Abstract
The main goals of TKA are pain relief and improvement of function and range of motion (ROM). To ascertain whether TKA in patients with stiff knees would relieve pain and improve functional outcome and ROM, we asked four questions: whether (1) Knee Society and WOMAC scores would improve after TKA; (2) poor preoperative ROM would improve after TKA; (3) the revision rate of TKA in stiff knees would be high; and (4) complication rates would be high in these patients after TKA. We retrospectively reviewed 74 patients (86 knees) with stiff knees (mean age, 56.8 years) who underwent TKAs with a condylar constrained or a posterior stabilized prosthesis. The minimum followup was 5 years (mean, 9.1 years; range, 5–12 years). The mean preoperative Hospital for Special Surgery knee score and Knee Society knee and functional scores were 42, 11, and 42 points, respectively, and postoperatively they were 84, 90, and 84 points, respectively. Preoperative and postoperative total WOMAC scores were 73 and 34 points, respectively. One knee (1.2%) had aseptic loosening of the tibial component and 12 knees (14%) had complications. Despite a relatively high rate of complications, most patients had substantial improvement in function.
Levels of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main goals of TKA are pain relief, improvement of ambulatory ability, and improvement of ROM. The amount of ROM achieved postoperatively is determined by the amount of preoperative ROM, especially if it was less than 50° [6, 7, 15, 21, 25]. Therefore, preoperative ROM of 50° or less is a challenging dilemma for surgeons. Some investigators have described inconsistent ROM, high risk of complications, and high revision rates, especially in patients with ankylosed knees [18, 22]. However, others have reported that postoperative ROM in patients with stiff and ankylosed knees can be the same as ROM in patients with flexible knees, and low complication rates in these TKAs [20, 21].
Numerous studies had small patients cohorts [1, 3, 4, 10–13, 15, 16, 19, 21, 26], and although higher complication rates and suboptimal outcomes after TKA were reported, there may be a tendency to underestimate complications [22]. Two studies had large patient cohorts [3, 24]. Although Bhan et al. [3] assessed their data using Knee Society knee and function scores, WOMAC scores, including social and emotional functional scores, were not used. Rajgopal et al. [24] did not assess their data using Knee Society knee and function scores or WOMAC scores.
We questioned whether TKA in patients who have been highly incapacitated by their stiff and often postinfected knees would have improvement of pain and function. To ascertain whether TKA in these patients would improve functional outcome and ROM, we asked whether: (1) knee and pain scores, distance walked (endurance), and physical, social, and emotional functions would be improved after TKA; (2) poor preoperative ROM would be improved after TKA; (3) revision rates of TKA in stiff knees would be high; and (4) complication rates would be high in these patients after TKA.
Materials and Methods
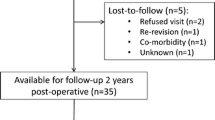
We retrospectively reviewed the records of 92 patients (103 knees) with stiff knees who underwent TKA between January 1995 and January 2002. Preoperative ROM of the knee was limited in all patients: a mean of 40° and range of 10°–50°. During this period, we performed 1770 primary TKAs in 1033 patients. These 103 knees therefore reflected 6% of the total operated during that period. Eleven patients were excluded from this review because of persistent residual pyogenic or tuberculous infection, leaving 81 patients with 93 stiff knees. Seven patients (seven knees) were lost to followup before 1 year after surgery, leaving 74 patients (80%) who underwent TKAs of 86 knees. Four patients died unrelated to the TKA between 5 and 8 years after surgery; they were included in this study. The records of these patients were entered in an ongoing computerized study that was continuously updated. Unless the patient was lost to followup (n = 7), all of the knees were reviewed by an orthopaedic surgeon (YWC) not connected with the original surgery and the data entered into the computerized record. No patient had active pyogenic or tuberculous infection or active drainage at the time of the operation. There were 11 men and 63 women with a mean age of 56.8 years (range, 26–72 years). The mean duration of stiffness was 15.7 years (range, 10–26 years). The duration from prior infection to TKA was 20.4 years (range, 10–21 years). Forty-five of 86 stiff knees had previous arthrotomy and débridement of the knee. Most of the patients could not walk to the bathroom or leave their home unless in a wheelchair. They were highly incapacitated by their stiff and often postinfected knees. Tibiofemoral alignment was recorded preoperatively in all knees. Seventy-two knees (84%) were in 8.5° varus (range, 5°–8°) and 14 knees (16%) were in 5.7° valgus (range, 5°–7°). The minimum followup was 5 years (mean, 9.1 years; range, 5–12 years) (Table 1).
