Opinion statement
Pyridoxine-dependent epilepsy (PDE) is a rare autosomal recessive disorder and is considered as a prototypical form of metabolic epilepsy. Characterized by recurrent seizures in the prenatal, neonatal, and/or postnatal periods that are resistant to conventional anti-epileptic drugs, PDE is responsive to pharmacological dosages of pyridoxine. Presently, however, there are no clear dose recommendations for long-term treatment. While pyridoxine supplementation is the first line of treatment and should be initiated in all confirmed PDE patients at an early age, various other treatment strategies are emerging. These include a lysine-restricted diet and arginine fortification. These will be discussed in light of current evidence, together with recommendations for best management of patients with this rare but treatable metabolic epilepsy, and future research and collaborative efforts, including the International PDE Consortium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pyridoxine-dependent epilepsy (PDE, MIM #266100) is a rare autosomal recessive disorder and is considered as a prototypical form of metabolic epilepsy. It is characterized by recurrent seizures in the prenatal, neonatal, and/or postnatal periods that are resistant to conventional anti-epileptic drugs (AED), but responsive to pharmacological dosages of pyridoxine [1••, 2]. Hunt et al. first described PDE in 1954 in a newborn with pharmaco-resistant seizures that were controlled immediately after parenteral administration of a multivitamin cocktail containing vitamin B6 [3]. In the more than six decades since, over 200 cases of PDE have been reported [4–8]. The point prevalence of PDE may vary from 1:20,000 to 1:600,000, based on the degree of systematic ascertainment via a therapeutic trial with pyridoxine [9–11]. The underlying genetic defect was identified in 2006 as mutations in ALDH7A1 resulting in the deficiency of α–aminoadipic semialdehyde dehydrogenase (antiquitin), which is involved in cerebral lysine catabolism (MIM #107323) [12]. Folinic acid-responsive seizures are caused by mutations in the same gene [13]. Antiquitin (ATQ) deficiency results in the accumulation of intermediate substrates arising from lysine degradation proximal to the deficient enzyme activity, including α –aminoadiphic semialdehyde (AASA), Δ-1-piperidine-6-carboxylate (P6C) and pipecolic acid (Fig. 1). Inactivation of pyridoxal 5’ phosphate (PLP) via chemical reaction with P6C is the pathophysiological mechanism of pyridoxine dependency [14••].
PDE typically presents within hours or days of birth with seizures that are refractory to AEDs. In some instances, seizures have been reported to occur intrauterine, with onset at the end of the last trimester. Late onset and other atypical forms of PDE, including infants whose seizures first respond to AEDs but relapse weeks to months later with refractory seizures, and patients whose seizures are not controlled by initial large doses of pyridoxine but which respond at a later time to a second trial, have also been reported in the literature [4, 15–18].
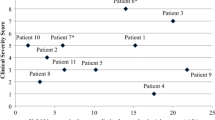
PDE patients have a heterogeneous clinical phenotype. The neonatal epileptic encephalopathy presentation may include gastrointestinal symptoms such as emesis and abdominal distention, sleeplessness, hyper-alertness, irritability, paroxysmal facial grimacing and abnormal eye movements. These striking findings are associated with recurrent partial motor seizures, generalized tonic seizures or myoclonus. Depending upon the phenotype, response (if any) to AEDs and timing of the initiation of pyridoxine supplementation, complex partial seizures, infantile spasms and other myoclonic seizures, as well as a mixed seizure pattern and recurrent status epilepticus, may develop [8, 19–22, 11]. Brain activity on EEG is non-specific, and can remain abnormal even with pyridoxine therapy [23]. PDE patients also have associated neurodevelopmental disabilities, ranging from mild to severe developmental delay/intellectual disability commonly affecting the domains of expressive language, along with a low-normal motor/performance IQ [4, 19, 20, 24]. Magnetic resonance imaging studies show different patterns, from white matter lesions, general cerebral atrophy, corpus callosum hypoplasia or dysplasia, to a structurally normal brain [25•, 26].
Clinical phenotypes of PDE can be classified into three groups: Group 1 consists of patients with complete seizure control, with pyridoxine and normal development; Group 2 consists of patients with complete seizure control with pyridoxine, but with developmental delay; and Group 3 consists of patients with persistent seizures and developmental delay despite pyridoxine. Despite extensive studies, correlations between the genotype and these phenotypic categories have not yet been established [1••, 27].
