Abstract
Background
Gender-specific differences in knee and hip anatomy have been well documented. Although it has been accepted these differences exist, there is controversy regarding if and how these differences should be addressed with gender-specific implant designs.
Questions/purposes
(1) What are the anatomic and morphologic differences, if any, in the knee and hip between men and women? (2) Do gender-specific TKA designs provide better clinical functioning, survivorship, and improved fit in women? (3) How have anatomic differences in the hip been addressed, if at all, by THA?
Methods
We conducted a systematic review of the MEDLINE database to identify all articles reviewing basic science and clinical outcomes of gender-specific total knee and total hip implants. From these, we reviewed 253 studies.
Results
The anatomic studies elucidated multiple differences in the anatomy of knees and hips between men and women. All reviewed studies report similar clinical function and satisfaction scores between men and women for gender-specific TKA and no improvement in these scores when comparing gender-specific TKA to unisex TKA. Current modularity in THA appears to accommodate any anatomic differences in the hip.
Conclusions
Based on the available literature, there is no difference in the outcome of patients with a gender-specific knee arthroplasty versus a unisex arthroplasty. It does not appear gender-specific THAs would provide any benefit over current systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With more than 200,000 primary THAs and 400,000 primary TKAs performed annually, a number expected to increase up to fivefold by the year 2030, there is a large and growing population of patients who will have these procedures performed [34]. Recent studies have attempted to summarize the causes and epidemiology of revision procedures [5, 6, 39] and what can be done to minimize clinical and radiographic failures [34, 35]. One aspect where surgeons and patients may differ, however, lies in the difference between a patient’s and surgeon’s definition of a successful procedure. Two reports have suggested nearly 40% of patients believe their expectations had not been fully met by their total joint arthroplasty [8, 44].
Many surgeons have attempted to improve postoperative function and to provide a more accurate restoration of preoperative, and even predisease, anatomy. Related to those attempts, various studies have described anatomic differences in the hips and knees of men and women, including altered aspect ratios in the distal femur and proximal femur [4, 18, 24, 41], differences in Q angles [1, 19, 50], trochlear groove dimensions [40], and femoral neck and head morphology [38, 42, 51]. This work led to some orthopaedic device manufacturers developing “gender-specific” total knee prostheses in an attempt to provide more options for the surgeon and patient (such as incorporating more sizes, differing aspect ratios, altered trochlear grooves, and other features). Additionally, as a greater understanding of the variability of hip and knee anatomy has been attained [2, 9, 40, 49], implants have been redesigned with more modularity in their systems.
We performed a systematic review of the literature to answer the following questions: (1) What are the anatomic differences, if any, in the knee and hip between men and women? (2) Do gender-specific TKA designs provide better functional survivorship, clinical outcomes, and improved fit in women? (3) How have anatomic differences in the hip been addressed, if at all, by THA?
Materials and Methods
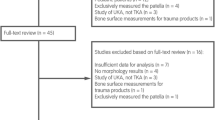
A query of the PubMed database was performed to find any relevant studies addressing either gender-specific total joint arthroplasty (knee or hip) or addressing anatomic differences between men and women. The following search string was used to perform this query: “(((hip[title] or knee[title]) and (arthroplasty[title] or replacement[title])) and (gender[title] or female[title] or sex[title])) OR ((hip[title] or knee[title]) and (gender[title] or female[title] or sex[title])) NOT fracture NOT athlete.” This search yielded 253 studies. Reports were excluded based on the following criteria: (1) articles not in English; (2) any articles that did not pertain to the adult hip, knee, or the arthroplasty of either; and (3) studies pertaining to outcomes after revision knee or hip arthroplasty. We excluded 169 studies based on these criteria, leaving 96 reports (Fig. 1). There were 14 additional reports added from the reference lists of these articles, giving a total of 110 reports. It should be noted, throughout this manuscript, the term “gender” is used to refer to both “sex” (as determined by chromosomal type) and “gender” (as determined by societal and cultural conventions). As such, there may be overlap in specific outcome based on sex and gender, and in general, the term “gender” will be used throughout to refer to both.
