Abstract
This study aimed to compare the effect of excess iodine and herbs with excess iodine on treating iodine deficiency-induced goiter from the perspective of oxidative stress and to measure selenium values in Chinese herbs. One hundred twenty 4-week-old Wistar rats were selected and randomly divided into four groups after inducing iodine-deficiency goiter: normal control group (NC), model control group (MC), iodine excess group (IE), and herbs with iodine excess group (HIE). The activities of oxidative enzymes and levels of oxidative products were measured using biochemical tests. The expression of 4-hydroxynonenal (4-HNE) in the thyroid was detected by immunohistochemistry and the expression of peroxiredoxin 5 (PRDX5) by the Western blot and immunohistochemistry. Selenium values in iodine-excessive herbs were measured by hydride generation-atomic fluorescence spectrometry. The herbs with iodine excess were tested to contain rich selenium. The activities of superoxide dismutase (SOD) and PRDX5 increased markedly, and the values of malondialdehyde (MDA) and 4-HNE decreased significantly in the HIE group. In conclusion, compared with excess iodine, herbs with excess iodine damaged thyroid follicular cells less, which may be related to the increase of antioxidant capacity and rich selenium values in iodine-excessive herbs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
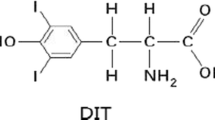
Excessive iodine intake cannot make iodine deficiency-induced goiter recover completely. Moreover, iodine overdose is harmful to iodine-deficient individuals [1]. At the same level of iodine excess, iodine-rich herb compound recipes are distinctly better than simple excessive iodine, and no obvious injuries could be seen on the thyroid [2]. However, comparative studies on the therapeutic mechanisms of excessive iodine and iodine-rich herbs on iodine deficiency-induced goiter have not yet been reported. Oxidative stress is one of the main mechanisms to cause thyroid impairment in iodine-deficient individuals through iodine overdose [3]. The unsaturated fatty acids of thyroid follicular epithelial cell membranes are susceptible to be injured by oxidative stress to cause lipid peroxidation [4] and will produce overabundant aldehyde metabolites, such as 4-hydroxynonenal (4-HNE), to damage cellular structures and cause protein degeneration through cross-linking and DNA damage. PRDX5 may reduce H2O2 to water and regulate intracellular lipid peroxide levels, so they can accurately reflect the level of oxidative stress in the thyroid [5,6]. Selenium was proven to be one of the trace elements closely related to human health by Schwarz in 1957, which functions in many ways physiologically, especially through its antioxidative action. Selenium is usually richly stored in the thyroid. Since the co-deficiency of iodine and selenium leads to goiter, supplementation of both iodine and selenium works better for goiter treatment than mono-supplementation of iodine. Here, we test our hypothesis that iodine-rich herbs would be more effective in treating goiter than excess iodine alone in a rat model of iodine-deficient goiter.
Materials and Methods
Experimental Materials
-
1.
Animals and diet: All experimental protocols were approved by the ethics committee of Liaoning University of Traditional Chinese Medicine (TCM), and all procedures were performed in accordance with the ethical standards. Wistar rats of 4 weeks old were provided by the Experimental Animal Center of China Medical University, with animal license number SCXK Beijing 2009-0004. Iodine-deficient diet, whose iodine content was 20 μg/kg, was made of maize, millet, and beans (73:20:7) from severe iodine-deficient areas (Daliangjianfang Village, Longhua County, Chengde City, Hebei Province, China) and appropriate amount of additives.
-
2.
Drugs: Decoction of iodine-rich herbs—seaweed 15 g, kelp 15 g, and tangle 7.5 g—with iodine content of 1,900.36 μg/L [7] was prepared by the manufacturing laboratory of The Affiliated Hospital of Liaoning University of TCM. The seaweed, kelp, and tangle, of 105 g each were offered by the Pharmacy of the Affiliated Hospital of Liaoning University of TCM. High iodine water, prepared by potassium iodate and deionized water, has iodine content of 1,900 g/L.
