Abstract
The stromal-derived factor-1 alpha (SDF-1α) and vascular endothelial growth factor (VEGF) play an important role in angiogenesis and exert a significant trophic function. SDF-1α is a chemoattractant for endothelial progenitor cells derived from bone marrow and promotes new blood vessel formation. VEGF regulates all types of vascular growth, stimulates angiogenesis, and is involved in the induction of lymphangiogenesis. The possibility of using these growth factors for regenerative medicine is currently under investigation. The angiogenic potential of a pBud-SDF-1α-VEGF165 bicistronic plasmid construct which simultaneously encodes VEGF165 and SDF-1α genes cDNA was evaluated in this study. The conditioned medium collected from HEK293T cells transfected with the pBud-SDF-1α-VEGF165 plasmid was shown to stimulate the formation of capillary-like structures by human umbilical vein-derived endothelial cells (HUVEC) on Matrigel and to increase the proliferative activity of these cells in vitro. Thus, the pBud-SDF-1α-VEGF165 plasmid exhibits angiogenic properties in cell cultures in vitro. As interest in the development of non-viral techniques for regenerative medicine increases, this plasmid which simultaneously expresses VEGF165 and SDF-1α may provide a platform for advanced methods of stimulating therapeutic angiogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiogenesis, the formation of new blood vessels through the migration and proliferation of differentiated endothelial cells from the existing network of capillaries and postcapillary venules, is being actively studied as a therapeutic approach for tissue regeneration in ischemic lesions of the heart and peripheral blood vessels, as well as the treatment of complications caused by progression of these diseases [1]. Therapeutic angiogenesis is mainly aimed to stimulate natural processes of the formation and further growth of blood vessels that provide revascularization of damaged tissues and organs [2].
Lack of oxygen is the main stimulating factor of angiogenesis under both physiological and pathological conditions. Hypoxia stimulates the secretion of most pro-angiogenic factors [3]. Pro-angiogenic factors such as vascular endothelial growth factor (VEGF) [4,5,6], fibroblast growth factor (FGF) [7, 8], and hepatocyte growth factor (HGF) [9] promote the growth of new blood vessels in vivo when administered intramuscularly or intraarterially.
Members of the VEGF family regulate all types of vascular growth, control vasculogenesis and chemotaxis of inflammatory cells, stimulate angiogenesis, are involved in the induction of lymphangiogenesis, and upregulate other pro-angiogenic factors [10]. The use of recombinant VEGF in lower limb ischemia and ischemic myocardial damage in in vivo models increases the density of a microvascular network resulting from the formation of collaterals in hypoxia-damaged tissues [11,12,13].
Members of the FGF family, such as FGF1 and FGF2, are nonspecific angiogenesis inducers which influence the development and formation of a vascular bed and its functional activity through regulatory mechanisms responsible for cell migration, proliferation, and differentiation [14]. In vivo experiments have demonstrated that recombinant FGF2 was safe and effective in the treatment of ischemic damage [15, 16]. Another angiogenesis inducer is platelet-derived growth factor (PDGF), which also supports the proliferation of fibroblasts and glial cells [17, 18].
One of the essential factors for neovascularization is stromal-derived factor-1 alpha (SDF-1α) which is involved in the activation, differentiation, and migration of immune cells, wound healing, and tissue repair [19]. SDF-1α also plays an important role in the migration, recruitment, and retention of endothelial progenitor cells (EPCs) in the area of ischemic injury [20]. SDF-1α levels rise in ischemic tissues, contributing to the formation of an SDF-1α gradient between peripheral blood and ischemiс tissue and the attraction of EPCs [21]. SDF-1α was shown to promote neovascularization in vitro and in vivo [22]. However, the clinical use of recombinant growth factors for angiogenic therapy is limited by the need to optimize administration methods, dosage, and treatment duration since recombinant proteins have a short half-life in the bloodstream [23].
The future of regenerative medicine is associated with the development of gene- and cell-based technologies [24]. Due to their unique plasticity, stem and progenitor cells can differentiate into various cell types, including vascular endothelial cells, thereby participating in a new vascular bed formation [25, 26]. Stem cells secrete various pro-angiogenic factors, such as VEGF and FGF2, which mediate paracrine effects in an ischemic lesion, resulting in the induction of angiogenesis [25, 27]. Transplantation of stem cells derived from peripheral blood or bone marrow has been shown to relieve symptoms of ischemic damage such as claudication and back pain, and also to promote wound healing in patients with ulceration [26, 28]. However, the therapeutic efficacy of stem cells may vary depending on a donor as well as their source. For example, bone marrow-derived stem cells were shown to induce blood vessel regeneration more effectively than those derived from adipose tissue [28, 29]. In addition, there are other limitations of therapeutic approaches that use stem cells to induce angiogenesis. The lack of sufficient clinical trial data proving the therapeutic efficacy of stem cells is one of them. Molecular mechanisms of inducing angiogenesis by stem cells are still unclear; most clinical trials have been non-randomized and the preferred method and regime of administration, as well as therapeutically effective amounts of cells, have not been defined. In addition, the safety of this therapeutic approach cannot be described since its long-term effects on the human body have not been evaluated [26, 30].
The use of gene and gene-cell therapy to induce angiogenesis has been one of the latest advances in regenerative medicine. Plasmid vectors and recombinant adeno- or adeno-associated viruses are usually used to deliver therapeutic genes to damaged tissues [31]. In contrast to recombinant growth factors, gene constructs act in the target tissue from one to several weeks and provide a less dramatic and longer-lasting increase in pro-angiogenic factor levels, which precludes frequent and repeated injections and body sensitization [32]. Delivery of the VEGF gene to ischemic tissues using a plasmid or adenovirus has been shown to significantly improve tissue perfusion and oxygenation and to result in neovascularization in a hind limb ischemia rodent model [33]. Long-term treatment results (at least 5 years) in patients with chronic lower limb ischemia (CLLI) showed the use of the gene-therapeutic drug “Neovasculgen” (VEGF165 gene encoding plasmid) provided a stable positive effect in the vast majority of patients with stages II and III CLLI. All the patients showed good tolerability; no side effects and complications were observed [34]. In addition, the use of “Neovasculgen” significantly reduced the manifestations of diabetic neuropathy [35].
Applying plasmid and viral vectors encoding genes of trophic factors increases the therapeutic efficacy of stem cells. More and more studies provide evidence that genetically modified stem cells with overexpression of therapeutic genes give better results in the induction of angiogenesis than native stem cells [36].
