Abstract
Purpose of Review
We aimed to highlight disease-related and treatment-related complications of Behçet syndrome (BS) based on previous and recent studies and our own experience.
Recent Findings
The Behçet’s Disease Overall Damage Index is a newly developed instrument to assess damage in BS. Validation studies showed that damage is already present in some patients at diagnosis and continues to progress during the follow-up, mainly related to treatment complications. Nervous system and eye involvement are important causes of long-term disability. Cyclophosphamide seems to be associated with infertility and an increased risk of malignancies among BS patients, prompting the consideration of shortening the treatment duration. Flares in mucocutaneous manifestations have been reported with tocilizumab, and de novo BS manifestations with secukinumab therapy.
Summary
Earlier diagnosis and treatment are essential to prevent disease-related damage in BS. Treatment-related complications seem to be the leading cause of damage during the disease course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
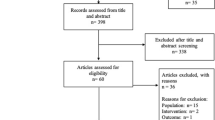
Behçet syndrome (BS) is a systemic vasculitis that can cause important disability and mortality depending on disease severity and the organs that are involved. There is a heterogeneous disease course with variability in disease expression across patients and within the same patient over time. The mucocutaneous, musculoskeletal, ocular, and vascular domains are usually more active during the early years, whereas neurologic and gastrointestinal domains may present later in the disease course. Oral ulcers, genital ulcers, papulopustular lesions, erythema nodosum-like lesions, and arthritis may run a course with frequent recurrences [1,2,3,4]. Although these do not cause damage except for genital ulcer scars, they may have an important impact on the quality of life [5, 6]. In contrast, disease activity in organ domains frequently results in permanent damage (Table 1) [7]. In addition to the damage caused by disease manifestations, glucocorticoids and immunosuppressives used in the management of these manifestations can also cause complications [8••]. A recent study that explored the mortality rate and causes of death in BS showed that the mean age of death was 52.8 years among men and 58.4 years among women, compared with 71.2 years among men and 79.8 years among women in the general population [9•]. When the underlying cause of death was related to BS, infections were the most common cause (25.1%) followed by organ dysfunction (21.6%) and arterial events (15.2%). The aim of this review is to highlight the disease-related and treatment-related complications of BS and possible measures for alleviating these complications.
Damage Accrual in Behçet Syndrome
The development of Behçet’s specific instruments for assessing damage has made it possible to formally evaluate and score damage in patients with BS. These instruments enabled better identification of organ-related damage in BS, compared with the previously used vasculitis damage index which is a damage instrument that is used generically in different types of vasculitis [10••].
The initial validation study of Behçet’s Disease Overall Damage Index (BODI) had shown that 56% of their patients had at least one damage item at the time of that study [10••]. Damage was present in the ocular domain in 23.2% of the patients, mucocutaneous domain in 20.6%, neuropsychiatric domain in 17.1%, vascular domain in 14%, musculoskeletal domain in 7.5%, cardiovascular domain in 4.4%, gastrointestinal domain in 2.6%, and reproductive domain in 1.3% of the patients. A multivariate analysis showed that male sex, disease duration, previous use of tumor necrosis factor (TNF) alpha inhibitors, and involvement of vascular, nervous system, or gastrointestinal system domains were associated with higher damage scores. A more recent study that reported on the 2-year follow-up of these patients showed that there was damage progression in 19% of these patients [11••]. Interestingly, damage accrual over time seemed to be more treatment-related, with 41% of the new damage items considered as related to glucocorticoid use. This study additionally showed that damage accrual is associated with impaired quality of life, especially affecting the emotional domains. A similar rate of damage progression was reported in a study from Iran [12]. Among 274 patients with a median follow-up duration of 40 months, 19.3% of the patients had an increase in their damage scores. A younger age at disease onset, shorter disease duration, and more severe disease were independent predictors of damage progression in this study.
