Abstract
Background
Labral refixation rather than resection provides better pain relief and function after femoroacetabular impingement (FAI) surgery. When the labrum is absent, degenerated, or is irreparable, reconstruction may provide a favorable biomechanical environment for the hip. However, it is unclear whether labral reconstruction relieves pain and restores function.
Question/Purposes
In patients undergoing FAI surgery with concomitant labral reconstruction, (1) Do they note subjective improvement in pain at latest followup? (2) What is their postoperative activity level? (3) What are the complications, reoperation rates, and reasons for failure?
Methods
We retrospectively reviewed all 19 patients who underwent labral reconstruction in 20 hips at the time of surgical hip dislocation between August 2007 and February 2011. We assessed improvement in pain and function, complications, and subsequent surgery through a chart review and questionnaire. The minimum followup was 12 months (average, 26.4 months; range, 12–56 months).
Results
Three hips in three patients were converted to THA within 36 months of their surgical hip dislocation for continued preoperative pain. Of the 17 hips not undergoing THA, 15 reported subjective improvement in preoperative pain and function. The average UCLA score was 8.5 (range, 5–10). We observed no complications associated with the labral reconstruction itself.
Conclusion
The majority of patients with reconstructed acetabular labra reported improvement in their hip pain and function after surgery. The causes of persistent symptoms and conversion to THA remain uncertain. The data and conclusions of this study are limited secondary to lack of objective outcome measures.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) is a well-recognized prearthritic hip condition [9, 12, 16], which has gained increased attention over the last decade. FAI results from a structural abnormality within the hip that leads to contact between the femoral head-neck junction and the acetabulum, typically during flexion and internal rotation. Repetitive contact of this sort can lead to cartilage degeneration and labral pathology [1, 10]. FAI has been classified into two types based on the structural abnormality responsible: cam and pincer [1, 16]. Cam-type FAI is caused by an abnormally shaped proximal femur and femoral head, which abuts the acetabulum with activities and generates shear stress at the acetabular rim and causes outside-in avulsion of the cartilage from subchondral bone of the rim, usually anterosuperiorly. Labral tears in cam-type FAI often occur late and can be accompanied by avulsion of the articular cartilage from the labral base but the periphery of the labrum may be preserved [1, 16]. Pincer-type FAI, in contrast, is caused by a structural abnormality on the acetabular side of the hip. Most commonly, pincer-type FAI is caused by acetabular overcoverage in cases of coxa profunda or protrusio or may occur in patients performing repeated activities in which the hip is placed into extreme ROMs. Labral degeneration occurs early in the natural history of pincer-type FAI, and continued trauma leads to rim chondromalacia, cyst formation, and additional bony deposition along the acetabular rim usually worsening the degree of overcoverage [11].
Because the labrum is commonly involved in patients with FAI, there has been increased interest in the function of the acetabular labrum and its clinical relevance. Over the past 20 years, evidence has emerged suggesting the clinical and mechanical importance of the acetabular labrum. Ferguson et al. [6] investigated the material properties of the bovine acetabular labrum. They propose a mechanism for the seal effect the labrum creates and demonstrated the manner in which the labrum contributes to stability of the hip. Ferguson et al. [5] also characterized the seal effect of the acetabular labrum and its importance in maintaining intraarticular pressures and fluid film lubrication. Maintenance of negative intraarticular pressures and fluid film lubrication would minimize cartilage-cartilage contact, thereby minimizing wear. In their in vitro experiments, Crawford et al. [3] demonstrated the mechanical contribution of the labrum’s seal effect to hip stability. Using a three-dimensional motion analysis system and cadaveric specimens with intact, vented, and torn acetabular labra, they found 43% to 60% less force was required to distract the femur a standardized distance after venting or tearing of the labrum. From the biomechanical data available, it would seem reasonable to conclude that an intact labrum provides a biomechanical advantage to the hip and repair, reattachment, or reconstruction of the labrum may improve the biomechanics of the hip and may thereby slow the progression of arthritis.
Five clinical series to date reporting on the results of FAI surgery (four arthroscopic and one open) have shown the importance of labral preservation and noted that if the labrum is reattached as opposed to resected, patients have improved pain and function as determined by postoperative hip function scores [4, 7, 14, 15]. It would seem logical to consider based on these studies that reconstruction of the labrum may improve the mechanics of the hip and lead to better pain relief and function. We recently described a surgical technique for reconstructing the labrum in patients with degenerated or absent labrum using ligamentum teres capitis [20]. However, it is unclear whether labral reconstruction relieves pain and allows return to function.