Preoperative clinical, hematologic, and radiographic data were recorded, including any history of documented pyogenic or tuberculous infection on previous surgical procedures on the involved knee, relevant laboratory findings, and clinical features such as draining sinuses. If radiolucent areas that might represent localized osteolysis were present, this was considered when the TKA was planned. All laboratory findings were within normal limits before surgery. Eight weeks preoperatively, we attempted aspiration of each knee that had a previous pyogenic or tuberculous infection. If fluid could not be aspirated, saline washings were taken for culture. Cultures of the aspirated fluid, washings, and excised specimens were grown for aerobic, anaerobic, and tubercle bacilli; none was positive for pyogenic or tubercle bacilli. Histopathologic preparations of the resected tissues and smears were negative. No patient was deferred because of a positive preoperative aspiration. To prove there was no ongoing infection, erythrocyte sedimentation rate, C-reactive protein level, and leukocyte count with differential count on the aspirate, were monitored at 6 weeks, 3 months, 6 months, and 1-year after surgery.
Epidural normotensive anesthesia was used for all procedures. Forty-five knees were approached through a medial parapatellar incision that followed the previous incisional scar and 41 knees without a previous incisional scar were approached through an anterior midline incision. A V-Y quadricepsplasty was performed in 40 knees (47%) to avoid patellar tendon avulsion. The quadriceps muscle was moderately atrophied, but reasonable muscle mass was maintained in all knees. No knee had a tibial tuberosity osteotomy to position the patella above the joint line. The patella was left in the position in which it started. An intramedullary jig was used for resection of the femur, and an extramedullary jig was used for the tibia. Soft tissue balancing then was performed. Stability of the knee was assessed by application of varus-valgus and anteroposterior stress with the knee in 0° extension and 30° flexion after the trial tibial and femoral components were inserted.
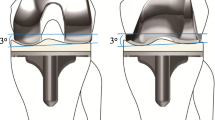
We implanted the NexGen Legacy constrained condylar knee (LCCK) prosthesis® (Zimmer, Inc, Warsaw, IN) in 29 knees and NexGen Legacy posterior-stabilized (LPS)® prosthesis (Zimmer, Inc) in the remaining 57 knees. Both prostheses were available in the operating room. After the trial NexGen LPS femoral and tibial components were inserted, the knee stability was tested manually. If the knee was stable in the coronal plane but unstable in the sagittal plane, the NexGen LPS prosthesis was used. If the knee was unstable in the coronal and sagittal planes, the LCCK prosthesis was used. Elongated stems on the tibial and femoral component were used in 14 knees when the bone stock deficiency was too severe to obtain stable fixation of the components. These stems always were cemented. The surface of the cancellous bone was prepared by pulsatile lavage, and all prostheses were implanted with cement. Antibiotics were not impregnated in the cement because all laboratory findings for infection were negative preoperatively. The capsule was closed and the V-Y quadricepsplasty site was repaired while the knee was maintained in 15° flexion to minimize extension after the operation. The joint line was not elevated intentionally to facilitate flexion. There was no collateral ligament or extensor mechanism avulsion during surgery.
Postoperatively, a continuous passive motion machine was used for passive ROM exercise twice daily for 30 minutes each time. The machine settings were advanced incrementally under the supervision of the therapist. Active ROM exercise was performed by patients under the supervision of the therapist. Patients began standing at the bedside or walking with crutches or a walker twice daily for 30 minutes each time under the supervision of the therapist on the second postoperative day. The patients used crutches or walker with full weightbearing for 6 weeks, and thereafter, a cane as needed. No patient received outpatient physiotherapy after they were discharged from the hospital.
Routine followups were scheduled at postoperative intervals of 6 weeks, 3 months, 6 months, 1 year, and yearly thereafter. At these intervals, the patients were evaluated and radiographs were obtained. Preoperative and postoperative review data were recorded according to the system of the Knee Society (KS) [8] and the Hospital for Special Surgery (HSS) [9]. The WOMAC [2] score was determined at each followup.
Active ROM in the supine position was determined for all patients on two occasions by one of the authors (JSK or YHK) using a standard (60-cm) clinical goniometer before the operation and at the time of the review. The patients were told to bend their knees as much as they would while lying in a supine position. At each followup, we obtained anteroposterior radiographs with the patient standing and supine, a lateral radiograph, and a skyline patellar radiograph. One of the authors (JSK) evaluated radiographs for the presence and location of all radiolucent lines at the bone-cement interface according to the recommendation of the KS [8]. The chance-corrected kappa coefficient [14] was calculated to determine intraobserver agreement of radiographic measurements (for radiolucency at the bone-cement interface). Intraobserver agreement ranged from 0.61 to 0.80.