In our cohort, among 300 patients who were included in a study that aimed to validate BODI, 181 (60.3%) already had at least one damage item at the time of BS diagnosis [13]. Mucocutaneous scar was the most common damage item at diagnosis (48.6%), followed by posterior segment changes (10%) and deep vein thrombosis (4.6%). This finding underlines the importance of early diagnosis in BS, in order to prevent damage that can occur very early in the disease course. Damage progressed in 56 (19%) of these patients, and the mean time to the development of the first damage item was 1.15 years. Cataracts (5.6%), peripheral neuropathy (2.6%), avascular necrosis (1.6%), and diabetes (1.6) were damage items that seemed to be treatment-related, rather than disease-related in our cohort.
Disease-Specific Complications
Mucocutaneous and Joint Involvement
Mucocutaneous and joint involvement rarely lead to serious complications and permanent damage but may still have a negative impact on functional status, health-related quality of life, and employment status in BS [5, 14•, 15,16,17].
Oral ulcers are the most common lesions in BS, with a prevalence of 97–100%. Among the three types of oral ulcers in BS, minor oral ulcers (< 10 mm in diameter) are the most common type (85–99%) and heal without scarring within 7 to 10 days. Major oral ulcers (≥ 10 mm in diameter) are deeper, more painful, and rarely observed. They heal slowly and tend to leave scars. Herpetiform oral ulcers (1–3 mm in diameter) are also rare and may occasionally leave scars.
Genital ulcers are specific for BS and occur in 50% to 75% of BS patients. A prospective study showed that genital ulcers heal with hypopigmented scar in 66% of men and in 60% of women with BS. If the genital ulcers are larger than 1 cm in diameter scarring is almost inevitable [18].
Erythema nodosum-like lesions are red, painful inflammatory lesions which can be seen in up to 50% of BS patients. They usually occur in lower extremities and are less frequently seen in other body parts. They heal within 1 to 6 weeks and may leave post-inflammatory hyperpigmentation.
Papulopustular lesions are frequent (30–96%) but non-specific lesions in BS. They tend to be located in lower extremities and to persist at older ages more frequently in BS patients, compared to healthy and diseased controls. They usually cause cosmetic issues rather than functional impairment.
Joint involvement is seen in around 50% of BS patients, either as arthritis or arthralgia. Arthritis in BS has mainly asymmetrical, mono/oligo articular character, usually affects medium or large joints, and heals without deformity within a few weeks. However, joint involvement may still cause functional disability and fatigue [17] and has a negative impact on health-related quality of life and employment status [5, 14•, 15].
Ocular Involvement
Ocular involvement is seen in around 50% of BS patients and is the most significant cause of morbidity. The most common types of ocular inflammation in BS are panuveitis, retinitis, and retinal vasculitis. Isolated anterior uveitis occurs in 10–15% of BS patients. Hypopyon which indicates severe ocular attack is seen in 6–12% of BS patients and resolves without damage. Cystoid macular edema can occur both during exacerbation and after the resolution of inflammation and may lead to visual impairment.
In a long-term outcome survey, patients registered between 1977 and 1983 were evaluated after 20 years of their initial visit [7]. They showed that a total of 44% (64/146) of male and 21% (8/38) of female patients had a loss of useful vision (visual acuity of ≤ 0.1) at the end of follow-up. In another retrospective study, 880 consecutive patients who were seen between 1980 and 1998 were studied [19]. They demonstrated that the risk of blindness at 1, 5, and 7 years were 9%, 26%, and 30% for patients admitted to the hospital in 1980s whereas the risk decreased to 5%, 16%, and 21% in patients admitted to the hospital after 1990. The same group also compared the 3-year visual outcome of BS uveitis patients presented in the 1990s to those in the 2000s [20]. They showed that the risk of useful vision loss was 27.6% in the 1990s while it was 12.9% in the 2000s. In another retrospective study, the risk of severe visual loss was 13% at 10-year in BS uveitis patients who presented between 2000 and 2010, excluding patients with irreversible visual loss at presentation [21]. The prognosis of Behçet’s uveitis is observed to improve over decades, and it is thought to be associated with the use of effective immunosuppressive treatments, particularly biologics.
Glaucoma and cataracts may occur in BS patients with uveitis, either as a result of recurrent attacks or due to medications. Secondary glaucoma was reported in 11 to 22% of BS uveitis patients in retrospective studies [22,23,24].