It should be noted that most studies describe the use of gene constructs encoding a single therapeutic gene. Plasmid or viral constructs that encode VEGF121 [37], FGF1 [38], HGF [39], etc. have been described. Combined gene therapy with several therapeutic genes, for example, FGF2 and Cyr61, was used in a mouse critical lower limb ischemia model [40]. The combination of therapeutic factor genes in genetic constructs is intended to improve neovascularization in damaged tissues [41], as well as providing other trophic functions depending on the transgene contained within the construct. Genetically modified HEK293 cells with a plasmid construct that encodes VEGF and bone morphogenetic protein 2 (BMP2) have been shown to exhibit pro-osteogenic and pro-angiogenic properties [42].
In the present work, we evaluate the possible therapeutic efficacy of a bicistronic plasmid construct that simultaneously encodes VEGF165 and SDF-1α gene cDNA to induce angiogenesis.
Material and Methods
Codon Optimization of SDF-1α and VEGF165 Gene cDNA and Its Cloning into a Bicistronic Plasmid Expression Vector
The GenScript’s OptimumGene™ Gene Design system (GenScript) was used to optimize the codon composition of SDF-1α and VEGF165 genes with nucleotide sequences of SDF-1α (GeneBank #AY429472.1, 270 bp) and VEGF165 (GeneBank #AF486837.1, 576 bp) mRNAs as a matrix. De novo synthesis of cDNA nucleotide sequences of SDF-1α and VEGF165 genes and their cloning into pBudCE4.1 plasmid vector (Invitrogen, USA) was performed using GenScript. A restriction analysis with the use of SacI and MluI endonucleases and sequencing was done to confirm the correct assembling of the pBud-SDF-1α-VEGF165 gene construct.
Preparation and Purification of Plasmid DNA
The pBud-SDF-1α-VEGF165 plasmid was amplified in Escherichia coli DH5a cells and isolated from the bacterial cells using the GeneJET Plasmid Midiprep Kit (Thermo Fisher Scientific Inc., USA) according to the manufacturer’s instructions. The purity of the isolated plasmid DNA (pDNA) was assessed by the ratio of its absorbance at 260 and 280 nm (A260/A280) with a NanoDrop 2000 spectrophotometer (Thermo Fisher Scientific Inc., USA). An A260/A280 ratio value of the pDNA used in this study was between 1.8 and 2.0, which confirmed its purity.
Cell Cultures
HEK293T cells were purchased from the American Type Culture Collection (ATCC Number: CRL-11268, Manassas, VA, USA).
Adipose tissue and umbilical vein samples were provided by the Republican Clinical Hospital for research purposes in compliance with ethical standards and in accordance with the current legislation. The protocol was approved by the Biomedicine Ethics Expert Committee of the Kazan Federal University (No. 3, 23.03.2017). A written informed consent was obtained from the donors.
Human adipose-derived stem cells (hADSCs) were isolated as previously described [43]. Subcutaneous adipose tissue samples were obtained during routine liposuction. Blood was removed from the lipoaspirate by centrifugation in a saline solution under sterile conditions in a laminar flow cabinet. The cells obtained were incubated in 0.2% collagenase solution (159 PE/mg, Biolot, Russia) for 45 min at 37 °C with shaking. The digested tissue was centrifuged at 1400 rpm for 5 min at room temperature.
HEK293T cells and hADSCs were cultured in Dulbecco’s Modified Eagle Medium (DMEM, Sigma-Aldrich, USA) supplemented with 10% fetal bovine serum (FBS, Invitrogen, USA), 2 mM l-glutamine (PanEco, Russia), and antibiotics (100 U/mL penicillin, 100 μg/mL streptomycin, Biolot, Russia) at 37 °C in a humidified atmosphere containing 5% CO2.
Human umbilical vein endothelial cells (HUVEC) were isolated from a 20–30-cm umbilical cord. The external surface of the umbilical cord had been treated with sterile Hanks solution (PanEco, Russia) containing antibiotics (100 U/mL penicillin, 100 μg/mL streptomycin, Biolot, Russia) and the ends of the umbilical cord were removed (about 1 cm from each end). The umbilical vein cavity was washed with sterile Hanks solution to completely remove any blood and then filled with a 0.25% sterile trypsin-EDTA solution (Invitrogen, USA) and subjected to enzymatic dissociation. This was achieved with a PBS solution preheated to 37 °C and incubation at 37 °C for 20 min.
The trypsin-EDTA solution containing endothelial cells was collected in a 50-mL tube with 2 mL of FBS. The cells were precipitated by centrifugation (1700 rpm for 10 min) and the pellet resuspended in a growth medium. The HUVEC were cultured in a MCDB 131 medium (Sigma-Aldrich, USA) containing 20% FBS (Invitrogen, USA), 2 mM l-glutamine (PanEco, Russia), antibiotics (100 U/mL penicillin, 100 μg/mL streptomycin, Biolot, Russia), 2 ng/mL FGF2 (Sigma-Aldrich, USA), 10 ng/mL VEGF (Sigma-Aldrich, USA), 10 ng/mL EGF (Sigma-Aldrich, USA), and 10 μg/mL heparin (Sigma-Aldrich, USA). The cells were seeded in 10-cm Petri dishes coated with a 0.2% gelatin solution (Millipore, USA) and cultured at 37 °C in a humidified atmosphere containing 5% СО2 [44].
Cell passaging with a 0.25% trypsin-EDTA solution (Invitrogen, USA) and the replacement of the growth medium were performed according to standard protocols.
Immunophenotyping of hADSCs
hADSCs were immunophenotyped with the use of the BD Stemflow™ Human MSC Analysis Kit (BD Biosciences, USA). In addition, antibodies to CD29 (Cat. No. 102208, BioLegend, USA) and CD166 (Cat. No. 2319515, SONY, USA) were also employed. Appropriate isotype-matched, nonreactive fluorochrome-conjugated antibodies were used as controls. Cell populations were analyzed with FACS Aria III (BD Biosciences, USA) as previously described [45] and the data were processed with the BD FACSDiva™ software, version 7.0.
Genetic Modification of Cells
HEK293T and hADSCs were genetically modified (transfected) with the pBud-SDF-1α-VEGF165 plasmid using TurboFect transfection reagent (Thermo Fisher Scientific Inc., USA) according to the manufacturer’s protocol. For transfection, the cells were seeded in 12-well culture plates and grown to 60–70% confluence. The transfection efficiency was assessed with a pEGFP-N2 plasmid vector (BD Biosciences Clontech, Germany) expressing enhanced green fluorescent protein (EGFP).
