Abstract
Purpose of review
The purpose of this review is to report recent advances in treatment of neonatal seizures, with a specific focus on new literature since a 2013 systematic review performed by this author (Slaughter) and others. There is a paucity of data with regard to well-defined status epilepticus (SE) in neonates, so treatment of recurrent seizures was also included in this inquiry. We aimed to summarize the efficacy and safety profiles of current therapeutic options as well as describe trends in medication selection in the neonatal intensive care unit (NICU) setting.
Recent findings
Phenobarbital remains first-line therapy in practice, though there is increasing evidence of its neurotoxicity and long-term sequelae. Bumetanide failed an open-label trial for efficacy, demonstrated an increased risk for hearing loss, and has since fallen out of favor for use in this population. New agents, such as levetiracetam and topiramate, still have very limited data but appear to be as efficacious as older medications, with more favorable side effect profiles.
Summary
There are limited high-level evidence-based data to guide treatment of neonatal seizures. Emerging research focusing on drug mechanisms and safety profiles may provide additional information to guide decisions; however, further research is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neonatal seizures are one of the most common reasons for neurologic consultation in the NICU, and can have significant negative consequences on the infant’s neurodevelopment [1, 2]. The approach to diagnosis and treatment of neonatal seizures has evolved over time. This review focuses specifically on recent advances in knowledge regarding acute treatment of SE in the neonatal period. It is notable that much of the literature available is in the setting of recurrent neonatal seizures, rather than well-defined SE.
Neonatal seizures are fundamentally different from seizures at older ages. Neonatal seizures are predominantly symptomatic secondary to acute brain injury (hypoxic-ischemic injury, hemorrhage, stroke, or CNS infection) and are associated with high rates of morbidity and mortality. Seizures tend to be focal, rather than generalized, because of immature neuronal networks. The physiology of the immature brain which is necessary for rapid neurodevelopment results in a lower seizure threshold. Excitatory neurotransmitter receptors (glutamate) mature faster than their inhibitory counterparts, such as GABA [3, 4]. This observation partially explains the suboptimal effectiveness of some standard anticonvulsants, and may provide new targets for treatment. Additionally, gestational age affects the expression of seizures. Full-term infants are more likely to have continuous seizure activity (SE), while preterms are more likely to have recurrent seizures; interictal duration increases with chronologic age [5, 6]. Survivors of neonatal seizures may have sequelae across cognitive and motor domains, as well as increased risk for future epilepsy [7, 8, 9•].
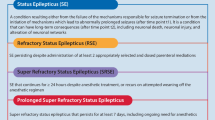
Clinical diagnosis of seizures in neonates is very difficult. Neuronal networks are immature at birth, and, as a result of incomplete myelination, seizures are often subtle or lack motor manifestations altogether [8, 9•, 10]. Between 80 and 90% of electrographic seizures in neonates do not have a clinical correlate; to accurately diagnose seizures in this population, EEG monitoring is required [9•, 11, 12]. One major limitation in the current literature is the varied use of EEG for seizure detection. Some studies include clinically diagnosed seizures while others require electrographic confirmation, and there is a varying duration of recording to confirm treatment effectiveness. There is also variation across studies regarding which neonatal seizures are being studied; some evaluate treatment of recurrent seizures while other studies limit their population to infants with SE. Even in adults, the definition of SE varies between groups [13]. There are emerging attempts in the literature to unify these definitions. The ACNS guidelines designate SE as electrographic seizure totaling > 50% of a 1-h (or more) recording epoch [14]. However, the majority of studies referenced in this paper include treatment applied to both discrete recurrent seizures and SE.
Pharmacologic treatment of seizures is challenging because of the rapidly changing physiology of newborns, including neurotransmitter responsiveness and drug distribution and metabolism. Gestational age, chronologic age, and concurrent therapy, such as hypothermia, all impact metabolism and responsiveness to anticonvulsants. For example, GABA-mediated neurotransmission matures over gestation and early postnatal life. In the immature brain, GABA receptor activation is excitatory rather than inhibitory due to the intracellular to extracellular chloride gradient that relies on developmentally regulated chloride transporters [8]. This gradient matures at different rates in different areas of the brain.
SE in the neonate is considered a medical emergency and clearly requires intervention. However, our understanding of the success and potential consequences of specific treatments is complicated by difficulty distinguishing medication effects from the effects of the seizures themselves, or from consequences of the underlying etiology of seizures. As the scientific community learns more about the detrimental effects of anticonvulsants used most commonly in this age group, neurologists must consider new approaches to neonatal seizure treatment [15,16,17].
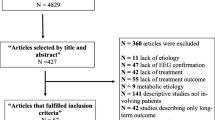
In this review paper, we build on a prior systematic review of treatments for neonatal seizures [18••] by performing an updated search for recent literature on neonatal seizures and anticonvulsants, utilizing the following PubMed search criteria: National Library of Medicine Medical Subject Heading [MeSH] term “seizures/therapy” AND (“Infant, Newborn”[Mesh] OR neonat*) AND (Humans[Mesh] AND English[lang]) for September 2011 through current time (December 2018 used in the search). We reviewed resulted abstracts and have included in our discussion any original research studies if they (a) address SE or recurrent seizures in the neonatal population and if (b) cessation of seizures/seizure control was confirmed by EEG or amplitude integrated EEG. We also report briefly on recent data regarding potential neurodevelopmental side effects of anticonvulsants in animal models of neonatal seizure, and opinion statements by leaders in the field.