-
3.
Main reagents and instruments: Superoxide dismutase (SOD) kit, xanthine oxidase (XOD kit), glutathione peroxidase (GSH-Px) kit, H2O2 kit, malondialdehyde (MDA) kit (Nanjing Jiancheng Bioengineering Institute, China), polyclonal antibodies of goat anti-mouse 4-HNE and polyclonal antibodies of rabbit anti-rat PRDX5 (Santa Cruz, USA), instant SABC Peroxidase kit (Boster, Wuhan, China), and IgG antibody of alkaline phosphatase kit (Beijing Zhongshan Biotech Limited Company, China) were used. Nitric acid, perchloric acid, hydrochloric acid, sodium hydroxide, sodium borohydride, potassium ferricyanide, and standard selenium liquid were from Hongrui Chemical Co. Ltd. (Shanghai, China). T6 new century spectrophotometer (Beijing Persee, China), UV spectrophotometer (UV-visible Spectrometer, UV300, Germany), electrophoresis apparatus (Bio-Rad, PowerPac200), vertical panel electrophoresis equipment (Bio-Rad, Mini-Protein III), DYY-40B transfer electrophoresis tanks (Beijing Liuyi Instrument Factory, China), and high-speed refrigerated centrifuge (Sigma-31k 5C, USA) were used. Atomic fluorescence spectrophotometer was from Kechuang Haiguang Instrument Co., Ltd. (Beijing, China), and electric hot plate and automatic temperature control digestion furnace were from Troody Technology (Shanghai, China).
Experimental Method
-
1.
Modeling, grouping, and treatment factors: After being fed with the standard diet for a week, in all 120 rats, 30 rats were randomly selected as the NC group, which were then fed with a standard diet and double-distilled water during the whole course. The remaining 90 rats were fed with a low-iodine diet, along with 1 % sodium perchlorate, containing double-distilled water for 19 days, followed by double-distilled water for 2 days (3 weeks in total), to produce iodine deficiency-induced goiter rats. Then, they were randomly divided into three groups, namely model control (MC) group, iodine excess (IE) group, and herbs with iodine excess (HIE) group, all of which were fed with a low-iodine diet. The MC group were fed with double-distilled water every day, the IE group were fed with high iodine water every day, and the HIE group were fed with concentrated iodine-rich decoction, and the dosage administered was calculated by human body surface area, for which the crude drug should be 4.7 g/kg per day. At 0 and 8 weeks after modeling, 15 rats were killed at each time point. The thyroid glands of two rats were observed by an electron microscope, eight by HE staining and immunohistochemistry, and five by Western blot.
-
2.
Specimen collection: The urine samples were collected and stored in a −20 °C freezer after the rats were kept in metabolic cages for a 24-h fast. They were euthanatized after receiving 20 % urethane as intraperitoneal anesthesia and were weighed. Blood samples were obtained from the abdominal aorta, and serum was separated by centrifugation at 3,000 rpm/min and kept at −20 °C until analysis. Wet weight of the thyroid gland was weighed by electronic scales instantly after separation from the body and fixed instantly by 4 % paraformaldehyde for quantitative morphological and immunohistochemical detection. The thyroid specimens for transmission electron microscopy were fixed with 2.5 % glutaraldehyde within 30 s from separation. The thyroid specimens used for Western blot detection were stored instantly in liquid nitrogen at −80 °C.
-
3.
Urine iodine was analyzed by arsenic cerium catalysis spectrophotometry (Standards of the People’s Republic of China on Health Industry).
-
4.
Thyroid function and thyroid relative weight: Serum thyroid-stimulating hormone (TSH) was measured by enzyme-linked immunosorbent assay (ELISA; United States Rapidbio (RB) Company). Serum totals of T3 (TT3) and T4 (TT4) were measured by radioimmunoassay method (RIA; Beijing SBRT Science Technology Development Center). The thyroid relative weight was calculated by the wet thyroid weight divided by body weight.