Patients presenting with unexplained early onset epilepsy and poor response to AEDs should be assessed for PDE. Situations under which PDE screening should be considered are clearly outlined by Stockler et al. [14••]. PDE diagnosis is based upon determination of AASA/P6C in urine, plasma and/or cerebral spinal fluid (CSF). Over time, pipecolic acid has proven less reliable than AASA for diagnosis, given its limited sensitivity and specificity. Thus, pipecolic acid is a secondary marker, and should only be used in conjunction with AASA. ALDH7A1 molecular analysis should be performed for diagnostic confirmation. If sequencing does not reveal point mutations, testing for insertions/deletions is indicated.
The differential diagnosis of neonatal epileptic encephalopathy is quite diverse and includes not only inborn errors of metabolism such as PDE, but also an array of other genetic conditions (single gene defects and chromosomal copy number variants), along with acquired disorders such as fetal or neonatal brain injury from maternal or postnatal infection, exposure to teratogens, pre-/perinatal hypoxia and/or ischemia, and intracerebral hemorrhage. High AASA is not only a distinctive characteristic for PDE. Elevated levels are also seen in patients with molybdenum cofactor deficiency and isolated sulfite oxidase deficiency, particularly in children with epileptic encephalopathy and atypical response to pyridoxine [28, 29]. Other forms of vitamin B6 responsive epilepsy include pyridoxamine 5′-phosphate oxidase (PNPO) deficiency, hyperprolinemia II (ALH4A1), and tissue non-specific alkaline phosphatase (TNSALP) deficiency. As patients with PNPO deficiency may present with a similar clinical phenotype, this rare metabolic disorder must also be kept in mind, and for patients with medically intractable neonatal seizures who do not respond to pyridoxine, a trial of pyridoxal phosphate (PLP) should also be instituted. Similarly, tissue non-specific alkaline phosphatase (TNSALP) deficiency must be considered in young patients with medically refractory neonatal or infantile seizures, particularly when signs of abnormal bone mineralization with or without low serum alkaline phosphatase are present; seizures in this condition improve on pyridoxine treatment [14••].
Treatment
For an overview of currently available treatments for PDE, the reader is referred to Table 1.
Pharmacological treatments
Pyridoxine
The standard treatment of PDE includes lifelong pyridoxine supplementation in pharmacologic doses. In an acutely seizing infant, an initial single—or more—100 mg dose of pyridoxine should be given intravenously without delay; given the risk of apneas, this should be administered in a controlled environment. Treatment with oral pyridoxine (15–30 mg/kg/day, divided in two to three doses) should be continued until negative biochemical or genetic testing excludes PDE.
At present, there are no clear dose recommendations for long-term treatment. In a regular diet, the recommended daily allowance for pyridoxine is 0.5 mg for infants and 2 mg for adults. In most patients with PDE, therapeutic pyridoxine dosages vary between 15 and 30 mg/kg/day in infants, or up to 200 mg/day in neonates and 500 mg/day in adults. Some patients respond to small doses. These oral dosages seem to be safe in long-term treatment. Higher pyridoxine doses may cause sensory, and rarely, motor neuropathy, which may be reversible [30, 31]. Nerve conduction studies are performed to exclude sensory neuropathy as an adverse effect of pyridoxine treatment. This test is performed either upon clinical evidence of neuropathy or as a regular monitoring (e.g., annually), in particular if high doses (>500 mg/day or >30 mg/kg/day) are used. Some patients experience breakthrough seizures during febrile illness. In these cases, higher (e.g., double) dosages may be given during the first 3 days of febrile illnesses.
Despite sufficient seizure control with oral pyridoxine, in most cases (80 %), long-term patient outcome with PDE remains poor, especially with respect to neurodevelopment [19, 27].
