Opinion statement
Dementia, especially Alzheimer’s disease, is an important cause of seizures and epilepsy midst the elderly. With the increasing life span, the incidence of dementia and epilepsy is expected to increase exponentially. Care of patients with advanced dementia can be demanding and seizures add to this burden. Though recognition of seizures in these patients can be difficult, seizures in these patients tend to be highly responsive to pharmacological therapy. However, choosing the right antiepileptic drug can be a challenge and complicated by altered kinetics and polypharmacy. While ongoing seizures can worsen the cognitive status in these patients, antiepileptic drugs could also add to the cognitive burden. The newer generation drugs show promise in terms of their side effect profile without compromising on the efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dementia is an acquired disorder characterized by a chronic decline in cognition in one or more cognitive domains. About 3–6 % of patients over 60 years of age develop dementia [1–3]. The incidence increases with age, and after 60 years of age, there is a doubling of prevalence with every 5 years of increase in age [4–6]. Based on presumed etiology and mechanism, dementia has been broadly classified into two main categories: primary (degenerative) and secondary (symptomatic) type [7]. Selective neuronal loss occurring in functionally connected areas is the mechanism behind primary degenerative dementias. Typical examples of this include Alzheimer’s dementia (AD) and Lewy body dementia (LBD). Secondary dementias occur with conditions like direct tissue damage, raised intracranial pressure or as a consequence of dysfunction from endocrine, toxic, or metabolic conditions. A classification of dementia based on etiology has been described in detail by Emre et. al. [7]. Though the exact prevalence of specific subtypes of dementia is not very clear, the top three types, namely AD, LD, and vascular dementia (VD), likely compose the majority of all cases of dementia.
Incidence of epilepsy is bimodal with a second peak happening in the elderly. Nearly 25 % of new onset seizures happen in patients over 65 years of age [8]. Neurodegenerative conditions are an important etiologic factor causing about 10 % of new onset seizures in the elderly [9••, 10]. Of these, dementia, especially AD disease, has been shown to be associated with an increased risk for unprovoked seizures [9••]. In addition, following an obvious precipitating event like stroke, patients with dementia are more susceptible to developing seizures than controls [11]. Moreover, seizures in these patients do not appear to be merely an epiphenomenon but actually contribute to worsening cognition [12]. A study that surveyed institutionalized patients with AD found a worsening cognitive status following the onset of seizures [13]. Data from animal studies has illuminated our understanding on how epileptiform abnormalities and seizures may be involved early in the pathogenesis of cognitive abnormalities and could potentially be a disease-modifying target in the management of these patients [14, 15].
Elderly with dementia have preexisting social problems secondary to cognitive decline, such as loss of independence. Seizures in this setting can further worsen the quality of life and add to care giver burden [8, 16]. In addition, the prolonged postictal period seen in these patients would further complicate care and increase risk for accidents and injuries [8, 17]. In this review article, we will first discuss the incidence of seizures in patients with dementia and the proposed mechanisms behind this. We will then discuss management of seizures in the elderly with special attention to drug therapy. While we attempt to discuss seizures in dementia as a group, readers are cautioned to the fact that most of the literature is from patients with AD and there is a real paucity of data regarding seizures in other forms of dementia.
Incidence and seizure types in patients with dementia
Despite the increasing prevalence of dementia, few studies have actually looked into the incidence of seizures among the various subtypes of dementia. A recent study from the UK looked at the incidence of seizures in patients aged over 65 years with a diagnosis of either AD or VD. Age-matched patients without dementia were used as control in this study [18]. This study found an increased incidence of seizures in patients with both AD and VD, 5.6/1000 person-years (PY) and 7.5/1000 PY respectively, as opposed to 0.8/1000 PY in the control population. Sherzai et al. analyzed data from the Nationwide Inpatient Sample between 1999 and 2008 and found that patients with AD were three times more likely, while non-alzheimer's dementia (NAD) patients were twice as likely to have seizures when compared with controls (OR of 3.07 [95 % CI = 2.98–3.16] and 2.20 [95 % CI = 2.14–2.27]) [19•]. An earlier study which looked at the Rochester residents aged 55 years and older also found that both AD and NAD are associated with an increase in incidence of seizure [20]. Neither of the above studies differentiate among the subtypes of NAD. Most of the other data that we have stems forth from study of patients with AD, likely due to its higher prevalence. Data on the incidence of seizures in other forms of dementia is rather sparse [4]. Of note, most of the studies on patients with AD have used NINCDS-ADRDA criteria, and only a few of their patients had a pathological confirmation of the cause of dementia [9••]. Though the criteria are sensitive, there is a likelihood of commixture of other types of dementia.