Specific anticonvulsant agents in the treatment of neonatal SE
Phenobarbital
Currently, the most common first-line medication for SE in the neonate is phenobarbital [19] (Table 1). Dosing is typically 20 mg/kg IV once, sometimes followed by repeated dosing and/or 5 mg/kg/day maintenance dosing. This is a GABA-A receptor agonist, typically inhibitory in the adult nervous system though potentially excitatory in immature neurons in which the intracellular to extracellular chloride gradient is reversed [3]. It is metabolized in the liver, can induce the cytochrome p450 system, and is primarily renally excreted. In 1999, Painter et al. published a prospective randomized trial in which phenobarbital (goal free level 25 μg/mL) and phenytoin (goal free level 3 μg/mL) were equally effective for control of neonatal seizures, with complete seizure cessation in 43% and 45% of neonates respectively [20]. Seizures were controlled in approximately 60% of babies when the alternate agent was added after the failure of the first. This study considered treatment of all neonatal seizures, not specifically SE. As mentioned in the 2013 review paper, some studies reported a lower response rate to phenobarbital, ranging from 6% complete response to 25% and 29% [21]. However, further neonatal seizure treatment studies that included phenobarbital reported similar rates of seizure cessation to Painter’s study [22, 35].
In the last several years, few studies have provided additional information on neonatal seizure control with phenobarbital. Pathak et al. published results in 2012 of an open-label, randomized controlled trial of phenobarbital versus phenytoin in neonates, finding cessation of clinical seizures in 14.5% of the phenytoin-treated group and 72% of the phenobarbital-treated group [39]. Seizure cessation was based on clinical observation, though brief EEG was performed 48–72 h after apparent clinical seizure control to confirm the absence of ongoing seizure. A 2016 study by Spagnoli et al. retrospectively reviewed charts of 91 infants with neonatal seizures, though specifically excluded those with SE [23]. Similar to earlier neonatal seizure studies, a 62% “complete response” to phenobarbital was found. It was noted that the presence of EEG-only seizures predicted a poor response (refractoriness). A 2016 study by Low et al. reported on 19 infants with electrographic seizures, monitored by continuous EEG with seizure burden analysis techniques [40]. Phenobarbital-treated infants had a 74% seizure reduction at 1 h after administration, and seizures were completely abolished in 65% of cases at the 1-h time interval with a single dose 20 mg/kg of phenobarbital. However, the reduction in seizure burden was no longer significant within 4 h of phenobarbital administration, suggesting that the effectiveness is not sustained. It was noted that the response to phenobarbital was better (more likely to result in short-term seizure cessation) with a lower seizure burden before administration, suggesting that giving phenobarbital early may be more successful. Relevant to our discussion of SE, if seizure burden is already severe, phenobarbital could be less effective.
Concerningly, data has begun to accumulate about potential long-term consequences of even a single dose of phenobarbital in neonatal mammalian models. It has been known since the early 2000s that phenobarbital and several other anticonvulsants (phenytoin, diazepam, clonazepam, vigabatrin, and valproic acid) induce neuronal apoptosis in the neonatal rat brain [41, 42]. This has been confirmed in other studies including Kim et al. in 2007, who also reported that levetiracetam even at supratherapeutic doses did not cause neuronal cell death in animal models [43]. Forcelli et al. found phenobarbital to cause apoptosis in several important limbic regions of the rat brain following neonatal exposure [17]. Phenobarbital also causes apoptosis in the developing white matter (oligodendrocytes) in neonatal models, and again levetiracetam notably did not [44]. Both phenobarbital and midazolam increase the neuronal injury from SE in several brain regions of neonatal rat pups [45]. Additionally, phenobarbital exposure neonatally results in acute and longer-term changes in the proteome and inhibits neurogenesis in the dentate gyrus with measurable effects on learning and memory in a rat model [46, 47]. Even a single dose in the neonatal period can cause long-term synaptic changes—specifically in hippocampal and striatal neurons [48]. The cumulative evidence of potential harm from neonatal exposure to phenobarbital, while not able to be systematically studied in human subjects, suggests that alternative treatments for neonatal seizures are highly desirable.
Phenytoin/fosphenytoin
Phenytoin (or fosphenytoin, its prodrug) is another classic, first-generation anticonvulsant for treatment of SE in children and adults (Table 1). It has fairly well-established efficacy in these populations, with a mechanism of action involving blockade of voltage-gated sodium channels. Risks for cardiac arrhythmias and hypotension, narrow safety margin due to nonlinear pharmacokinetics, high potential for interactions with other medications such as phenobarbital, and need for frequent blood-level monitoring have necessitated caution with use in neonates. Dosing is usually 20 mg/kg (approximate goal free phenytoin level 3 μg/mL). As described above, Painter et al. found phenytoin to achieve seizure cessation in about half of the cases of neonatal seizures [20]. Bye and Flanagan used phenytoin as second line after phenobarbital, and 5 of 32 neonates who did not have seizure cessation with phenobarbital alone did with the phenytoin [25].
No recent/updated studies were found in our literature search to specifically address the use of phenytoin or fosphenytoin in neonatal seizures or neonatal SE. It is still commonly used as second-line treatment after phenobarbital in many institutions, likely due to familiarity with its use in older populations. Notably, it does induce apoptosis in neonatal rat brain models and also seems to show an effect on synaptogenesis in the striatum when used in the developing brain [16, 17, 41, 42].
Levetiracetam
Levetiracetam is a second-generation anticonvulsant with FDA approval for use in adults in 1999 and added approval in 2012 as an adjunctive medication for treatment of focal onset seizures in infants and children age 1 month and older. Its mechanisms of action are incompletely understood, but it is thought to have inhibitory action via binding to the synaptic vesicle protein SV2a, which controls neurotransmitter release and vesicle transport in neurons. It may also inhibit calcium- and potassium-gated channels [49]. Levetiracetam has favorable pharmacologic characteristics for use in neonates and infants, with linear kinetics, low protein binding, and lack of liver metabolism [49, 50]. Roughly two-thirds of the administered drug is excreted unchanged in the urine. Drug clearance is faster in children compared to adults, but slower in the young infant population (under 6 months old) [50, 51].