Immunofluorescence Assay
HEK293T cells genetically modified with pBud-SDF-1α-VEGF165 plasmid were used for an immunofluorescence assay of the SDF-1α and VEGF165 expression and immunofluorescence evaluated 48 h after cell transfection. For this purpose, the cells were fixed with methanol for 10 min at − 20 °C and washed with a TBS solution (50 mM Tris, 150 mM NaCl, pH 7.6). They were incubated with primary polyclonal antibodies to VEGF (1:100, sc-152, Santa Cruz Biotechnology, Inc., USA) and SDF-1 (1:100, sc-28876, Santa Cruz Biotechnology, Inc., USA) in TBS for 1 h at room temperature. Then, the cells were washed with TBS solution and incubated with Alexa-488-conjugated secondary antibodies (1:1000, A-11008, Life Technologies Corporation, USA) for 1 h at room temperature in the dark. After washing with TBS, a DAPI fluorescent dye (1 ng/μL; Invitrogen, USA) was added and the cells again incubated for 5 min and washed with TBS.
Microscopy
Cell morphology and fluorescence were evaluated under an Axio Observer.Z1 inverted fluorescence microscope (Carl Zeiss, Germany) using the AxioVisionRel.4.8. software.
ELISA
To analyze the VEGF165 protein expression, we used a conditioned medium (CM) collected 24 h after transfection of HEK293T cells and hADSCs with the pBud-SDF-1α-VEGF165 plasmid. The CM was collected in separated tubes and centrifuged at maximum speed for 5 min, and the supernatant was transferred into new tubes and stored at − 20 °C. The VEGF concentration in the CM (10× diluted) was determined using the VEGF-ELISA-BEST Kit (A-8784, Vector, Russia) according to the manufacturer’s recommendations. The optical density in the wells was measured with the Infinite M200Pro reader (Tecan Trading AG, Switzerland) in a two-wave mode: the main filter — 450 nm and the reference filter — 655 nm.
Formation of Capillary-Like Structures on Matrigel
When a monolayer reached a density of 70–80%, HUVEC (passage 2) were removed from the plate with trypsinization and resuspended in a growth factor-free MCDB 131 medium (Cat. # M8537, Sigma-Aldrich, USA) containing 10% FBS and 30% CM of native or genetically modified HEK293T cells. HUVEC (2 × 104 cells) were cultured in a 96-well plate on a thin layer of Matrigel™ Matrix (BD Biosciences, USA) at 37 °C in a humidified atmosphere containing 5% CO2. The formation of capillary-like structures was evaluated after 16–18 h. A tube formation (a total network length in pixels) was quantified with an angiogenesis analyzer plugin for ImageJ [46].
Сell Proliferation Assay
HUVEC (passage 2) (5 × 103 cells) were cultured in growth factor-free MCDB 131 containing 10% FBS for 24 h, and then, the medium was refreshed with the addition of 30% CM from native or genetically modified HEK293T cells. The HUVEC proliferation was evaluated after 24 h using the CellTiter 96® AQueous Non-Radioactive Cell Proliferation Assay (Promega, USA). Optical density in the wells was measured using the Infinite M200Pro reader (Tecan Trading AG, Switzerland) in the two-wave mode: the main filter — 490 nm and the reference filter — 630 nm.
Statistical Analysis
The data obtained were analyzed using the GraphPad Prism 7 software (GraphPad Software) with one-way ANOVA followed by a Tukey HSD post hoc comparison test. Significant probability values were denoted as follows: *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001, ns — no statistically significant difference.
Results and Discussion
VEGF is an important signaling protein involved in vasculogenesis and angiogenesis. Five isoforms of human VEGF mRNA consisting of 121, 145, 165, 189, and 206 amino acids are known. VEGF121 and VEGF165 transcripts are found in most cells and tissues of the body [47]. VEGF121 lacks the amino acids encoded by exon 7 of the VEGF gene, which is present in VEGF165 and provides its ability to bind to heparin and heparan sulfate. The binding of VEGF165 to VEGF receptors on the surface of vascular endothelial cells is modulated by the addition of exogenous heparin or heparan sulfate and is inhibited after the cleavage of endothelial cells with heparinase. A number of studies have shown that the activity of VEGF165 as a endothelial cell mitogen may be higher than that of VEGF121 [48, 49].
SDF-1, also known as the chemokine (C-X-C motif) ligand 12 (CXCL12), is a CXC chemokine and a ligand for CXCR-4 receptor. There are two known isoforms, SDF-1α and SDF-1β, which are encoded by a single gene and are formed as a result of different splicing [50]. SDF-1 acts as a growth factor for B cells and stimulates their proliferation. The transmission of CXCR4–CXCL12 signals promotes chemotaxis, increases proliferation, and inhibits apoptosis in many types of cells. During embryogenesis, SDF-1 controls the migration of hematopoietic cells from the fetal liver to bone marrow and the formation of large blood vessels. In adulthood, SDF-1 plays an important role in angiogenesis by attracting EPCs from bone marrow through a CXCR4-dependent mechanism [51].
Wild-type nucleotide sequences of coding regions of VEGF165 and SDF-1α genes contain a tandem of rare codons that can stop translation or reduce its effectiveness. By optimizing the wild-type codon composition of the SDF-1α gene, the codon adaptation index was (CAI) improved from 0.77 to 0.88. When optimizing the wild-type codon composition of the VEGF165 gene, the CAI was improved from 0.81 to 0.87. To increase the mRNA stability, the GC composition was optimized and extended regions with high GC pairs were removed. In addition, potential cis-acting sites were removed in the process of optimization. The codon optimization did not change the amino acid sequences of SDF-1α and VEGF165 genes which consisted of 89 and 191 amino acid residues, respectively. It enhanced the efficacy of mRNA translation into polypeptides, thereby increasing the efficacy of expression vectors that can be useful for gene therapy. The more frequently a codon used to encode an amino acid occurs in the body, the faster it will be transmitted by ribosomes owing to the high intracellular concentration of tRNA recognizing this codon. For this reason, the most common synonymous codons of a recipient are used as optimal ones. It is believed that such modifications can increase the expression efficacy of a therapeutic gene. The optimization of codon composition is carried out using the site-directed mutagenesis or chemical synthesis of the nucleotide sequence de novo [52].