The manuscripts were screened to assess the following information: (1) What are the reported anatomic differences in knees and hips between men and women? (2) How does gender affect survivorship and clinical functioning after undergoing gender-specific TKA? (3) How does gender affect outcomes in THA that could necessitate the further allocation of resources to the development of gender-specific THA? Further, studies were excluded that limited patient inclusion based on diagnosis (other than osteoarthritis), focused specifically on physical rehabilitation after total joint arthroplasty, had a minimum followup of less than 2 years, reported on the same patient cohort as another study, had duplicate MEDLINE records, reported on non-gender-specific TKA, or were an opinion or review article. All manuscripts meeting these criteria were grouped according to the above questions, and the following data were extracted to a spreadsheet for each: the type of study, the number of joints and patients studied, the specific anatomic and morphologic differences noted between genders (eg, distal femoral aspect ratio, Q angle, femoral neck morphology, etc), clinical outcomes reported on (eg, Knee Society scores, Hip Society scores, WOMAC, etc), implant or radiographic survivorship, any treatment disparities, and any differences in patients’ predisposition to undergo arthroplasty or perception of the success of their arthroplasty. One author (AJJ) reviewed all studies to determine whether or not they met these criteria. If there was any question as to the relevance of a study, a consensus was reached among all three authors (AJJ, CRC, MAM).
Upon reviewing the screened literature, 29 reports met these criteria. There were 20 reports on the anatomic differences in the hip or knee between men and women [4, 7, 11, 12, 14, 15, 17–19, 22–24, 26, 30, 37, 38, 42, 47, 50, 51]. Of these 20 reports, there were 15 focusing on the knee and five focusing on the hip (Table 1). There were four reports specifically on clinical outcomes after gender-specific TKA [10, 31, 32, 45] (two of which had a prospective, randomized design [31, 32]), and one additional study assessing whether women received benefit from expanded prosthesis sizes [16]. Four studies reported on the effect of gender and modularity on clinical outcomes in THA [25, 33, 36, 46].
The quality of the two Level I studies was assessed by all authors (AJJ, MAM, CRC), with discrepancies resolved by discussion and consensus. The following parameters were evaluated and given a value of done, not done, or unclear: randomization, allocation, concealment, and blinding (participants, assessors, analysts). Additional factors (baseline demographic comparability of groups and followup period) were evaluated as adequate, inadequate, or unclear (Table 2). A failure to properly blind participants, assessors, and analysts was the most common deficiency.
Results
The reported anatomic differences between the knees of men and women were found in the following areas: bone size [24], distal femoral aspect ratio [4, 24], tibial aspect ratio [24], anterior condylar height of the distal femur [18, 41], patellar dimensions, Q angle [1, 19, 50], rotation of the trochlear groove [41], and contact surface area of the patella [11] (Table 3). One study [12] of 60 human cadaver knees (from 16 male and 25 female donors) reported no difference in anatomy, including distal femoral aspect ratio. There were also reports suggesting body type morphology played a role in the anatomic structure of the knee, and this may be in addition to differences based solely on gender [3]. Four studies reported increased rates of cartilage loss in women [13, 15, 17, 21], one study reported an increasing incidence of osteophytes in women, compared to men, older than 60 years [23], and another study reported increased varus/valgus laxity in women [47]. There were several anatomic differences found between hips of men and women in the literature reviewed, including bone size [7, 30, 38], femoral offset [38, 51], proximal femoral shape [42, 51], and trabecular patterns [51].
Four studies clinically or radiographically addressed gender-specific TKA and one study reviewed TKAs that had an increased number of smaller size options available that were not specifically marketed as “gender-specific.” Two Level I studies by Kim et al. [31, 32] each reported on a separate cohort of female patients in Korea who underwent bilateral TKA. There was a total of 446 TKAs performed in 223 patients. The patients were randomized to determine which knee was to receive either a gender-specific implant or a unisex implant. The authors found no difference (in either study) in Knee Society, WOMAC, ROM, or satisfaction scores. They also concluded the gender-specific implants did not fit better than standard implants (131 standard implants had a fit described as “good,” compared to only 29 gender-specific implants). A study by Clarke and Hentz [10] radiographically compared three cohorts: a group of women (42 knees, 42 women) who had unisex TKAs, a group of men (41 knees, 41 men) who had unisex TKAs, and a group of women (39 knees, 39 women) who had gender-specific TKAs. The authors concluded women in both groups had higher rates of medial or lateral overhang of the femoral component. The study by Emerson and Martinez [16] compared a group of 183 patients (90 women, 93 men) who had four sizing options available at the time of surgery to a group of 212 patients (106 women, 106 men) who had an additional three smaller sizes available and found in the group that had smaller sizes available 56 women and 19 men had improved implant fit with one of the smaller sizes. Early Knee Society scores and ROMs (6-month followup visit) were similar among all groups.