The changes in KS and WOMAC scores were evaluated with two-tailed Student’s t tests. All analyses were performed with SPSS, Version 14.0 (SPSS Inc, Chicago, IL) with two-tailed Student’s t tests.
Results
Total knee arthroplasty in patients who have been incapacitated with stiff knees improved their pain, function, and ROM. Knee and pain scores, distance walked (endurance), and physical, social, and emotional functions improved after TKA (Table 2). Preoperative ROM (mean, 40°; range, 10°–50°) improved substantially after the operation (mean, 102°; range, 65°–145°) (Table 2). No patient had postoperative manipulation of the knee to improve ROM. Sixty-five knees (76%) obtained greater than 90° flexion and the remaining 21 knees (24%) obtained less than 90° flexion.
We observed no radiolucency at the bone-cement interface in 70 knees (Fig. 1), and 15 knees had an incomplete radiolucent line less than 1 mm in width at the interface between the tibia and tibial component. One knee had a complete radiolucent line wider than 2 mm around the tibial component, which was loose.
Preoperative and postoperative radiographs illustrate the case of a 69-year-old woman with polyarticular adult-onset rheumatoid arthritis. She was bedridden for 40 years. She underwent bilateral simultaneous THAs followed by bilateral simultaneous TKAs and has been ambulating using two crutches since these surgeries. (A) A preoperative anteroposterior radiograph of both knees shows osseous ankylosis in severe flexion. Preoperative lateral radiographs of the (B) right and (C) left knees show osseous ankylosis in 90° flexion. (D) An anteroposterior radiograph of both knees taken 9 years postoperatively shows the LCCK prostheses with femoral and tibial extensions are in place in good alignment. No radiolucent line is visible at the bone-cement interface of the tibial component. Lateral radiographs of the (E) right and (F) left knees taken 9 years postoperatively show the LCCK prostheses with femoral and tibial extensions in place and in good alignment. No radiolucent line is visible at the bone-cement interface of the femoral, tibial, and patellar components. A distal tip of the femoral stem is visible proximally.
The complication rate was relatively high (Table 3). Seventy-four knees (86%) had no complications and the remaining 12 knees (14%) had complications. Five knees (6%) had skin necrosis at the edge of the incision site, which healed after débridement and repeat wound closure in all but one. A skin graft was needed to achieve closure in that knee. A pyogenic infection developed in three knees (3%); no bacteria had grown on cultures of specimens from these knees preoperatively, but Staphylococcus aureus was identified in one knee and Staphylococcus epidermidis was identified in two knees postoperatively. Two of these three knees had débridement and exchange of the tibial polyethylene liner and the patients were given intravenous antibiotics for 6 weeks. There was no recurrence of infection until the latest followup. One knee required removal of the prosthesis and arthrodesis. Periprosthetic fractures occurred after falls in two patients (two knees, 2.3%) at 3 and 5 years, respectively, after surgery. Open reduction and internal fixation was required, and osseous union was obtained in these two knees. Two patients (two knees, 2.3%) had quadriceps tendon rupture at 2 and 3 years, respectively, after surgery. These two patients had frequent episodes of knee buckling while they descended downhill or downstairs. They were advised to have repair of the ruptured quadriceps tendon, however, they refused.
Discussion
The amount of ROM achieved after TKA is determined by the amount of preoperative ROM, especially if the ROM was less than 50° [6, 7, 17, 21, 25]. Therefore, preoperative ROM of 50° or less is a challenging problem. To ascertain whether TKA in patients with stiff knees would improve functional outcome and ROM, we asked four questions: whether pain score, distance walked (endurance), and physical, social, and emotional functions would be improved after TKA; whether poor preoperative ROM would improve after TKA; whether revision rates of TKA in stiff knees would be high; and whether complication rates would be high in these patients after TKA.
There are several limitations of this study. First, the knee scoring systems are prone to interobserver variability. Second, we have no interobserver variability to ensure reliability in interpreting radiolucent lines and loosening. These assessments are somewhat unreliable and therefore the scores are prone to some ranges, and we might have underestimated the incidence of radiolucent lines or loosening. Third, accuracy of measurement of ROM of the knee with a clinical goniometer would be less than that compared with using an electrogoniometer or fluoroscopically guided radiographic measurements [23].
