Abstract
This study demonstrated the mechanisms of boron effects in a rat model and provided a scientific basis for the rational of boron use. These findings were achieved by investigating the effects of boron (10, 20, 40, 80, 160, 320, and 640 mg/L in drinking water or 1.5, 3, 6, 12, 24, 48, and 96 mg/kg BW) on rat serum immunoglobulins (IgGs), splenic cytokines, lymphocyte subsets, as well as on lymphocyte proliferation and apoptosis. Addition of 20 (3) and 40 (6) mg/L (mg/kg BW) of boron to drinking water significantly increased rat serum IgG concentrations, splenic IFN-γ and IL-4 expression as well as the number of splenic CD3+, CD4+ and proliferating cell nuclear antigen (PCNA)+ cells. Supplementation of drinking water with 40 mg/L (6 mg/kg BW) boron also markedly increased splenic IL-2 expression and the CD4+/CD8+ cell ratio and reduced splenic CD8+ cell number. Supplementation with 80 mg/L (12 mg/kg BW) boron significantly increased CD3+ and PCNA+ cell numbers (P < 0.05) and decreased the IL-10 expression in the spleen. Addition of 320 (48) and 640 (96) mg/L (mg/kg BW) boron markedly reduced the serum IgG concentrations; splenic IL-2 and IL-10 expression; the number of CD3+, CD4+ and PCNA+ cells; and increased the number of splenic CD8+ and caspase-3+ cells and promoted caspase-3 expression in CD3+ cells. In conclusion, these findings suggest that the supplementation of rat drinking water with 20(3) and 40(6) mg/L (mg/kg BW) boron can markedly enhance humoral and cellular immune functions, while boron concentrations above 320 mg/L (48 mg/kg BW) can have an inhibitory effect or even toxicity on immune functions. These results exhibit a U-shaped response characteristic of low and high doses of boron supplementation on immune function and imply that proper boron supplementation in food for humans and animals could be used as an immunity regulator.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Boron is widely used in various areas, including agriculture, food, cosmetics, and pharmaceutical industries [1], and boron environmental concentration increases year after year. Therefore, a number of studies have focused on the defining the beneficial and harmful effects of boron on human and animal health. Previous studies have shown that boron is a trace element required for living creatures and that it is indispensable for humans and animals. Boron is a regulator of metabolism [2–4] and plays an important role in the maintenance of normal physiological functions in animals [5]. Deprivation or deficiency of boron can induce disorders of immunity, reproduction, and embryonic development. Researchers found that a shortage of boron exacerbated adjuvant arthritis [6], resulted in testicular and ovarian atrophy, increased mortality rate of frog and zebrafish embryos, and impaired development of mouse embryos [2, 4, 7]. Appropriate amounts of boron were shown to promote bone development, improve bone strength [8], and to enhance growth and productive performance in animals [9, 10]. In addition, it was shown to modulate the levels of T3 and T4 [11], which affect insulin and luteinizing hormone levels and affect anti-oxidative function and capacity of DNA against oxidative damage [12, 13]. Recent findings indicated that boron was related with innate and acquire immune responses. Proper boron supplementation can increase the percentage of hemocytes and neutrophils [14], enhance antibody levels in rats injected with the human typhoid vaccine [15], increase the number of circulatory natural killer (NK) cells and CD8+/CD4− lymphocytes [16], and suppress the expression of LPS-induced pro-inflammatory cytokine TNF-α [17]. In contrast, a high dose of boron resulted in testicular atrophy, decreased sperm count, abnormal embryonic development, and increased mortality rate [18, 19]. It also resulted in gastrointestinal disorders, swelling and granular degeneration of renal tubular cells [20], and impaired growth of immune organs with significant structural defects [21]. However, the exact required amounts of boron for growth and development in animals remain unclear, and the harmful amounts also need more studies.
Immunity protects the body against infection by endogenous and exogenous pathogens and plays a decisive role in maintaining health. Although the effect of boron on immune functions in animals has been verified, the relationship between the amount of boron consumed and the immune functions in mammals as well as the underlying mechanisms are still unclear. By studying the effects of various boron concentrations on indicators, such as splenic cytokines, T cell subsets, and splenic lymphocyte proliferation and apoptosis, the present study demonstrated the mechanisms of boron effects on immunity and provided a scientific basis for the rational use of boron.
Methods
Experimental Animals and Animal Feeding
Healthy 96 specific pathogen-free (SPF) 23-day-old male Sprague Dawley (SD) rats (weight 55 ± 2 g, lot: 2013-09-02) were purchased from the Laboratory Animal Center of the Anhui Medical University in Anhui province of China. The study was conducted at the Anhui Science and Technology University during the fall (September to December) of 2013 and lasted 70 days. The use of all experimental animals was reviewed and approved by the Anhui Laboratory Animal Care Committee. All animal experimental procedures were performed according to the “Guide for Laboratory Animal Care and Use” and complied with the “Guide for National Laboratory Animal Healthcare and Use.” Animal feed was purchased from the Qinglongshan breeding farm in the Jiangning District of Nanjing city. The main nutritional ingredients of the feed (serial number: GB14921.1-2001) were ≤10% water, ≥18.15% crude protein, ≥4.03% crude fat, ≥5.12% crude fiber, and ≥7.94% crude ash. The boron concentration was 1.71 mg/kg in this rat diet.
Experimental Design
After 1 week of adaptive feeding, the 96 rats were randomly assigned to a control group and 7 test groups, of 12 rats each. The non-treated control group (NC) was given autoclaved distilled water while the test groups (groups 1 to 7) were given boron-supplemented water in the form of boric acid. For these animals, concentrations of 10 (1.5), 20 (3), 40 (6), 80 (12), 160 (24), 320 (48), and 640 (96) mg/L (mg/kg body weight) boron, respectively, were added to the distilled drinking water. No boron was detected in the distilled water, prior to supplementation. Water intake of each rat was recorded before the experiment, and water containing boron was offered according to average water intake during experiment. The experiments were conducted over 60 days in the Laboratory Animal Center of Anhui Science and Technology University. Animals were housed in separate ventilated cages at 22–25 °C, 50–60% humidity, light/dark cycle = 14:10, and had free access to food and water. All cage covers and water bottles were sterilized before use. At 8:30 every morning during the experimental period, all of the rats were monitored for their mental state, activity level, and tail color. The water and food intake were recorded, and the clinical criteria were used to assess animal health and general welfare. If rats became ill, severely ill, or even moribund, they were anesthetized, weighed, and dissected to expose the heart for blood collection, and then bleed to death.