There were five studies that specifically compared THAs on the basis of gender. Kostamo et al. [33] reviewed clinical outcomes in 4114 primary THAs performed in 3461 patients, 1924 of whom were women. At a mean followup of greater than 11 years (range, 2–27 years), the Kaplan-Meier revision rate was similar (p = 0.14) in women and men: 8.3% versus 9.3%, respectively. Another study, by Traina et al. [46], reviewed the use of 1050 modular stemmed THAs in men and 1080 in women. They found no difference in the 11-year survivorship (96.0% in women compared to 97.6% in men) or dislocation rates (0.9% in women compared to 0.5% in men). A shorter neck was used more frequently in women than in men (796 and 541 times, respectively). Lavernia et al. [36] reported on 532 patients (658 hips), consisting of 316 women and 216 men. Of note was a decreased perceived function (as measured by Quality of Well-Being and SF-36 Physical Function and Bodily Pain scores) in the women starting at 6 to 7 years after THA. This was similar to the findings in a group of 1120 patients (432 men, 688 women) reported on by Holtzman et al. [25] who underwent THA. Using functional status, pain levels, and the ability to perform activities of daily living as metrics, the authors concluded women had less functional ability at the time of THA and did not do as well at 1-year followup when compared with men.
Discussion
Despite high clinical survivorship after TKA and THA, controversy has remained in the literature regarding whether gender-specific TKA provides superior results over unisex TKA and whether gender-specific arthroplasties are needed in general. Although there are well-documented anatomic differences between the genders, it is uncertain whether a “gender-specific” total joint arthroplasty is the appropriate solution to these differences. Therefore, we evaluated what has been published regarding differences between the genders to answer the following questions: (1) What are the reported anatomic differences in knees between men and women? (2) How does gender affect survivorship and clinical outcomes after undergoing gender-specific TKA? (3) How have anatomic differences in the hip been addressed, if at all, by THA?
The major limitation of this report was the limited information in the literature regarding the ability of gender-specific total joint arthroplasty to correctly restore female joint anatomy while improving clinical functionality and improving survivorship. While there are a few studies assessing clinical outcomes of gender-specific TKA [10, 31, 32, 45], albeit at short followup periods, there are even fewer reports on the results of gender-specific THA [33, 46]. This is more of a failure of the surgeons and manufacturers who advocate the need for gender-specific knee designs to conduct large-scale prospective trials to compare these outcomes. A second major limitation is the absence of long-term followup of any studies relating to gender-specific implants. Although short-term studies can adequately assess and compare the initial pain and functional scores, as well as radiographic fit, it is not possible to provide any quantitative evidence on the durability and longevity of one type of implant over another. We do believe conclusions can be drawn from these studies, as well as the anatomic studies comparing the difference in knee anatomy between patients of different gender, height, or body morphology.
Although there are some anatomic differences found between men and women, upon review of the literature, these assumptions may not hold true in all patients, as some men may have femoral or tibial anatomy more closely resembling that of a woman and vice versa. For example, in several reports, the Q angle has long been purported to be different between men and women [1, 20, 26, 27, 50]. However, a recent study by Grelsamer et al. [19] suggested this was a misconception propagated through the literature because some early reports failed to incorporate subject height into the analysis of Q angle. Upon further comparison, it was found Q angle is more directly associated with patient height than gender [19]. Another study by Bellemans et al. [3] analyzed the distal femoral and tibial anatomy of 1000 individuals of white European descent and found, in addition to having anatomy that varied by gender, body morphology (ie, endomorph, mesomorph, ectomorph) played a major role in the determination of the anatomic characteristics of the knee. However, despite these differences by body morphology, a majority (98%) of the smallest knees were in women, while 81% of the largest knees came from men. This indicates, although a gender-specific knee might be beneficial to some women, there might still be a percentage of women who are not appropriately treated with a TKA, as they might have femoral or tibial anatomy more closely resembling that of a man.