We therefore determined in patients undergoing FAI surgery with concomitant labral reconstruction: (1) whether pain subjectively improved at latest followup; (2) whether postoperative activity level was enhanced; and (3) the complications, reoperation rates, rate of progression to THA, and reasons for failure.
Patients and Methods
One hundred fifty-five patients (178 hips) underwent surgical hip dislocation for FAI between August 2002 and February 2011. Beginning in 2007, two surgeons (RJS, RTT) began reconstructing the acetabular labrum using ligamentum teres capitis or fascia lata autograft in select patients undergoing open surgical hip dislocation. Inclusion criteria for this study population included age older than 15 years, having undergone open surgical hip dislocation and labral reconstruction, and a minimum of 1-year followup. This cohort consisted of 20 hips in 19 patients. Five hips were in five males and 15 hips in 14 females. Average patient age was 28.6 years (range, 16–50 years). Predominant pathology addressed was pincer type in 10 hips, cam type in five hips, and combined in five hips. All patients underwent surgical hip dislocation with femoroacetabular osteoplasty; three hips also underwent reverse periacetabular osteotomy. Outerbridge scores [17] were assigned based on intraoperative findings with a mean score of 1.4 (range, 0–4). No patients were lost to followup. Minimum followup was 12 months (average, 26.4 months; range, 12–56 months). Last followup was either at the clinic (four hips) or by telephone or mail questionnaire (16 hips). The minimum clinic followup was 2 months (average, 14.5 months; range, 2–45 months). Institutional review board approval was obtained before starting this review.
Standard preoperative workup included physical examination, AP pelvis and crosstable lateral hip radiographs, and in 16 of 20 hips, an MR arthrogram was performed to assess the labrum and articular cartilage. Indications for surgery were based on symptoms, positive impingement sign on physical examination [10], and radiographic findings consistent with either cam- or pincer-type impingement. The indications for labral reconstruction were largely based on review of imaging and intraoperative findings and included ossification or degeneration of the existing labrum to the extent that reattachment was not possible, absence of the labrum as a result of previous labral débridement, and global acetabular rim trimming, which resulted in insufficient residual labrum to seal the hip.
Ligamentum teres capitis (nine hips) and fascia lata (11 hips) autografts were used to reconstruct the acetabular labrum in 19 patients (20 hips) undergoing open surgical dislocation, and in some cases surgical hip dislocation and periacetabular osteotomy, for treatment of FAI. All patients underwent a surgical hip dislocation as described by Ganz et al. [8]. The surgical technique of digastric trochanteric osteotomy and dislocation proceeded as described but with special emphasis on preservation of as much ligamentum teres capitis as possible. The reconstruction of the acetabular labrum proceeded as described by Sierra and Trousdale [20]. As noted in their study, one limitation of reconstructing the labrum with ligamentum teres capitis is its relatively short length. To address this issue, in cases in which the ligamentum teres capitis was insufficient to reconstruct the area of damaged or absent labrum, fascia lata was harvested through the same incision for this purpose. Briefly, the graft tissue was harvested and cleaned of synovial tissue. Short but wide ligamentum teres capitis grafts were opened longitudinally to increase the length. The acetabular rim was trimmed back to a bleeding surface, and the graft was subsequently fixed in place using 2-mm suture anchors.
Postoperative care involved routine surgical hip dislocation rehabilitation consisting of limitation of flexion to 90° and limiting internal and external rotation for 4 weeks. Patients were maintained at toe-touch weightbearing for 4 weeks postoperatively in an effort to protect the osteotomy and then advanced to weightbearing as tolerated after that. ROM using a continuous passive motion machine to prevent adhesions and stiffness was used for 6 weeks and low-resistance exercise bike use began in Week 2.
The typical plan for postoperative patients involves followup visits at 2 months, 4 months, 12 months, and every year thereafter with a physical examination and radiographs. Given that this routine requires substantial travel for many patients, it is altered as needed to meet patient needs. As part of this study, telephone/questionnaire followup was attempted for all patients meeting inclusion criteria to provide the most up-to-date information possible; however, this is not part of the typical followup schedule. Postoperative radiographic imaging includes an AP pelvic radiograph and frog-leg and crosstable lateral radiographs. No further cross-sectional imaging is performed except in cases with continued pain if clinically indicated. All patients had preoperative and postoperative radiographs available, and the minimum postoperative radiographic followup was 2 months (mean, 13.8 months; range, 2–45 months).