Sample Collection and Preparation
At the end of the study, ten rats from each group were anesthetized by gas anesthesia systems (ABS) under the euthanasia condition: 4–5% inhalant anesthesia (isoflurane) was administered for induction followed by 1–2% for maintenance; while the rat was being anesthetized, weighed, the chest opened to expose the heart, the blood collected from the heart, then the animal bled to death. Sterile, procoagulant, and heparin anticoagulant vacuum blood collection tubes (Sekisui Medical Co., Ltd., Japan) were used to collect procoagulant and anticoagulant blood, respectively, from the right ventricle. The anticoagulant blood was used for blood physiological index detection, and the serum was separated from the procoagulant blood by centrifugation. The spleen was extracted and weighed. A portion was excised and fixed in 4% paraformaldehyde in PBS for immunohistochemistry (IHC), and the rest was stored in liquid nitrogen for cytokine detection.
Detection of Serum Immunoglobulins
The procoagulant blood was left at room temperature for 2 h (h) and then centrifuged for 15 min (min) at 3000 rpm/min at 4 °C (Beckman Allegra X-30R; Beckman Coulter Trading Co., Ltd., China) to separate the serum. Serum concentrations of immunoglobulin (Ig)G, IgA, and IgM were determined using the automated biochemical analyzer (BS-200, Mindray Medical International Limited, China).
Detection of Cytokine Concentrations
Spleen tissues were homogenized over an ice bath and centrifuged for 15 min at 3000 rpm/min at 4 °C. The supernatant was collected and stored at −80 °C. Splenic IL-2, IL-4, IL-10 and IFN-γ concentrations were determined using the ELISA test kits (RD Biosciences, Inc., USA) following the manufacturer’s protocols, and the absorbance was measured using a microplate reader (Multiskan GO, Thermo Fisher Scientific Inc., USA). The correlation coefficients of the IL-2, IL-4, IL-10 and IFN-γ standard curves were 0.9915, 0.9912, 0.9903, and 0.9901, respectively.
Immunohistochemistry
The expression levels of CD3, CD4, CD8 proliferating cell nuclear antigen (PCNA) and the apoptosis protein caspase-3 in splenic T cells were determined using the streptavidin-biotin-peroxidase complex (SABC) immunohistochemical method. After 72 h of fixation in 4% paraformaldehyde (in PBS), spleen tissues were washed, dehydrated with graded ethanol series, and cleared in xylene, embedded in paraffin. Samples were laterally sliced into 6-μm-thick sequential sections using a paraffin section machine (RM2235, Leica Biosystems, Germany). One tissue section per 30 sections was fixed on a poly-lysine-coated glass slide and stored at 37 °C for immunohistostaining.
Immunohistostaining
Tissue sections were dewaxed in xylene; rehydrated in graded ethanol and distilled water; washed three times in 0.01 mol/L PBS (pH 7.4), for 5 min each wash; and immersed in 0.1 mol/L citrate buffer (pH 6.0). Antigen was retrieved for 15 min using the microwave antigen retrieval method followed by cooling to room temperature, as previously described in detail [22]. Sections were then washed three times in 0.01 mol/L PBS for 5 min each wash and incubated for 30 min at room temperature in 3% hydrogen peroxide (prepared in methanol) to remove endogenous peroxidase followed by washing three more times in 0.01 mol/L PBS for 5 min each wash. Sections were then incubated for 30 min at room temperature in 10% normal goat serum (prepared in 0.01 mol/L PBS) to block non-specific secondary binding. After removal of the normal goat serum, drops of rabbit anti-rat or mouse anti-human primary antibody were added and incubated at 4 °C overnight. On the next day, tissue sections were allowed to reach room temperature for 30 min, washed three times in 0.01 mol/L PBS for 5 min each wash, followed by addition of drops of biotinylated goat anti-rabbit (1:200 dilution, Proteintech Group, Inc., USA), or horse anti-mouse secondary antibody (1:200 dilution, ZSGB-BIO OriGene, China), and incubation at 37 °C for 2 h. Sections were washed three times in 0.01 mol/L PBS for 5 min each wash, followed by addition of drops of streptavidin-labeled tertiary antibody (1:200 dilution, Proteintech Group, Inc., USA) and incubation at 37 °C for 2 h. Finally, sections were washed two times using PBS (0.01 mol/L) for 5 min each time. 3,3′-Diaminobenzidine (DAB) substrate solution was pre-incubated for 30 min at room temperature (Sigma-Aldrich, Inc., USA) and added to the sections. Incubation with DAB chromogen was allowed for 5 min; then, nuclei were stained with hematoxylin for 3 min. This was followed by dehydration with graded ethanol, clearing in xylene, and mounting with neutral gum. Primary antibodies used were as follows: rabbit anti-CD3 polyclonal antibody (Abcam Inc., USA, 1:200 dilution), rabbit anti-CD4 polyclonal antibody (Santa Cruz Biotechnology, Inc., USA, 1:200 dilution), rabbit anti-CD8 polyclonal antibody (Santa Cruz Biotechnology, Inc., USA, 1:200 dilution), mouse anti-human PCNA polyclonal antibody dilution (Cell Signaling Technology, Inc., USA, 1:2000 dilution), and rabbit anti-caspase-3 polyclonal antibody (Proteintech Group, Inc., USA, 1:200 dilution).
Spleen IHC sections were visualized and photographed using the Olympus BX51 Upright Fluorescence Microscope camera system (Olympus Co. Ltd., Japan). Fifteen spleen transverse sections were selected from each rat of each treatment group for immunohistostaining. Five regions were evenly selected from the top, bottom, left, right, and center areas of each section, to be photographed. Statistical analysis of stained positive cells was done using the IPP6.0 image analysis software.