-
5.
Thyroid morphology: The cellular morphology of thyroid stained with routine HE was observed with an optical microscope, and the height of thyroid follicular epithelial cells and the area and volume of follicular cavities were calculated by MetaMorph Image Analysis System/Olympus (DP10)/microscopy (BX51) of UIC Corporation of USA. The ultrastructures of thyroid follicular epithelial cells were evaluated by transmission electron microscopy (Carl Zeiss, Germany).
-
6.
MDA was measured by thiobarbituric acid (TBA) assay, GSH-Px by glutathione peroxidase assay, SOD by xanthine oxidase assay, H2O2 by ammonium molybdate assay, and XOD by catalytic hypoxanthine method. Kits were provided by Nanjing Jiancheng Bioengineering Institute, and procedures were performed according to the instructions of the manufacturer.
-
7.
The expressions of 4-HNE and PRDX5 were measured by immunohistochemistry, following the instructions of instant SABC peroxidase kit of Wuhan Boster Company. Positive staining was localized in the cytoplasm and colored in brown. The results were semiquantitatively analyzed by the abovementioned MetaMorph Computer Image Analysis System to integrate optical density values to reflect the relative content of positive substances.
-
8.
The expression of PRDX5 was also analyzed by Western blot method. Thyroid samples of 100 mg were mixed with 500-μL ice-cold cell lysis solution, and tissue blocks were cut up followed by ultrasonic grinding in the ice water bath and centrifuged at 12,000 rpm for 1 h at 4 °C to obtain the supernatant. The protein concentration was measured by the phenol reagent method, and samples were adjusted with a lysis buffer to the same concentration based on the test results. Protein samples of 50 μL were taken with the supernatant separated by 10 % SDS-PAGE and plate conditions of 150 V; 30 mA of Bio-Rad electrophoresis plate were adopted for 1.5 h. Incubation with PRDX5 primary antibodies (1:400) was carried out for 2 h at room temperature and then alkaline phosphatase secondary antibodies (1:2,000) added for 2 h at room temperature. TTBS was used to wash for 5 min × 2 and TBS for 5 min × 1. An enzymatic method was used with a color-developing agent for coloration, and Scion Image Corporation analysis software was used to perform quantitative analysis of the blots.
Statistical Analysis
Urinary iodine value was represented by median urinary iodine (MUI) and the rest by x ± s. T test was used for comparison of two sample means, while variance analysis was used for comparison of more than two samples. P < 0.05 was considered to be statistically significant. All data were put in an Excel spreadsheet and statistically managed with SPSS 17.0 package.
Results
-
1.
The MUI of each group are shown in Table 1.
Table 1 Rat MUI in different groups (micrograms per liter) -
2.
The function and relative weight of the thyroid in each group are given in Table 2.
Table 2 Effect of different treatments on thyroid function and relative thyroid weight in iodine-deficient rats (x ± s) -
3.
The thyroid morphology and quantitative observation under an optical microscope are depicted in Fig. 1.
-
4.
Transmission electron microscopy
The microvilli on the surface of the follicular epithelial cells in the MC group were rare, and the shape of the nuclei was irregular. A part of the nuclear membrane gap was enlarged. The intracytoplasmic rough endoplasmic reticulums were dilated into pools or large bubble-like shapes. A small part of mitochondrial cristae was reduced. The microvilli on the surface of the follicular epithelial cells in the IE group were less with the irregular shape of the nuclei, and the intranuclear heterochromatin was gathered to the edge. The intracytoplasmic rough endoplasmic reticulums were dilated to a bubble-like shape. Parts of the mitochondrial cristae were reduced, and the myeloid body was turned up. There were more lysosomes close to the membrane surface. The number of microvilli on the surface of the follicular epithelial cells in the HIE group increased, and the shapes of the nuclei were irregular. The intranuclear heterochromatin was gathered to the edge. There were more rough endoplasmic reticulums dilated mildly. The Golgi apparatus was in a minor expansion. The mitochondrial cristae were slightly reduced (see Fig. 2).