There are no large population or prospective studies on levetiracetam use in neonates, but multiple small studies have demonstrated efficacy in seizure reduction (with EEG confirmation) and tolerability in this population as outlined in our 2013 review [18••, 26, 27, 52, 53] (Table 1). Loading doses in these studies ranged from 10 to 50 mg/kg. Reported side effects include somnolence and irritability, but there were no serious adverse events leading to medication discontinuation or escalation of medical care [51, 54].
Despite limited data, levetiracetam use to treat neonatal seizures has increased dramatically in the last decade, from 1.4 to 14% from 2005 to 2014 [55]. Levetiracetam is often the second-line drug, given after failure of phenobarbital [19]. In a small subset of patients given levetiracetam first line for seizure treatment (22 patients), there was no significant difference in seizure recurrence rate compared to phenobarbital (64% vs 65%). Median loading dose was 20 mg/kg. This study included clinically diagnosed seizures as well as EEG-confirmed events and was not limited to SE [56•].
Topiramate
Topiramate was first reported to have antiseizure activity in 1986 and was initially FDA approved as an add-on therapy for focal onset seizures in adults [57]. It is currently FDA approved for first-line treatment of focal and generalized onset seizures in patients 2 years and older. Its mechanism of action includes reduced voltage-gated sodium channel conduction, increased GABA-evoked inhibitory current, and blockade of glutamatergic kainite/AMPA receptors. Its GABA interaction is independent of the benzodiazepine receptor system [58]. It is partially metabolized in the liver and is more rapidly metabolized in patients receiving hepatic enzyme-inducing drugs. Likewise, topiramate is a mild inducer of the P450 system. It is renally excreted, more rapidly in children than adults [59]. Hypothermia slows absorption and elimination [60]. Anticonvulsant efficacy in animal models is comparable to phenytoin and carbamazepine [61]. It is currently only available in enteral form.
Data are available on topiramate in pediatric SE confirmed by cEEG in patients as young as 2 months. Patients experienced seizure cessation within 24 h of treatment starting at a high initial dose of 10 mg/kg/day enterally divided BID × 2 days followed by 5 mg/kg divided BID [28]. Titrating up from lower starting doses (2–3 mg/kg/day) can also be effective within 24 h of achieving a goal dose of 5–6 mg/kg/day [62].
Intermittent neonatal seizures refractory to standard treatment may respond to topiramate (Table 1). In children aged 0–24 months with refractory seizures on polytherapy, adding enteral topiramate was associated with > 80% reduction in seizure frequency, although response was sometimes delayed after the first month of treatment using up to 40 mg/kg/day [63]. Glass et al. reported that 4 of 5 neonates with seizures refractory to phenobarbital had reduction or cessation of seizures after adding topiramate 10 mg/kg/day [64]. Use in preterm infants has been limited. Riesgo et al. reported three cases of preterm neonates with seizures refractory to at least 3 traditional anticonvulsants. All infants achieved seizure-freedom with the addition of topiramate at approximately term equivalent once they were titrated up to a dose of 3.5 to 8 mg/kg/day [65]. In preterm infants, there may be an increased risk of necrotizing enterocolitis [30]. Other short-term risks include appetite suppression, sedation, and acidosis.
There may be benefits of topiramate beyond acute treatment of seizures. A neuroprotective effect in the setting of neuronal ischemia has been demonstrated in cultured rat neurons, in an adult rat cardiac arrest model, and in neonatal rats with carotid occlusion [66,67,68]. Topiramate given at 10 mg/kg/day × 3 days along with therapeutic hypothermia for neonatal HIE may reduce the risk of epilepsy [29].
Despite minimal published data, neurologists are using topiramate in the NICU. In a survey of 55 neurologists, 55% reported using topiramate for neonatal seizures, mostly as second- or third-line therapy. It was believed by 60% of respondents to be effective. Nearly one-third reported side effects attributed to topiramate, most often irritability or feeding problems and metabolic acidosis [69].
Bumetanide
Bumetanide is a loop diuretic that blocks the NKCC1 transporter which is responsible for the high intracellular chloride gradient in immature neurons. This gradient results in cell depolarization when GABA-mediated chloride channels open. One possible reason for the difficulty in treating neonatal seizures is that traditionally used medications enhance GABA transmission, which in immature cells is paradoxically excitatory. Several in vitro and animal models suggested that blocking NKCC1 transport with bumetanide improved the efficacy of phenobarbital in controlling seizures [31, 32]. However, an open-label phase 1/2 trial for dose finding and feasibility ended early. The study failed to show efficacy (80% seizure reduction) and there was an increased risk of hearing loss in bumetanide-treated infants [33]. Bumetanide is an enticing therapy with a mechanism of action directed at the unique aspects of neonatal neuronal neurotransmission, but the drug itself has fallen out of favor for neonatal seizures after results of the trial were published (Table 1).
Midazolam/benzodiazepines
Midazolam and other benzodiazepines are GABA-A agonists which can be used for sedation, anesthesia, and anxiety treatment in addition to seizure control. Benzodiazepines as a group are the most common seizure rescue medications utilized in adult and older pediatric age groups. However, use in neonates as an anticonvulsant has been somewhat limited due to the sedative properties (potentially leading to respiratory suppression, a concern if the infant is not already mechanically ventilated), and possible hypotension which could lead to hypoperfusion of brain tissue that has already sustained hypoxic-ischemic injury). There is also concern for neurotoxicity specifically in the neonatal age group; apoptotic neurodegeneration has been shown in some animal models after exposure to midazolam, and its historical use for anesthesia in this age group has led to studies demonstrating negative long-term consequences on learning [70, 71]. Diazepam has neuronal apoptotic effects in neonatal rats [42]. Midazolam can induce apoptosis at low doses and necrosis at higher doses in animal models [72]. In addition, as mentioned previously, Torolira et al. demonstrated in a rat model that treatment with a single dose of either phenobarbital or midazolam actually exacerbated the acute neuronal injury from SE in several different brain regions [73].