For the purpose of this review, telephone followup was conducted by an author (JAW) and consisted of a standardized series of questions assessing pain and function (Appendix A). Patients were asked whether they had pain and, if so, were asked to describe its location, severity (mild, moderate, severe), and frequency (constant, daily, occasional, rarely, with strenuous activity only). Participants were also asked to rate their hip now compared with before surgery (1–5; 1 = much worse, 2= worse, 3 = the same, 4 = better, 5 = much better). The UCLA activity score [1] was assessed in all hips. UCLA activity score ranges from 1 to 10: 1 = wholly inactive to 10 = regularly participate in impact sports. Additional surgery or progression to THA was noted. The UCLA activity scores and hip pain findings were excluded from further analysis in those patients undergoing THA. For patients not successfully contacted by phone or questionnaire, responses to questions asking patients to compare their hip with before surgery and to indicate whether they would undergo the procedure again (Appendix A, questions 6 and 7) were unavailable for analysis; these are noted in the subsequent data tables.
Results
Of the 16 patients (17 hips) who did not proceed to THA, all except two hips in two patients noticed symptomatic improvement (Table 1). Patients reported subjective pain reduction in 14 hips compared with before surgery or were pain-free at last clinical followup, one patient reported mild pain in one hip at last followup, and two hips were rated as the same. Some degree of pain was reported in 11 of 17 hips not having undergone THA. Two patients reported constant pain in two hips, daily pain occurred in four hips, occasional pain in two hips, rare pain in three hips, and pain only with high activity levels in one hip. Of these hips in patients who continued to experience pain, six rated their pain as mild, six rated their pain as moderate, and none rated their pain as severe when present. Pain localized to the groin in only six hips and to the lateral aspect of the proximal thigh (greater trochanter) in eight hips (locations not mutually exclusive).
The average UCLA score [1] at latest followup was 8.5 (range, 5–10) in 16 patients (17 hips) in those not having undergone THA (Table 1). Eight patients achieved a UCLA activity score of 10 of 10 after surgical hip dislocation and labral reconstruction. Only five of 17 patients not progressing to THA failed to achieve a UCLA score of 8 or greater after FAI surgery with labral reconstruction.
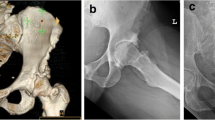
There were no complications associated with the labral reconstruction itself. Nineteen additional operations were performed on 13 hips in 13 patients (Table 2). Routine removal of hardware was performed in 12 hips. Two patients (two hips) underwent lysis of adhesions between the anterior capsule and femoral head-neck junction and one hip underwent an iliopsoas release for persistent pain (later THA). Three hips in three patients progressed to THA during the course of this study. In two of three hips that progressed to THA, substantial degenerative changes were noted during surgical hip dislocation (Table 2). In the third patient who progressed to THA, the articular cartilage appeared nearly normal, but the patient had previously undergone two arthroscopic procedures with labral resection with no improvement in symptoms. One additional patient underwent hip arthroscopy for continued hip pain (Fig. 1). In two of the patients who underwent THA (Fig. 2) and in the patient who underwent hip arthroscopy (Fig. 1), the labral grafts were healed to the rim of the acetabulum, were grossly viable (stable to probing, healed to acetabular rim), and seemingly functioning as a pseudolabrum. No complications were seen related to the reconstruction itself.
Discussion
In patients with FAI, the acetabular labrum is affected either early or late in the disease process. In cases in which the labrum has been previously resected, is deficient, ossified, or irreparably torn, reconstruction of the labrum with autogenous tissue may be warranted. This study sought to investigate patients undergoing FAI surgery with labral reconstruction to determine the subjective improvement in pain they experienced, the level of activity they attain postoperatively, and to determine the complications and reoperation rates including conversion to THA.