Double Immunofluorescence
Expression of the apoptotic protein caspase-3 in splenic CD3+ T cells was detected using double immunofluorescence labeling. With the previous steps the same as those of IHC, tissue sections were incubated overnight at 4 °C with a rabbit anti-CD3 polyclonal antibody (Abcam Inc., USA, 1:200 dilution). The following day, sections were warmed to room temperature for 30 min, washed three times in 0.01 mol/L PBS for 5 min each wash, followed by addition of drops of DyLight 549-labeled goat anti-rabbit secondary antibody (CWBIO, China, 1:200 dilution), and incubated at 37 °C for 2 h. Sections were then washed three times in 0.01 mol/L PBS for 5 min each wash and incubated with 10% normal goat serum at room temperature for 30 min; the serum was removed, and drops of rabbit anti-caspase-3 polyclonal antibody (Proteintech Group, Inc., USA, 1:200 dilution) were then added and incubated at 4 °C overnight. The next day sections were warmed to room temperature for 30 min and washed three times in 0.01 mol/L PBS for 5 min each wash; drops of DyLight 488-labeled goat anti-rabbit secondary antibody (CWBIO, China, 1:200 dilution) were added and incubated at 37 °C for 2 h and washed three more times in 0.01 mol/L PBS for 5 min each wash. Drops of 4′,6-diamidino-2-phenylindole, dilactate (DAPI) solution (Sigma-Aldrich, Inc., USA, 1:10,000 dilution) were added and incubated at room temperature for 30 min, followed by washing three more times in 0.01 mol/L PBS, for 5 min each wash, and then mounting in 75% glycerol. The results were visualized and photographed using the Olympus BX51 Upright Fluorescence Microscope camera system (Olympus Co. Ltd, Japan).
Statistical Analysis
All data were expressed as mean ± SD. One-way ANOVA was performed on the experimental data using the SPSS 22.0 statistical software (SPSS Inc., Chicago, IL, USA). Levene’s test and Kolmogorov-Smirnov test were used to determine the homogeneity of variance and normality of distribution, respectively. Significant differences in the data were analyzed by the Dunnett’s test. P < 0.05 was considered statistically significant, and P < 0.01 was considered statistically extremely significant.
Results
Effect of Boron on Serum Immunoglobulin Levels in Rats
The effect of boron on the concentrations of serum immunoglobulins in rats is shown in Fig. 1. There was no significant change in serum IgA concentration among all groups (P > 0.05). Compared with the NC group, serum IgM concentration in group 7 was significantly reduced by 38.91% (P < 0.01). Serum IgG concentrations of groups 2 and 3 were significantly increased by 12.08 and 18.46% (P < 0.05), respectively, compared to the NC group. In contrast, for groups 6 and 7, it was significantly decreased by 19.46 and 18.45% (P < 0.01), respectively, compared to the NC group.
The concentration of serum immunoglobulins in rats. The serum samples were collected from rats, followed by serum biochemical analyzer for determination of serum immunoglobulin concentrations. Compared with the 0 mg B/L, The serum IgA concentration had no significant change in the treatment groups; the serum IgM concentration in 640 mg B/L was significantly reduced by 38.91%; the serum IgG concentrations of 20 and 40 mg B/L were significantly increased by 12.08 and 18.46%, respectively; conversely, the IgG concentrations of 320 and 640 mg B/L were significantly decreased by 19.46 and 18.45%, respectively. One asterisk indicates a significant difference (P < 0.05) and two asterisks indicate an extremely significant difference (P < 0.01) in the column
Effect of Boron on Splenic Cytokine Levels in Rats
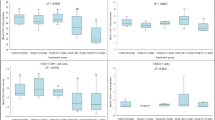
The effects of boron on splenic cytokines concentrations are shown in Fig. 2. Compared to the NC group, the IL-2 concentration was significantly increased by 8.13% (P < 0.05) in group 3, whereas it was significantly decreased by 7.76 and 11.92% (P < 0.05 or P < 0.01) in groups 6 and 7, respectively. Compared with the NC group, IFN-γ concentration in the spleen was significantly elevated by 18.47 and 24.55% (P < 0.01) in groups 2 and 3, respectively, while it was significantly reduced by 6.85 and 15.05% (P < 0.05 or P < 0.01) in groups 5 and 7, respectively. Splenic IL-4 concentration was significantly increased by 7.40 and 9.43% (P < 0.05 or P < 0.01) in groups 2 and 3, respectively, and highly significantly decreased by 9.41% (P < 0.01) in group 7. Furthermore, the splenic IL-10 concentration was markedly elevated by 6.81% (P < 0.05) in group 2 whereas it was significantly or extremely significantly reduced by 9.77, 7.67, 10.66 and 11.04% (P < 0.05 or P < 0.01) in groups 4–7, respectively.
The concentration of splenic cytokines in rats. The spleen samples were homogenized, and supernatants were collected and used in ELISA assays for measurement of IL-2 (A), INF-γ (B), IL-4 (C) and IL-10 (D) concentrations in the spleen. Compared to the 0 mg B/L, the IL-2 concentration was significantly increased by 8.13% in 40 mg B/L, whereas it was significantly decreased by 7.76 and 11.92% in 320 and 640 mg B/L, respectively; the IFN-γ concentration was significantly elevated by 18.47 and 24.55% in 20 and 40 mg B/L, respectively, while it was significantly reduced by 6.85 and 15.05% in 160 and 640 mg B/L, respectively; the IL-4 concentration was significantly increased by 7.40 and 9.43% in 20 and 40 mg B/L, respectively and highly significantly decreased by 9.41% in 640 mg B/L. Furthermore, the splenic IL-10 concentration was markedly elevated by 6.81% in 20 mg B/L, whereas it was significantly or extremely significantly reduced by 9.77, 7.67, 10.66 and 11.04% in 80–640 mg B/L, respectively. One asterisk indicates a significant difference (P < 0.05) and two asterisks indicate an extremely significant difference (P < 0.01) in the column
Effect of Boron on the Number of Splenic CD3+, CD4+, and CD8+ Lymphocytes in Rats
Results from immunohistochemical staining showed that the cytoplasm of CD3+ cells was brown whereas the cytoplasm of CD4+ and CD8+ cells was yellowish brown. CD3+ cells were mainly distributed in the splenic periarteriolar lymphoid sheaths, and they first increased then decreased following the increase of boron supplementation (Fig. 3). CD4+ and CD8+ cells were mainly distributed within and at the margins of the splenic periarteriolar lymphoid sheaths. As the boron concentration increased, the number of CD4+ cells first showed an increase then a decreasing trend, while the results were the reverse in CD8+ cells (Figs. 4 and 5). Statistics on the number of positive immune cells per unit area showed that compared to the NC group, CD3+ cell numbers were significantly increased by 26.04, 40.10 and 17.23% (P < 0.01 or P < 0.05) in groups 2, 3 and 4, respectively, whereas it was markedly reduced by 19.30 and 16.55% (P < 0.05) in groups 6 and 7, respectively. There were no significant differences in CD3+ cells in groups 1, 5 and the NC group (P > 0.05) (Fig. 6a). CD4+ cells were significantly or highly significantly elevated by 20.55 and 34.92% (P < 0.05 or P < 0.01) in groups 2 and 3, respectively, and were significantly reduced by 14.98, 23.3 and 28.24% (P < 0.05 or P < 0.01) in groups 5, 6 and 7, respectively (Fig. 6b). Moreover, CD8+ cells were highly significantly decreased by 19.52% (P < 0.01) in group 3 and significantly increased by 16.39 and 15.57% (P < 0.05) in groups 6 and 7, respectively (Fig. 6c). The ratio of CD4+/CD8+ cells per unit area first showed a clear increase then a decreasing trend, with the highest value in group 3 and lowest value in group 7 (Fig. 6d).