-
5.
A comparison of serum SOD, GSH-Px, the XOD activity and contents of H2O2, and MDA can be seen in Table. 3.
Table 3 Effect of different treatments on serum SOD activity (units per liter) and GSH-Px activity (units), H2O2 content (millimoles per liter), MDA content (millimoles per milliliter) and XOD activity (units per liter) in iodine-deficient rats (x ± s) -
6.
A comparison of the expression of 4-HNE in the thyroid by immunohistochemical assay can be seen in Table 4 and Fig. 3.
Table 4 Effect of different treatments on thyroid 4-HNE and PRDX5-positive rate (x ± s) in iodine-deficient rats -
7.
A comparison of the expression of 4-HNE in the thyroid by immunohistochemistry is shown in Table 4 and Fig. 4.
-
8.
A comparison of the expression of 4-HNE in the thyroid by Western blot is shown in Fig. 5.
-
9.
Selenium values in herbs can be seen in Table 5.
Table 5 Selenium values in herbs
Discussion
Iodine supplementation is the most effective treatment for iodine deficiency-induced goiter, but excessive iodine intake for iodine-deficient individuals leads to not only iodine-induced hyperthyroidism (IIH) and autoimmune thyroid diseases (AITD), but also to high iodine-induced goiter [8]. After epidemiological investigations for water iodine, urinary iodine, and goiter rate, Zhiheng et al. revealed that there was a “u”-shaped curve relationship about drinking water iodine, urinary iodine, and goiter rate, i.e., the lower the water iodine or urinary iodine, the easier to cause iodine deficiency-induced goiter; and the higher the water iodine or urinary iodine, the easier to cause excess iodine-induced goiter. Animal experiments also indicated that MUI > 300 μg/L might have a toxic effect on iodine-deficient goiter, and injuries tended to be more severe as the amount and duration of iodine intake increased, so excessive iodine supplement could not completely restore iodine deficiency-induced goiter [1,9]. Many et al. [10] revealed that rats with hyperplastic goiter induced by iodine deficiency, which were fed with a diet of normal iodine concentration, might subsequently experience necrosis of the thyroid epithelial cell, while those fed with a high-iodine diet might show more serious damage. The mechanism was related to oxidative stress. Excess iodine may promote oxygen free radicals to reduce the antioxidant defense capability. I2 itself is a highly active molecule which can react with proteins, lipids, and nucleic acids to generate a variety of aliphatic iodocompounds accompanied by reactive oxygen species generation and lipid peroxidation in the process, resulting in the damage to the structure of the cell membrane and mitochondrial membrane [11].
This study shows that the damage to the thyroid was visible under light microscopy and electron microscopy following excessive iodine supplement for iodine-deficient rats, and the goiter recovered incompletely. Serum H2O2 content and XOD activity in rats increased significantly with more free radicals and MDA, lipid peroxidation product, as well as more serious oxidative stress impairment; serum SOD activity and GSH-Px activity reduction was the manifestation of the decrease in anti-oxidizing capability. And we also found that the expression of 4-HNE in the thyroid increased, and expression of PRDX5 was reduced, which suggested that the antioxidant defense capacity was distinctly reduced, and oxidative stress impairment increased markedly after receiving excessive iodine supplement for iodine-deficient rats.