Vascular Involvement
The frequency of vascular involvement varies between 15 and 50% and it is one of the leading causes of morbidity and mortality in BS. The range of vascular involvement includes frequently occurring and recurrent conditions, such as superficial thrombophlebitis and deep vein thrombosis in the lower extremities. Additionally, less common venous conditions like inferior vena cava thrombosis (IVCT) and superior vena cava thrombosis, Budd-Chiari syndrome (BCS), and rare arterial conditions, including both pulmonary and non-pulmonary arterial involvement, occur in BS patients.
Lower extremity deep vein thrombosis is the most common type of vascular involvement in BS patients (70%) [25]. Due to its relapsing course and extensive venous involvement, severe post-thrombotic syndrome has been observed in 18 to 51% of patients in different series and venous claudication occurs in 32% of patients [26•, 27]. Leg ulcer is one of the debilitating complications of severe post-thrombotic syndrome in BS and may cause unemployment in 46% of these patients [28].
BCS due to thrombosis in hepatic vein and/or suprahepatic or hepatic IVC is a rare vascular manifestation of BS (2–4%), but it is associated with a high mortality rate (14–50%) [29, 30]. BCS typically presents with abdominal pain, ascites, collaterals on the abdominal wall, scrotal edema, and diffuse swelling in the lower extremities. During the course of the disease, jaundice, encephalopathy, splenomegaly, hypersplenism, and bleeding from esophageal varices can develop as a result of liver failure. Among those patients, the mortality rate has been reported as 60% [29]. In a subgroup of BCS patients, the condition may have a silent presentation without any of these severe symptoms, and their mortality rate has been reported as less than 10% [29].
Superior vena cava thrombosis constitutes around 9% of vascular involvement in BS [25] and usually presents with swelling and cyanosis of the face, neck, and upper extremities. Venous collaterals can be observed on the chest wall. It generally has a benign course, rarely relapses, and may be complicated with pleural effusion, chylothorax, and mediastinal fibrosis [31]. A retrospective study including 28 BS patients with superior vena cava thrombosis reported that there is an increased risk of obstructive sleep apnea in those patients compared to other BS patients [32].
Hepatic and suprahepatic IVCT can lead to BCS, while infrahepatic IVCT is typically observed as an extension of lower extremity deep vein thrombosis in BS patients. Patients may have abdominal or lower back pain during acute thrombosis. Severe post-thrombotic syndrome, leg ulcers, and venous collaterals are the long-term complications of infrahepatic IVCT.
Arterial involvement constitutes 15% of all vascular complications in BS, and the overall mortality rate, regardless of the type of arterial involvement, has been reported as 14% [33].
Pulmonary arterial involvement is a rare form of involvement (< 5%) characterized by aneurysm and/or thrombosis in the pulmonary arteries, but it is the leading cause of mortality in BS. In the early 1990s, the mortality rate was reported as 50%, but it has since decreased to around 25% in later reports, which is attributed to earlier recognition and prompt treatment [34,35,36]. Hemoptysis resulting from the rupture of an aneurysm can be massive and life-threatening. Hemoptysis may also occur due to bronchial artery enlargement as a long-term complication [37]. Other observed symptoms are dyspnea, cough, chest pain, pleural effusion, and thickening. Chronic thromboembolic pulmonary hypertension might rarely be seen in BS patients with pulmonary arterial involvement as a long-term complication [38].
Peripheral artery aneurysms in BS typically manifest as painful, hyperemic, and pulsatile masses, carrying a higher risk of rupture or leakage compared to distal ischemia. On the contrary, abdominal aortic aneurysms present with nonspecific symptoms such as back pain and abdominal discomfort, yet they still carry the high risk of rupture and mortality.
Arterial occlusion or stenosis, which can lead to claudication, gangrene of extremities, or organ infarction depending on the site of involvement, as well as intracardiac thrombosis that may be complicated by valve insufficiency or pulmonary hypertension, are other rare forms of arterial involvement in BS.