In an attempt to localize where gender-neutral knee implants may cause problems to the patient resulting in postoperative pain, Mahoney and Kinsey [37] intraoperatively measured the overhang of the femoral component, using 10 specific zones, in 437 TKAs. They found nearly two-thirds of the implants in women had overhang in at least one zone and calculated an attributable risk percent implying 39% of postoperative pain was directly related to this femoral component overhang. Therefore, based on the results of that study, better results for women might be achieved by implanting components with more appropriate aspect ratios. Manufacturing companies might not need to promote “gender-specific” knee prostheses but rather focus more on increased modularity to allow the surgeon to select more custom-sized components to allow for any individual’s unique anatomy (based on distal femoral and tibial aspect ratios, patella size, and Q angle).
While there has been a study suggesting women may have more difficulty returning to a higher functional status after THA [29], another study determined, in the Medicare population, women have greater disability at the time of surgery than men, which leads to the argument, if women do, in fact, perform worse after THA, it is because they have later progression of disease at the time of presentation than men [28]. Much as with the anatomy of the knee, several forensic analyses have suggested there are anatomic differences in hips between the genders [38, 42, 43, 48, 51]. These include bone size, femoral offset, proximal femoral shape, bone mineral content, and trabecular patterns. However, despite these differences, the only study specifically addressing the question of gender and its effect on THA reported women had higher survivorship than men, and there was no difference in the improvement in clinical outcome scores (Harris hip score, SF-12) between men and women, despite men having higher functional scores than women [33]. The study by Traina et al. [46] noted women required, on average, shorter necks, possibly implicating current modular THA systems may already adequately address the differences in hip anatomy between men and women. This review did not specifically address modular hip components and whether smaller component sizes were typically used in women so it is difficult to draw this conclusion. However, it would seem logical the anatomic differences can be accommodated with the modularity of THA components.
To return to the original question posed by the title of this report (do we need gender-specific total joint arthroplasty?), although the scientific evidence suggests there may be anatomic differences in knees between the genders, it appears these differences may be more multifactorial than just based on gender. Body morphology, height, gender, and bone size all contribute to an individual’s unique bone dimensions. Although we acknowledge there are some anatomic difference in the shape of the knee between men and women, no benefit from gender-specific TKAs has been shown in early clinical reports. The published experience with hip arthroplasty systems with increased proximal modularity has not shown a difference in results between men and women, and we do not believe gender-specific THAs would provide any new benefit over these current prostheses. We emphasize long-term, prospective randomized studies will be required for both hips and knees to answer these questions.
References
Aglietti P, Insall JN, Cerulli G. Patellar pain and incongruence. I. Measurements of incongruence. Clin Orthop Relat Res. 1983;176:217–224.
Bachmann HS, Hanenkamp S, Kornacki B, Frey UH, Bau M, Siffert W, Wedemeyer C. Gender-dependent association of the GNAS1 T393C polymorphism with early aseptic loosening after total hip arthroplasty. J Orthop Res. 2008;26:1562–1568.
Bellemans J, Carpentier K, Vandenneucker H, Vanlauwe J, Victor J. The John Insall Award. Both morphotype and gender influence the shape of the knee in patients undergoing TKA. Clin Orthop Relat Res. 2010;468:29–36.
Blaha JD, Mancinelli CA, Overgaard KA. Failure of sex to predict the size and shape of the knee. J Bone Joint Surg Am. 2009;91(Suppl 6):19–22.
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133.
Bozic KJ, Ong K, Lau E, Kurtz SM, Vail TP, Rubash HE, Berry DJ. Risk of complication and revision total hip arthroplasty among Medicare patients with different bearing surfaces. Clin Orthop Relat Res. 2010;468:2357–2362.