Data on benzodiazepine efficacy in neonatal seizures is limited and conflicting (Table 1). Prior studies have reported responses to midazolam (as second-line after phenobarbital) ranging from 0 of 3 subjects with low-dose midazolam (0.06 mg/kg bolus then maximum 0.15 mg/kg/h maintenance), to 13 of 13 subjects with higher dosing (0.15 mg/kg bolus followed by 0.06–1 mg/kg/h maintenance) [22, 35]. In one study of continuous midazolam infusion (0.06–0.2 mg/kg/h), without initial bolus dosing, 4 of 8 subjects were found to have a partial response; however, this was not sustained more than 6 h [36]. Several other small case series exist utilizing single doses of lorazepam but without consistent use of EEG monitoring, and seizure recurrence within a few hours seems to be quite frequent even if an initial response was seen.
Review of more recent literature revealed one study that met our search criteria [34]. This study specifically focused on the effectiveness of midazolam as a continuous drip in the setting of recurrent seizures in newborns undergoing cooling for perinatal asphyxia. Twenty-three percent of infants receiving midazolam for anticonvulsant use after failure of phenobarbital therapy had successful seizure control (reduction in EEG seizure burden of > 80%). When considering infants on a midazolam drip for sedation as well as those receiving it for anticonvulsant therapy, the study found that 64% had at least one episode of hypotension, even with the use of inotropes. In a population already having experienced cerebral hypoxia/ischemia perinatally, additional hypotension is highly undesirable. The authors noted a direct relationship between plasma midazolam concentration and decrease from baseline mean arterial blood pressure; notably, asphyxiated patients would be at risk to have decreased midazolam clearance due to kidney and liver dysfunction, potentially leading to high accumulated levels.
Lidocaine
Lidocaine is a type 1b antiarrhythmic drug first synthesized in 1948. It blocks fast voltage-gated sodium channels in neurons and the cardiac conduction system. It is metabolized by the P450 system. Clearance is primarily renal and is reduced by 24% by hypothermia [37, 74].
Lidocaine was first reported to be effective for neonatal seizures in 1988. A series of 46 newborns with recurrent seizures confirmed by EEG or cerebral function monitor received lidocaine bolus followed by continuous infusion after failure of phenobarbital. Seizures stopped in 83% (38) of neonates within 4 h after lidocaine was given; however, the study was not clear on how long the medication was effective in seizure control. There was a dose-dependent effect with best results after a loading dose of 2 mg/kg and infusion of 6 mg/kg/h [38] (Table 1). This study did not identify any adverse reactions. Infusion for 6 h did not result in serum levels that are reported to cause toxicity in adults [75].
In one study comparing lidocaine to midazolam as second line after phenobarbital, there was not a statistically significant difference in the effectiveness of these two drugs [35]. A retrospective chart review reported lidocaine to be more effective than midazolam as second-line therapy, especially in patients with hypoxic-ischemic encephalopathy; 77% of neonates responded to lidocaine compared to 50% responding to midazolam [36]. Notably, in this study, response to the medication included reduction of seizure duration, as opposed to complete cessation or a percent decrease in seizure frequency.
Lidocaine has potentially serious short-term side effects including bradycardia in 5% of neonates, other arrhythmias, and with serum concentration > 15 mg/L, can actually cause seizures [76, 77] [78]. It is generally recommended to avoid lidocaine in patients with congenital heart disease, liver disease, or renal impairment [76].
Other possible interventions
There are additional intravenous medications used in pediatric and adult treatment of SE that could be considered in the neonatal population, such as ketamine or lacosamide. However, current data in neonates is essentially limited to small case reports, and use would require extrapolation from studies in older children.
Ketamine is an N-methyl-D-aspartate receptor antagonist with class IV evidence for treatment of refractory SE [79, 80]. There is literature from animal models that ketamine may cause neuronal apoptosis [81]; however, clinically, it appears to be well tolerated, and does not appear to cause respiratory depression, which would be favorable in neonates. In a case series including children as young as 2 months, Ilvento et al. found ketamine to be safe and effective in treating refractory SE with no major adverse events reported. A prospective study of preterm (< 33 week) infants that received ketamine for endotracheal intubation (one-time dosing range of 1–5 mg/kg) did not find any difference in neurodevelopmental outcomes at 2 years of age compared to a control group [82].
Lacosamide enhances inhibition of slow sodium channels and is used predominantly as adjunctive therapy for focal onset seizures, but also has a role in treatment of SE and refractory SE. Its intravenous formulation lends to its appeal for use in SE. A case series by Arkilo et al., which included a child as young as 4 weeks, found lacosamide infusion to be safe (only reported side effects were sedation and ataxia) and efficacious [83]. Lacosamide was found to have neuroprotective properties against hypoxia-ischemia in neonatal rat model, which suggests potential added benefit in the neonatal population [84].
Conclusions and future directions
There is very limited high-level evidence-based data to guide treatment of neonatal seizures, despite the frequency and severity of this problem in NICUs. We provide an overview of several pharmacologic options, but find that most have suboptimal data on efficacy and safety to support their use in this population. Additionally, our understanding of medication-induced neurotoxicity continues to grow, further highlighting the need for ongoing research.