Central Nervous System Involvement
Neurologic involvement in BS (NBS) is seen less frequently (5–10%), yet it is a significant cause for morbidity and mortality [39]. It is classified as parenchymal NBS (75–80%) and non-parenchymal NBS (10–20%) [40, 41].
Parenchymal NBS usually presents with symptoms like headache, dysarthria, ataxia, hemiparesis, cranial neuropathies, or corticospinal symptoms. It is considered the primary cause of severe disability and mortality in NBS patients. Two studies which were published in late 1990s and early 2000s showed that around 50% of patients with NBS had become physically and/or mentally disabled within 10 years after the onset of NBS [40, 41]. Mortality has been reported in around 10–12% [40,41,42]. On the other hand, just as observed in ocular involvement, improvement in the prognosis of NBS has also been noted in subsequent years. A group reported that among 115 NBS patients, 25% became disabled or died after a median follow-up of 73 months [42].
Cerebral venous sinus thrombosis (CVST) is the main type of non-parenchymal NBS and generally has a favorable outcome compared to parenchymal NBS. CVST present with severe headache, papilledema, and sixth-nerve palsy due to intracranial hypertension. Since hemorrhagic venous infarction due to CVST in BS is very unlikely, severe symptoms such as hemiparesis, confusion, and seizure are quite rare. On the other hand, total blindness due to prolonged intracranial hypertension and optic atrophy was reported in 6 out of 64 CVST patients with BS [43]. Other CVST-related complications reported in the same cohort are persistent headache (n = 6), visual impairment (n = 4), altered cognition (n = 3), hemiparesis (n = 2), and tinnitus (n = 2).
Cognitive changes, memory impairment, and psychiatric symptoms such as euphoria, loss of insight, and disinhibition may rarely occur either due to parenchymal NBS or other forms of neurologic involvement in BS [39].
Gastrointestinal Involvement
Gastrointestinal involvement in BS (GIBS) can affect the whole gastrointestinal tract from mouth to anus. Its frequency varies between < 1 and 60% according to geographic location with a higher prevalence in Far East Asia [44]. Symptoms of GIBS range from mild abdominal discomfort, nausea, and diarrhea to weight loss, severe abdominal pain, GI bleeding, fistula, and perforation which may require surgical intervention. A retrospective Korean study reported that among 130 GIBS patients, 71.5% of them were in remission or had a mild course at 5 years while 28.5% of patients experienced a severe clinical course with multiple relapses or chronic symptoms [45]. Another retrospective study from Turkey with a mean follow-up of 7.5 years found that among 60 GIBS patients, 20% of them had a relapsing course. Overall 80% were in remission, 5% had died due to non-GI-related causes, and 8% were still active at the time of the survey [44]. The rate of surgical treatment either for resistant disease or for intestinal complications such as perforation, fistula, or severe bleeding was found to be 20% at 1 year, 27–33% at 5 years, and 31–46% at 10 years [46, 47].
Amyloidosis
AA amyloidosis is a rare complication in patients with BS. In a recent study, the frequency of AA amyloidosis in BS patients followed between 1976 and 2000 was compared to those followed between 2001 and 2017, and it was observed that the prevalence of AA amyloidosis decreased from 0.62 to 0.054% [48•].
Myelodysplastic Syndrome
The association between BS and myelodysplastic syndrome has been defined in several case series [49, 50•]. Severe or treatment refractory GIBS and trisomy 8 are the common features of this association.
Epididymitis
Epididymitis in patients with BS presents with pain, tenderness, and swelling in testicles. The symptoms generally resolve spontaneously, but relapses are frequent. It usually has a favorable prognosis and permanent damage related with epididymitis in BS patients is rare. Salpingitis has also been rarely observed.
Treatment-Specific Complications
Treatment options other than glucocorticoids for BS mainly include colchicine, conventional immunosuppressive agents (azathioprine, cyclosporine-A, mycophenolate, thalidomide, and cyclophosphamide), interferon-alpha, biologic agents (TNF inhibitors, tocilizumab, interleukin-1 inhibitors, and secukinumab), and small molecules (apremilast, tofacitinib, and baricitinib). Commonly reported adverse events with these agents are summarized in Table 2. Complications associated with each drug are detailed below.