Hesdorffer et al. showed that the diagnosis of dementia and AD is associated with a sixfold increase in incidence of seizures [20]. Their finding was similar to that of an earlier study by Romanelli et al. [21]. A prospective study that followed patients with a diagnosis of AD for about 8 years showed the cumulative incidence of seizures to be about 7.75 % and a yearly unprovoked seizure incidence of about 1 % [14]. However, a follow-up of this study that looked at a larger cohort of patients found a lower than expected incidence of 1.5 %. However, in this study, a significant number of patients had events, which were of uncertain etiology. These could potentially represent seizures, and if these were included in the calculation, the incidence was as high as 13 % [22]. Notwithstanding the above examples, literature is flooded with widely differing incidence rates. Studies quote that 1–64 % of patients with AD have at least one unprovoked seizure [9••]. Many of the studies are small and the others differ in characterization of dementia and seizures. In addition, selection bias, inclusion of patients with other symptomatic causes for seizures, and lack of control for medications taken by the patients are some other factors likely contributing to the differences seen [9••].
Predictive factors for seizure occurrence in patients with dementia
Enquiry into factors predicting the occurrence of seizures again reveals significant controversy. Earlier studies in this area saw a correlation between duration of dementia with seizure incidence [4, 9••, 20, 23]. Recent study by Imfeld et al. also showed a trend for longer duration of AD to be associated with seizure incidence, though this finding was not statistically significant [18]. In contrast to this, several of the recently published articles have found that younger patients with dementia are more prone to developing seizures [19•, 22]. A unifying explanation to the seeming inconsistency regarding age would be a correlation between disease severity and seizure incidence [9••]. Along the same lines of argument, patients with early onset dementia tend to have a swift progression of the disease. Consistent with this hypothesis, Irizarry et al. found on analysis of clinical trials data that patients with greater cognitive impairment had a higher incidence of seizures [24•]. However, there is data to dispute even this hypothesis [14, 25]. In the study by Amatniek et al., African-American ethnicity and epileptiform findings on electroencephalogram (EEG) were found to be predictive of seizure incidence [14]. However, considering the small sample size of this study, the findings of difference in incidence with race may not be generalizable.
Seizure types in patients with dementia
Most of the earlier studies in patients with dementia have suggested that generalized convulsive seizures are the most common type [12, 20, 21]. In the prospective study by Scarmeas et al., six of the seven patients with definite seizures had generalized convulsions. Besides these patients, 36 patients had events that were of uncertain etiology. These potentially could have been complex partial seizures (CPS)[22]. The study by Bernardi et al. also showed that CPS with secondary generalization was the most common seizure type [26]. CPS in these patients most commonly manifest as confusion spells (dyscognitive) with minimal motor manifestations and hence can be difficult to distinguish from behavioral changes and are highly likely to go unrecognized [8]. As a consequence to the above, the reported incidence of CPS in these patients is likely a gross underestimation accounting for the discrepancy in incidence between the studies.
Pathophysiology
Though the higher incidence of seizures in dementia has been known for a while, the mechanisms underlying this process have been merely speculative. Structural changes, especially in the mesial temporal lobes, including neuronal loss and gliosis may play an etiologic role in this process. In fact, several observers have seen an increase in the incidence of hippocampal sclerosis in the elderly people with dementia [27, 28]. Data from animal studies shows that accumulating amyloid beta protein (Abeta) can in and of itself elicit epileptiform abnormalities even in the absence of neurodegeneration [25]. Abeta has been shown to alter neuronal membrane properties and make pyramidal cells hyperexcitable [29]. Moreover, EEG monitoring of mice that have overexpression of Abeta has epileptiform abnormalities and unprovoked seizures. Along the lines of this finding, in the study by Scarmeas et al., all the dementia patients who developed seizures during the course of the study, at autopsy, showed Alzheimer’s type pathology with no evidence for hippocampal sclerosis. There is an increased incidence of seizures in familial forms of AD, and patients with Down’s syndrome have an increase in prevalence of seizures with age [9••, 14, 30]. These conditions are associated with either an increase in Abeta or increased aggregation of Abeta, suggesting a causative role of this in seizures [25].
Apolipoprotein E (Apo(E)) is a known risk factor for dementia of Alzheimer’s type. This lipoprotein has also been shown to increase neuronal membrane excitability [25]. Patients with Apo(E) appear to have a greater incidence of epileptiform abnormalities [31], and temporal lobe epilepsy (TLE) patients with apo(E) positivity have been shown to have worse seizures and memory impairment.