Further exploration of newer anticonvulsant agents such as levetiracetam and topiramate is of particular interest, due to their lack of neuronal apoptosis in animal models. Levetiracetam has favorable pharmacokinetics and safety in neonates, appears to have promising initial evidence for efficacy as a second-line agent, and its use has become increasingly common in practice, even ahead of definitive evidence for efficacy in first-line use. Topiramate also has the potential to be useful and causes minimal sedation, but right now, without an IV formulation, its use in the acutely ill neonate is limited. Topiramate may have neuroprotective properties, which would be of particular benefit in this population. Lacosamide has minimal evidence yet for use in neonates, but with an IV formulation available and good tolerability in older infants, may be on the horizon for further investigation. As evidence becomes clearer regarding seizure treatments for term neonates, there will be a need to examine these same drugs in specific populations such as preterm infants or hypothermia-treated infants.
In practice, it is a delicate balance to attempt to avoid or limit duration of exposure to the anticonvulsants with known detrimental side effects, while also treating seizures effectively and minimizing risk of recurrent seizures. Neonatal seizure treatment is an active and exciting area of research, but the need for additional data is critical so that the evidence can be safely and appropriately applied to the clinical situations we currently face.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nardou R, Ferrari DC, Ben-Ari Y. Mechanisms and effects of seizures in the immature brain. Semin Fetal Neonatal Med. 2013;18:175–84. https://doi.org/10.1016/j.siny.2013.02.003.
Ben-Ari Y, Holmes GL. Effects of seizures on developmental processes in the immature brain. Lancet Neurol. 2006;5:1055–63. https://doi.org/10.1016/S1474-4422(06)70626-3.
Jensen FE. Developmental factors in the pathogenesis of neonatal seizures. J Pediatr Neurol. 2009;7:5–12. https://doi.org/10.3233/JPN-2009-0270.
Jensen FE. The role of glutamate receptor maturation in perinatal seizures and brain injury. Int J Dev Neurosci. 2002;20:339–47.
Scher MS, Hamid MY, Steppe DA, Beggarly ME, Painter MJ. Ictal and interictal electrographic seizure durations in preterm and term neonates. Epilepsia. 1993;34:284–8.
Scher MS, Aso K, Beggarly ME, Hamid MY, Steppe DA, Painter MJ. Electrographic seizures in preterm and full-term neonates: clinical correlates, associated brain lesions, and risk for neurologic sequelae. Pediatrics. 1993;91:128–34.
Glass HC, Numis AL, Gano D, Bali V, Rogers EE. Outcomes after acute symptomatic seizures in children admitted to a neonatal neurocritical care service. Pediatr Neurol. 2018;84:39–45. https://doi.org/10.1016/j.pediatrneurol.2018.03.016.
Jensen FE. Neonatal seizures: an update on mechanisms and management. Clin Perinatol. 2009;36:881–900, vii. https://doi.org/10.1016/j.clp.2009.08.001.
• Abend NS, Wusthoff CJ. Neonatal seizures and status epilepticus. J Clin Neurophysiol. 2012;29:441–8. https://doi.org/10.1097/WNP.0b013e31826bd90d This paper describes a working definition of neonatal status epilepticus and summarizes the electrographic signature of neonatal seizures.
Hellström-Westas L, Boylan G, Ågren J. Systematic review of neonatal seizure management strategies provides guidance on anti-epileptic treatment. Acta Paediatr. 2015;104:123–9. https://doi.org/10.1111/apa.12812.
Murray DM, Boylan GB, Ali I, Ryan CA, Murphy BP, Connolly S. Defining the gap between electrographic seizure burden, clinical expression and staff recognition of neonatal seizures. Arch Dis Child Fetal Neonatal Ed. 2008;93:F187–91. https://doi.org/10.1136/adc.2005.086314.
Wusthoff CJ, Dlugos DJ, Gutierrez-Colina A, Wang A, Cook N, Donnelly M, et al. Electrographic seizures during therapeutic hypothermia for neonatal hypoxic-ischemic encephalopathy. J Child Neurol. 2011;26:724–8. https://doi.org/10.1177/0883073810390036.
Leitinger M, Trinka E, Gardella E, Rohracher A, Kalss G, Qerama E, et al. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15:1054–62. https://doi.org/10.1016/S1474-4422(16)30137-5.
Tsuchida TN, Wusthoff CJ, Shellhaas RA, Abend NS, Hahn CD, Sullivan JE, et al. American clinical neurophysiology society standardized EEG terminology and categorization for the description of continuous EEG monitoring in neonates: report of the American Clinical Neurophysiology Society critical care monitoring committee. J Clin Neurophysiol. 2013;30:161–73. https://doi.org/10.1097/WNP.0b013e3182872b24.
Gutherz SB, Kulick CV, Soper C, Kondratyev A, Gale K, Forcelli PA. Brief postnatal exposure to phenobarbital impairs passive avoidance learning and sensorimotor gating in rats. Epilepsy Behav. 2014;37:265–9. https://doi.org/10.1016/j.yebeh.2014.07.010.
Forcelli PA, Janssen MJ, Vicini S, Gale K. Neonatal exposure to antiepileptic drugs disrupts striatal synaptic development. Ann Neurol. 2012;72:363–72. https://doi.org/10.1002/ana.23600.
Forcelli PA, Kim J, Kondratyev A, Gale K. Pattern of antiepileptic drug-induced cell death in limbic regions of the neonatal rat brain. Epilepsia. 2011;52:e207–11. https://doi.org/10.1111/j.1528-1167.2011.03297.x.
•• Slaughter LA, Patel AD, Slaughter JL. Pharmacological treatment of neonatal seizures: a systematic review. J Child Neurol. 2013;28:351–64. https://doi.org/10.1177/0883073812470734 This review provides an in-depth assessment of the literature available regarding neonatal seizure treatment as of 2013; our current review references this data and adds more recently available literature.