De novo synthesis of codon-optimized nucleotide sequences of VEGF165 and SDF-1α gene cDNA and its subcloning into a modified pBudС4.1-based plasmid vector (Invitrogen, USA) were carried out by GenScript. The pBudCE4.1 vector is designed for cloning and simultaneous independent expression of two genes. The SDF-1α gene expression in the pBudCE4.1 vector plasmid is under the control of the human cytomegalovirus (CMV) immediate-early promoter that of the VEGF165 gene is controlled by the human elongation factor 1α subunit (EF-1α) (Fig. 1). Independent expression of recombinant genes under the control of two strong constitutionally active promoters CMV and EF-1α improves the efficacy of transgene delivery to target cells. A restriction analysis (Fig. 1) and sequencing were done to confirm the correct assembling of the pBud-SDF-1α-VEGF165 genetic construct. Two fragments sized 4806 bp (contains a segment of the pBudС4.1 plasmid with the VEGF165 gene) and 697 bp (contains a segment of the pBudС4.1 plasmid with the SDF-1α gene) were obtained as a result of restriction cleavage with SacI and MluI enzymes.
Analysis of pBud-SDF-1α-VEGF165 plasmid. A plasmid map (a). Restriction enzyme digest of pBud-SDF-1α-VEGF165 (b). Agarose gel electrophoresis. Band 1—native undigested pBud-SDF-1α-VEGF165 plasmid. Band 2—pBud-SDF-1α-VEGF165 plasmid digested with SacI and MluI restriction enzymes. М—DNA molecular weight marker III (GenScript, USA)
Mesenchymal stem cells were isolated from human adipose tissue and immunophenotyped. Isolated hADSCs expressed CD44 (91.8%), CD73 (99.4%), CD99 (93.4%), CD29 (96.5%), and CD166 (86.2%) markers, but did not express those of hematopoietic cells (Fig. 2).
HEK293T cells and hADSCs with the pBud-SDF-1α-VEGF165 plasmid were genetically modified (transfected) with a TurboFect transfection reagent (Thermo Fisher Scientific Inc., USA) according to the manufacturer’s protocol. To evaluate the transfection efficiency, a pEGFP-N2 plasmid vector (BD Biosciences Clontech, Germany) expressing EGFP was used as a positive control. EGFP expression levels were evaluated 24 h and 48 h after transfection with fluorescence microscopy. After transfection, the vast majority of HEK293T cells and hADSCs had green fluorescence, which indicated efficient transfection (data are not shown).
To assess the expression of SDF-1 and VEGF in transfected HEK293T cells, an immunofluorescence assay was performed with polyclonal antibodies to SDF-1 and VEGF. The immunofluorescence assay of HEK293T cells transfected with the pBud-SDF-1α-VEGF165 plasmid demonstrated a positive reaction with antibodies to SDF-1 and VEGF (Fig. 3), thereby confirming the secretion of SDF-1α and VEGF165 recombinant proteins in genetically modified HEK293T cells.
Immunofluorescence assay of SDF-1 and VEGF expression in HEK293T cells transfected with the pBud-SDF-1α-VEGF165 plasmid. 48 h after transfection. BF — phase-contrast microscopy. AlexaFluor488 — staining with primary antibodies to VEGF or SDF-1 and secondary Alexa-488-conjugated antibodies. GOI — gene of interest. DAPI — staining with a DAPI fluorescent dye. Merge — combined blue and green fluorescence. NTC — non-transfected cells. Scale: 100 μm
The VEGF concentration in the CM collected from HEK293T cells and hADSCs 24 h after transfection was determined by ELISA. There was a statistically significant (p ≤ 0.0001) increase in the VEGF secretion by more than 50 and 20 times in pBud-SDF-1α-VEGF165-transfected HEK293T cells and hADSCs, respectively, as compared with non-transfected cells and those transfected with a pEGFP-N2 reporter plasmid (Fig. 4). Thus, transfected HEK293T cells and hADSCs were shown to express VEGF and SDF-1 recombinant proteins, indicating successful genetic modification of these cells.
Mesenchymal stem cells (MSCs) are known to have regenerative properties that can be enhanced by the addition of genes of pro-angiogenic trophic growth factors and cytokines. During transplantation, MSCs can stimulate angiogenesis in two ways: either by exerting paracrine effects (stimulating the formation of blood vessels from host tissue by secreting angiogenic factors) or by differentiating into endothelial or pericyte-like cells which are actively involved in the formation of new blood vessels [53]. Plasmid vectors are one of the safest vectors for genetic modification of MSCs since they have low immunogenicity and minimal risk of insertional mutagenesis [54]. Genetic modification of hADSCs with the pBud-SDF-1α-VEGF165 plasmid vector can increase the therapeutic potential of these cells through SDF-1α and VEGF165 overexpression. Other authors have proposed using pBudCE4.1 vector for the enhanced expression of bioactive recombinant growth factors, in particular VEGF-111, in mammalian cells (CHO-dhfr- and HEK 293 cell lines) [55].
SDF-1 factor plays an important role in the mobilization and migration of MSCs, which can migrate directly to ischemic tissues along the SDF-1 concentration gradient [36]. MSCs are known to be capable of differentiating into endothelial cells in the presence of SDF-1α. The transplantation of SDF-1α-genetically modified MSCs (MSCs-SDF-1α) was shown to reduce the size of infarction and fibrosis and to increase vascular density and left ventricular wall thickness in a rat model of myocardial infarction. The measurement of hemodynamic parameters showed an improvement in the left ventricular performance in the MSCs-SDF-1α group [56]. Thus, the modification of MSCs with a combination of SDF-1α and VEGF165 genes cannot only increase vascularization but also provide a targeted migration to ischemic tissues due to the SDF-1α expression.
Various studies have shown cytokines and growth factors to stimulate the growth of blood vessels. To study the efficacy of angiogenesis paracrine stimulation with genetically modified cells which simultaneously express SDF-1α and VEGF165, we used a model of HUVEC proliferation in vitro.
To investigate the angiogenic efficacy of HEK293T cells transfected with the pBud-SDF-1α-VEGF165 plasmid, the CM effect on the formation of capillary-like structures by HUVEC on Matrigel was evaluated. For this purpose, a CM from НЕК293Т transfected with the pBud-SDF-1α-VEGF165 plasmid was added to a growth medium used to harvest HUVEC. At the same time, the proliferation activity of HUVEC reflected stimulating effects of soluble factors released into the growth medium as a result of normal HEK293T cell functioning, as well as the expression of a transgene encoding secreted growth factors.