New data from animal experiments also proposes a more central role for seizures and epileptiform activity in the pathogenesis of cognitive dysfunction. In the mice model of AD, a host of inhibitory responses occurs in response to the high levels of epileptiform abnormalities, such as sprouting of inhibitory terminals and synaptic protein changes [25]. In turn, these changes were shown to lead to cognitive decline in these mice [32]. Further, knocking out tau in these animals, which blocks the excitatory effects of Abeta, revokes the changes seen above including the cognitive decline [33]. This illustrates that seizures in AD may actually be involved early in the disease process and contributes to the pathogenesis of cognitive abnormalities. A corollary that follows this assumption is that control of the hyperexcitability in this population could at least slow down the cognitive decline in these patients. This hypothesis will need further testing in the human population.
Treatment
Seizures in the elderly can present just as a confusion spell. Unlike the younger population, the motor manifestations are usually lacking, and the confusion tends to be protracted with a waxing and waning quality [34, 35]. These features tend to make the diagnosis difficult, requiring a high index of suspicion. While the basic principles of seizure management in the elderly are similar to the rest of the population, significant differences do exist. The most important initial step in management is to rule out acute symptomatic seizures (seizures due to a recent acute cause) and other etiologies that tend to resemble seizures such as syncope, arrhythmias, metabolic disturbances, transient ischemic attack (TIA), transient global amnesia (TGA), and psychogenic disorders. This requires a careful history of the event, comorbidities, and medication use and could prove to be much more challenging in the elderly than in the young [8]. History taking in these patients could be rather demanding secondary to memory deficits of the patient. The fact that many of these patients are institutionalized and have limited social interactions further decreases the probability of finding a witness [34]. Additional recommended investigations would include obtaining an EEG, lab work to rule out toxic and metabolic etiologies, and imaging studies, preferably a magnetic resonance imaging (MRI). Evaluation of the need for treatment should follow this. Only patients with a second seizure or who have a high risk for recurrent seizures should be treated. As mentioned previously, the tangible predictive factors for seizure recurrence in this population are still a matter of debate. However, studies point to the severity of dementia and the presence of epileptiform abnormalities on EEG to be moderately predictive of seizure recurrence [14, 15, 22]. In addition to the above recommendations, an empiric treatment may be warranted at times despite negative investigations, if the index of suspicion is rather high. It would be prudent to choose an antiepileptic drug with minimal cognitive effects in this scenario.
EEG findings in dementia
EEG is commonly obtained following a seizure both in the outpatient and in-hospital settings. Most of the EEG findings in dementia are nonspecific and primarily serve to rule out other causes for the decrease in cognition. In fact, EEG tends to be normal in the earlier stages of AD, and the ability of EEG to differentiate between the different subsets of dementia is also rather limited [36]. AD in moderate stages is associated with a slowing down of the posterior dominant rhythm and an increase in theta during wakefulness [36]. There is worsening of the slowing with advancing dementia. Triphasic looking waves with posterior predominance has been reported in advanced stages of dementia [36, 37]. Epileptiform abnormalities are usually sparse in this population of patients even if they continue to have seizures [22]. Prolonged video EEG or ambulatory EEGs can significantly increase the yield of capturing epileptiform abnormalities but remains an underused investigation [38].
Pharmacokinetic changes with aging
One of the major factors to take in to account while choosing an antiepileptic drug (AED) is the pharmacokinetic changes that happen with aging. Almost every aspect of drug physiology, namely absorption, distribution, metabolism, and excretion changes with age. Some AEDs like phenytoin are highly susceptible to these effects, and its levels in the elderly can fluctuate as much as tenfold [39, 40]. Reduced gastric motility and blood flow coupled with low gastric acid production can vary the absorption of acidic and alkaline drugs [34]. The absorption of highly water-insoluble drugs like phenytoin or carbamazepine can be dependent on the hydration status of the patient, with poor hydration contributing to decreases in absorption. The normal aging process is usually associated with a decrease in total protein, albumin, and altered protein binding [4]. The protein binding of the drugs can be further altered in the presence of hepatic and renal disease. A decrease in the lean body mass and increase in fat stores also tends to change the volume of distribution of the AEDs, especially the fat soluble ones. The highly lipophilic drugs like barbiturates and benzodiazepines, as a result, tend to get concentrated in the fat stores and have a prolonged duration of action. Hepatic mass, blood flow, and drug metabolism appear to decrease by about 10 %, every decade after 40 years. The oxidative reactions catalyzed by the cytochrome P450 (CYP 450) enzyme system appear to be particularly affected. Metabolism of drugs, those that are heavily dependent on this mechanism such as phenytoin, phenobarbital, valproic acid, carbamazepine, oxcarbazepine, lamotrigine, benzodiazepines, and tiagabine, could potentially be delayed, especially in the presence of hepatic disease [4]. A similar decrease in renal clearance of drugs has also been reported secondary to the decrease in glomerular filtration rate (GFR) with age. Drugs that primarily depend on renal function for excretion are gabapentin, levetiracetam, and topiramate [38]. In general, it would be wise to titrate drugs slowly in the elderly with close monitoring of levels and side effects.