Glass HC, Kan J, Bonifacio SL, Ferriero DM. Neonatal seizures: treatment practices among term and preterm infants. Pediatr Neurol. 2012;46:111–5. https://doi.org/10.1016/j.pediatrneurol.2011.11.006.
Painter MJ, Scher MS, Stein AD, Armatti S, Wang Z, Gardiner JC, et al. Phenobarbital compared with phenytoin for the treatment of neonatal seizures. N Engl J Med. 1999;341:485–9. https://doi.org/10.1056/NEJM199908123410704.
Boylan GB, Rennie JM, Pressler RM, Wilson G, Morton M, Binnie CD. Phenobarbitone, neonatal seizures, and video-EEG. Arch Dis Child Fetal Neonatal Ed. 2002;86:F165–70.
Castro Conde JR, Hernández Borges AA, Doménech Martínez E, González Campo C, Perera Soler R. Midazolam in neonatal seizures with no response to phenobarbital. Neurology. 2005;64:876–9. https://doi.org/10.1212/01.WNL.0000152891.58694.71.
Spagnoli C, Seri S, Pavlidis E, Mazzotta S, Pelosi A, Pisani F. Phenobarbital for neonatal seizures: response rate and predictors of refractoriness. Neuropediatrics. 2016;47:318–26. https://doi.org/10.1055/s-0036-1586214.
Low E, Boylan GB, Mathieson SR, et al. Cooling and seizure burden in term neonates: an observational study. Arch Dis Child Fetal Neonatal Ed. 2012;97:F267–72. https://doi.org/10.1159/000443782.
Bye AM, Flanagan D. Spatial and temporal characteristics of neonatal seizures. Epilepsia. 1995;36:1009–16.
Khan O, Chang E, Cipriani C, Wright C, Crisp E, Kirmani B. Use of intravenous levetiracetam for management of acute seizures in neonates. Pediatr Neurol. 2011;44:265–9. https://doi.org/10.1016/j.pediatrneurol.2010.11.005.
Abend NS, Gutierrez-Colina AM, Monk HM, Dlugos DJ, Clancy RR. Levetiracetam for treatment of neonatal seizures. J Child Neurol. 2011;26:465–70. https://doi.org/10.1177/0883073810384263.
Perry MS, Holt PJ, Sladky JT. Topiramate loading for refractory status epilepticus in children. Epilepsia. 2006;47:1070–1. https://doi.org/10.1111/j.1528-1167.2006.00564.x.
Filippi L, Fiorini P, Catarzi S, Berti E, Padrini L, Landucci E, et al. Safety and efficacy of topiramate in neonates with hypoxic ischemic encephalopathy treated with hypothermia (NeoNATI): a feasibility study. J Matern Fetal Neonatal Med. 2018;31:973–80. https://doi.org/10.1080/14767058.2017.1304536.
Courchia B, Kurtom W, Pensirikul A, Del-Moral T, Buch M. Topiramate for seizures in preterm infants and the development of necrotizing enterocolitis. Pediatrics. 2018;142:e20173971. https://doi.org/10.1542/peds.2017-3971.
Dzhala VI, Brumback AC, Staley KJ. Bumetanide enhances phenobarbital efficacy in a neonatal seizure model. Ann Neurol. 2008;63:222–35. https://doi.org/10.1002/ana.21229.
Cleary RT, Sun H, Huynh T, Manning SM, Li Y, Rotenberg A, et al. Bumetanide enhances phenobarbital efficacy in a rat model of hypoxic neonatal seizures. PLoS One. 2013;8:e57148. https://doi.org/10.1371/journal.pone.0057148.
Pressler RM, Boylan GB, Marlow N, Blennow M, Chiron C, Cross JH, et al. Bumetanide for the treatment of seizures in newborn babies with hypoxic ischaemic encephalopathy (NEMO): an open-label, dose finding, and feasibility phase 1/2 trial. Lancet Neurol. 2015;14:469–77. https://doi.org/10.1016/S1474-4422(14)70303-5.
van den Broek MP, van Straaten HL, Huitema AD, et al. Anticonvulsant effectiveness and hemodynamic safety of midazolam in full-term infants treated with hypothermia. Neonatology. 2015;107:150–6. https://doi.org/10.1159/000368180.
Boylan GB, Rennie JM, Chorley G, Pressler RM, Fox GF, Farrer K, et al. Second-line anticonvulsant treatment of neonatal seizures: a video-EEG monitoring study. Neurology. 2004;62:486–8.
Shany E, Benzaqen O, Watemberg N. Comparison of continuous drip of midazolam or lidocaine in the treatment of intractable neonatal seizures. J Child Neurol. 2007;22:255–9. https://doi.org/10.1177/0883073807299858.
Hellström-Westas L, Svenningsen NW, Westgren U, Rosén I, Lagerström PO. Lidocaine for treatment of severe seizures in newborn infants. II. Blood concentrations of lidocaine and metabolites during intravenous infusion. Acta Paediatr. 1992;81:35–9.
Hellström-Westas L, Westgren U, Rosén I, Svenningsen NW. Lidocaine for treatment of severe seizures in newborn infants. I. Clinical effects and cerebral electrical activity monitoring. Acta Paediatr Scand. 1988;77:79–84.
Pathak G, Upadhyay A, Pathak U, Chawla D, Goel SP. Phenobarbitone versus phenytoin for treatment of neonatal seizures: an open-label randomized controlled trial. Indian Pediatr. 2013;50:753–7.
Low E, Stevenson NJ, Mathieson SR, Livingstone V, Ryan AC, Rennie JM, et al. Short-term effects of phenobarbitone on electrographic seizures in neonates. Neonatology. 2016;110:40–6. https://doi.org/10.1159/000443782.