The iodine-rich herbs can make the iodine-deficient goiter recover well. In the HIE group, although the serum XOD value increased, the serum content of H2O2, MDA, and expression of 4-HNE in the thyroid lowered significantly; the serum GSH-Px activity decreased significantly, and the expression of PRDX5 in the thyroid increased markedly compared with those of the IE group. The thyroid follicular epithelial cell impairment was mild because of the reduced generation of oxygen radicals in the rats’ body and thyroids and the strengthened antioxidant defense capability. Treatment with iodine-rich herbs of iodine deficiency-induced goiter has a long history in Chinese medicine. Over ten prescriptions for the treatment of iodine deficiency-induced goiter in the book Important Prescriptions Worth a Thousand Gold, written by Sun Si-miao, Tang Dynasty, contained iodine-rich herbs, in which seaweed and kelp were the most frequently used herbs, and no thyroid impairment had been reported. The principle of formulating prescription adopted by our study stemmed from a classical prescription, seaweed jade kettle decoction, which was the representative prescription for treatment of iodine deficiency-induced goiter documented in the book Orthodox Manual of External Medicine, written by Chen Shi-gong, Ming Dynasty. In this decoction, seaweed is the monarch medicine, and kelp and seaweed are the minister medicine.
The selenium value in grain from a low selenium field is 0.006 mg/kg in China, which is a thousand times lower than that from a high selenium field (4–8 mg/kg). The selenium value in selenium-rich rice is 0.236 mg/kg, which is approximately four times higher than that in normal rice (0.059 mg/kg). This study shows that seaweed, tangle, and kelp contain extremely rich selenium compared with both normal rice and selenium-rich rice. The impairment in thyroids of iodine-deficient individuals caused by iodine-rich herbs was mild, which may be related to rich selenium in herbs.
Except for the liver and kidney, the thyroid contains more selenium than other organs and tissues, which means that selenium plays an important role in the thyroid. Being the main ingredient in many proteins, selenium is involved in thyroid hormone synthesis, maintaining thyroid integrity under strong oxidative stress and controlling the thyroid hormone metabolism in other tissues [12]. A certain selenium concentration is helpful to the balance of the oxidation-reduction system in the thyroid cells, preventing the thyroid cells from being impaired by oxidation. As the primary prevention system against H2O2, GSH-Px maintains the integrity of the cell membrane through clearing away peroxide, namely H2O2, lipids, and phospholipids and regulates the arachidonic acid synthesis, controlling inflammation and oxidation impairment. Duntas [13] found that selenium supplement could improve GSH-Px activity in patients with AITD, clearing away the excessive H2O2. Xu et al. [14] put forward that GSH-Px activity might be reduced in the thyroid due to excessive iodine but increased after selenium supplement. Therefore, we propose that the resistance of thyroid oxidative overstress by herbs with iodine excess may be related to their rich load of selenium. Herbs with iodine excess could be a more natural way of treating iodine-deficient goiter when compared with supplementing both iodine and selenium separately.
Both serum TT4 and TT3 values increased in the IE group, while the serum TT4 value in the HIE group increased significantly. But no marked decrease in the serum TSH value was seen in both groups, which indicated high serum thyroid hormone levels. Iodine-induced hyperthyroidism is difficult to be avoided in the process of iodine supplement, but it is generally a transient disorder, and the thyroid hormone levels will be gradually reduced to normal. In future experiments, we will extend the observation time to study on the effect of iodine-rich herbs on the long-term serum thyroid hormone status.
The MUI in iodine-rich herbs after an 8-week treatment was significantly higher than those of the IE group. That may be caused by two different forms of iodine, organic iodine in iodine-rich herbs, and inorganic iodine in potassium iodate, which may result in different absorption and metabolic processes and different renal elimination rates [15]. The relevant study has not been seen in the present literature yet. We are planning to compare the pharmacokinetics between iodine-rich herbs and inorganic iodine in vivo in the future.
Vitamin E can partly alleviate the cytotoxicity caused by excessive iodine supplement in iodine-deficient individuals, but has no effect on the recovery of goiter [16]. Compared with excessive iodine intake, iodine-excessive herbs may cause less oxidative damage to thyroid follicular cells and make iodine deficiency-induced goiter recover more completely, which may be related to the enhanced antioxidant capacity in the body and thyroid while improving iodine intake. On the grounds of our data, we might speculate that treatment with iodine-rich herbs may reduce the occurrence risk of autoimmune thyroiditis in iodine deficiency autoimmune thyroiditis-susceptible individuals.