The distribution of CD3+ lymphocytes and CD3 expression in rat spleens. The spleen tissue sections were used in immunohistochemical staining for the expression of CD3 in the splenic lymphocytes. The CD3+ lymphocytes were stained as yellowish brown. The expression of CD3 in the splenic lymphocytes in the NC group (a) and groups 1–7 (b–h) differed as boron supplementation increased in drinking water. The negative control (i) of immunohistochemical staining is also shown. Bar = 50 μm. SC splenic cord, SN splenic nodule, PLS periarteriolar lymphoid sheaths, MZ marginal zone (color figure online)
The distribution of CD4+ lymphocytes and CD4 expression in rat spleens. The spleen tissue sections were used in immunohistochemical staining for the expression of CD4 in the splenic lymphocytes. The CD4+ lymphocytes were stained as yellowish brown. The expression of CD4 in the splenic lymphocytes in the NC (control group) (a) and groups 1–7 (b–h) differed as boron supplementation increased in drinking water. The negative control (i) of immunohistochemical staining is also shown. Bar = 50 μm. SN splenic nodule, PLS periarteriolar lymphoid sheaths, MZ marginal zone (color figure online)
The distribution of CD8+ lymphocytes and CD8 expression in rat spleens. The spleen tissue sections were used for immunohistochemical staining for the expression of CD8 in the splenic lymphocytes. The CD8+ lymphocytes were stained as yellowish brown. As indicated, the CD8 expression in the splenic lymphocytes in the NC group (a) and groups 1–7 (b–h) differed as boron supplementation increased in drinking water. The negative control (i) of immunohistochemical staining is also shown. Bar = 50 μm. MZ marginal zone, PLS periarteriolar lymphoid sheaths (color figure online)
Determination of the number and ratio of positive cells in rat spleens by immunohistochemical staining. The number of CD3+ (a), CD4+ (b), and CD8+ (c) cells per unit area in the spleen was counted by using the IPP6.0 image analysis software, and the ratio of CD4+/CD8+ cells (d) was also analyzed. One asterisk indicates a significant difference (P < 0.05) and two asterisks indicate an extremely significant difference (P < 0.01) in the column
Effect of Boron on Splenic Lymphocyte Proliferation and Apoptosis in Rats
In this study, the immunohistochemical staining of PCNA and caspase-3 were used to determine the proliferation and apoptosis of splenic lymphocytes (Figs. 7 and 8). Results showed that the nuclei of PCNA+ cells were stained blackish brown (Fig. 7), and the cytoplasm of caspase-3+ cells were stained yellowish brown (Fig. 8). These two types of cells were distributed at various levels among the white and red pulps of the spleen. As the concentration of boron supplement increased, the number of PCNA+ cells were first increased then decreased, whereas it was the reverse for caspase-3+ cells. Statistics on the number of positive immune cells per unit area showed that compared to the control group, the number of splenic PCNA+ cells were highly significantly increased by 68.88, 75.80, 58.33 and 57.57% (P < 0.01) in groups 1, 2, 3 and 4, respectively, and were significantly reduced by 22.18 and 17.22% (P < 0.05) in groups 5 and 7, respectively (Fig. 9a). Splenic caspase-3+ cells were highly significantly decreased by 29.14, 22.05 and 28.26% (P < 0.01) in groups 1, 2 and 3, respectively, whereas they were significantly increased by 14.49 and 31.91% (P < 0.05 or P < 0.01) in groups 5 and 6, respectively. There were no significant differences in the number of caspase-3+ cells between the other groups and the control group (Fig. 9b).
The distribution of PCNA+ cells and PCNA expression in rat spleens. The spleen tissue sections were used in immunohistochemical staining for the expression of PCNA in the spleen. The PCNA+ cells were stained as brown black. As indicated, the PCNA expression in the spleen in the NC group (a) and groups 1–7 (b–h) differed as the boron supplementation in drinking water increased. The negative control (i) of immunohistochemical staining is also shown. Bar = 50 μm. SN splenic nodule, PLS periarteriolar lymphoid sheaths (color figure online)
The distribution of caspase-3+ cells and caspase-3 expression in rat spleens. The spleen tissue sections were used in immunohistochemical staining for the expression of caspase-3 in the spleen. The caspase-3+ cells were stained as brown-black. As indicated, the caspase-3 expression in the spleen in the NC group (a) and groups 1–7 (b–h) was differed as boron supplementation in drinking water increased. The negative control (i) of immunohistochemical staining was provided. Bar = 50 μm. SN splenic nodule, PLS periarteriolar lymphoid sheaths (color figure online)
Detection of the number and PCNA+ and caspase-3+ cells in rat spleens by immunohistochemical staining. The number of PCNA+ (b) and caspase-3+ cells (b) per unit area was counted by using the IPP6.0 image analysis software in the spleen. One asterisk indicates a significant difference (P < 0.05) and two asterisks indicate an extremely significant difference (P < 0.01) in the column
Effect of Boron on the Apoptosis of Splenic CD3+ Lymphocytes in Rats
The double immunofluorescence results are shown in Fig. 10. As seen under the fluorescence microscope, the cytoplasm of splenic CD3+ and caspase-3+ cells were fluorescently red and green, respectively. Compared to the control group, the positive signal intensity for CD3 in the spleen gradually increased in groups 1, 2 and 3 while the signal intensity for caspase-3 gradually decreased in these three groups. The double positive signal intensity also gradually decreased. Compared with the control group, the signal intensities for splenic CD3 and caspase-3 gradually reduced and increased respectively in groups 4, 5 and 6, and the double positive signal intensities were significantly decreased in group 7.