Antiepileptic drug therapy
The present-day offers a wide array of AEDs to choose from. Very few studies have compared head to head the tolerability and efficacy of the newer to older generation AEDs in the elderly population. There is very little data that is dementia specific. A VA cooperative study randomized patients 60 years and older with new onset seizures to gabapentin, lamotrigine, or carbamazepine [41]. At the end of 1 year, patients on lamotrigine showed best retention, while those on carbamazepine showed the worst. Patients in this study dropped out primarily secondary to intolerance than differences in efficacy between the drugs. An earlier study by Brodie et al. showed a similar finding with patients on carbamazepine having a higher dropout rate than lamotrigine [42].
Data on the actual efficacy of antiepileptic drugs is scant. However, the available data appears to show that seizures in this population are likely to be easily controlled [1, 9••, 43]. A retrospective review of patients with neurodegenerative diseases showed that their response to AEDs is actually better than that seen in the general population [1]. Another small study looked at the response to levetiracetam monotherapy in patients with new-onset seizures and AD. 72 % of these patients were seizure free at the end of 1 year [43]. However, long-term data on prognosis is not available. Available data appears to show that the newer generation AEDs are equally as effective as the older generation drugs, if not better. In the VA cooperative study, there were no statistically significant differences in the efficacy between the AEDs [41]. Even in the study by Brodie et al. quoted above, lamotrigine appeared to show a greater efficacy in terms of seizure control at 16 weeks [42]. It is conceivable then that side effect profile of medications and drug-drug interactions would have a more significant role to play in drug selection.
A possibility that still remains underexplored is the appropriate antiepileptic drug which can potentially have beneficial effects in patients with dementia. The older generation drug valproic acid has been known to have some mood stabilizing effect in addition to the antiepileptic properties. In addition, studies have quoted some theoretical advantages to the use of this drug in patients with AD based on properties such as histone deacetylase inhibition. However, the drug also has a theoretical concern of worsening AD by influencing insulin sensitivity [44]. Moreover, a small study that looked at its efficacy in controlling aggression and agitation in AD did not find it effective [45]. The concern for worsening of disease and the poor tolerability does not make it a drug of choice in treating elderly patients [44]. Levetiracetam has already been shown to be better tolerated and efficacious in management of seizures in patients with AD [43]. A recent paper has shown that lacosamide, through effects on collapsin-response mediator protein (CRMP) can potentially decrease axonal sprouting following traumatic brain injury in rats [46]. This process could theoretically decrease epileptogenesis, and in lieu of the theory that inhibitory axonal sprouting may account for the cognitive problems seen, this drug may help modify the disease process in AD [47]. The clinical implication of this is yet to be seen. Another small study showed that treatment of AD patient with lamotrigine leads to improvement in cognition and mood. The authors propose that this is likely due to the antiglutamatergic effect of this drug [48].
Adverse effects of antiepileptic drugs
As detailed above, the adverse effects of the AEDs are likely to play a primary role in drug selection. The adverse effects of the antiepileptic drugs commonly used in the elderly are listed in Table 1. Saving some common side effects and idiosyncratic reactions, most of the long-term consequences appear to stem forth from the hepatic enzyme induction property of the older and some newer generation antiepileptic drugs [49••]. These adverse effects commonly manifest as bone problems, drug-drug interactions, and increase in markers of cardiovascular risk. Elderly patients with dementia may be especially susceptible to these effects owing to their lifestyle and polypharmacy. These will be discussed in detail below.
Antipsychotics and antidepressants are commonly used in patients with dementia. Most of the commonly used medications in the above class of drugs are metabolized by the Cytochrome P 450 (CYP) enzyme system. Several studies have now shown that the serum concentration of these drugs can be markedly lowered by the enzyme-inducing AEDs, sometimes as much as 60 % [49••, 50]. Conversely, when such an inducing AED is withdrawn, it can lead to toxicity from the antipsychotics or antidepressants. Significant cognitive effects can result from changes in the blood level of these medications, especially in elderly with dementia. In addition, most of the cancer chemotherapeutic agents also suffer the same fate of increased metabolism describe above. This is also important to take into consideration, as the elderly have an increased incidence of brain tumors [51, 52]. Addition of a new medication in the elderly on enzyme-inducing agents or changes in dosage should take the above interactions in to consideration.