With systemic or intramuscular administration of genetic drugs, endothelial cells are not always a target for direct gene therapy. However, endothelial cells are one of the main targets of paracrine stimulation by endogenous or recombinant growth factors in angiogenesis. For this reason, a model of the conditioned medium which modulates paracrine processes of angiogenesis stimulation in vitro was chosen. HUVEC were cultured on Matrigel in a growth factor-free MCDB 131 medium with a reduced amount of FBS (10%). This is because, the use of MCDB 131 medium containing 20% FBS and growth factors will prevent the evaluation of the effects of recombinant factors (VEGF165 and SDF-1α) from a conditioned medium of HEK293T cells on the HUVEC proliferation and the formation of capillary-like structures on Matrigel. The growth factor-free MCDB 131 containing 10% FBS can maintain the viability of HUVEC but limits their ability to proliferate.
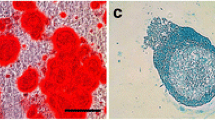
The CM from HEK293T cells genetically modified with the pBud-SDF-1α-VEGF165 plasmid was shown to stimulate the formation of capillary-like structures by HUVEC in vitro, unlike CM of non-transfected cells or HEK293T cells transfected with the pEGFP-N2 plasmid (Fig. 5a–c). Fewer capillary-like structures were formed in the HUVEC cultured in MCDB 131 medium without growth factors and FBS or with 10% FBS when compared with other study groups (Fig. 5 d and e). The formation of capillary-like structures was most obvious in HUVEC cultured in MCDB 131 containing 20% FBS and FGF2, VEGF, and EGF recombinant growth factors (Fig. 5f).
Formation of capillary-like structures by HUVEC on Matrigel. Concentration of CM from HEK293Т is 30%. CM from non-transfected cells (NTC) (a). CM from transfected with pEGFP-N2 cells (b). CM from the cells transfected with the pBud-SDF-1α-VEGF165 (c). FBS and growth factor-free MCDB 131 (d). Growth factor-free MCDB 131 with 10% FBS (e). MCDB 131 with 20% FBS and recombinant growth factors (f). Scale: 500 μm
The conditioned medium collected from HEK293T cells transfected with the pBud-SDF-1α-VEGF165 plasmid promoted the formation of the largest number of nodes, junctions, meshes, and segments of HUVEC on Matrigel as compared with the CM from native or pEGFP-N2-transfected HEK293T cells (p < 0.0001, Fig. 6). Interestingly, there was no statistically significant difference in the number of meshes formed by HUVEC on Matrigel when cultured with the addition of CM from pBud-SDF-1α-VEGF165 plasmid-transfected HEK293T cells and by HUVEC cultured in MCDB 131 containing 20% FBS and recombinant growth factors. The longest tube formed by HUVEC cultured in MCDB 131 containing 20% FBS and recombinant growth factors was about 30,000 μm. The CM collected from pBud-SDF-1α-VEGF165 plasmid-transfected HEK293T cells promoted tubes with an average length of 25,000 μm, three times longer than that of the tubes formed by HUVEC when cultured with the addition of CM from native or pEGFP-N2-transfected HEK293T cells (p < 0.0001, Fig. 6). However, tubes formed by HUVEC cultured in the addition of CM from pBud-SDF-1α-VEGF165 plasmid-transfected HEK293T cells were shorter than those of HUVEC cultured in MCDB 131 containing 20% FBS and recombinant growth factors (p < 0.01, Fig. 6). Similarly, numbers of nodes, junctions, meshes, and segments of HUVEC on Matrigel were higher in samples cultured in MCDB 131 containing 20% FBS and recombinant growth factors compared with HUVEC cultured with the addition of CM from pBud-SDF-1α-VEGF165 plasmid-transfected HEK293T cells (p < 0.05, Fig. 6).
Quantitative analysis of nodes, junctions, meshes, and tube length formed by HUVEC on Matrigel. Conditioned medium collected from HEK293T cells transfected with various plasmid constructs was added at a final concentration of 30%. Complete medium — MCDB 131 medium containing 20% FBS and recombinant growth factors. Poor medium — FBS and growth factor-free MCDB 131 medium. Data are presented as mean ± standard deviation (n = 3).
Genetic modification of HEK293T cells with the pBud-SDF-1α-VEGF165 plasmid was also shown to promote the secretion of recombinant growth factors in the CM, which in turn, when added to HUVEC, increases their proliferation by more than 20% when compared with CM from native HEK293T and pEGFP-N2 plasmid-transfected HEK293T cells (p < 0.0001, Fig. 7). Interestingly, the proliferative activity of HUVEC was 23% higher when cultured in MCDB 131 medium containing 20% FBS and recombinant growth factors compared with HUVEC cultured with the addition of CM from pBud-SDF-1α-VEGF165 plasmid-transfected HEK293T cells (p < 0.0001, Fig. 7). The results show that genetic modification of HEK293Т cells with the pBud-SDF-1α-VEGF165 vector may contribute to an improvement of the angiogenic potential of these cells, confirmed by increases in migration, proliferation, and organization of endothelial cells into vessel-like structures.
Proliferative activity of HUVEC. Conditioned medium collected from HEK293T cells transfected with various plasmid constructs was added at a final concentration of 30%. Complete medium — MCDB 131 medium containing 20% FBS and recombinant growth factors. Poor medium — FBS and growth factor-free MCDB 131 medium. The proliferative activity of HUVEC with the addition of the CM from non-transfected HEK293T cells (NTC) is taken as 100%. Data are presented as mean ± standard deviation (n = 3).
Other studies have also shown that the combination of SDF-1α and VEGF significantly increases EPC-mediated angiogenesis by reducing apoptotic EPCs. SDF-1α also induces the release of VEGF from EPCs, which further increased the mitogenic response to VEGF [21]. It was also shown that CXCL12 can enhance the expression of VEGF, placental growth factor (PLGF), FGF2, and stem cell factor (SCF) genes in vitro [57]. Thus, the combination of VEGF and SDF-1α in gene or gene-cell therapy is a promising strategy for therapeutic neovascularization.
Conclusions
The angiogenic potential of the pBud-SDF-1α-VEGF165 plasmid expressing VEGF165 and SDF-1α has been evaluated in the present study. We showed that pBud-SDF-1α-VEGF165-transfected HEK293T cells and hADSCs expressed VEGF and SDF-1 recombinant proteins. The CM collected from HEK293T cells transfected with the pBud-SDF-1α-VEGF165 plasmid was used to investigate the angiogenic potential of the medium. We observed that the CM collected from pBud-SDF-1α-VEGF165-transduced HEK293T cells stimulated the formation of capillary-like structures by HUVEC on Matrigel in vitro. The proliferative activity of HUVEC after cultivation with the addition of CM from pBud-SDF-1α-VEGF165-transfected HEK293T cells was also assessed and shown to increase the proliferative activity of HUVEC by more than 20% when compared with the CM from native and pEGFP-N2 plasmid-transfected cells. Thus, the pBud-SDF-1α-VEGF165 plasmid exhibits angiogenic properties in cell culture in vitro. As the development of non-viral technologies for regenerative medicine is of the utmost interest, the pBud-SDF-1α-VEGF165 plasmid which simultaneously expresses VEGF165 and SDF-1α can provide the basis for new strategies for the treatment of ischemic diseases in human.