The immunofluorescence staining of CD3+ and caspase-3+ cells in rat spleens. The caspase-3 expression of CD3+ cells in the spleen in the NC group (0 mg/L) and groups 2 (20 mg/L), 3 (40 mg/L), 5 (160 mg/L), 6 (320 mg/L), and 7 (640 mg/L) were analyzed by using double immunofluorescence staining. The CD3+ cells showed red fluorescence. The caspase-3+ cells showed green fluorescence. The nucleus was stained as blue fluorescence by DAPI. The CD3+ caspase-3+ was represented double positive cells. The CD3+ Caspase-3+ DAPI represented merged double positive cells and DAPI-stained nucleus. Bar = 50 μm (color figure online)
Discussion
Effect of Boron on Immune Functions in the Rat Spleen
Animal immune response can be divided into non-specific and specific immunity. Non-specific immunity is the first defense barrier against pathogens, and it mainly includes physical barriers (such as the skin, mucosa, blood brain barrier, and placental barrier), innate immune cells (such as monocytes, macrophages, leukocytes, and dendritic cells), and innate immune molecules (such as complement and lysozyme) [23]. Specific immunity is acquired after birth and as the second defense barrier against the infection by pathogenic microbes, and it is mainly composed of T lymphocytes, B lymphocytes and cytokines [24]. Many studies have found that nutrition plays an important role in the maintenance of immune cell activity, as well as both the non-specific and specific immune responses [25]. There is growing evidence revealing that certain kinds of micronutrients could regulate and enhance immune functions [26]. For example, in humans, the recommended selenium intake is 55-400 μg/day for adults; supplementation of 200 μg/day selenium for 8 weeks enhances the activity of NK, promotes the secretion of cytokines by T lymphocytes, and improves both the specific and non-specific immune functions. Selenium deficiency can reduce the concentration of immunoglobulin and hence weaken immune functions [27–29]. Zinc is an essential trace element for the proliferation and differentiation of lymphocytes (12-15 mg Zn/day for humans), enhances macrophage and NK cell activity (58 mg Zn/kg in the diet, for BALB/c mice), promotes antibody production (75 mg Zn/kg in the diet for beef heifers), and induces the T-helper type 1 (Th1) response (30 or 60 μM/L Zn for PBMC in human); it also helps to maintain the integrity of the skin and mucosa [30–33]. Recent studies have shown that boron is also an essential trace element for humans and animals and that it plays a critical role in the development of immune organs and efficiency of the immune function. Boron deficiency could result in immune dysfunction, while proper boron supplementation could promote the development and affect the structures and anti-oxidative functions of immune organs [34]. At the same time, proper boron supplementation could enhance immune function, for example, supplementation of 2.5 mg/day can significantly increase white blood cell numbers and the percentage of polymorphonuclear leukocytes in women [14], supplementation of 1.75 mg boron/kg for 44 days can significantly increase IgM and IgG levels in rats injected with the human typhoid vaccine [15], and supplementation of 2.0 mg boron/kg increases the number of circulatory NK cells and CD8+/CD4− lymphocytes in rats after injection of M ycobacterium butyricum [16]. The addition of 25 μmol/L boric acid can significantly decreased LPS-induced TNF-α secretion and mRNA expression of THP-1 cells [17]. However, an excess of boron has damaging and toxic effects on the development and function of immune organs [21]. According previous studies, the minimum nutritional requirements of boron for a human is 0.25–0.35 mg B/day [35]; the World Health Organization (WHO) considers an acceptable range of intake for total boron of 1–13 mg B/day for adult human [36], while acceptable daily intake (ADI) of boron is 18 mg B/day (0.3 mg B/kg/day) for 60-kg women or 70-kg men [37]. However, following previous studies, the minimum nutritional requirement of boron for rat is no more than 0.3 mg B/kg/day, and the no observed adverse effect level (NOAEL) of boron for developmental toxicity and reproductive toxicity in rat are 9.6 and 26 mg B/kg/day, respectively [38, 39]. Those studies showed that the nutritional requirements and NOAEL of boron for different species have obvious difference. In our studies, the intake of boron is 1.5, 3.0 and 6.0 mg B/kg in the rat of 10, 20 and 40 mg B/L, respectively, which has exceeded minimum nutritional requirements but has not reached the level of NOAEL in rat. However, the intake of boron are 48 and 96 mg B/kg in the rat of 320 and 640 mg B/L have greatly exceeded level of NOAEL. So, in our study, the supplementation of boron in rats was included the proper dosage and toxic dosage, which indicated that the boron could possibly have beneficial effects or toxic effects on immune function in rats.