Patients with epilepsy are at a higher risk for fractures [49••, 53, 54]. This is especially true when patients are on enzyme-inducing antiepileptic drugs as suggested by a reduced bone mineral density (BMD) in these patients [55]. Despite some controversy in the literature regarding the mechanism behind this, augmented metabolism of vitamin D and the resulting hyperparathyroidism and speedy bone turnover is believed to be the contrivance behind the bone pathology [53]. Elderly with dementia are likely to have limited sun exposure and exercise which makes them highly vulnerable to bone problems. Enzyme induction with the older generation AEDs would greatly add to this preexisting burden. This coupled with instability and dizziness that is a common adverse effect of several AEDs significantly increases their fracture risk. Another consequence of enzyme induction is the effect on markers of cardiovascular risk. Patients on enzyme-inducing AEDs are at increased risk for having high serum cholesterol, low-density lipoprotein (LDL), and triglycerides. Other markers of cardiovascular risk such as lipoprotein(a), homocysteine, and C-reactive protein (CRP) have also been shown to be similarly increased in patients on enzyme inducers [49••, 56]. These effects gain special importance in the elderly who are already at an increased risk for cardiovascular disease because of their age.
When considering the side effects, the cognitive effects of certain AEDs deserve a special mention [4]. Though, with common use, most of these medications are usually well-tolerated with mild cognitive effects, elderly with dementia tend to be more susceptible to these effects [4, 57]. The older generation AEDs like phenytoin, valproic acid, carbamazepine, and phenobarbital appear to have more cognitive effects than the new-generation agents. Of the newer generation drugs, topiramate has been shown to affect verbal memory, cognitive speed, and attention [4]. In general, newer generation non-enzyme-inducing medications would be a judicious first choice, especially since there appears to be no significant differences in efficacy.
Medications used in dementia that can potentially worsen seizures
Treatment of dementia and related comorbidities can potentially induce or worsen seizures. Though this remains a theoretical concern, very few studies have actually looked into this probability. Cholinergic agonists have been known to induce seizures in animal models [9••, 58]. Some case reports, drug registry data, and at least one small pilot study done on patients with epilepsy expressed this concern [58]. However, a randomized double-blinded study to evaluate improvement in memory in patients with epilepsy did not find an increase in seizure frequency with the use of donepezil [59]. However, the brain of patients with dementia may react differently to these medications. Memantine is a N-methyl-d-aspartate (NMDA) receptor antagonist used in the treatment of mild to moderate AD. Some case reports exist which show an increase in incidence of seizures when patients are treated with memantine [60]. A review of patient data from various clinical trials showed an association between seizures and memantine use in univariate analysis [24•]. In contrast, there is animal data to suggest that memantine can have antiepileptic properties [9••, 61, 62]. A recent study that aimed to identify the incidence of seizures among patients with dementia aged 65 years and older did not find any difference in seizure incidence with treatment with either acetylcholinesterase inhibitors (AChEI) or memantine [18]. Clearly, larger studies are needed to further evaluate the above concerns.
Antidepressants and antipsychotics are other medications that are used commonly in patients with dementia, especially at advanced stages. The data for most of the newer generation antidepressants and antipsychotics in therapeutic doses appears to be safe from a seizure perspective with only a marginal increase in the risk of seizure incidence over general population [63]. An exception among the newer generation antidepressants to this general rule is bupropion [64, 65]. Of the older generation antidepressants, maprotiline, amoxapine, and clomipramine also appear to be associated with a higher risk for seizure occurrence. Amongst the antipsychotics, chlorpromazine and clozapine appear to be most seizurogenic. In the pooled analysis of dementia patients from various clinical trials described above, patients on antipsychotics had a higher incidence of seizures [24•]. The study however did not look at medication-specific incidences. Notwithstanding the above general principles, elderly patients with dementia could be more susceptible to the adverse effects from these medications, which should promote a gradual and slow up titration of these medications [66].
Summary
Patients with dementia are at an increased risk for seizures. Recognition and treatment of seizures in this population are important and likely could improve their cognitive status. For the most part, seizures in these patients appear to be easy to control, and the choice of antiepileptic drug would be heavily influenced by their side effect profile and drug-drug interactions. The field is unfortunately beset by a paucity of studies. The need for more studies in this field cannot be overemphasized especially with the predicted increase in the incidence of dementia. Studies are specifically needed to identify the incidence of seizures among the various subtypes of dementia, appropriate drug therapy, and the potential for other therapies to induce seizures.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rao SC, Dove G, Cascino GD, Petersen RC. Recurrent seizures in patients with dementia: frequency, seizure types, and treatment outcome. Epilepsy Behav. 2009;14(1):118–20.