Bittigau P, Sifringer M, Ikonomidou C. Antiepileptic drugs and apoptosis in the developing brain. Ann N Y Acad Sci. 2003;993:103–14 discussion 123-104.
Bittigau P, Sifringer M, Genz K, Reith E, Pospischil D, Govindarajalu S, et al. Antiepileptic drugs and apoptotic neurodegeneration in the developing brain. Proc Natl Acad Sci U S A. 2002;99:15089–94. https://doi.org/10.1073/pnas.222550499.
Kim JS, Kondratyev A, Tomita Y, Gale K. Neurodevelopmental impact of antiepileptic drugs and seizures in the immature brain. Epilepsia. 2007;48(Suppl 5):19–26. https://doi.org/10.1111/j.1528-1167.2007.01285.x.
Kaushal S, Tamer Z, Opoku F, Forcelli PA. Anticonvulsant drug-induced cell death in the developing white matter of the rodent brain. Epilepsia. 2016;57:727–34. https://doi.org/10.1111/epi.13365.
Torolira D, Suchomelova L, Wasterlain CG, Niquet J. Widespread neuronal injury in a model of cholinergic status epilepticus in postnatal day 7 rat pups. Epilepsy Res. 2016;120:47–54. https://doi.org/10.1016/j.eplepsyres.2015.11.005.
Kaindl AM, Koppelstaetter A, Nebrich G, Stuwe J, Sifringer M, Zabel C, et al. Brief alteration of NMDA or GABAA receptor-mediated neurotransmission has long term effects on the developing cerebral cortex. Mol Cell Proteomics. 2008;7:2293–310. https://doi.org/10.1074/mcp.M800030-MCP200.
Stefovska VG, Uckermann O, Czuczwar M, Smitka M, Czuczwar P, Kis J, et al. Sedative and anticonvulsant drugs suppress postnatal neurogenesis. Ann Neurol. 2008;64:434–45. https://doi.org/10.1002/ana.21463.
Al-Muhtasib N, Sepulveda-Rodriguez A, Vicini S, Forcelli PA. Neonatal phenobarbital exposure disrupts GABAergic synaptic maturation in rat CA1 neurons. Epilepsia. 2018;59:333–44. https://doi.org/10.1111/epi.13990.
Mruk AL, Garlitz KL, Leung NR. Levetiracetam in neonatal seizures: a review. J Pediatr Pharmacol Ther. 2015;20:76–89. https://doi.org/10.5863/1551-6776-20.2.76.
Glauser TA, Mitchell WG, Weinstock A, Bebin M, Chen D, Coupez R, et al. Pharmacokinetics of levetiracetam in infants and young children with epilepsy. Epilepsia. 2007;48:1117–22. https://doi.org/10.1111/j.1528-1167.2007.01090.x.
Merhar SL, Schibler KR, Sherwin CM, et al. Pharmacokinetics of levetiracetam in neonates with seizures. J Pediatr. 2011;159:152–154.e153. https://doi.org/10.1016/j.jpeds.2011.03.057.
Khan O, Cipriani C, Wright C, Crisp E, Kirmani B. Role of intravenous levetiracetam for acute seizure management in preterm neonates. Pediatr Neurol. 2013;49:340–3. https://doi.org/10.1016/j.pediatrneurol.2013.05.008.
Ramantani G, Ikonomidou C, Walter B, Rating D, Dinger J. Levetiracetam: safety and efficacy in neonatal seizures. Eur J Paediatr Neurol. 2011;15:1–7. https://doi.org/10.1016/j.ejpn.2010.10.003.
Venkatesan C, Young S, Schapiro M, Thomas C. Levetiracetam for the treatment of seizures in neonatal hypoxic ischemic encephalopathy. J Child Neurol. 2017;32:210–4. https://doi.org/10.1177/0883073816678102.
Ahmad KA, Desai SJ, Bennett MM, Ahmad SF, Ng YT, Clark RH, et al. Changing antiepileptic drug use for seizures in US neonatal intensive care units from 2005 to 2014. J Perinatol. 2017;37:296–300. https://doi.org/10.1038/jp.2016.206.
• Glass HC, Shellhaas RA, Wusthoff CJ, et al. Contemporary profile of seizures in neonates: a prospective cohort study. J Pediatr. 2016;174:98–103.e101. https://doi.org/10.1016/j.jpeds.2016.03.035 This well-designed prospective study describes current practice trends and outcomes among neonates with seizures treated with anticonvulsants
Maryanoff BE, Nortey SO, Gardocki JF, Shank RP, Dodgson SP. Anticonvulsant O-alkyl sulfamates. 2,3:4,5-Bis-O-(1-methylethylidene)-beta-D-fructopyranose sulfamate and related compounds. J Med Chem. 1987;30:880–7.
Rosenfeld WE. Topiramate: a review of preclinical, pharmacokinetic, and clinical data. Clin Ther. 1997;19:1294–308.
Rosenfeld WE, Doose DR, Walker SA, Baldassarre JS, Reife RA. A study of topiramate pharmacokinetics and tolerability in children with epilepsy. Pediatr Neurol. 1999;20:339–44.
Filippi L, la Marca G, Fiorini P, Poggi C, Cavallaro G, Malvagia S, et al. Topiramate concentrations in neonates treated with prolonged whole body hypothermia for hypoxic ischemic encephalopathy. Epilepsia. 2009;50:2355–61. https://doi.org/10.1111/j.1528-1167.2009.02302.x.
Patsalos PN, Sander JW. Newer antiepileptic drugs. Towards an improved risk-benefit ratio. Drug Saf. 1994;11:37–67.
Kahriman M, Minecan D, Kutluay E, Selwa L, Beydoun A. Efficacy of topiramate in children with refractory status epilepticus. Epilepsia. 2003;44:1353–6.