References
Ouma, G. O., Jonas, R. A., Usman, M. H., & Mohler, E. R., 3rd. (2012). Targets and delivery methods for therapeutic angiogenesis in peripheral artery disease. Vascular Medicine, 17(3), 174–192.
Yla-Herttuala, S., Rissanen, T. T., Vajanto, I., & Hartikainen, J. (2007). Vascular endothelial growth factors: biology and current status of clinical applications in cardiovascular medicine. Journal of the American College of Cardiology, 49(10), 1015–1026.
Bulgin, D. (2015). Therapeutic Angiogenesis in Ischemic Tissues by Growth Factors and Bone Marrow Mononuclear Cells Administration: Biological Foundation and Clinical Prospects. Current Stem Cell Research & Therapy, 10(6), 509–522.
Takeshita, S., Zheng, L. P., Brogi, E., Kearney, M., Pu, L. Q., Bunting, S., Ferrara, N., Symes, J. F., & Isner, J. M. (1994). Therapeutic angiogenesis. A single intraarterial bolus of vascular endothelial growth factor augments revascularization in a rabbit ischemic hind limb model. The Journal of Clinical Investigation, 93(2), 662–670.
Bauters, C., Asahara, T., Zheng, L. P., Takeshita, S., Bunting, S., Ferrara, N., Symes, J. F., & Isner, J. M. (1995). Site-specific therapeutic angiogenesis after systemic administration of vascular endothelial growth factor. Journal of Vascular Surgery, 21(2), 314–324 discussion 324-315.
Zisa, D., Shabbir, A., Mastri, M., Suzuki, G., & Lee, T. (2009). Intramuscular VEGF repairs the failing heart: role of host-derived growth factors and mobilization of progenitor cells. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, 297(5), R1503–R1515.
Sato, K., Laham, R. J., Pearlman, J. D., Novicki, D., Sellke, F. W., Simons, M., & Post, M. J. (2000). Efficacy of intracoronary versus intravenous FGF-2 in a pig model of chronic myocardial ischemia. The Annals of Thoracic Surgery, 70(6), 2113–2118.
Efthimiadou, A., Asimakopoulos, B., Nikolettos, N., Giatromanolaki, A., Sivridis, E., Papachristou, D. N., & Kontoleon, E. (2006). Angiogenic effect of intramuscular administration of basic and acidic fibroblast growth factor on skeletal muscles and influence of exercise on muscle angiogenesis. British Journal of Sports Medicine, 40(1), 35–39 discussion 35-39.
Morishita, R., Nakamura, S., Hayashi, S., Taniyama, Y., Moriguchi, A., Nagano, T., Taiji, M., Noguchi, H., Takeshita, S., Matsumoto, K., Nakamura, T., Higaki, J., & Ogihara, T. (1999). Therapeutic angiogenesis induced by human recombinant hepatocyte growth factor in rabbit hind limb ischemia model as cytokine supplement therapy. Hypertension, 33(6), 1379–1384.
Li, W. W., Talcott, K. E., Zhai, A. W., Kruger, E. A., & Li, V. W. (2005). The role of therapeutic angiogenesis in tissue repair and regeneration. Advances in Skin & Wound Care, 18(9), 491–500 quiz 501-492.
Takeshita, S., Pu, L. Q., Stein, L. A., Sniderman, A. D., Bunting, S., Ferrara, N., Isner, J. M., & Symes, J. F. (1994). Intramuscular administration of vascular endothelial growth factor induces dose-dependent collateral artery augmentation in a rabbit model of chronic limb ischemia. Circulation, 90(5 Pt 2), II228–II234.
Becit, N., Ceviz, M., Kocak, H., Yekeler, I., Unlu, Y., Celenk, C., & Akin, Y. (2001). The effect of vascular endothelial growth factor on angiogenesis: an experimental study. European Journal of Vascular and Endovascular Surgery : The Official Journal of the European Society for Vascular Surgery, 22(4), 310–316.
Pearlman, J. D., Hibberd, M. G., Chuang, M. L., Harada, K., Lopez, J. J., Gladstone, S. R., Friedman, M., Sellke, F. W., & Simons, M. (1995). Magnetic resonance mapping demonstrates benefits of VEGF-induced myocardial angiogenesis. Nature Medicine, 1(10), 1085–1089.
Kottakis, F., Polytarchou, C., Foltopoulou, P., Sanidas, I., Kampranis, S. C., & Tsichlis, P. N. (2011). FGF-2 regulates cell proliferation, migration, and angiogenesis through an NDY1/KDM2B-miR-101-EZH2 pathway. Molecular Cell, 43(2), 285–298.
Laham, R. J., Rezaee, M., Post, M., Sellke, F. W., Braeckman, R. A., Hung, D., & Simons, M. (1999). Intracoronary and intravenous administration of basic fibroblast growth factor: myocardial and tissue distribution. Drug Metabolism and Disposition: The Biological Fate of Chemicals, 27(7), 821–826.
Lazarous, D. F., Shou, M., Stiber, J. A., Dadhania, D. M., Thirumurti, V., Hodge, E., & Unger, E. F. (1997). Pharmacodynamics of basic fibroblast growth factor: route of administration determines myocardial and systemic distribution. Cardiovascular Research, 36(1), 78–85.
Deepa, K., Rodionov, R. N., Weiss, N., & Parani, M. (2013). Transgenic expression and functional characterization of human platelet derived growth factor BB (hPDGF-BB) in tobacco (Nicotiana tabacum L.). Applied Biochemistry and Biotechnology, 171(6), 1390–1404.
Choi, J. H., Kim, S., Sapkota, K., Park, S. E., & Kim, S. J. (2011). Expression and production of therapeutic recombinant human platelet-derived growth factor-BB in Pleurotus eryngii. Applied Biochemistry and Biotechnology, 165(2), 611–623.
Yang, F., Xue, F., Guan, J., Zhang, Z., Yin, J., & Kang, Q. (2018). Stromal-Cell-Derived Factor (SDF) 1-Alpha Overexpression Promotes Bone Regeneration by Osteogenesis and Angiogenesis in Osteonecrosis of the Femoral Head. Cellular Physiology and Biochemistry, 46(6), 2561–2575.