The specific immune responses in animals include humoral immunity and cellular immunity. Humoral immunity is mediated mostly by the production of antibodies from B cells, and cellular immunity is mediated by T cells and the cytokines they secrete [40]. Fry et al. [41] found that the supplementation of 5 and 50 mg/kg boron in diets could increase the cattle anti-pig erythrocyte IgG titers but had no effect on the anti-pig erythrocyte IgM titers. The current study demonstrated that the supplementation of 20 and 40 mg/L boron in rat drinking water increased serum IgG levels and the number of splenic CD3+ T cells in varying degrees. The supplementation of 320 and 640 mg/L boron had a reverse effect, indicating that appropriate boron supplementation can markedly enhance humoral and cellular immune functions, and high doses of boron have inhibitory or even toxic effects. T cells can be categorized into helper T cells (CD4+ T cells), cytotoxic T cells (CD8+ T cells), effector T cells, suppressor T cells, memory T cells, and delayed-type hypersensitive (DTH) T cells [42]. The CD4+ T cell and CD8+ T cell are both important T cell subset in the immune system, CD4+ T cells can help and enhance the cellular immune function, and CD8+ T cells can kill target cells labeled with specific antigens [43]. Therefore, the ratio of CD4+/CD8+ T cell is an important indicator of the cellular immune function and the change in the number of CD4+ T cell and CD8+ T cell [44]. Within normal limits (1.4–2.0, human), the increase of CD4+/CD8+ T cell ratio shows that the number of CD4 cells increased and the number of CD8 cells decreased, which indicate that the cellular immune function is enhanced; the decrease of CD4+/CD8+ T cell ratio shows that the number of CD4 cells decreased and the number of CD8 cells increased, which indicate that the cellular immune function is weakened. However, when the ratio of CD4+/CD8+ T cell exceed the normal range (<1.4 or >2.0), it indicates that the cellular immune function disorder. The ratio of CD4+/CD8+ T cell less than 1.4 is mainly present in immune deficiency disease (HIV), malignant tumor, leukemia, and some viral infections; the ratio of CD4+/CD8+ T cell more than 2.0 is mainly present in autoimmune disease. In our study, the increase of splenic CD4+/CD8+ T cell ratio in 20 and 40 mg B/L in the normal range, which indicates enhancement of cellular immune function in rats and then improve the ability of the body to resist virus infection. Based on the different types of cytokines they secrete, CD4+ T cells are divided into Th1 and Th2 subsets. Th1 cells mainly secrete IL-2, IFN-γ and TNF-β, which help with the production of antibodies involved in cellular immunity and DTH responses. Th2 cells mainly secrete IL-4, IL-6 and IL-10 which can stimulate the proliferation of B cells and the secretion of antibodies to participate in humoral immunity [45]. Changes in the secretion and concentration of Th1 and Th2 cytokines directly influence the immune functions of CD4+ T cells. Several studies have found that inadequate intake of trace elements can have significant impact on cellular immune functions. Zinc deficiency can reduce CD4+ T cells and increase CD8+ T cells, which in turn suppress the synthesis and secretion of IL-2, and supplementation of zinc can promote the expressions of IL-2 and IFN-γ [46–48]. In the present study, addition of 20 and 40 mg/L boron in drinking water could significantly increase the number of splenic CD4+ T cells and promote the secretions and expressions of IL-2 IFN-γ, and IL-4. The reverse effects were observed in addition of 320 and 640 mg/L boron. Our results showed a U-shaped response characteristic of rat immune function response to low and high boron concentrations, which was consistency with prior research [49, 50] and also indicated that appropriate boron supplementation can enhance specific immune functions by influencing the ratio of T lymphocyte subsets and the secretion of associated cytokines.
Effect of Boron on Splenic Lymphocyte Proliferation and Apoptosis in Rats
In the immune system, proliferation and apoptosis of lymphocytes affect the maintenance of the number and ratio of various lymphocyte subsets as well as the general function of the immune system. PCNA is a type of non-histone nucleoprotein which is specifically expressed during the S phase of proliferating cells. It is involved in many cellular events, such as being a cell cycle regulatory protein or a DNA polymerase δ accessory protein that participates in cellular damage repair, cell cycle regulation, and chromosome recombination [51]. The level of PCNA expression is an indicator of a cell’s proliferative state [52, 53]. Caspase-3, as one of the most important members of the caspase family, is responsible for the enzymatic cleavage of all or a part of the key proteins which leads to the completion of the apoptotic program during apoptosis. Therefore, it is an enzyme marker for the occurrence of cellular apoptosis [54]. Results from the current study found that boron plays an important regulatory role in the proliferation and apoptosis of lymphocytes. Previous studies have shown that appropriate selenium supplementation can promote T cell proliferation in vivo (50–400 ng Se/ml for bovine PBMC) and in vitro (2 mg Se/kg diet for C57BL/6J mice), whereas selenium deficiency can cause abnormal (nitric oxide) NO metabolism, thus inducing an increase in splenic lymphocyte apoptosis [55–57]. Proper zinc supplementation can enhance the proliferation of cattle lymphocytes in vitro (80 mg Zn/kg in the diet of pregnant Sahiwal cows), increase the activity of superoxide dismutase, and reduce the inhibitory effect of lead on lymphocyte proliferation. Zinc deficiency, on the other hand, can suppress T cell proliferation and induce the apoptosis of Th2 cells [58]. The present study showed that the addition of 20 and 40 mg/L boron in rat drinking water could significantly increase the number of splenic PCNA+ cells, decrease caspase-3+ cells, and reduce the expression of caspase-3 in CD3+ T cells. Whereas the supplementation of 640 mg/L boron markedly lowered the number of splenic PCNA+ cells, the supplementation of 160 and 320 mg/L boron significantly increased the number of splenic caspase-3+ cells. The previous results indicated that appropriate boron supplementation could promote lymphocyte proliferation and inhibit apoptosis, while high doses of boron could inhibit lymphocyte proliferation and promote apoptosis. Furthermore, an interesting observation in the present study showed that the supplementation of 640 mg/L boron in drinking water not only slightly reduced the number of splenic caspase-3+ cells but it also inhibited the expression of caspase-3 in splenic CD3+ cells. The reason might be that excessive boron supplementation caused structural damages in the rat spleens, which subsequently led to the reduction of splenic T cells and other immune cells. The effect of boron on the immune system might be a new strategy to improve animal and human immune response. The current study indicated that the proper concentration of boron improved immune function, and high-level boron had a toxic effect on the immune system in vivo. However, how the boron dose modulates the number of CD3+, CD4+, PCNA+ cells and the exact mechanisms and signaling pathways related to these effects is not yet fully understood. Therefore, further studies, including more in vivo experiments are needed to shed more knowledge on these mechanisms and pathways involved in these effects of boron.
Conclusions
In conclusion, supplementation of 20 and 40 mg/L boron in rat drinking water increased the level of serum IgG; hemoglobin concentration; the number of leukocytes, erythrocytes, lymphocytes, and monocytes; induced an increase in splenic CD3+ T cells; and enhanced non-specific and specific immune responses. It also increased the number of splenic CD4+ T cells and the CD4+/CD8+ T cell ratio, promoting the synthesis and secretion of IL-2, IFN-γ and IL-4 in the spleen, and thus enhancing cellular immune functions. In contrast, the supplementation of 160–640 mg/L boron reduced the non-specific and specific immune responses to varying degrees and decreased cellular immune functions. The regulation of boron on the immune functions in the spleen was mainly achieved through its influence on splenic lymphocyte subsets, secretion of associated cytokines, and the proliferation and apoptosis of these lymphocytes.
