Abstract
Background
Hospital-acquired infections caused by methicillin-resistant Staphylococcus aureus (MRSA) are a source of morbidity and mortality. S. aureus is the most common pathogen in prosthetic joint infections and the incidence of MRSA is increasing.
Questions/Purposes
The purposes of this study were (1) to determine the MRSA prevalence density rate at a specialty orthopaedic hospital before and after implementation of a screening and decolonization protocol, (2) to compare our prevalence density with that of an affiliated university hospital to control for changes in MRSA prevalence density that might have been independent of the decolonization protocol, and (3) to measure the admission prevalence density rate of MRSA in an elective orthopaedic surgery population and the compliance rate of 26 patients with the protocol.
Methods
In October 2008, we implemented a MRSA screening and decolonization protocol for patients undergoing elective orthopaedic surgery. Nasal swabs were used for screening and mupirocin nasal ointment and chlorhexidine skin antisepsis where prescribed for decolonization to all patients. At the surgical visit, compliance was measured and the patients who were MRSA positive received vancomycin for antibiotic prophylaxis. Institution wide surveillance for multidrug-resistant organisms, including MRSA provided a comparison of the change in MRSA burden at the orthopaedic hospital versus the university hospital.
Results
Before implementation of the preoperative staphylococcal decolonization protocol there were 79 MRSA-positive cultures in 64,327 patient-days for a prevalence density rate of 1.23 per 1000 patient-days. After protocol implementation, 53 MRSA-positive cultures were identified in 63,860 patient-days for a rate of 0.83 per 1000 patient-days. Before the protocol, the MRSA prevalence density at the specialty hospital was similar to that of the university hospital; after implementation of the protocol, the prevalence density at the specialty hospital was 33% lower than that of the university hospital. The MRSA admission prevalence was 3.02%. The compliance rate was greater than 95%.
Conclusions
Implementation of a staphylococcal decolonization protocol at a single specialty orthopaedic hospital decreased the prevalence density of MRSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Healthcare payers, such as Medicare, consider hospital-acquired conditions, including hospital-acquired infections, to be preventable and a measure of clinical quality. The recently enacted Patient Protection and Affordable Care Act includes provisions that will change how hospitals are paid for the delivery of medical care, including nonreimbursements for many hospital-acquired infections [1]. Staphylococcus aureus (S. aureus) is a common cause of hospital-acquired infections, such as catheter-associated bloodstream infections, hospital-acquired pneumonia, and surgical site infections (SSIs) [2, 3, 7]. SSIs associated with prosthetic joints lead to considerable patient morbidity and contribute a large burden on the healthcare budget. In 2010 in New York State, 54.4% of hip SSIs were caused by S. aureus [12]. Increased compliance with perioperative antibiotic prophylaxis has reduced the number of SSIs associated with primary prosthetic joint replacements to less than 2% [17]. Nonetheless, methicillin-resistant S. aureus (MRSA) SSIs are common in the United States [2, 3, 9, 12]. Therefore, developing strategies for decreasing perioperative MRSA colonization is important. As much as 30% of healthy adults carry S. aureus in the anterior nares and are at two to nine-times higher risk for any hospital-onset staphylococcal infections after surgical procedures of all types when compared with patients who are noncolonized [16].
Mupirocin is a topical antistaphylococcal antibiotic with an FDA-approved indication for decolonization of the anterior nares [13, 14]. A recent study [5] found that intranasal mupirocin prevents postoperative S. aureus infections in patients who were colonized with S. aureus before surgery. In a randomized, double-blinded study of orthopaedic patients, the use of mupirocin was found to reduce the rate of S. aureus infections to five times lower than that of the placebo group [7]. The cost-effectiveness of universal S. aureus detection in high-risk patient populations for reduction of SSIs and all nosocomial infections attributable to S. aureus has been reported in several studies [1, 4, 6, 13, 16].
In this study, we (1) evaluated the MRSA prevalence density rate at a specialty orthopaedic hospital before and after implementation of a screening and decolonization protocol, (2) compared our prevalence density with that of an affiliated university hospital to control for changes in MRSA prevalence density that might have been independent of the decolonization protocol, and (3) to measure the admission prevalence density rate of MRSA in an elective orthopaedic surgery population and the compliance rate of 26 patients with the protocol.
Materials and Methods
New York University (NYU) Hospital for Joint Disease is a 226-bed, specialty orthopaedic hospital that performs more than 16,000 surgeries annually. Our orthopaedic hospital is located 1 mile from a clinical campus that includes Tisch Hospital, a 726-bed university hospital, and the Rusk Institute, a 161-bed acute rehabilitation hospital. All three hospitals comprise the NYU Langone Medical Center, an urban teaching institution in New York City, USA. Infection control measures to prevent MRSA transmission, such as use of isolation precautions and environmental cleaning, did not change during the study period.