Prophylactic prenatal and postnatal treatment
Prenatal treatment of an at-risk or confirmed PDE fetus with supplemental pyridoxine given during pregnancy may prevent intrauterine seizures and improve neurodevelopmental outcome [32]. Prenatal treatment with high-dose pyridoxine followed by postnatal treatment was shown to be effective in preventing seizures, but failed to mitigate poor cognitive outcomes in two affected offspring in a family with a homozygous stop codon in exon 14 of ATQ (Y380X) [31]. In contrast, Bok et al. reported good developmental outcomes after prenatal treatment in three patients homozygous for the missense mutation in the same gene (E399Q) [33] when oral pyridoxine was given to pregnant women at a dosage of 100 mg/day from early pregnancy. The dosage of 100 mg pyridoxine/day seems to be safe, as it has been used for the treatment of hyperemesis gravidarum without fetal side effects [32].
Adverse effects, including increased seizure activity, have been seen in children with high pyridoxine or PLP intake [34, 35]. A neonate with a positive family history was on prophylactic intrauterine treatment with pyridoxine, and treatment was continued postnatally until PDE was ruled out. On day 15, while on treatment, the patient developed status epilepticus and encephalopathy. Upon receiving the final biochemical results, pyridoxine treatment was discontinued and his condition improved [36]. Thus, biochemical and genetic testing should be done as soon as possible, in order to limit unnecessary (high-dose) treatment with pyridoxine.
Pyridoxal phosphate
Some patients with medically refractory seizures and unresponsiveness to pyridoxine may respond to PLP. In most, PNPO deficiency has been identified as the underlying genetic condition [37, 38], but idiopathic PLP response can occur as well [39]. As PLP has the potential to treat both PNPO deficiency [40, 41] and PDE, some centers advocate its use (30 mg/kg/day divided into three doses) as the first line form of vitamin B6, while other centers advocate its consecutive use when pyridoxine, given over 3 consecutive days, has failed to control seizures [37]. In any case, treatment should be continued until results from metabolic investigations in urine, blood and CSF are available, as well as confirmation via molecular analysis of PNPO. As shown in animal experiments and communicated via anecdotal reports in humans, high PLP concentrations in the brain can lead to convulsions and liver damage [42].
Both vitamers (pyridoxine and PLP) are relatively inexpensive. However, PLP tablets cost six to ten times more than pyridoxine products and are less readily available in North America and the rest of the world [43]. Therefore, from a practical standpoint, local availability of PLP may determine how this particular vitamer is used and studied.
Folinic acid
Response to folinic acid was seen in patients who initially did not respond well to pyridoxine, but who later received a confirmed PDE diagnosis. However, the underlying mechanism for this has yet to be established. Folinic acid (3–5 mg/kg/day) may have a potential benefit as an add-on treatment in neonates, especially in the presence of incomplete pyridoxine responsiveness or breakthrough seizures. In older patients, 10–30 mg/day is recommended [13]. Whether long-term folinic acid provides benefit once the seizures are stabilized remains to be determined. High-dose folinic acid therapy can also exacerbate a seizure disorder and the clinical benefit must be closely monitored.
Diet intervention
Lysine-restricted diet
While treatment with pyridoxine compensates for chemical PLP inactivation, the accumulation of substrates from lysine degradation is not sufficiently reduced (Fig. 1). The presence of these potentially neurotoxic compounds could explain the partial efficacy of pyridoxine, as 75–80 % of patients suffer from developmental delay or intellectual disability (IQ < 70), despite excellent seizure control in the majority of patients [25•]. Standard treatment for inborn errors of metabolism affecting catabolic pathways of essential amino acids consists of substrate reduction for the deficient enzyme through dietary modification. Thus, for ATQ deficiency, dietary lysine restriction can reduce the accumulation of lysine-derived substrates and possibly contribute to the improvement of cerebral function (neurodevelopment, cognition, behavior, and seizure control).
Based on this rationale, an open-label observational study was conducted to test the effectiveness and safety of dietary lysine restriction as an adjunct to pyridoxine therapy on chemical biomarkers, seizure control, and developmental outcome in seven children with confirmed ATQ deficiency [44•]. The results from the study show that dietary lysine restriction (evidence level IV): 1) is tolerated without adverse events; 2) leads to significant decreases of potentially neurotoxic biomarkers in different body compartments; and 3) has potential benefit for seizure control and neurodevelopmental outcomes. The lysine-restricted diet is thus a promising add-on therapy for ATQ deficiency, with the potential to improve short-term and long-term clinical outcomes.