Brinckmann P, Hoefert H, Jongen HT. Sex differences in the skeletal geometry of the human pelvis and hip joint. J Biomech. 1981;14:427–430.
Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16:740–747.
Chang HJ, Mehta PS, Rosenberg A, Scrimshaw SC. Concerns of patients actively contemplating total knee replacement: differences by race and gender. Arthritis Rheum. 2004;51:117–123.
Clarke HD, Hentz JG. Restoration of femoral anatomy in TKA with unisex and gender-specific components. Clin Orthop Relat Res. 2008;466:2711–2716.
Csintalan RP, Schulz MM, Woo J, McMahon PJ, Lee TQ. Gender differences in patellofemoral joint biomechanics. Clin Orthop Relat Res. 2002;402:260–269.
Dargel J, Michael JW, Feiser J, Ivo R, Koebke J. Human knee joint anatomy revisited: morphometry in the light of sex-specific total knee arthroplasty. J Arthroplasty. 2010 March 3 [Epub ahead of print].
Ding C, Cicuttini F, Blizzard L, Scott F, Jones G. A longitudinal study of the effect of sex and age on rate of change in knee cartilage volume in adults. Rheumatology (Oxford). 2007;46:273–279.
Ding C, Cicuttini F, Scott F, Glisson M, Jones G. Sex differences in knee cartilage volume in adults: role of body and bone size, age and physical activity. Rheumatology (Oxford). 2003;42:1317–1323.
Eckstein F, Siedek V, Glaser C, Al-Ali D, Englmeier KH, Reiser M, Graichen H. Correlation and sex differences between ankle and knee cartilage morphology determined by quantitative magnetic resonance imaging. Ann Rheum Dis. 2004;63:1490–1495.
Emerson RH Jr, Martinez J. Men versus women: does size matter in total knee arthroplasty? Clin Orthop Relat Res. 2008;466:2706–2710.
Faber SC, Eckstein F, Lukasz S, Muhlbauer R, Hohe J, Englmeier KH, Reiser M. Gender differences in knee joint cartilage thickness, volume and articular surface areas: assessment with quantitative three-dimensional MR imaging. Skeletal Radiol. 2001;30:144–150.
Fehring TK, Odum SM, Hughes J, Springer BD, Beaver WB Jr. Differences between the sexes in the anatomy of the anterior condyle of the knee. J Bone Joint Surg Am. 2009;91:2335–2341.
Grelsamer RP, Dubey A, Weinstein CH. Men and women have similar Q angles: a clinical and trigonometric evaluation. J Bone Joint Surg Br. 2005;87:1498–1501.
Guerra JP, Arnold MJ, Gajdosik RL. Q angle: effects of isometric quadriceps contraction and body position. J Orthop Sports Phys Ther. 1994;19:200–204.
Hanna FS, Bell RJ, Cicuttini FM, Davison SL, Wluka AE, Davis SR. The relationship between endogenous testosterone, preandrogens, and sex hormone binding globulin and knee joint structure in women at midlife. Semin Arthritis Rheum. 2007;37:56–62.
Hanna FS, Teichtahl AJ, Wluka AE, Wang Y, Urquhart DM, English DR, Giles GG, Cicuttini FM. Women have increased rates of cartilage loss and progression of cartilage defects at the knee than men: a gender study of adults without clinical knee osteoarthritis. Menopause. 2009;16:666–670.
Hernborg J, Nilsson BE. Age and sex incidence of osteophytes in the knee joint. Acta Orthop Scand. 1973;44:66–68.
Hitt K, Shurman JR 2nd, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003;85(Suppl 4):115–122.
Holtzman J, Saleh K, Kane R. Gender differences in functional status and pain in a Medicare population undergoing elective total hip arthroplasty. Med Care. 2002;40:461–470.
Horton MG, Hall TL. Quadriceps femoris muscle angle: normal values and relationships with gender and selected skeletal measures. Phys Ther. 1989;69:897–901.
Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227.
Karlson EW, Daltroy LH, Liang MH, Eaton HE, Katz JN. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med. 1997;102:524–530.
Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD. Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplasty. 2006;21:559–566.