Colchicine
Gastrointestinal symptoms such as diarrhea, nausea, abdominal pain, cytopenia, myalgia, and elevated liver enzymes are the most common side effects of colchicine. Discontinuing therapy, reducing the colchicine dose, or switching to another colchicine preparation is usually sufficient to alleviate these effects in most patients [51, 52]. Impaired sperm production has been reported with colchicine [53], and it should be discontinued in such patients. Rhabdomyolysis is one of the most serious side effects of colchicine, and when planning to initiate a new drug in a patient already using colchicine, one should consider its potential interaction with CYP3A4 inhibitors, such as clarithromycin [54]. Due to its narrow therapeutic index, colchicine should be used with caution in patients with renal impairment.
Azathioprine
Gastrointestinal symptoms, cytopenia, and elevated liver enzymes are the most common reasons for discontinuing azathioprine or reducing the dose [44, 55,56,57]. Interestingly, pancreatitis, which is observed in 7% of patients with inflammatory bowel disease [58], does not appear to be a concern for BS patients. Patients may need to be screened for thiopurine methyltransferase deficiency, in populations that this condition is common. In populations where thiopurine methyltransferase deficiency is rare, starting with a low dose and gradually increasing until the targeted dose is reached may be an option. Hematological malignancies, especially myelodysplastic syndrome, are the most common types of malignancies among BS patients [59, 60]. Although these studies have not found an increased risk of malignancy with azathioprine use in BS patients, hematologic malignancies should be considered in patients with persistent cytopenia or elevated mean corpuscular volume despite discontinuing azathioprine [49], and non-melanoma skin cancer should be screened in BS patients using azathioprine.
Cyclosporine-A
Hirsutism, renal dysfunction, hypertension, gingival hypertrophy, gastrointestinal symptoms, hyperlipidemia, impaired glucose tolerance, increased uric acid, and paresthesia are commonly reported adverse events in randomized controlled trials [61,62,63,64]. Patients should be monitored for hypertension after initiating cyclosporine-A. If hypertension is detected, the drug should be discontinued instead of adding an antihypertensive agent. Due to its association with the development of nervous system involvement in BS, the use of cyclosporine is not recommended in patients with nervous system involvement or those who develop neurological symptoms such as headaches and paresthesia while on the medication [65].
Mycophenolate
The prospective trial of mycophenolate mofetil in BS was terminated due to the exacerbation of mucocutaneous lesions [66]. However, such adverse effects have not been observed in 10 patients treated with mycophenolate sodium [67]. For patients experiencing gastrointestinal intolerance, which is one of the most common side effects of mycophenolate, switching from mycophenolate mofetil to mycophenolate sodium may be considered [68].
Thalidomide
Teratogenicity, an increased risk of thromboembolism, and neurotoxicity limit the use of thalidomide in BS patients despite its rapid onset of action and effectiveness in treating mucocutaneous lesions and gastrointestinal involvement [69].
Cyclophosphamide
While serving as a life-saving treatment option for vascular involvement of BS patients, the use of cyclophosphamide may carry the risk of severe toxicity. Frequently observed side effects include bone marrow suppression, infections, hemorrhagic cystitis, infertility, nausea, infusion reactions, and alopecia. In addition to these common side effects, less frequently cardiovascular toxicity, the syndrome of inappropriate antidiuretic hormone secretion, gonadal failure, pulmonary fibrosis, and malignancies may be observed. In our survey of 198 BS patients treated with cyclophosphamide, 9% of the patients experienced short-term adverse events, mainly hemorrhagic cystitis (n = 7) and infection (n = 4). In the long-term follow-up, 30% developed infertility, and 8% developed malignancies, with bladder carcinoma being the most common [8••]. A nested case–control study from China found a tenfold increased risk of malignancy associated with cyclophosphamide use among BS patients [59]. As a result, we no longer recommend its use for extended durations and in oral form, which can lead to an increased cumulative dose [69]. We also routinely use mesna to reduce the risk of hemorrhagic cystitis.