Wang W, Wu S, Cheng X, Dai H, Ross K, Du X, et al. Prevalence of Alzheimer’s disease and other dementing disorders in an urban community of Beijing, China. Neuroepidemiology. 2000;19(4):194–200.
Rocca WA, Bonaiuto S, Lippi A, Luciani P, Turtù F, Cavarzeran F, et al. Prevalence of clinically diagnosed Alzheimer’s disease and other dementing disorders: a door-to-door survey in Appignano, Macerata Province. Italy Neurol. 1990;40(4):626–31.
Mendez M, Lim G. Seizures in elderly patients with dementia: epidemiology and management. Drugs Aging. 2003;20(11):791–803.
Drachman DA. If we live long enough, will we all be demented? Neurology. 1994;44(9):1563–5.
Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1–2):125–32.
Emre M. Classification and diagnosis of dementia: a mechanism-based approach. Eur J Neurol. 2009;16(2):168–73.
Ghosh S, Jehi LE. New-onset epilepsy in the elderly: challenges for the internist. Cleve Clin J Med. 2014;81(8):490–8.
Friedman D, Honig LS, Scarmeas N. Seizures and epilepsy in Alzheimer’s disease. CNS Neurosci Ther. 2012;18(4):285–94. A comprehensive literature review that discusses the incidence of seizures, seizure types, EEG findings and treatment in patients with Alzheimer’s dementia.
Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935-1984. Epilepsia. 1993;34(3):453–68.
Cordonnier C, Hénon H, Derambure P, Pasquier F, Leys D. Influence of pre-existing dementia on the risk of post-stroke epileptic seizures. J Neurol Neurosurg Psychiatry. 2005;76(12):1649–53.
McAreavey MJ, Ballinger BR, Fenton GW. Epileptic seizures in elderly patients with dementia. Epilepsia. 1992;33(4):657–60.
Volicer L, Smith S, Volicer BJ. Effect of seizures on progression of dementia of the Alzheimer type. Dementia. 1995;6(5):258–63.
Amatniek JC, Hauser WA, DelCastillo-Castaneda C, Jacobs DM, Marder K, Bell K, et al. Incidence and predictors of seizures in patients with Alzheimer’s disease. Epilepsia. 2006;47(5):867–72.
Larner AJ. Epileptic seizures in AD patients. Neuromolec Med. 2010;12(1):71–7.
Laccheo I, Ablah E, Heinrichs R, Sadler T, Baade L, Liow K. Assessment of quality of life among the elderly with epilepsy. Epilepsy Behav. 2008;12(2):257–61.
Theodore WH. The postictal state: effects of age and underlying brain dysfunction. Epilepsy Behav. 2010;19(2):118–20.
Imfeld P, Bodmer M, Schuerch M, Jick SS, Meier CR. Seizures in patients with Alzheimer’s disease or vascular dementia: a population-based nested case–control analysis. Epilepsia. 2013;54(4):700–7.
Sherzai D, Losey T, Vega S, Sherzai A. Seizures and dementia in the elderly: nationwide inpatient sample 1999-2008. Epilepsy Behav. 2014;36:53–6. A large retrospective study that looked at Nationwide Inpatient Sample and showed a higher incidence of seizures with AD and NAD.
Hesdorffer DC, Hauser WA, Annegers JF, Kokmen E, Rocca WA. Dementia and adult-onset unprovoked seizures. Neurology. 1996;46(3):727–30.
Romanelli MF, Morris JC, Ashkin K, Coben LA. Advanced Alzheimer’s disease is a risk factor for late-onset seizures. Arch Neurol. 1990;47(8):847–50.
Scarmeas N, Honig LS, Choi H, Cantero J, Brandt J, Blacker D, et al. Seizures in Alzheimer disease: who, when, and how common? Arch Neurol. 2009;66(8):992–7.
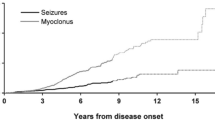
Risse SC, Lampe TH, Bird TD, Nochlin D, Sumi SM, Keenan T, et al. Myoclonus, seizures, and paratonia in Alzheimer disease. Alzheimer Dis Assoc Disord. 1990;4(4):217–25.
Irizarry MC, Jin S, He F, Emond JA, Raman R, Thomas RG, et al. Incidence of new-onset seizures in mild to moderate Alzheimer disease. Arch Neurol. 2012;69(3):368–72. Large study that looked at pooled data from 10 Alzheimer disease cooperative study clinical trials to identify the incidence of seizures.