Our study is limited in several ways. First, we report on a limited patient population, and followup was short as a result of the relatively recent development of the surgical technique used. The short followup interval and relatively small patient population limit our ability to determine factors predictive for failure (or success). Second, although our patient-reported postoperative pain scores seem similar to those described in the literature for open surgical hip dislocation to address FAI [2, 4], they are descriptive data rather than statistical and are not compared with any control group. Third, the clinical benefits noticed by the subjects of this study are likely related to the correction of the underlying structural abnormality of the hip rather than the labral reconstruction performed. It is difficult to discern how much of any benefit arises from the reconstruction alone. Finally, this study reports preliminary, subjective pain relief findings, complications, and function scores after surgery; it is limited by the lack of both preoperative and postoperative objective outcome measures. Despite these limitations, early reporting of short-term data for new procedures is prudent to publicly evaluate and discuss the role of such procedures in clinical practice and to refine their technique to maximize the benefits conferred to the patient.
Subjective improvement in symptoms was seen in 15 of 20 hips, whereas three progressed to THA and two patients (two hips) felt their symptoms were similar to preoperatively. Six hips in six patients continued to have pain on a daily or constant basis. None of these have had progression of symptoms, and of those six patients, four rated their hip as better or much better compared with their preoperative status at latest followup. Therefore, although many patients reported continued pain, the majority of these also noted subjective improvement from their preoperative pain level. Our findings are in line with what has been published previously but cannot be compared directly because we did not obtain Harris hip scores in our patients. Harris hip scores in this patient population may not be the most appropriate way to measure pain relief or function noted by the discrepancies among continued subjective pain, reported symptom improvement, and objective function. That said, Espinosa et al. [4] demonstrated better clinical success in patients who underwent open surgical hip dislocation with labral repair compared with those undergoing labral excision, findings supported in hips undergoing arthroscopic FAI surgery [14, 15, 18, 19]. The symptomatic improvement noted in our data supports these findings, because our patient-reported postoperative pain and function are similar to those reported in the groups of patients undergoing reattachment rather than resection.
The present study cohort achieved an average postoperative UCLA score of 8.5. Viewed alongside the pain findings at last followup, these scores demonstrate the difficulty of defining clinical success or improvement in FAI surgery. Many patients (11 of 17 not progressing to THA) reported continued pain in or about the operative hip, yet only three of those 11 were had postoperative UCLA scores below 8 with none below 5. Two patients indicated they would not undergo such an operation again: one noted subjective improvement in their hip pain and one noted no change, yet they achieved postoperative UCLA scores of 8 and 10. These apparent contradictions complicate the assessment of clinical success or failure. Preoperative UCLA scores were not available for patients in this cohort, so functional gains after surgery cannot be assessed; however, it is encouraging that the vast majority of patients undergoing FAI surgery with labral reconstruction are able to achieve a high level of function postoperatively. The relatively high UCLA scores after FAI surgery with labral reconstruction seem to mirror the improvement in Harris hip scores noted in several studies on arthroscopic [14, 15, 18, 19] and open FAI surgery [5], although these cannot be compared directly.
We observed a low rate of complications in this series of surgical hip dislocations. The complications associated with surgical hip dislocation have been previously reported in the literature [13, 21]. There was no deleterious effect associated with labral reconstruction itself, and we are unaware of studies reporting deleterious effects of sacrifice of the ligamentum teres capitis or sections of fascia lata and identified none in our patients. In three reoperations, we had the opportunity to evaluate the gross anatomic appearance of our labral reconstruction with formation of what seemed to be a pseudolabrum. Although we have evidence from several patients that the labral reconstructions healed as intended to the acetabular rim, we do not have evidence to suggest whether the labral graft had the intended sealing effect on the joint. Adhesions in between the femoral head and neck junction and the capsule have been reported. In this series, two patients required lysis of adhesions and cannot be attributed solely to the labral reconstruction itself. We now routinely use a continuous passive motion machine in all patients after surgical hip dislocation to minimize this complication. We remove almost all hardware routinely at 3 to 6 months from surgery because symptomatic hardware is not uncommonly seen; thus, the reoperation rate in this cohort is understandably high (13 of 20 hips [65%]). The relatively low rate of progression to THA (three of 20 hips [15%]) is comparable to other series discussing FAI surgery [3].