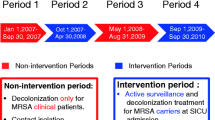
In October 2008, the orthopaedic hospital implemented a staphylococcal decolonization protocol during preadmission testing clinic visits for patients undergoing arthroplasty or spine fusion. The university and rehabilitation hospitals did not implement a decolonization protocol and therefore served as a control. We reviewed all microbiology results at the NYU Langone Medical Center to identify S. aureus clinical cultures obtained during the baseline period (January 2007–October 2008) and after implementation of the new decolonization protocol (November 2008–July 2010). We excluded isolates that were surveillance cultures and outpatient cultures.
Greater than 92% of all scheduled admissions to our institution for elective orthopaedic surgery attended the preadmission testing clinic, during which swabs of both nares were obtained by a clinic nurse and submitted to the microbiology laboratory for S. aureus culture. Isolates were tested for methicillin susceptibility by either disc diffusion or CHROMagar™ methods (CHROMagar™, Paris, France). Regardless of the culture results, all patients were prescribed a 5-day course of twice-daily applied 2% mupirocin nasal ointment and skin antisepsis with either a preoperative chlorhexidine shower the night before surgery (October 2008–October 2009) or chlorhexidine wipes the night before and day of surgery (October 2009–June 2010). At the surgical visit, the operating room nurse asked about treatment compliance, and there was a self-reported 96% compliance with mupirocin nasal treatment and 99% compliance rate with the chlorhexidine shower. Nasal screening results were available for all patients on the day of surgery. Patients who were MRSA-negative were administered standard perioperative antibiotic prophylaxis with either cefazolin or clindamycin at least 30 minutes before incision and for 24 hours postoperatively (Fig. 1). By contrast, patients who were MRSA-positive received vancomycin intravenously at least 30 minutes before incision and every 12 hours thereafter for 24 hours.
Patients scheduled for admission to our institution for elective orthopaedic surgery attended the preadmission testing (PAT) clinic. During the visit swabs of both nares were obtained and submitted to the microbiology laboratory for S. aureus culture. Regardless of the culture results all patients were provided with a prescription for a 5-day course of 2% mupirocin nasal ointment and a preoperative chlorhexidine shower the night before surgery. Nasal screening results were available for all patients on the day of surgery and MRSA-positive carriers were given vancomycin intravenously at least 30 minutes before incision and every 12 h thereafter for 24 hours or two total doses. All patients with MRSA-negative results were administered either cefazolin or clindamycin antibiotic prophylaxis at least 30 minutes before incision and for 24 h postoperatively. Any patient who was noncompliant and had a positive MRSA or MSSA culture received a 5-day course of mupirocin.
Since January 2007 all microbiology laboratory reports for inpatients at NYU Langone Medical Center have been routinely reviewed by infection control practitioners as part of surveillance for multidrug-resistant organisms including MRSA, multidrug-resistant gram-negative bacteria, and vancomycin-resistant enterococci. We calculated MRSA and methicillin-sensitive S. aureus (MSSA) prevalence density rates for each facility in accordance with current guidelines for metrics of multidrug-resistant organisms by including the first MRSA or MSSA clinical isolate (regardless of specimen source) obtained from a hospitalized patient. Subsequent isolates for a given patient and any culture obtained for surveillance purposes (including those obtained in the preadmission testing clinic) were excluded. Rate per 1000 patient days is calculated using hospital census data [8]. A MRSA admission prevalence rate for patients having elective orthopaedic surgery at our orthopedic hospital was calculated by including only MRSA isolates obtained in the preadmission testing clinic (surveillance cultures) per 1000 patients.
Compliance with the decolonization protocol was determined using a standardized preoperative nursing assessment on admission for surgery where patients self-reported their use of the mupirocin nasal ointment and chlorhexidine wash.
Statistical analysis was performed using SPSS® version 20.0 (IBM®, Armonk, New York, USA). Dichotomous variables were compared using Pearson’s Chi square test. Variables with p < 0.05 were considered statistically significant. The study was reviewed and approved by the Institutional Review Board for New York University School of Medicine. There was no external funding in this investigation.