The evidence, however, remains limited, and as with any diet, lysine restriction poses a burden on patients and families, often in conflict with social and cultural traditions [45]. Also, such dietary treatment cannot be taken lightly: it requires monitoring by a specialist and metabolic dietician, with regular clinical follow-up, dietary protocols, and laboratory testing. Different effects can be expected based on the patient’s prenatal history, associated congenital brain abnormalities, genotype and other factors, and further study is required.
Based on the positive outcomes of this study, including the limited evidence level and experience with this burdensome diet, an international PDE Consortium developed and published consensus recommendations for implementation of lysine restriction along with monitoring and follow-up [46••]. Such standardization allows a systematic evaluation of the safety and effectiveness of this novel therapy, and helps to generate more solid evidence to substantiate its potential benefits.
In summary, every patient with confirmed ATQ deficiency treated with pyridoxine 15-30 mg/kg/day whose seizures are not well controlled and/or whose neurodevelopment is abnormal, is eligible for dietary lysine restriction, which can be initiated after baseline investigations. Its use is recommended throughout life. Lysine intake is based on the guidelines for Glutaric Aciduria type I by Kölker et al. [47], using both the World Health Organization (WHO) guidelines [48] and a paper by Yannicelli et al. [49] as additional references. These recommendations for age-dependent lysine restriction are detailed in the Consortium Recommendations paper [46••]. To allow for more precise and consistent lysine intake, a lysine prescription, rather than a simpler protein restriction, is recommended (at least during the initiation of the diet in the first year of life). Daily lysine intake should be managed to maintain the plasma lysine level within the lower normal reference range. In order to meet the recommended daily protein intake [48, 50], the diet may include commercially available, lysine-free amino acid formulas approved for use in conditions affecting lysine metabolism. Lysine-free amino acid formulas are often supplemented with vitamins and minerals in order to provide adequate or significant intake of these nutrients, and adequate supply of iron, minerals and vitamins must be confirmed by regular laboratory testing. Where lysine-free amino acid formulas are not used, vitamin and mineral supplement preparations must be added. Because limited amounts of high protein from the meat, fish and dairy food groups will be consumed, the use of fats and oils, carbohydrates and special low protein sources are often necessary to provide adequate caloric intake.
Safety monitoring at baseline and every 1–6 months thereafter (frequency depending on age and duration of treatment) includes measurement of lysine and branched-chain amino acids in plasma, albumin, pre-albumin, iron parameters, calcium, phosphate, 25-OH-vitamin D3, zinc, selenium, complete blood count, folic acid, and vitamin B12 in serum or plasma. Main outcomes include the biochemical parameters (PA and α-AASA levels in body fluids), seizure control and neurodevelopmental parameters.
In order to reduce the burden of the diet for patients and family/caregivers, an App has been developed to calculate lysine content, and to facilitate the management and monitoring the lysine-restricted diet, including documentation of food records. The App will be launched, free of charge, at the end of 2014 (www.pdeonline.org). The designers, in collaboration with Genetic Metabolic Dietitians International, Inc. (GMDI), aim to support patient families, and improve therapeutic adherence and thereby their experience, and ultimately disease outcomes.
Arginine fortification
Cerebral lysine influx and oxidation can be modulated by arginine, which competes with lysine for transport at the blood–brain barrier (cationic amino acid transporter 1, CAT1, which is one of three CATs that are called system y+) and the inner mitochondrial membrane (mitochondrial ornithine carriers, ORNT1 and ORNT2) [51]. It is hypothesized that arginine supplementation will compete with lysine, thereby reducing the excess lysine influx into the brain, which can lead to accumulation of the neurotoxic substrates caused by ATQ deficiency. The relationship between arginine fortification and plasma lysine has been proven in GA1 treatment, indicating that transport competition exists at both cerebrovascular and gastrointestinal barriers, suggesting that their co-administration is key to their efficacy.
Arginine fortification has proven safe as an add-on treatment to lysine restriction, as well as effective in improving outcomes in GA1 over the past 10 years [47, 52]. Following 12 months of arginine supplementation at 400 mg/kg/day, together with pyridoxine 200 mg/kg/day, a decrease in CSF α-AASA and improvement in general abilities, as well as verbal and motor functions, were reported [53]. These patients did not receive a lysine-restricted diet. In order to further restrict cerebral lysine influx, arginine supplementation of 150 mg/kg/day was initiated as triple therapy adjunct to the lysine-restricted diet and pyridoxine. This resulted in near normalization of urine AASA and plasma pipecolic acid, and improvement in developmental and cognitive domains, specifically in motor skills and speech. Furthermore, a decrease in brain lysine influx after arginine supplementation was noted [54].