Palop JJ, Mucke L. Epilepsy and cognitive impairments in Alzheimer disease. Arch Neurol. 2009;66(4):435–40.
Bernardi S, Scaldaferri N, Vanacore N, Trebbastoni A, Francia A, D’Amico A, et al. Seizures in Alzheimer’s disease: a retrospective study of a cohort of outpatients. Epileptic Disord. 2010;12(1):16–21.
Blass DM, Hatanpaa KJ, Brandt J, Rao V, Steinberg M, Troncoso JC, et al. Dementia in hippocampal sclerosis resembles frontotemporal dementia more than Alzheimer disease. Neurology. 2004;63(3):492–7.
Dickson DW, Davies P, Bevona C, Van Hoeven KH, Factor SM, Grober E, et al. Hippocampal sclerosis: a common pathological feature of dementia in very old (> or = 80 years of age) humans. Acta Neuropathol. 1994;88(3):212–21.
Minkeviciene R, Rheims S, Dobszay MB, Zilberter M, Hartikainen J, Fülöp L, et al. Amyloid beta-induced neuronal hyperexcitability triggers progressive epilepsy. J Neurosci. 2009;29(11):3453–62.
Lai F, Williams RS. A prospective study of Alzheimer disease in down syndrome. Arch Neurol. 1989;46(8):849–53.
Ponomareva NV, Selesneva ND, Jarikov GA. EEG alterations in subjects at high familial risk for Alzheimer’s disease. Neuropsychobiology. 2003;48(3):152–9.
Palop JJ, Jones B, Kekonius L, Chin J, Yu GQ, Raber J, et al. Neuronal depletion of calcium-dependent proteins in the dentate gyrus is tightly linked to Alzheimer’s disease-related cognitive deficits. Proc Natl Acad Sci U S A. 2003;100(16):9572–7.
Roberson ED, Scearce-Levie K, Palop JJ, Yan F, Cheng IH, Wu T, et al. Reducing endogenous tau ameliorates amyloid beta-induced deficits in an Alzheimer’s disease mouse model. Science. 2007;316(5825):750–4.
Jenssen S, Schere D. Treatment and management of epilepsy in the elderly demented patient. Am J Alzheimers Dis Other Demen. 2010;25(1):18–26.
Sheth RD, Drazkowski JF, Sirven JI, Gidal BE, Hermann BP. Protracted ictal confusion in elderly patients. Arch Neurol. 2006;63(4):529–32.
Jenssen S. Electroencephalogram in the dementia workup. Am J Alzheimers Dis Other Demen. 2005;20(3):159–66.
Primavera A, Traverso F. Triphasic waves in Alzheimer’s disease. Acta Neurol Belg. 1990;90(5):274–81.
Waterhouse E, Towne A. Seizures in the elderly: nuances in presentation and treatment. Cleve Clin J Med. 2005;72 Suppl 3:S26–37.
Birnbaum A, Hardie NA, Leppik IE, Conway JM, Bowers SE, Lackner T, et al. Variability of total phenytoin serum concentrations within elderly nursing home residents. Neurology. 2003;60(4):555–9. Erratum in: Neurology. 2003 May 27;60(10):1727.
Hayes MJ, Langman MJ, Short AH. Changes in drug metabolism with increasing age: 2. phenytoin clearance and protein binding. Br J Clin Pharmacol. 1975;2(1):73–9.
Rowan AJ, Ramsay RE, Collins JF, Pryor F, Boardman KD, Uthman BM, et al. VA cooperative study 428 group. new onset geriatric epilepsy: a randomized study of gabapentin, lamotrigine, and carbamazepine. Neurology. 2005;64(11):1868–73.
Brodie MJ, Overstall PW, Giorgi L. Multicentre, double-blind, randomized comparison between lamotrigine and carbamazepine in elderly patients with newly diagnosed epilepsy. the UK Lamotrigine Elderly Study Group. Epilepsy Res. 1999;37(1):81–7.
Belcastro V, Costa C, Galletti F, Pisani F, Calabresi P, Parnetti L. Levetiracetam monotherapy in Alzheimer patients with late-onset seizures: a prospective observational study. Eur J Neurol. 2007;14(10):1176–8.
Borhani Haghighi A, Sabayan B. Can prolonged administration of valproic acid put patients with epilepsy at higher risk for development of Alzheimer’s disease? Epilepsy Behav. 2008;12(1):206–7.
Herrmann N, Lanctôt KL, Rothenburg LS, Eryavec G. A placebo-controlled trial of valproate for agitation and aggression in Alzheimer's disease. Dement Geriatr Cogn Disord. 2007;23(2):116-9.