Kersnic B, Iglic A, Kralj-Iglic V, Jaklic A, Srakar F, Pernus F, Antolic V. Determination of the femoral and pelvic geometrical parameters that are important for the hip joint contact stress: differences between female and male. Pflugers Arch. 1996;431(6 Suppl 2):R207–R208.
Kim YH, Choi Y, Kim JS. Comparison of a standard and a gender-specific posterior cruciate-substituting high-flexion knee prosthesis: a prospective, randomized, short-term outcome study. J Bone Joint Surg Am. 2010;92:1911–1920.
Kim YH, Choi Y, Kim JS. Comparison of standard and gender-specific posterior-cruciate-retaining high-flexion total knee replacements: a prospective, randomised study. J Bone Joint Surg Br. 2010;92:639–645.
Kostamo T, Bourne RB, Whittaker JP, McCalden RW, MacDonald SJ. No difference in gender-specific hip replacement outcomes. Clin Orthop Relat Res. 2009;467:135–140.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009;24:195–203.
Lavernia CJ, Alcerro JC, Contreras JS, Rossi MD. Patient Perceived Outcomes After Primary Hip Arthroplasty: Does Gender Matter? Clin Orthop Relat Res. 2010 August 11 [Epub ahead of print].
Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010;92:1115–1121.
Mall G, Graw M, Gehring K, Hubig M. Determination of sex from femora. Forensic Sci Int. 2000;113:315–321.
Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010;468:3070–3076.
Petterson SC, Raisis L, Bodenstab A, Snyder-Mackler L. Disease-specific gender differences among total knee arthroplasty candidates. J Bone Joint Surg Am. 2007;89:2327–2333.
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:35–46.
Purkait R. Sex determination from femoral head measurements: a new approach. Leg Med (Tokyo). 2003;5(Suppl 1):S347–S350.
Purkait R. Triangle identified at the proximal end of femur: a new sex determinant. Forensic Sci Int. 2005;147:135–139.
Suda AJ, Seeger JB, Bitsch RG, Krueger M, Clarius M. Are patients’ expectations of hip and knee arthroplasty fulfilled? A prospective study of 130 patients. Orthopedics. 2010;33:76–80.
Tanavalee A, Rojpornpradit T, Khumrak S, Ngarmukos S. The early results of gender-specific total knee arthroplasty in Thai patients. Knee. 2010 October 30 [Epub ahead of print].
Traina F, De Clerico M, Biondi F, Pilla F, Tassinari E, Toni A. Sex differences in hip morphology: is stem modularity effective for total hip replacement? J Bone Joint Surg Am. 2009;91(Suppl 6):121–128.
van der Esch M, Steultjens MP, Lems WF, Dekker J. Gender difference in varus-valgus laxity in osteoarthritis of the knee. Scand J Rheumatol. 2007;36:157–159.
Wheatley BP. An evaluation of sex and body weight determination from the proximal femur using DXA technology and its potential for forensic anthropology. Forensic Sci Int. 2005;147:141–145.
Whittle J, Steinberg EP, Anderson GF, Herbert R, Hochberg MC. Mortality after elective total hip arthroplasty in elderly Americans: age, gender, and indication for surgery predict survival. Clin Orthop Relat Res. 1993;295:119–126.
Woodland LH, Francis RS. Parameters and comparisons of the quadriceps angle of college-aged men and women in the supine and standing positions. Am J Sports Med. 1992;20:208–211.
Yates LB, Karasik D, Beck TJ, Cupples LA, Kiel DP. Hip structural geometry in old and old-old age: similarities and differences between men and women. Bone. 2007;41:722–732.
Author information
Authors and Affiliations
Corresponding author
Additional information
MAM is a consultant for Stryker Orthopaedics (Mahwah, NJ) and Wright Medical Technologies Inc (Arlington, TN) and receives royalties from Stryker Orthopaedics. The remaining authors have no disclosures to make. No external funding was received specifically in support of this work.
About this article
Cite this article
Johnson, A.J., Costa, C.R. & Mont, M.A. Do We Need Gender-specific Total Joint Arthroplasty?. Clin Orthop Relat Res 469, 1852–1858 (2011). https://doi.org/10.1007/s11999-011-1769-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-1769-2