Emerging therapies
Perez et al. provided proof-of-concept in cells for antisense therapy in PDE [2]. They reported the clinical, biochemical and genetic analysis of 12 unrelated patients with ATQ deficiency, including seven novel mutations changes. Transcriptional profile analysis showed the silent nucleotide change c.75C>T to be a novel splicing mutation creating a new donor splice site in exon 1. Antisense therapy of the aberrant mRNA splicing in a lymphoblast cell line harboring this mutation was successful, suggesting that this strategy may be a means of rescuing splice site changes in ALDH7A1 and preventing neurologic damage.
Conclusion and future directions
In conclusion, a therapeutic trial with pyridoxine should be performed in all patients with pharmaco-resistant epilepsies, until negative biochemical or genetic testing excludes PDE. Pyridoxine supplementation is the first line of treatment and should be initiated in all PDE patients at an early age. Therapeutic pyridoxine should be administered for life at dosages between15 and 30 mg/kg/day in infants, or up to 200 mg /day in neonates and 500 mg /day in adults, together with adequate safety monitoring. Prophylactic intrauterine treatment with supplemental pyridoxine in fetuses and neonates at risk of PDE can be considered for better outcomes; however, treatment exposure should be limited to the shortest possible interval so as to prevent any potential problems related to toxicity. Recently developed novel therapies based on the pathophysiology of PDE—i.e., lysine-restricted diet and arginine fortification—also provide potential treatment options.
Future research should focus on a better understanding of the phenotypic spectrum of PDE, its natural history, determination of the appropriate dose of pyridoxine supplementation (by both age and genotype-phenotype); the utility of the longitudinal measurements of levels of α-AASA and other biomarkers for disease management; the role of folinic acid in the treatment of PDE; and the effectiveness and long-term outcomes of a lysine-restricted diet and arginine fortification, along with optimal dosing of the different treatment regimens.
PDE, being a rare disease, poses some inherent challenges to research, which include small patient numbers spread around the world; under-diagnosis due to insufficient awareness; clinical heterogeneity; incomplete insight into the clinical spectrum and genotype–phenotype correlation; limited financial resources; and diverse specialists treating this metabolic epilepsy [55]. Suggested methods to overcome these roadblocks include establishment of a task force, the International PDE Consortium (www.pdeonline.org), to develop recommendations for treatment; use of digital tools and databases to unite patients and families, scientists and clinicians, and to facilitate knowledge dissemination; and novel trial methodologies with the simultaneous use of different study designs allowing inclusion of all patients, irrespective of age, severity, symptoms, and interventions.
Collaboration and sharing of data is of primary importance. To that end, we have established a longitudinal prospective ‘PDE patient registry’ (accessible viawww.pdeonline.org) that enables investigators to evaluate the utility of genotype, levels of biochemical markers, clinical neuropsychological studies and imaging modalities, thereby providing valuable insights into the natural history of PDE and improving the evidence for treatments.
Finally, novel approaches to early detection, and ultimately newborn screening, are being developed, such as the P6C measurement via dried bloodspot analysis [56]. Once implemented, this analysis will be instrumental in effectively determining the frequency of this treatable condition, while also providing an opportunity to initiate treatment immediately after birth, so as to prevent and control seizures, and ultimately limit brain damage in affected individuals.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance, •• Of major importance
Mills PB, Footitt EJ, Mills KA, et al. Genotypic and phenotypic spectrum of pyridoxine-dependent epilepsy (ALDH7A1 deficiency). Brain. 2010;133:2148–59. Publication providing a detailed overview of the genotypic and (wide!) phenotypic spectrum of patients with PDE due to ATQ deficiency, along with their response to vitamin B6 treatment.
Pérez B, Gutiérrez-Solana LG, Verdú A, et al. Clinical, biochemical, and molecular studies in pyridoxine-dependent epilepsy. Antisense therapy as possible new therapeutic option. Epilepsia. 2013;54:239–48.
