cell line expressing human factor VIII-related antigen established by hybridization. Proceedings of the National Academy of Sciences, 80, 3734–3737.
Garcia Soriano, F., Virag, L., Jagtap, P., Szabo, E., Mabley, J. G., Liaudet, L., et al. (2001). Diabetic endothelial dysfunction: the role of poly(ADP-ribose) polymerase activation. Nature Medicine, 7, 108–113.
Helyar, S. G., Patel, B., Headington, K., El Assal, M., Chatterjee, P. K., Pacher, P., et al. (2009). PCB-induced endothelial cell dysfunction: role of poly(ADP-ribose) polymerase. Biochemical Pharmacology, 78, 959–965.
Mabley, J. G., Suarez-Pinzon, W. L., Hasko, G., Salzman, A. L., Rabinovitch, A., Kun, E., et al. (2001). Inhibition of poly (ADP-ribose) synthetase by gene disruption or inhibition with 5-iodo-6-amino-1,2-benzopyrone protects mice from multiple-low-dose-streptozotocin-induced diabetes. British Journal of Pharmacology, 133, 909–919.
Jagtap, P., Soriano, F. G., Virag, L., Liaudet, L., Mabley, J., Szabo, E., et al. (2002). Novel phenanthridinone inhibitors of poly (adenosine 5′-diphosphate-ribose) synthetase: potent cytoprotective and antishock agents. Critical Care Medicine, 30, 1071–1082.
Virag, L., Robaszkiewicz, A., Rodriguez-Vargas, J. M., & Oliver, F. J. (2013). Poly(ADP-ribose) signaling in cell death. Molecular Aspects of Medicine, 34, 1153–1167.
Soriano, F. G., Pacher, P., Mabley, J., Liaudet, L., & Szabo, C. (2001). Rapid reversal of the diabetic endothelial dysfunction by pharmacological inhibition of poly(ADP-ribose) polymerase. Circulation Research, 89, 684–691.
Marzolini, C., Telenti, A., Decosterd, L. A., Greub, G., Biollaz, J., & Buclin, T. (2001). Efavirenz plasma levels can predict treatment failure and central nervous system side effects in HIV-1-infected patients. AIDS, 15, 71–75.
Burger, D., van der Heiden, I., la Porte, C., van der Ende, M., Groeneveld, P., Richter, C., et al. (2006). Interpatient variability in the pharmacokinetics of the HIV non-nucleoside reverse transcriptase inhibitor efavirenz: the effect of gender, race, and CYP2B6 polymorphism. British Journal of Clinical Pharmacology, 61, 148–154.
la Porte, C. J., Sabo, J. P., Beique, L., & Cameron, D. W. (2009). Lack of effect of efavirenz on the pharmacokinetics of tipranavir-ritonavir in healthy volunteers. Antimicrobial Agents and Chemotherapy, 53, 4840–4844.
Andrabi, S. A., Dawson, T. M., & Dawson, V. L. (2008). Mitochondrial and nuclear cross talk in cell death: parthanatos. Annals of the New York Academy of Sciences, 1147, 233–241.
Yu, S. W., Andrabi, S. A., Wang, H., Kim, N. S., Poirier, G. G., Dawson, T. M., et al. (2006). Apoptosis-inducing factor mediates poly(ADP-ribose) (PAR) polymer-induced cell death. Proceedings of the National Academy of Sciences, 103, 18314–18319.
Chen, M., Zsengeller, Z., Xiao, C. Y., & Szabo, C. (2004). Mitochondrial-to-nuclear translocation of apoptosis-inducing factor in cardiac myocytes during oxidant stress: potential role of poly(ADP-ribose) polymerase-1. Cardiovascular Research, 63, 682–688.
Liu, F., Jiang, N., Xiao, Z. Y., Cheng, J. P., Mei, Y. Z., Zheng, P., et al. (2016). Effects of poly (ADP-ribose) polymerase-1 (PARP-1) inhibition on sulfur mustard-induced cutaneous injuries in vitro and in vivo. PeerJ, 4, e1890.