In conclusion, the data presented here are consistent with the improvement in pain and Harris hip scores seen in the literature on the surgical treatment of FAI [2, 4, 14, 15, 18, 19], including the subjective improvement in pain in 15 of 20 hips (15 of 17 not undergoing THA) and high postoperative UCLA activity scores (average, 8.5; range, 5–10). Our complications were also similar to those previously reported [13, 21], and no complications were directly related to the reconstruction itself. The relatively low rate of progression to THA noticed in this series is consistent with that reported elsewhere in the literature [3]. Further clinical studies reporting the long-term pain and function improvement and rate of conversion to THA in patients undergoing labral reconstruction as well as those comparing such data with the long-term pain and function improvement and rate of conversion to THA in patients undergoing labral resection are needed. Additionally, biomechanical and animal studies focusing on labral reconstruction would help determine the role of the reconstructed labrum. With the available data, labral reconstruction during open surgery to address FAI appears to be a reasonable surgical alternative, although further investigation is required.
References
Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018.
Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 2010;468:555–564.
Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, Vega CE, Patel RV, Miller AR, McCarthy JC, Lowe WR, Noble PC. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22.
Espinosa N, Beck M, Rothenfluh DA, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am. 2007;89(Suppl 2):36–53.
Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178.
Ferguson SJ, Bryant JT, Ito K. The material properties of the bovine acetabular labrum. J Orthop Res. 2001;19:887–896.
Fujii M, Nakashima Y, Noguchi Y, Yamamoto T, Mawatari T, Motomura G, Iwamoto Y. Effect of intra-articular lesions on the outcome of periacetabular osteotomy in patients with symptomatic hip dysplasia. J Bone Joint Surg Br. 2011;93:1449–1456.
Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124.
Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272.
Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120.
Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;429:262–271.
Ito K, Minka MA 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176.
Krueger A, Leunig M, Sibenrock KA, Beck M. Hip arthroscopy after previous surgical hip dislocation for femoroacetabular impingement. Arthroscopy. 2007;23:1285–89.
Larson CM, Giveans MR. Arthroscopic débridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376.
Larson CM, Giveans MR, Stone RM. Arthroscopic débridement versus refixation of hte acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021.
Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66.
Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43B:752–757.
Philippon MJ, Briggs KK, yen TM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction; minimum two year follow-up. J Bone Joint Surg Br. 2009;91:16–23.
Schilders E, Dimitrakopoulou A, Bismil Q, Marchant P, Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement: a comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg Br. 2011;93:1027–1032.
Sierra RJ, Trousdale RT. Labral reconstruction using the ligamentum teres capitis: report of a new technique. Clin Orthop Relat Res. 2009;467:753–759.
Sink EL, Beaule PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011;93:1132–1136.
Acknowledgments
We thank Gregory Boone of Mayo Medical School for his help with this article and Donna Riemersma in the Orthopedic Department Manuscript Office for her help in the submission of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors receives funding from Biomet Orthopedics (Warsaw, IN, USA) (RJS) and DePuy Orthopaedics (Warsaw, IN, USA), Wright Medical (Arlington, TN, USA), Mako Surgical (Fort Lauderdale, FL, USA), and Ortho Development Corp. (Draper, UT, USA) (RTT).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Appendix A. Study questions
Appendix A. Study questions
You recently underwent an open surgical hip dislocation with reconstruction of your acetabular labrum with either ligamentum teres capitus or fascia lata autograft.
-
1.
Do you currently have pain in your operative hip?
If NO: Skip to Question #6
If YES: Continue to Question #2?
-
2.
How often do you have pain in the operative hip? (constant, daily, occasionally, with activity, rarely)
-
3.
How would you describe your pain? (deep, shallow, dull, sharp, electric, burning)
-
4.
How severe is your pain (mild, moderate, severe)?
-
5.
Would you say your pain is more frequently deep, in your groin, or on the side of your hip?
-
6.
How is your hip compared with before surgery? (much better, better, the same, worse, much worse)
-
7.
If you could make the decision again–given how you feel now, and what you know about the recovery from surgery—would you decide to undergo the procedure again?
-
8.
Now, I will ask you about your current activity level. I will read several choices that may describe your current activity level; please tell me which one best describes your current activity level. (See attached UCLA activity score.)
About this article
Cite this article
Walker, J.A., Pagnotto, M., Trousdale, R.T. et al. Preliminary Pain and Function After Labral Reconstruction During Femoroacetabular Impingement Surgery. Clin Orthop Relat Res 470, 3414–3420 (2012). https://doi.org/10.1007/s11999-012-2506-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2506-1