Hunt AD, Stokes J, McCrory WW, Stroud HH. Pyridoxine dependency: report of a case of intractable convulsions in an infant controlled by pyridoxine. Pediatrics. 1954;13:140–5.
Baxter P. Pyridoxine dependent and pyridoxine responsive seizures. In: Baxter P, ed. Vitamin responsive conditions in paediatric neurology. London: MacKeith Press; 200. pp 109–65.
Gospe Jr SM. Current perspectives on pyridoxine-dependent seizures. J Pediatr. 1998;132:919–23.
Gospe Jr SM. Pyridoxine-dependent seizures: findings from recent studies pose new questions. Pediatr Neurol. 2002;26:181–5.
Gospe Jr SM. Neonatal vitamin-responsive epileptic encephalopathies. Chang Gung Med J. 2010;33:1–12.
Haenggeli C-A, Girardin E, Paunier L. Pyridoxine-dependent seizures, clinical and therapeutic aspects. Eur J Pediatr. 1991;150:452–5.
Ebinger M, Schultze C, Konig S. Demographics and diagnosis of pyridoxine-dependent seizures. J Pediatr. 1999;134:795–6.
Been JV, Bok LA, Andriessen P, et al. Epidemiology of pyridoxine dependent seizures in the Netherlands. Arch Dis Child. 2005;90:1293–6.
Baxter P. Epidemiology of pyridoxine dependent and pyridoxine responsive seizures in the UK. Arch Dis Child. 1999;81:431–3.
Mills PB, Struys E, Jakobs C, et al. Mutations in antiquitin in individuals with pyridoxine-dependent seizures. Nat Med. 2006;12:307–9.
Gallagher RC, Van Hove JL, Scharer G, et al. Folinic acid-responsive seizures are identical to pyridoxine-dependent epilepsy. Ann Neurol. 2009;65:550–6.
Stockler S, Plecko B, Gospe Jr SM, et al. Pyridoxine dependent epilepsy and antiquitin deficiency: clinical and molecular characteristics and recommendations for diagnosis, treatment and follow-up. Mol Genet Metab. 2011;104:48–60. Mini review on Pyridoxine Dependent Epilepsy that explains the clinical presentation, pathophysiology, mutational spectrum, diagnostic markers, along with methods for screening and diagnosis of PDE and the treatment options with follow-up strategy.
Bankier A, Turner M, Hopkins IJ. Pyridoxine dependent seizures-a wider clinical spectrum. Arch Dis Child. 1983;58:415–8.
Bass NE, Wyllie E, Cohen B, et al. Pyridoxine-dependent epilepsy: the need for repeated pyridoxine trials and the risk of severe electrocerebral suppression with intravenous pyridoxine infusion. J Child Neurol. 1996;11:422–4.
Coker S. Postneonatal vitamin B6-dependent epilepsy. Pediatrics. 1992;90:221–3.
Goutières F, Aicardi J. Atypical presentations of pyridoxine-dependent seizures: a treatable cause of intractable epilepsy in infants. Ann Neurol. 1985;17:117–20.
Basura GJ, Hagland SP, Wiltse AM, et al. Clinical features and the management of pyridoxine-dependent and pyridoxine-responsive seizures: review of 63 North American cases submitted to a patient registry. Eur J Pediatr. 2009;168:697–704.
Baxter P, Griffiths P, Kelly T, et al. Pyridoxine-dependent seizures: demographic, clinical, MRI and psychometric features, and effect of dose on intelligence quotient. Dev Med Child Neurol. 1996;38:998–1006.
Kluger G, Blank R, Paul K, et al. Pyridoxine-dependent epilepsy: normal outcome in a patient with late diagnosis after prolonged status epilepticus causing cortical blindness. Neuropediatrics. 2008;39:276–9.
Ohtsuka Y, Hattori J, Ishida T, et al. Long-term follow-up of an individual with vitamin B6-dependent seizures. Dev Med Child Neurol. 1999;41:203–6.
Nabbout R, Soufflet C, Plouin P, et al. Pyridoxinedependent epilepsy: a suggestive electroclinical pattern. Arch Dis Child Fetal Neonatal Ed. 1999;81:F125–9.
Baynes K, Tomaszewski Farias S, Gospe Jr SM. Pyridoxine-dependent seizures and cognition in adulthood. Dev Med Child Neurol. 2003;45:782–5.