Deshane, J., Chen, S., Caballero, S., Grochot-Przeczek, A., Was, H., Li Calzi, S., Lach, R., Hock, T. D., Chen, B., Hill-Kapturczak, N., Siegal, G. P., Dulak, J., Jozkowicz, A., Grant, M. B., & Agarwal, A. (2007). Stromal cell-derived factor 1 promotes angiogenesis via a heme oxygenase 1-dependent mechanism. The Journal of Experimental Medicine, 204(3), 605–618.
Yu, J. X., Huang, X. F., Lv, W. M., Ye, C. S., Peng, X. Z., Zhang, H., Xiao, L. B., & Wang, S. M. (2009). Combination of stromal-derived factor- 1alpha and vascular endothelial growth factor gene-modified endothelial progenitor cells is more effective for ischemic neovascularization. Journal of Vascular Surgery, 50(3), 608–616.
Ho, T. K., Tsui, J., Xu, S., Leoni, P., Abraham, D. J., & Baker, D. M. (2010). Angiogenic effects of stromal cell-derived factor-1 (SDF-1/CXCL12) variants in vitro and the in vivo expressions of CXCL12 variants and CXCR4 in human critical leg ischemia. Journal of Vascular Surgery, 51(3), 689–699.
Gorenoi, V., Brehm, M. U., Koch, A., & Hagen, A. (2017). Growth factors for angiogenesis in peripheral arterial disease. Cochrane Database of Systematic Reviews, (6), CD011741.
Inampudi, C., Akintoye, E., Ando, T., & Briasoulis, A. (2018). Angiogenesis in peripheral arterial disease. Current Opinion in Pharmacology, 39, 60–67.
King, A., Balaji, S., Keswani, S. G., & Crombleholme, T. M. (2014). The Role of Stem Cells in Wound Angiogenesis. Advances in Wound Care, 3(10), 614–625.
Hou, L., Kim, J. J., Woo, Y. J., & Huang, N. F. (2016). Stem cell-based therapies to promote angiogenesis in ischemic cardiovascular disease. American Journal of Physiology. Heart and Circulatory Physiology, 310(4), H455–H465.
Solovyeva, V. V., Blatt, N. L., Shafigullina, A. K., & Rizvanov, A. A. (2012). Endogenous secretion of vascular endothelial growth factor by multipotent mesenchymal stromal cells derived from human third molar dental follicles. Cellular Transplantation and Tissue Engineering, 7(3), 155–158.
Fierro, F. A., Magner, N., Beegle, J., Dahlenburg, H., Logan White, J., Zhou, P., Pepper, K., Fury, B., Coleal-Bergum, D. P., Bauer, G., Gruenloh, W., Annett, G., Pifer, C., & Nolta, J. A. (2018). Mesenchymal stem/stromal cells genetically engineered to produce vascular endothelial growth factor for revascularization in wound healing and ischemic conditions. Transfusion.
Bortolotti, F., Ukovich, L., Razban, V., Martinelli, V., Ruozi, G., Pelos, B., Dore, F., Giacca, M., & Zacchigna, S. (2015). In vivo therapeutic potential of mesenchymal stromal cells depends on the source and the isolation procedure. Stem Cell Reports, 4(3), 332–339.
Raval, Z., & Losordo, D. W. (2013). Cell therapy of peripheral arterial disease: from experimental findings to clinical trials. Circulation Research, 112(9), 1288–1302.
Sanada, F., Taniyama, Y., Kanbara, Y., Otsu, R., Ikeda-Iwabu, Y., Carracedo, M., Rakugi, H., & Morishita, R. (2015). Gene therapy in peripheral artery disease. Expert Opinion on Biological Therapy, 15(3), 381–390.
Yla-Herttuala, S., & Baker, A. H. (2017). Cardiovascular Gene Therapy: Past, Present, and Future. Molecular Therapy, 25(5), 1095–1106.
Walder, C. E., Errett, C. J., Bunting, S., Lindquist, P., Ogez, J. R., Heinsohn, H. G., Ferrara, N., & Thomas, G. R. (1996). Vascular endothelial growth factor augments muscle blood flow and function in a rabbit model of chronic hindlimb ischemia. Journal of Cardiovascular Pharmacology, 27(1), 91–98.
Chervyakov, Y. V., Staroverov, I. N., Vlasenko, O. N., Bozo, I. Y., Isaev, A. A., & Deev, R. V. (2016). Five-year results of treating patients with chronic lower limb ischaemia by means of gene engineering. Angiol Sosud Khir, 22(4), 38–44.
Kalinin, R. E., Suchkov, I. A., Deev, R. V., Mzhavanadze, N. D., & Krylov, A. A. (2018). Gene-mediated induction of angiogenesis in inoperable patients with atherosclerosis and diabetes mellitus. Angiol Sosud Khir, 24(2), 33–40.
Luo, R., Lu, Y., Liu, J., Cheng, J., & Chen, Y. (2019). Enhancement of the efficacy of mesenchymal stem cells in the treatment of ischemic diseases. Biomedicine & Pharmacotherapy = Biomedecine & Pharmacotherapie, 109, 2022–2034.
Stewart, D. J., Hilton, J. D., Arnold, J. M., Gregoire, J., Rivard, A., Archer, S. L., Charbonneau, F., Cohen, E., Curtis, M., Buller, C. E., Mendelsohn, F. O., Dib, N., Page, P., Ducas, J., Plante, S., Sullivan, J., Macko, J., Rasmussen, C., Kessler, P. D., & Rasmussen, H. S. (2006). Angiogenic gene therapy in patients with nonrevascularizable ischemic heart disease: a phase 2 randomized, controlled trial of AdVEGF(121) (AdVEGF121) versus maximum medical treatment. Gene Therapy, 13(21), 1503–1511.
Niebuhr, A., Henry, T., Goldman, J., Baumgartner, I., van Belle, E., Gerss, J., Hirsch, A. T., & Nikol, S. (2012). Long-term safety of intramuscular gene transfer of non-viral FGF1 for peripheral artery disease. Gene Therapy, 19(3), 264–270.
Shigematsu, H., Yasuda, K., Sasajima, T., Takano, T., Miyata, T., Ohta, T., Tanemoto, K., Obitsu, Y., Iwai, T., Ozaki, S., Ogihara, T., Morishita, R., & Group, H. G. F. S. (2011). Transfection of human HGF plasmid DNA improves limb salvage in Buerger's disease patients with critical limb ischemia. International Angiology : a Journal of the International Union of Angiology, 30(2), 140–149.