Wilson SM, Ki Yeon S, Yang XF, Park KD, Khanna R. Differential regulation of collapsin response mediator protein 2 (CRMP2) phosphorylation by GSK3ß and CDK5 following traumatic brain injury. Front Cell Neurosci. 2014;8:135.
Wilson SM, Khanna R. Specific binding of lacosamide to collapsin response mediator protein 2 (CRMP2) and direct impairment of its canonical function: implications for the therapeutic potential of lacosamide. Mol Neurobiol. 2014;20.
Tekin S, Aykut-Bingöl C, Tanridağ T, Aktan S. Antiglutamatergic therapy in Alzheimer’s disease–effects of lamotrigine. Short Commun J Neural Transm. 1998;105(2–3):295–303.
Brodie MJ, Mintzer S, Pack AM, Gidal BE, Vecht CJ, Schmidt D. Enzyme induction with antiepileptic drugs: cause for concern? Epilepsia. 2013;54(1):11–27. Very good review article discussing the metabolic consequences of the enzyme inducing AEDs and their pathogenesis.
Spina E, Perucca E. Clinical significance of pharmacokinetic interactions between antiepileptic and psychotropic drugs. Epilepsia. 2002;43 Suppl 2:37–44.
Sundaram MB. Etiology and patterns of seizures in the elderly. Neuroepidemiology. 1989;8(5):234–8.
Stephen LJ, Brodie MJ. Epilepsy in elderly people. Lancet. 2000;355(9213):1441–6.
Pack AM, Morrell MJ, Randall A, McMahon DJ, Shane E. Bone health in young women with epilepsy after one year of antiepileptic drug monotherapy. Neurology. 2008;70(18):1586–93.
Vestergaard P, Tigaran S, Rejnmark L, Tigaran C, Dam M, Mosekilde L. Fracture risk is increased in epilepsy. Acta Neurol Scand. 1999;99(5):269–75.
El-Hajj Fuleihan G, Dib L, Yamout B, Sawaya R, Mikati MA. Predictors of bone density in ambulatory patients on antiepileptic drugs. Bone. 2008;43(1):149–55.
Mintzer S, Skidmore CT, Abidin CJ, Morales MC, Chervoneva I, Capuzzi DM, et al. Effects of antiepileptic drugs on lipids, homocysteine, and C-reactive protein. Ann Neurol. 2009;65(4):448–56.
Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852–7.
Fisher RS, Bortz JJ, Blum DE, Duncan B, Burke H. A pilot study of donepezil for memory problems in epilepsy. Epilepsy Behav. 2001;2(4):330–4.
Hamberger MJ, Palmese CA, Scarmeas N, Weintraub D, Choi H, Hirsch LJ. A randomized, double-blind, placebo-controlled trial of donepezil to improve memory in epilepsy. Epilepsia. 2007;48(7):1283–91.
Savić A, Mimica N. Two cases of loss of consciousness after long-term memantine treatment. J Am Med Dir Assoc. 2013;14(5):375–6.
Creeley CE, Wozniak DF, Nardi A, Farber NB, Olney JW. Donepezil markedly potentiates memantine neurotoxicity in the adult rat brain. Neurobiol Aging. 2008;29(2):153–67.
Dhir A, Chopra K. Memantine delayed N-methyl-D-aspartate-induced convulsions in neonatal rats. Fundam Clin Pharmacol. 2014.
Pisani F, Oteri G, Costa C, Di Raimondo G, Di Perri R. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25(2):91–110.
Montgomery SA. Antidepressants and seizures: emphasis on newer agents and clinical implications. Int J Clin Pract. 2005;59(12):1435–40.
Johnston JA, Lineberry CG, Ascher JA, Davidson J, Khayrallah MA, Feighner JP, et al. A 102-center prospective study of seizure in association with bupropion. J Clin Psychiatry. 1991;52(11):450–6.
Franson KL, Hay DP, Neppe V, Dahdal WY, Mirza WU, Grossberg GT, et al. Drug-induced seizures in the elderly. causative agents and optimal management. Drugs Aging. 1995;7(1):38–48.
Compliance with Ethics Guidelines
Conflict of Interest
Kartik Sivaraaman and Vimala S. Vajjala declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Epilepsy
Rights and permissions
About this article
Cite this article
Sivaraaman, K., Vajjala, V.S. Seizures in Setting of Dementia. Curr Treat Options Neurol 17, 16 (2015). https://doi.org/10.1007/s11940-015-0342-9
Published:
DOI: https://doi.org/10.1007/s11940-015-0342-9