Results
Before implementation of the preoperative staphylococcal decolonization protocol (January 2007–October 2008), there were 79 MRSA clinical cultures in 64,327 patient-days at a rate of 1.23 per 1000 patient-days at our single specialty orthopaedic institution. After implementation of the decolonization protocol, 53 MRSA clinical cultures were identified in 63,860 patient-days at a rate of 0.83 per 1000 patient-days (p = 0.026) (Table 1).
During the same time period at the university and rehabilitation hospitals, there were 396 MRSA clinical cultures in 312,215 patient-days at a rate of 1.27 per 1000 patient-days. After the implementation of the decolonization protocol, there were 441 MRSA clinical cultures in 330,262 patient-days at a rate of 1.24 per 1000 patient-days (Table 1). Before the protocol, the MRSA prevalence density at the specialty hospital was similar to the university hospital; after implementation of the protocol, the prevalence density at the specialty hospital was 33% lower than that of the university hospital. Prevalence rates for MSSA before and after implementation of the decolonization protocol did not differ significantly at either hospital.
The MRSA admission prevalence density rate (or colonization rate) in patients undergoing preadmission testing for elective orthopaedic surgery was 3.02%. The patient-self-reported compliance rate for mupirocin treatment was 96% and the rate for the chlorhexidine shower was 98% (Table 2).
Discussion
MRSA-associated prosthetic joint infections lead to considerable patient morbidity and contribute a large burden to the healthcare budget. The purpose of this study was to evaluate the effect of a decolonization protocol on hospital MRSA burden in an orthopaedic surgery population. We found that a MRSA screening and decolonization protocol significantly decreased the prevalence density of MRSA. This decrease was not seen at our affiliated university hospital which did not adopt the screening protocol and further substantiates these findings.
This study has several limitations. First, we are unable to state definitively a cause-and-effect relationship between our decolonization protocol and the considerable decrease in MRSA burden. Other institutional changes during the study period at our institution could be responsible for the decreased rate. However, we attempted to account for this possibility with a comparison of MRSA rates in the baseline and postimplementation periods at the university hospital as a control group. The MRSA screening protocol was not implemented at the university hospital but all other institutional policies were similar between the two hospitals. The MRSA prevalence density at the university hospital did not vary during the study period and therefore lends evidence that the protocol was responsible for the decreased MRSA prevalence. Another weakness of the study is the calculation of MRSA prevalence density rates for each facility per 1000 patient days using hospital census data rather than incidence of SSIs. We performed a power analysis to determine the sample size necessary to reach statistical significance comparing SSIs and determined 115,000 patients would be needed. The low rate of postoperative prosthetic infections would make such a study impractical. Although overall incidence of prosthetic infections is low, the consequences of an infection for a patient can be devastating leading to significant morbidity, mortality, and healthcare cost. We did not measure resistance to mupirocin at baseline or postimplementation of our decolonization protocol. Although mupirocin resistance following mupirocin treatment has been observed, this phenomenon has not been widely reported after use for decolonization [15]. Specifically, among studies [5, 16, 17] reporting short-term use of mupirocin for perioperative decolonization similar to our protocol, an increase in the prevalence of MRSA strains was not observed. Finally, our conclusions are limited by the multiple components of our screening and decolonization protocol. We are unable to determine the specific contribution of each decolonization measure in decreasing MRSA burden.
The burden of MRSA was reduced by our screening and decolonization intervention. The staphylococcal decolonization protocol at our orthopaedic hospital may decrease the prevalence of MRSA by decreasing the risk of horizontal transmission of MRSA between patients. Reducing the MRSA burden in a hospital setting by instituting decolonization measures may reduce the incidence of nosocomial MRSA infections. Chlorhexidine was used as presurgical antisepsis throughout the study. Therefore, our findings during the 2-year study period may be an important finding for the surgical literature.
During the same period, the rate of MRSA at the main clinical campus remained constant. These findings showed a reduction in the MRSA burden at our orthopaedic hospital. Although we did not observe a decrease in risk of SSI in this study, reducing the prevalence density of MRSA may still be an important step to help reduce the risk of infection, as other research has shown MRSA exposure burden to be an independent risk factor for healthcare-associated acquisition of MRSA [16]. In our study, we used healthcare-associated and community-associated MRSA clinical isolates to define the exposure burden, as this better approximates the risk of exposure for a hospitalized patient. The MRSA colonization rate at preadmission testing for our patients having elective orthopaedic procedures was 3% and is similar to reported prevalence rates [9–11]. This is a significant proportion of patients at high-volume centers and warrants consideration of universal screening and a protocol to decolonize these patients.