Abbreviations
- SPF:
-
Specific pathogen free
- IHC:
-
immunohistochemistry
- WBC:
-
Leukocytes
- RBC:
-
Erythrocytes
- HGB:
-
Hemoglobin
- NEUT:
-
Neutrophils
- LYM:
-
Lymphocytes
- EOS:
-
Eosinophils
- BSA:
-
Basophils
- MON:
-
Monocytes
- H:
-
Hour
- Min:
-
Minute
- PCNA:
-
Proliferating cell nuclear antigen
- DAB:
-
3,3′-Diaminobenzidine
- Th1 cell:
-
T-helper type 1 cell
- NK cell:
-
Natural killer cell
- DTH:
-
Delayed-type hypersensitive
References
Price C, Strong P, Marr M, Myers C, Murray F (1996) Developmental toxicity NOAEL and postnatal recovery in rats fed boric acid during gestation. Toxicol Sci 32:179–193
Eckhert C, Rowe R (1999) Embryonic dysplasia and adult retinal dystrophy in boron-deficient zebrafish. J Trace Elem Exp Med 12:213–219
Fort D, Stover E, Strong P, Murray F, Keen C (1998) Chronic feeding of a low boron diet adversely affects reproduction and development in Xenopus laevis. J Nutr 129:2055–2060
Lanoue L, Strong P, Keen C (1999) Adverse effect of a low boron environment on the preimplantation development of mouse embryos in vitro. J Trace Elem Exp Med 12:235–250
Hunt C (2003) Dietary boron: an overview of the evidence for its role in immune function. J Trace Elem Exp Med 16:291–306
Neilsen F (2000) The emergence of boron as nutritionally important throughout the life cycle. Nutrition 16:512–514
Rowe R, Eckhert D (1999) Boron is required for zebrafish embryogenesis. J Exp Biol 202:1649–1654
Xu P, Hu W, Guo X, Zhang Y, Li Y et al (2006) Therapeutic effect of dietary boron supplement on retinoic acid-induced osteoporosis in rats [in Chinese]. Nan Fang Yi Ke Da Xue Xue Bao 26:1785–1788
Armstrong T, Spears J, Crenshaw T, Nielsen F (2000) Boron supplementation of a semipurified diet for weanling pigs improves feed efficiency and bone strength characteristics and alters plasma lipid metabolites. J Nutr 130:2575–2581
Mızrak C, Yenice E, Can M, Yıldırım U, Atik Z (2010) Effects of dietary boron on performance, egg production, egg quality and some bone parameters in layer hens. S Afr J Anim Sci 40:257–264
Armstrong T, Spears J, Lloyd K (2001) Inflammatory response, growth, and thyroid hormone concentrations are affected by long-term boron supplementation in gilts. J Anim Sci 79:1549–1556
Bakken N, Hunt C (2003) Dietary boron decreases peak pancreatic in situ insulin release in chicks and plasma insulin concentrations in rats regardless of vitamin D or magnesium status. J Nutr 133:3577–3583
Turkez H, Geyikoglu F (2010) Boric acid a potential chemoprotective agent against aflatoxin b1 toxicity in human blood. Cytotechnology 62:157–165
Nielsen F, Penland J (1999) Boron supplementation of perimenopausal women affects boron metabolism and indices associated with macromineral metabolism, hormonal status and immune function. J Trace Elem Exp Med 12:251–261
Bai Y, Hunt C, Newman S (1997) Dietary boron increases serum antibody (IgG and IgM) concentrations in rats immunized with human typhoid vaccine. Proc North Dakota Acad Sci 51:181
Hunt C, Idso J (1999) Dietary boron as a physiological regulator of the normal inflammatory response: a review and current research progress. J Trace Elem Exp Med 12:221–233
Cao J, Jiang L, Zhang X, Yao X, Geng C, Xue X, Zhong L (2008) Boric acid inhibits LPS-induced TNF-alpha formation through a thiol-dependent mechanism in THP-1 cells. J Trace Elem Med Biol 22:189–195
Ku W, Shih L, Chapin R (1993) The effects of boric acid (BA) on testicular cells in culture. Reprod Toxicol 7:321–331
Price C, Marr M, Myers C, Seely J, Heindel J et al. (1996) The developmental toxicity of boric acid in rabbits. Fundam Appl Toxicol 34:176–187
Bakirdere S, Orenay S, Korkmaz M (2010) Effect of Boron on Human Health. The Open Mineral Processing Journal 3:54–59
Jin E, Gu Y, Wang J, Jin G, Li S (2014) Effect of supplementation of drinking water with different levels of boron on performance and immune organ parameters of broilers. Ital J Anim Sci 13:206–214
Li J, Wang Z X, Shi D Z, Chen Y X (2010) Adult exposure to sasanguasaponin induces spermatogenic cell apoptosis in vivo through increased oxidative stress in male mice. Toxicol Ind Health 26:691–700
Medzhitov R, Janeway C (1997) Innate Immunity: The Virtues of a Nonclonal System of Recognition. Cell 91:295-298
Calder P (2006) Branched-chain amino acid and immunity. J Nutr 136:288S-293S
Calder P, Jackson A (2000) Under-nutrition, infection and immune function. Nutr Res Rev 13:3–29
Maggini S, Wintergerst E, Beveridge S, Hornig D (2007) Selected vitamins and trace elements support immune function by strengthening epithelial barriers and cellular and humoral immune responses. Brit J Nutr 98:S29–S35
Ryan-Harshman M, Aldoori W (2005) The relevance of selenium to immunity, cancer, and infectious/inflammatory diseases. Can J Diet Pract Res 66:98–102
Kiremidjian-Schumacher L, Roy M, Wishe H I, Stotzky G (1994) Supplementation with selenium and human immune cell functions. II. Effect on cytotoxic lymphocytes and natural killer cells. Biol Trace Elem Res 41:115–127
Arthur J, McKenzie R, Beckett G (2003) Selenium in the immune system. J Nutr 133:1457S–59S
Sandstead H H (1993) Zinc requirements, the recommended dietary allowance and the reference dose. Scand J Work Environ Health 19:128–131
Pang Z, Wang Y M, Zheng J (1992) Effects of zinc depletion and repletion on natural killer cell activity in aged mic. Asia Pac J Clin Nutr 1:95–100
Salyer G B, Galyean M L, Defoor P J, Nunnery G A, Parsons C H, Rivera J D (2004) Effects of copper and zinc source on performance and humoral immune response of newly received, lightweight beef heifers. J Anim Sci 82:2467–2473
Metz C H, Schröder A K, Overbeck S, Kahmann L, Plümäkers B, Rink L (2007) T-helper type 1 cytokine release is enhanced by in vitro zinc supplementation due to increased natural killer cells. Nutr 23:157–163