Knee scores for patients with stiff knees in series ranging from 11 to 84 knees have been reported from 14.6 to 42 points (mean, 30 points) before TKA to 74 to 89.5 points (mean, 79.1 points) after TKA [1, 3, 18–21, 24, 27]. Our results were comparable to those of previous studies (Table 4). The average postoperative KS and HSS knee scores and KS function scores for stiff knees in our series were lower than scores for mobile knees [6, 7, 15]. This may be because our patients had severely degenerated knees secondary to pyogenic, tuberculous, or traumatic arthritis or rheumatoid arthritis with polyarticular involvement. One clinical study reported 18 of the 21 patients (86%) with stiff knees had improved quality of life with improvement of deformity, function, and pain after TKA [18]. In the current series, we also found patients with stiff knees had improved quality of life with improvement of pain, walking, distance, deformity, and function after TKA (Table 2). The WOMAC scores for physical, social, and emotional functions also improved substantially after TKA (Table 2). The majority of patients were employed outside the home or were full-time homemakers.
Postoperative ROM in patients with stiff knees may not be comparable with ROM attained by patients without preoperative stiffness. Some authors have reported lack of consistent adequate motion in patients with stiff knees [18, 24]. One study suggests ROM of the knee after TKA in these patients may be indistinguishable from that achieved by a comparable group of patients with flexible knees [21]. However, in that series, a stiff knee was defined as one with less than 90° arc of flexion, and the small number of patients (13 patients) limits applicability of their conclusion to patients with more stiff knees. Postoperative arc of flexion ranging from 74° to 103° (mean, 87.1°) has been reported after TKA in stiff knees in series ranging from 11 to 84 knees (Table 4). Our results were comparable to those of previous studies [1, 3, 18, 19, 24, 27] (Table 4). Although we found knee motion after TKA disappointing in our patients, in all instances, overall motion improved. The arc of motion improved from 40° to 102°, which resulted in improvement in the functional capabilities of our patients. Therefore, although 102° motion conventionally would be considered a poor outcome, it improved the quality of life of these individuals. Preoperatively, most of the patients could not walk to the bathroom or leave their home unless in a wheelchair, but postoperatively, most patients were able to walk outside their homes. The ability to rise from a chair and walk to the bathroom can affect a patient’s quality of life immensely. In addition to improving the ROM, reducing fixed flexion contractures from an average of 25° to 3° greatly alleviates stress across the knee and improves the function of the knee [5].
Several studies reported good radiographic results after TKA in patients with stiff knees. One clinical series reported 91% (82 of 90 knees) of knees with no visible radiolucency at the bone-cement interface at a minimum of 2 years and mean of 6.2 years. Eight knees (9%), however, had a radiolucency of 1 mm in width distal to the tibial component [3]. In that series, one of 90 knees (1%) was revised because of aseptic loosening of the femoral component. In another clinical series [24], 67 of 84 knees (80%) had no radiolucencies, but 17 had radiolucencies of 1 mm or less at the bone-cement interface of the tibial component at a minimum of 4 years and mean of 9 years. In that series, no knee had aseptic loosening (clinically and radiographically) at the final followup. However, one study had a high revision rate for aseptic loosening (18.5% [five of 27 knees]) [16]. We had a low revision rate with a minimum 5-year followup. One knee (1%) had revision for aseptic loosening of the tibial component and rupture of the quadriceps tendon. We believe meticulous soft tissue dissection, improved surgical technique, and improved design of the prosthesis were the factors leading to the low revision rate.
The overall reported complication rate in various studies is 14.2% (34 of 283 knees; range, 3%–41%) [18, 19, 24, 27]. Our series had a similar complication rate (14% [12 of 86 knees]). In general, the complication rate was higher than that in more flexible knees, but this is expected because of multiple prior procedures, extensive soft tissue dissection, and longer operating time. Patients should be counseled preoperatively regarding the possibility of a suboptimal outcome compared with that of a standard TKA performed in a mobile knee, the need for prolonged physiotherapy, and a high complication rate. The relatively high rate of necrosis of the skin edges (6%) indicates the need for special care in handling the skin flaps. These five knees had skin that adhered to the bone before the operation. Similarly, high rates of skin edge necrosis have been reported after TKA with the use of similar implants in ankylosed knees [10, 11, 13]. When the skin is in poor condition, the patient might benefit from a muscle flap or skin graft at the time of the operation or a skin distension procedure, local, or microvascularized free flap as a preliminary step before the TKA.
Despite the relatively high complication rates and less than desired postoperative motion, most of our patients achieved an improvement in function. Based on our data and the literature, we therefore believe the procedure worthwhile even in patients with marked stiffness.
References
Aglietti P, Windsor RE, Buzzi R, Insall JN. Arthroplasty for the stiff and ankylosed knee. J Arthroplasty. 1989;4:1–5.
WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840.
Bhan S, Malhotra R, Kiran EK. Comparison of total knee arthroplasty in stiff and ankylosed knees. Clin Orthop Relat Res. 2006;451:87–95.
Bradley GW, Freeman MA, Albrektsson BE. Total prosthetic replacement of ankylosed knees. J Arthroplasty. 1987;2:179–183.
Cloutier JM, Sabouret P, Deghrar A. Total knee arthroplasty with retention of both cruciate ligaments: a nine to eleven-year follow-up study. J Bone Joint Surg Am. 1999;81:697–702.
Gatha NM, Clarke HD, Fuchs R, Scuderi GR, Insall JN. Factors affecting postoperative range of motion after total knee arthroplasty. J Knee Surg. 2004;17:196–202.
Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA. Factors affecting the range of motion of total knee arthroplasty. J Bone Joint Surg Br. 1993;75:950–955.
Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14.
Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765.
Kim YH, Cho SH, Kim JS. Total knee arthroplasty in bony ankylosis in gross flexion. J Bone Joint Surg Br. 1999;81:296–300.
Kim YH, Kim JS, Cho SH. Total knee replacement after spontaneous osseous ankylosis and take down of formal knee fusion. J Arthroplasty. 2000;15:453–460.
Kim YH, Koo HK, Kim JS. Comparison of fixed-bearing and mobile-bearing total knee arthroplasties. Clin Orthop Relat Res. 2001;392:101–115.
Kim YH, Oh SH, Kim JS. Conversion of a fused knee with use of a posterior stabilized total knee prosthesis. J Bone Joint Surg Am. 2003;85:1047–1050.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174.
Lizaur A, Marco L, Cebrian R. Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. J Bone Joint Surg Br. 1997;79:626–629.
Mahomed N, McKee N, Solomon P, Lahoda L, Gross AE. Soft tissue expansion before total knee arthroplasty in arthrodesed joints: a report of two cases. J Bone Joint Surg Br. 1994;76:88–90.
Malkani AL, Rand JA, Bryan RS, Wallrichs SL. Total knee arthroplasty with the kinematic condylar prosthesis: a ten-year follow-up study. J Bone Joint Surg Am. 1995;77:423–431.
McAuley JP, Harrer MF, Ammeen D, Engh GA. Outcome of knee arthroplasty in patients with poor preoperative range of motion. Clin Orthop Relat Res. 2002;404:203–207.
Montgomery WH 3rd, Insall JN, Haas SB, Becker MS, Windsor RE. Primary total knee arthroplasty in stiff and ankylosed knees. Am J Knee Surg. 1998;11:20–23.
Morag G, Kulidjian A, Zalzal P, Shasha N, Gross AE, Backstein D. Total knee replacement in previous recipients of fresh osteochondral allograft transplants. J Bone Joint Surg Am. 2006;88:541–546.
Mullen JO. Range of motion following total knee arthroplasty in ankylosed joints. Clin Orthop Relat Res. 1983;179:200–203.
Naranja RJ Jr, Lotke PA, Pagnano MW, Hanssen AD. Total knee arthroplasty in a previously ankylosed or arthrodesed knee. Clin Orthop Relat Res. 1996;331:234–237.
Nutton RW, van der Linden ML, Rowe PJ, Gaston P, Wade FA. A prospective randomized double-blind study of functional outcome and range of flexion following total knee replacement with the NexGen standard and high flexion components. J Bone Joint Surg Br. 2008;90:37–42.
Rajgopal A, Ahuja N, Dolai B. Total knee arthroplasty in stiff and ankylosed knees. J Arthroplasty. 2005;20:585–590.
Ryu J, Saito S, Yamamoto K, Sano S. Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Jt Dis. 1993;53:35–40.
Schurman JR 2nd, Wilde AH. Total knee replacement after spontaneous osseous ankylosis: a report of three cases. J Bone Joint Surg Am. 1990;72:455–459.
Spicer DD, Curry JI, Pomeroy D, Badenhausen WE Jr, Schaper LA, Suthers KE, Smith MW. Range of motion after arthroplasty for the stiff osteoarthritic knee. J South Orthop Assoc. 2002;11:227–230.
Acknowledgment
We thank Yoowang Choi, MD, clinical fellow, for collecting data for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial association (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Kim, YH., Kim, JS. Does TKA Improve Functional Outcome and Range of Motion in Patients with Stiff Knees?. Clin Orthop Relat Res 467, 1348–1354 (2009). https://doi.org/10.1007/s11999-008-0445-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0445-7