The majority of patients reported compliance with topical nasal mupirocin and chlorhexidine shower but it was not 100%. We determined before implementation of the protocol that it was more cost-effective to have everyone participate in the decolonization protocol regardless of their culture results. The preferential decolonization of only screened patients who were MRSA-positive may provide a way to improve compliance.
We found that implementation of a S. aureus screening and decolonization protocol, including mupirocin and chlorhexidine-based skin antisepsis for surgical patients, reduced the prevalence of MRSA at our orthopaedic hospital. Further study of interventions to reduce the burden of MRSA and MSSA may help reduce the incidence of nosocomial S. aureus infection.
References
Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vandenbroucke-Grauls CM, Roosendaal R, Troelstra A, Box AT, Voss A, van der Tweel I, van Belkum A, Verbrugh HA, Vos MC. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362:9–17.
Boucher HW, Corey GR. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008;46(suppl 5):S344–S349.
Caffrey AR, LaPlante KL. Changing epidemiology of methicillin-resistant Staphylococcus aureus in the Veterans Affairs Healthcare System, 2002–2009. Infection. 2012;40:291–297.
De Lucas-Villarrubia JC, Lopez-Franco M, Granizo JJ, De Lucas-Garcia JC, Gomez-Barrena E. Strategy to control methicillin-resistant Staphylococcus aureus post-operative infection in orthopaedic surgery. Int Orthop. 2004;28:16–20.
Groszkruger D. Perspectives on healthcare reform: a year later, what more do we know? J Healthc Risk Manag. 2011;31:24–30.
Kalmeijer MD, Coertjens H, van Nieuwland-Bollen PM, Bogaers-Hofman D, de Baere GA, Stuurman A, van Belkum A, Kluytmans JA. Surgical site infections in orthopedic surgery: the effect of mupirocin nasal ointment in a double-blind, randomized, placebo-controlled study. Clin Infect Dis. 2002;35:353–358.
Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, Harrison LH, Lynfield R, Dumyati G, Townes JM, Craig AS, Zell ER, Fosheim GE, McDougal LK, Carey RB, Fridkin SK. Active Bacterial Core surveillance (ABCs) MRSA Investigators. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771.
Lindeque B, Rutigliano J, Williams A, McConnell J. Prevalence of methicillin-resistant Staphylococcus aureus among orthopedic patients at a large academic hospital. Orthopedics. 2008;31:363.
Maranan MC, Moreira B, Boyle-Vavra S, Daum RS. Antimicrobial resistance in staphylococci: epidemiology, molecular mechanisms, and clinical relevance. Infect Dis Clin North Am. 1997;11:813–849.
Merrer J, Santoli F, Appere de Vecchi C, Tran B, De Jonghe B, Outin H. “Colonization pressure” and risk of acquisition of methicillin-resistant Staphylococcus aureus in a medical intensive care unit. Infect Control Hosp Epidemiol. 2000; 21:718–723.
Moyad TF, Thornhill T, Estok D. Evaluation and management of the infected total hip and knee. Orthopedics. 2008;31:581–588; quiz 589–590.
New York State Department of Health. Hospital-Acquired Infections, New York State, 2010. Available at: http://www.health.ny.gov/statistics/facilities/hospital/hospital_acquired_infections/2010/docs/hospital_acquired_infection.pdf. Accessed September 11, 2011.
Perl TM, Cullen JJ, Wenzel RP, Zimmerman MB, Pfaller MA, Sheppard D, Twombley J, French PP, Herwaldt LA. Mupirocin and the Risk of Staphylococcus aureus Study Team. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. N Engl J Med. 2002;346:1871–1877.
Schwarzkopf R, Takemoto RC, Immerman I, Slover JD, Bosco JA. Prevalence of Staphylococcus aureus colonization in orthopaedic surgeons and their patients: a prospective cohort controlled study. J Bone Joint Surg Am. 2010;92:1815–1819.
van Rijen M, Bonten M, Wenzel R, Kluytmans J. Mupirocin ointment for preventing Staphylococcus aureus infections in nasal carriers. Cochrane Database Syst Rev. 2008;4:CD006216.
Wenzel RP, Perl TM. The significance of nasal carriage of Staphylococcus aureus and the incidence of postoperative wound infection. J Hosp Infect. 1995;31:13–24.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351:1645–1654.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Hospital for Joint Diseases, NYU Langone Medical Center, New York, NY, USA.
About this article
Cite this article
Mehta, S., Hadley, S., Hutzler, L. et al. Impact of Preoperative MRSA Screening and Decolonization on Hospital-acquired MRSA Burden. Clin Orthop Relat Res 471, 2367–2371 (2013). https://doi.org/10.1007/s11999-013-2848-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-2848-3