Bok LA, Halbertsma FJ, Houterman S. Long-term outcome in pyridoxine-dependent epilepsy. Dev Med Child Neurol. 2012;54:849–54. Retrospective Study of PDE cohort of Dutch patients, evaluating the long-term outcome and correlations between patient characteristics and follow-up data.
Oliveira R, Pereira C, Rodrigues F, et al. Pyridoxine-dependent epilepsy due to antiquitin deficiency: achieving a favourable outcome. Epileptic Disord. 2013;15:400–6.
Scharer G, Brocker C, Vasiliou V, et al. The genotypic and phenotypic spectrum of pyridoxine-dependent epilepsy due to mutations in ALDH7A1. J Inherit Metab Dis. 2010;33:571–81.
Struys EA, Nota B, Bakkali A, et al. Pyridoxine-dependent epilepsy with elevated urinary α-amino adipic semialdehyde in molybdenum cofactor deficiency. Pediatrics. 2012;130:1716–9.
Mills PB, Footitt EJ, Ceyhan S, et al. Urinary AASA excretion is elevated in patients with molybdenum cofactor deficiency and isolated sulphite oxidase deficiency. J Inherit Metab Dis. 2012;35:1031–6.
McLachlan RS, Brown WF. Pyridoxine dependent epilepsy with iatrogenic sensory neuronopathy. Can J Neurol Sci. 1995;22:50–1.
Rankin PM, Harrison S, Chong WK, et al. Pyridoxine-dependent seizures: a family phenotype that leads to severe cognitive deficits, regardless of treatment regime. Dev Med Child Neurol. 2007;49:300–5.
Baxter P, Aicardi J. Neonatal seizures after pyridoxine use [letter]. Lancet. 1999;354:2082–3.
Bok LA, Been JV, Struys EA, et al. Antenatal treatment in two Dutch families with pyridoxine-dependent seizures. Eur J Pediatr. 2010;169:297–303.
Clayton PT. B6-responsive disorders: a model of vitamin dependency. J Inherit Metab Dis. 2006;29:317–26.
Hammen A, Wagner B, Berkhoff M, et al. A paradoxical rise of neonatal seizures after treatment with vitamin B6. Eur J Paediatr Neurol. 1998;2:319–22.
Hartmann H, Fingerhut M, Jakobs C, et al. Status epilepticus in a newborn treated with pyridoxine due to familial recurence risk for antiqutin deficiency-pyridoxine toxicity? Dev Med Child Neurol. 2011;53:1150–3.
Hoffmann GF, Schmitt B, Windfuhr M, et al. Pyridoxal 5′-phosphate may be curative in early-onset epileptic encephalopathy. J Inherit Metab Dis. 2007;30:96–9.
Bagci S, Zschocke J, Hoffmann GF, et al. Pyridoxal phosphate-dependent neonatal epileptic encephalopathy. Arch Dis Child Fetal Neonatal Ed. 2008;93:F151–2.
Wang H-S, Chou M-L, Hung P-C, et al. Pyridoxal phosphate is better than pyridoxine for controlling idiopathic intractable epilepsy. Arch Dis Child. 2005;90:512–5.
Mills PB, Camuzeaux SS, Footitt EJ, et al. Epilepsy due to PNPO mutations: genotype, environment and treatment affect presentation and outcome. Brain. 2014;137:1350–60.
Plecko B, Paul K, Mills P, et al. Pyridoxine responsiveness in novel mutations of the PNPO gene. Neurology. 2014;82:1425–33.
Kouyoumdjian JC, Ebadi J. Anticonvulsant activity of muscimol and gamma-aminobutyric acid against pyridoxal phosphate-induced seizures. J Neurochem. 1981;36:251–7.
Gospe Jr SM. Pyridoxine-dependent seizures: new genetic and biochemical clues to help with diagnosis and treatment. Curr Opin Neurol. 2006;19:148–53.
van Karnebeek CD, Hartmann H, Jaggumantri S, et al. Lysine restricted diet for pyridoxine-dependent epilepsy: first evidence and future trials. Mol Genet Metab. 2012;107:335–44. Outlines the results of an open-labeled observational study—first evidence of a positive effect of the lysine-restricted diet as a novel adjunct treatment for PDE.