References
Gao T-S, Teng W-P (2004) Effect of mild and moderate iodine excess on thyroid function and morphology in iodine deficiency rats. Chin J Endocrinol Metab 20:353–356
Gao T-S, Cui P, Li H-M et al (2008) A study on the effect of Seaweed Jade Kettle Decoction on thyroid function and morphology in iodine deficiency induced goiter rats. Chin J Basic Med Tradit Chin Med 14:113–116
Zhang N, Tong YJ, Shan Z-Y, Teng W-P (2006) Effect of Chronic mild and moderate iodine excess on thyroid anti-oxidative ability of iodine deficiency and non-iodine deficiency Wistar rats. Natl Med J Chin 86:1274–1278
Gobe G, Crane D (2010) Mitochondria, reactive oxygen species and cadmium in the kidney. Toxicol Letters 198(1):49–55
Milenkovic M, De Deken X et al (2007) Duox expression and related H2O2 measurement in mouse thyroid: onset in embryonic development and regulation by TSH in adult. J Endocrinol 192:615–626
Poncin S, Gerard A-C, Boucquey M et al (2008) Oxidative stress in the thyroid gland: from harmlessness to hazard depending on the iodine content. Endocrinology 149:424–433
Cui P, Gao T-S (2007) To measure the content of iodine in herbal medicine and compound prescription used in softening hard mass and disintegrating masses. Chin Arch Tradit Chin Med 25:1396–1398
Wu L, Yu JC, Kang WM, Ma ZQ (2013) Iodine nutrition and thyroid diseases. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 35(4):363–8
Gao T-S, Hu F-N, Teng W-P (2003) Effect of mild and moderate excessive iodine on thyroid function and morphology in non-iodine deficiency rats. Chin J Int Med 42:705–708
Many MC, Denef JF, Hamudi S et al (1986) Increased follicular heterogeneity in experimental colloid goiter produced by refeeding iodine excess after thyroid hyperplasia. Endocrinology 118:637–644
Denef JF, Many MC, Van den Hove MF (1996) Iodine-induced thyroid inhibition and cell necrosis: two consequences of the same free radical mediated mechanism? Mol Cel Endocrinology 121:101–103
Köhrle J (2013) Selenium and the thyroid. Curr Opin Endocrinol Diabetes Obes 20(5):441–8
Duntas LH (2006) The role of selenium in thyroid autoimmunity and cancer. Thyroid 16(5):455–460
Xu J, Yang XF, Guo HL et al (2006) Selenium supplement alleviated the toxic effects of excessive iodine in mice. Biol Trace Elem Res 111(1–3):229–238
Yun-xia J, Rong L, Guo-qing Z et al (2010) The research status and application of organic iodine. Guangdong Trace Elem Sci 17:12–15
Yu J, Shan Z, Chong W et al (2011) Vitamin E ameliorates iodine-induced cytotoxicity in thyroid. J Endocrinol 209:299–306
Acknowledgments
This work received grants from the Specialized Research Fund for the Doctoral Program of Higher Education of China (grant no. 20092133110004), Liaoning Province Education Department (grant no. 2009A492), and Talents Project of Liaoning Province Education Department (grant no. LR201026). And thanks for the support from Prof. Teng Weiping and Prof. Shan Zhongyan, Endocrinology and Metabolism Institute, China Medical University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gao, T., Shi, R., Qi, T. et al. A Comparative Study on the Effects of Excess Iodine and Herbs with Excess Iodine on Thyroid Oxidative Stress in Iodine-Deficient Rats. Biol Trace Elem Res 157, 130–137 (2014). https://doi.org/10.1007/s12011-013-9873-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-013-9873-7