Weiss, M., Kost, B., Renner-Muller, I., Wolf, E., Mylonas, I., & Bruning, A. (2016). Efavirenz causes oxidative stress, endoplasmic reticulum stress, and autophagy in endothelial cells. Cardiovascular Toxicology, 16, 90–99.
Molina, J. M., Peytavin, G., Perusat, S., Lascoux-Combes, C., Sereni, D., Rozenbaum, W., et al. (2004). Pharmacokinetics of emtricitabine, didanosine and efavirenz administered once-daily for the treatment of HIV-infected adults (pharmacokinetic substudy of the ANRS 091 trial). HIV Medicine, 5, 99–104.
Markowitz, M., Zolopa, A., Squires, K., Ruane, P., Coakley, D., Kearney, B., et al. (2014). Phase I/II study of the pharmacokinetics, safety and antiretroviral activity of tenofovir alafenamide, a new prodrug of the HIV reverse transcriptase inhibitor tenofovir, in HIV-infected adults. Journal of Antimicrobial Chemotherapy, 69, 1362–1369.
Neumann, T., Woiwod, T., Neumann, A., Ross, B., Von Birgelen, C., Volbracht, L., et al. (2004). Cardiovascular risk factors and probability for cardiovascular events in HIV-infected patients. Part II: gender differences. European Journal of Medical Research, 9, 55–60.
Triant, V. A., Lee, H., Hadigan, C., & Grinspoon, S. K. (2007). Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. Journal of Clinical Endocrinology and Metabolism, 92, 2506–2512.
Mabley, J. G., Horvath, E. M., Murthy, K. G., Zsengeller, Z., Vaslin, A., Benko, R., et al. (2005). Gender differences in the endotoxin-induced inflammatory and vascular responses: potential role of poly(ADP-ribose) polymerase activation. Journal of Pharmacology and Experimental Therapeutics, 315, 812–820.
Zaremba, T., Ketzer, P., Cole, M., Coulthard, S., Plummer, E. R., & Curtin, N. J. (2009). Poly(ADP-ribose) polymerase-1 polymorphisms, expression and activity in selected human tumour cell lines. British Journal of Cancer, 101, 256–262.
Zhang, F., Wang, Y., Wang, L., Luo, X., Huang, K., Wang, C., et al. (2013). Poly(ADP-ribose) polymerase 1 is a key regulator of estrogen receptor alpha-dependent gene transcription. Journal of Biological Chemistry, 288, 11348–11357.
Jog, N. R., & Caricchio, R. (2013). Differential regulation of cell death programs in males and females by Poly (ADP-Ribose) Polymerase-1 and 17beta estradiol. Cell Death and Disease, 4, e758.
Wing, L. Y., Chen, Y. C., Shih, Y. Y., Cheng, J. C., Lin, Y. J., & Jiang, M. J. (2009). Effects of oral estrogen on aortic ROS-generating and -scavenging enzymes and atherosclerosis in apoE-deficient mice. Experimental Biology and Medicine (Maywood), 234, 1037–1046.
Wong, C. M., Yung, L. M., Leung, F. P., Tsang, S. Y., Au, C. L., Chen, Z. Y., et al. (2008). Raloxifene protects endothelial cell function against oxidative stress. British Journal of Pharmacology, 155, 326–334.
Acknowledgements
Mary Faltz was supported by the Fonds National De La Recherche in Luxembourg (Reference 1007977).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faltz, M., Bergin, H., Pilavachi, E. et al. Effect of the Anti-retroviral Drugs Efavirenz, Tenofovir and Emtricitabine on Endothelial Cell Function: Role of PARP. Cardiovasc Toxicol 17, 393–404 (2017). https://doi.org/10.1007/s12012-016-9397-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-016-9397-4