Lebas, B., Galley, J., Renaud-Gabardos, E., Pujol, F., Lenfant, F., Garmy-Susini, B., Chaufour, X., & Prats, A. C. (2017). Therapeutic Benefits and Adverse Effects of Combined Proangiogenic Gene Therapy in Mouse Critical Leg Ischemia. Annals of Vascular Surgery, 40, 252–261.
Garanina, E. E., Mukhamedshina, Y. O., Salafutdinov, I. I., Kiyasov, A. P., Lima, L. M., Reis, H. J., Palotas, A., Islamov, R. R., & Rizvanov, A. A. (2016). Construction of recombinant adenovirus containing picorna-viral 2A-peptide sequence for the co-expression of neuro-protective growth factors in human umbilical cord blood cells. Spinal Cord, 54(6), 423–430.
Zhuravleva, M. N., Khaliullin, M. R., Masgutov, R. F., Deev, R. V., & Rizvanov, A. A. (2017). Recombinant Plasmid DNA Construct Encoding Combination of vegf165 and bmp2 cDNAs Stimulates Osteogenesis and Angiogenesis In Vitro. Bionanoscience, 7(2), 288–293.
Solovyeva, V. V., Salafutdinov, I. I., Tazetdinova, L. G., Masgutov, R. F., Khaiboullina, S. F., & Rizvanov, A. A. (2014). Genetic Modification of Adipose Derived Stem Cells with Recombinant Plasmid DNA pBud-VEGF-FGF2 Results in Increased of IL-8 and MCP-1 Secretion. Journal of Pure and Applied Microbiology, 8(Spl. Edn. 2), 523–528.
Khaiboullina, S. F., Rizvanov, A. A., Deyde, V. M., & St Jeor, S. C. (2005). Andes virus stimulates interferon-inducible MxA protein expression in endothelial cells. Journal of Medical Virology, 75(2), 267–275.
Solovyeva, V. V., Salafutdinov, I. I., Martynova, E. V., Khaiboullina, S. F., & Rizvanov, A. A. (2013). Human Adipose Derived Stem Cells Do Not Alter Cytokine Secretion in Response To The Genetic Modification With pEGFP-N2 Plasmid DNA. World Applied Sciences Journal, 26(7), 968–972.
Carpentier, G. (2012). Contribution: angiogenesis analyzer. ImageJ News, 5(Available: http://image.bio.methods.free.fr/ImageJ/?Angiogenesis-Analyzer-for-ImageJ.
Apte, R. S., Chen, D. S., & Ferrara, N. (2019). VEGF in Signaling and Disease: Beyond Discovery and Development. Cell, 176(6), 1248–1264.
Yue, X., & Tomanek, R. J. (2001). Effects of VEGF(165) and VEGF(121) on vasculogenesis and angiogenesis in cultured embryonic quail hearts. American Journal of Physiology. Heart and Circulatory Physiology, 280(5), H2240–H2247.
Keyt, B. A., Berleau, L. T., Nguyen, H. V., Chen, H., Heinsohn, H., Vandlen, R., & Ferrara, N. (1996). The carboxyl-terminal domain (111-165) of vascular endothelial growth factor is critical for its mitogenic potency. The Journal of Biological Chemistry, 271(13), 7788–7795.
Neuhaus, T., Stier, S., Totzke, G., Gruenewald, E., Fronhoffs, S., Sachinidis, A., Vetter, H., & Ko, Y. D. (2003). Stromal cell-derived factor 1alpha (SDF-1alpha) induces gene-expression of early growth response-1 (Egr-1) and VEGF in human arterial endothelial cells and enhances VEGF induced cell proliferation. Cell Proliferation, 36(2), 75–86.
Zheng, H., Fu, G., Dai, T., & Huang, H. (2007). Migration of endothelial progenitor cells mediated by stromal cell-derived factor-1alpha/CXCR4 via PI3K/Akt/eNOS signal transduction pathway. Journal of Cardiovascular Pharmacology, 50(3), 274–280.
Inouye, S., Sahara-Miura, Y., Sato, J., & Suzuki, T. (2015). Codon optimization of genes for efficient protein expression in mammalian cells by selection of only preferred human codons. Protein Expression and Purification, 109, 47–54.
Solovyeva, V. V., Kiyasov, A. P. and Rizvanov, A. A. (2016). Genetically Engineered Dental Stem Cells for Regenerative Medicine. Stem Cells Biol Reg, 93–107.
Serra, J., Alves, C. P. A., Brito, L., Monteiro, G. A., Cabral, J. M. S., Prazeres, D. M. F., & da Silva, C. L. (2019). Engineering of Human Mesenchymal Stem/Stromal Cells with Vascular Endothelial Growth Factor-Encoding Minicircles for Angiogenic Ex Vivo Gene Therapy. Human Gene Therapy, 30(3), 316–329.
Hojati, Z., & Dehghanian, F. (2015). Enhanced expression of bioactive recombinant VEGF-111 with insertion of intronic sequence in mammalian cell lines. Applied Biochemistry and Biotechnology, 175(8), 3737–3749.
Tang, J., Wang, J., Yang, J., Kong, X., Zheng, F., Guo, L., Zhang, L., & Huang, Y. (2009). Mesenchymal stem cells over-expressing SDF-1 promote angiogenesis and improve heart function in experimental myocardial infarction in rats. European Journal of Cardio-Thoracic Surgery : Official Journal of the European Association for Cardio-Thoracic Surgery, 36(4), 644–650.
Zhang, L., Zhou, Y., Sun, X., Zhou, J., & Yang, P. (2017). CXCL12 overexpression promotes the angiogenesis potential of periodontal ligament stem cells. Scientific Reports, 7(1), 10286.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
The work was funded by the Human Stem Cells Institute and performed according to the Russian Government Program of Competitive Growth of the Kazan Federal University. AR was supported by the state assignment 20.5175.2017/6.7 of the Ministry of Education and Science of the Russian Federation and the President of the Russian Federation grant НШ-3076.2018.4. IS and VS were supported by the Russian Foundation for Basic Research grant 16-04-01567.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol was approved by the Biomedicine Ethics Expert Committee of the Kazan Federal University (No. 3, 23.03.2017). Written informed consent was obtained from the donors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Solovyeva, V.V., Chulpanova, D.S., Tazetdinova, L.G. et al. In Vitro Angiogenic Properties of Plasmid DNA Encoding SDF-1α and VEGF165 Genes. Appl Biochem Biotechnol 190, 773–788 (2020). https://doi.org/10.1007/s12010-019-03128-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-019-03128-5