Hu Q, Li S, Qiao E, Tang Z, Jin E, et al (2014) Effects of Boron on Structure and Antioxidative Activities of Spleen in Rats. Biol Trace Elem Res 158:73–80
Nielsen FH (1998) Ultratrace elements in nutrition: Current knowledge and speculation. J Trace Elem Exp Med 11:251–274
Meccham S, Karakas S, Wallace A, Altum F (2010) Boron in human health: Evidence for dietary recommendations and public policies. Open Miner Process J 3:36–53
Qin JF (1998) Biological Essentiality of Boron and Its Health Effects in Humans. Guangdong Weiliang Yuansu Kexue (In Chinese) 6:1–14
Murray FJ (1995) A human health risk assessment of boron (boric acid and borax) in drinking water. Regul Toxicol Pharmacol 22:221–230
Ku WW, Chapin RE, Wine RN, Gladen BC (1993) Testicular toxicity of boric acid (BA): relationship of dose to lesion development and recovery in the F344 rat. Reprod Toxicol 7:305–319
Li P, Yin Y, Li D, Kim S, Wu G (2007) Amino acids and immune function. Brit J Nutr 98:237–252
Fry R, Lloyd K, Jacobi S, Siciliano P, Robarge W, et al (2010) Effect of dietary boron on immune function in growing beef steers. J Anim Physiol An N 94:273–279
Winter H, van den Engel N, Rüttinger D, Schmidt J, Schiller M, Poehlein C (2007) Therapeutic T cells induce tumor-directed chemotaxis of innate immune cells through tumor-specific secretion of chemokines and stimulation of B16 BL6 melanoma to secrete chemokines. J Transl Med 5:1–14
Murphy K, Reiner S (2002) The lineage decisions of helper T cells. Nat Rev Immunol 2:933–944
Chen W, Jin W, Hardegen N, Lei K, Li L, et al. Conversion of peripheral CD4 +CD25 – naïve T cells to CD4+CD25 + regulatory T cells by TGF-beta induction of transcription factor Foxp3. J Exp Med 198:1875–1886
O'Garra A, Murphy K (1994) Role of cytokines in determining T-lymphocyte function. Curr Opin Immunol 6:458–466
Berni C, Buccigrossi V, Passariello A (2011) Mechanisms of action of zinc in acute diarrhea. Curr Opin Gastroen 27:8–12
Bao B, Prasad A, Beck F, Bao G, Singh T, et al. Intracellular free zinc up-regulates IFN-γ and T-bet essential for Th1 differentiation in Con-A stimulated HUT-78 cells. Biochem Bioph Res Co 407:703–707
Gershwin M, German J, Keen C (2000) Nutrition and Immunology: Principles and Practice. Totowa: Humana Press
Rowe R I, Bouzan C, Nabili S, Eckhert C D (1998) The response of trout and zebrafish embryos to low and high boron concentrations is U-shaped. Biol Trace Elem Res 66:261–270
Fort D J, Rogers R L, McLaughlin D W, Sellers C M, Schlehat C L (2002) Impact of boron deficiency on Xenopus laevis. Biol Trace Elem Res 90:117–142
Moldovan G, Pfander B, Jentsch S (2007) PCNA, the Maestro of the Replication Fork. Cell 129:655–679
Uni C, Platin R, Sklan D (1998) Cell proliferation in chicken intestinal epithelium occurs both in the crypt and along the villus. J Comp Physiol B 168:241–248
Villar-Cheda B, Pérez-Costas E, Meléndez-Ferro M, Abalo X, Rodriguez-Muñoz R, et al. Proliferating cell nuclear antigen (PCNA) immunoreactivity and development of the pineal complex and habenula of the sea lamprey. Brain Res Bull 57:285–287
Skulachev V (1998) Cytochrome c in the apoptotic and antioxidant cascades. FEBS Lett 423:275-580
Stabel J, Nonnecke B, Reinhardt T (1990) Effect of in vitro selenium repletion on bovine lymphocyte proliferation. Nutr Res 10:1053–1059
Kiremidjian-Schumacher L, Roy M, Wishe H, Cohen M, Stotzky G (1990) Selenium and immune cell functions. I. Effect on lymphocyte proliferation and production of interleukin 1 and interleukin 2. Exp Bio Med 193:136–142
Wang Q, Lv Z, Li J, Li S, Xu S (2009) Effects of NO on splenic lymphocyte apoptosis induced by selenium deficiency in chickens. Chinese Journal of Animal Nutrition 21:454–461
Dang A, Prasad S, De K, Pal S, Mukherjee J, et al. Effect of supplementation of vitamin E, copper and zinc on the in vitro phagocytic activity and lymphocyte proliferation index of peripartum Sahiwal (Bos indicus) cows. J Anim Physiol An N 97:315–321
Acknowledgements
We are grateful to Shengnan Liu and Xia Li for detection the expressions of CD3, CD4, CD8, proliferating cell nuclear antigen (PCNA) and apoptosis protein (caspase-3) in splenic T cells. We also want to thank Xiaomei Wu and Han Xu for the detection of peripheral blood cells and serum immunoglobulins. This study was supported by the National Natural Science Foundation of China (31402154, 31502137, 31672502); grants from the Project Funded by China Postdoctoral Science Foundation (2014T70151); the Major National Science Research Program (973 Program) (2015CB943100); the Natural Science Project of Education Department in Anhui Province (KJ2014ZD09; KJ2014A055); the Key Discipline Construction Program of Anhui Science and Technology University, China (AKZDXK2015A04); and the Talents Special Foundation of Anhui Science and Technology University, China (ZRC2013354).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This article does not contain any studies with human or animal subjects performed by any of the authors. Ethics Committee approval was obtained from the Institutional Ethics Committee of Anhui Science and Technology University for the study in manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Erhui Jin and Shenghe Li contributed to this work equally.
Rights and permissions
About this article
Cite this article
Jin, E., Li, S., Ren, M. et al. Boron Affects Immune Function Through Modulation of Splenic T Lymphocyte Subsets, Cytokine Secretion, and Lymphocyte Proliferation and Apoptosis in Rats. Biol Trace Elem Res 178, 261–275 (2017). https://doi.org/10.1007/s12011-017-0932-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-017-0932-3