Stockler S, Moeslinger D, Herle M, et al. Cultural aspects in the management of inborn errors of metabolism. J Inherit Metab Dis. 2012;35:1147–52.
van Karnebeek CD, Stockler-Ipsiroglu S, Jaggumantri S, et al. Lysine-restricted diet as adjunct therapy for pyridoxine-dependent epilepsy: the PDE consortium consensus recommendations. JIMD Rep. 2014;15:1-11. Publication providing detailed recommendations for treatment of PDE with lysine-restricted diet—management strategy, monitoring and follow up- based on PDE consortium consensus.
Kolker S, Christensen E, Leonard JV, et al. Diagnosis and management of glutaric aciduria type I—revised recommendations. J Inherit Metab. 2011;34:677–94.
FAO/WHO/UNU. Energy and protein requirements. Geneva: Switzerland; 1985. 724.
Yannicelli S. Nutrition management of patients with inherited disorders of organic acid metabolism. In: Acosta PB, editor. Nutrition management of patients with inherited metabolic disorders. Boston: Jones and Bartlett publishers; 2010. p. 314.
Subcommittee on the Tenth Edition of the RDAs, Food and Nutrition Board, Commission on Life Sciences National Research Council. Recommended Dietary Allowances. 10 edn. Washington, DC: National Academy Press; 1989.
Sauer SW, Opp S, Hoffmann GF, et al. Therapeutic modulation of cerebral L-lysine metabolism in a mouse model for glutaric aciduria type I. Brain. 2011;134:157–70.
Kölker S, Boy SP, Heringer J, et al. Complementary dietary treatment using lysine-free, arginine-fortified amino acid supplements in glutaric aciduria type I—a decade of experience. Mol Genet Metab. 2012;107:72–80.
Mercimek-Mahmutoglu S, Cordeiro D, Cruz V, et al. Novel therapy for pyridoxine dependent epilepsy due to ALDH7A1 genetic defect: l-arginine supplementation alternative to lysine-restricted diet. Eur J Paediatr Neurol. 2014. doi:10.1016/j.ejpn.2014.07.001.
Shuen AY, Coughlin 2nd CR, Lefrancois M, et al. Combined triple therapy trial of pyridoxine lysine restricted diet and arginine supplementation in four patients with pyridoxine-dependent epilepsy. Mol Genet Metab. 2014;111:215–302.
van Karnebeek CD, Stockler S. Treatable inborn errors of metabolism causing intellectual disability: a systematic literature review. Mol Genet Metab. 2012;105:368–81.
Jung S, Tran NT, Gospe Jr SM, et al. Preliminary investigation of the use of newborn dried blood spots for screening pyridoxine-dependent epilepsy by LC-MS/MS. Mol Genet Metab. 2013;110:237–40.
Acknowledgements
The authors thank the members of the International PDE Consortium for their expertise and collaboration, in particular Dr. Sylvia Stockler-Ipsiroglu (University of British Columbia, Canada), Dr. Curtis Coughlin and Dr. Johan Van Hove (University of Colorado, USA), Dr. Sid Gospe (University of Washington, USA), (Dr. Levinus Bok (Maxima Medical Centre, The Netherlands), and Dr. Hans Hartmann (Hannover Medical School, Germany).
Funding
BC Children’s Hospital Foundation (First Collaborative Area of Innovation) and Rare Diseases Foundation, Vancouver, Canada
Compliance with Ethics Guidelines
Conflict of Interest
Clara D.M. van Karnebeek reports the receipt of grants from BC Children's Hospital Foundation, Vancouver Canada; from Michael Smith Foundation for Health Research, Vancouver, Canada; from the University of British Columbia (Bluma Tischler Post-Doctoral Fellowship); and from Rare Diseases Foundation, Vancouver, Canada, during the conduct of the study.
Sravan Jaggumantri reports no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pediatric Neurology
Rights and permissions
About this article
Cite this article
van Karnebeek, C.D.M., Jaggumantri, S. Current Treatment and Management of Pyridoxine-Dependent Epilepsy. Curr Treat Options Neurol 17, 7 (2015). https://doi.org/10.1007/s11940-014-0335-0
Published:
DOI: https://doi.org/10.1007/s11940-014-0335-0