Puri V, Ness S, Sattaluri SJ, Wang S, Todd M, Yuen E, et al. Long-term open-label study of adjunctive topiramate in infants with refractory partial-onset seizures. J Child Neurol. 2011;26:1271–83. https://doi.org/10.1177/0883073811406982.
Glass HC, Poulin C, Shevell MI. Topiramate for the treatment of neonatal seizures. Pediatr Neurol. 2011;44:439–42. https://doi.org/10.1016/j.pediatrneurol.2011.01.006.
Riesgo R, Winckler MI, Ohlweiler L, Ranzan J, Becker M, Salvador S, et al. Treatment of refractory neonatal seizures with topiramate. Neuropediatrics. 2012;43:353–6. https://doi.org/10.1055/s-0032-1327771.
Noh MR, Kim SK, Sun W, et al. Neuroprotective effect of topiramate on hypoxic ischemic brain injury in neonatal rats. Exp Neurol. 2006;201:470–8. https://doi.org/10.1016/j.expneurol.2006.04.038.
Edmonds HL, Jiang YD, Zhang PY, Shank R. Topiramate as a neuroprotectant in a rat model of global ischemia-induced neurodegeneration. Life Sci. 2001;69:2265–77.
Schubert S, Brandl U, Brodhun M, Ulrich C, Spaltmann J, Fiedler N, et al. Neuroprotective effects of topiramate after hypoxia-ischemia in newborn piglets. Brain Res. 2005;1058:129–36. https://doi.org/10.1016/j.brainres.2005.07.061.
Silverstein FS, Ferriero DM. Off-label use of antiepileptic drugs for the treatment of neonatal seizures. Pediatr Neurol. 2008;39:77–9. https://doi.org/10.1016/j.pediatrneurol.2008.04.008.
Young C, Jevtovic-Todorovic V, Qin YQ, Tenkova T, Wang H, Labruyere J, et al. Potential of ketamine and midazolam, individually or in combination, to induce apoptotic neurodegeneration in the infant mouse brain. Br J Pharmacol. 2005;146:189–97. https://doi.org/10.1038/sj.bjp.0706301.
Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–82.
Stevens MF, Werdehausen R, Gaza N, Hermanns H, Kremer D, Bauer I, et al. Midazolam activates the intrinsic pathway of apoptosis independent of benzodiazepine and death receptor signaling. Reg Anesth Pain Med. 2011;36:343–9. https://doi.org/10.1097/AAP.0b013e318217a6c7.
Torolira D, Suchomelova L, Wasterlain CG, Niquet J. Phenobarbital and midazolam increase neonatal seizure-associated neuronal injury. Ann Neurol. 2017;82:115–20. https://doi.org/10.1002/ana.24967.
van den Broek MP, Rademaker CM, van Straaten HL, et al. Anticonvulsant treatment of asphyxiated newborns under hypothermia with lidocaine: efficacy, safety and dosing. Arch Dis Child Fetal Neonatal Ed. 2013;98:F341–5. https://doi.org/10.1136/archdischild-2012-302678.
Malingré MM, Van Rooij LG, Rademaker CM, et al. Development of an optimal lidocaine infusion strategy for neonatal seizures. Eur J Pediatr. 2006;165:598–604. https://doi.org/10.1007/s00431-006-0136-x.
van Rooij LG, Toet MC, Rademaker KM, Groenendaal F, de Vries LS. Cardiac arrhythmias in neonates receiving lidocaine as anticonvulsive treatment. Eur J Pediatr. 2004;163:637–41. https://doi.org/10.1007/s00431-004-1513-y.
Rothstein P, Dornbusch J, Shaywitz BA. Prolonged seizures associated with the use of viscous lidocaine. J Pediatr. 1982;101:461–3.
DeToledo JC. Lidocaine and seizures. Ther Drug Monit. 2000;22:320–2.
Höfler J, Trinka E. Intravenous ketamine in status epilepticus. Epilepsia. 2018;59:198–206. https://doi.org/10.1111/epi.14480.
Höfler J, Rohracher A, Kalss G, Zimmermann G, Dobesberger J, Pilz G, et al. (S)-Ketamine in refractory and super-refractory status epilepticus: a retrospective study. CNS Drugs. 2016;30:869–76. https://doi.org/10.1007/s40263-016-0371-2.
Dong C, Anand KJ. Developmental neurotoxicity of ketamine in pediatric clinical use. Toxicol Lett. 2013;220:53–60. https://doi.org/10.1016/j.toxlet.2013.03.030.
Ilvento L, Rosati A, Marini C, L'Erario M, Mirabile L, Guerrini R. Ketamine in refractory convulsive status epilepticus in children avoids endotracheal intubation. Epilepsy Behav. 2015;49:343–6. https://doi.org/10.1016/j.yebeh.2015.06.019.
Arkilo D, Gustafson M, Ritter FJ. Clinical experience of intravenous lacosamide in infants and young children. Eur J Paediatr Neurol. 2016;20:212–7. https://doi.org/10.1016/j.ejpn.2015.12.013.
Kim GH, Byeon JH, Eun BL. Neuroprotective effect of lacosamide on hypoxic-ischemic brain injury in neonatal rats. J Clin Neurol. 2017;13:138–43. https://doi.org/10.3988/jcn.2017.13.2.138.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Epilepsy
Rights and permissions
About this article
Cite this article
Ahrens, S., Ream, M.A. & Slaughter, L.A. Status Epilepticus in the Neonate: Updates in Treatment Strategies. Curr Treat Options Neurol 21, 8 (2019). https://doi.org/10.1007/s11940-019-0546-5
Published:
DOI: https://doi.org/10.1007/s11940-019-0546-5