Interferon-Alpha
Flu-like symptoms such as fever, chills, headache, fatigue, and myalgia, as well as hair loss, cytopenia, elevated liver enzymes, and depression, have been reported as side effects of interferon-alpha therapy [64, 70]. Paracetamol or non-steroidal anti-inflammatory drugs are typically sufficient for managing flu-like symptoms. In a prospective study, interferon was associated with an increased risk of depression and suicidal behavior compared to BS patients using drugs other than interferon-alpha [71]. It is not recommended to combine it with azathioprine due to myelosuppression [72] or with other immunosuppressives agents. Interferon-alpha can induce autoimmunity, leading to immune-mediated side effects [73]. The thyroid gland is one of the most frequently affected organs; therefore, thyroid function tests should be monitored during therapy. Whether pegylated interferon-alpha is safer than interferon-alpha among BS patients is not known. However, it may be considered in patients experiencing side effects while on interferon-alpha.
TNF Inhibitors
The side effects of TNF inhibitors among BS patients are similar to those reported in other rheumatic diseases, with the exception of tuberculosis which is reported more frequently in BS. The side effects reported among BS patients include infusion reactions, injection site reactions, infections, cytopenia, induction of autoimmunity, paradoxical reactions, elevated liver enzymes, and interstitial lung disease [74••, 75, 76]. Among these, infusion reactions with infliximab are one of the most common reasons for discontinuing the treatment. Especially in cases where patients interrupt or re-initiate the treatment, there is a higher risk associated. Therefore, we typically administer the drug with premedication to such patients, even if they have not previously experienced infusion reactions. Infections are the most feared and well-known side effects of TNF inhibitors. BS patients, in particular, have been found to be more susceptible to tuberculosis reactivation compared to those with other rheumatic diseases treated with TNF inhibitors [77•]. This may be associated with corticosteroids and immunosuppressives that are commonly used together with TNF inhibitors in patients with BS. Therefore, every BS patient should be screened for tuberculosis infection according to local guidelines before initiating a TNF inhibitor.
Considering the potential link between TNF inhibitors and demyelinating diseases, heart failure, or malignancies [78,79,80], we prefer to use non-TNF biologic agents for patients with these conditions. The same approach is taken for patients who develop paradoxical reactions, such as palmoplantar pustulosis, sarcoidosis, and drug-induced lupus.
Tocilizumab
Tocilizumab was not effective in treating mucocutaneous lesions and may even exacerbate these lesions. Infusion reactions, infections, hyperlipidemia, and intestinal perforation that are known side effects of tocilizumab have also been reported among BS patients [81, 82, 83•, 84, 85].
Interleukin-1 Inhibitors
The advantage of interleukin-1 inhibitors, including anakinra and canakinumab, lies in their favorable safety profile, particularly with regard to infections [86]. However, their drug retention rate among BS patients, especially for anakinra, is low. Frequent relapses during treatment necessitate higher doses, and injection site reactions make the treatment more challenging to continue [87].
Secukinumab
Secukinumab is ineffective in treating uveitis due to BS [88], but may be an option for patients with refractory articular involvement [89]. However, it may exacerbate BS manifestations and lead to the development of new major organ involvement [90,91,92,93,94].
Apremilast
Apremilast is the first drug to be approved by the FDA for BS following the demonstration of its efficacy in phase 2 and 3 randomized controlled trials on OUs [95, 96]. Gastrointestinal side effects, which are the most common side effect of apremilast, usually start within 2 weeks following treatment and resolve within a month in most patients. Serious adverse events were rare in the long term across 15 randomized controlled studies, observed in less than 1% of the 4183 patients treated with apremilast for psoriasis, psoriatic arthritis, and BS [97••].
JAK Inhibitors
Tofacitinib and baricitinib are newly tested agents in BS. No thromboembolism has been reported and herpes zoster infection was the most common adverse event [98,99,100,101]. However, thromboembolism risk with these agents is documented among rheumatoid arthritis patients, and a large number of patients with long-term follow-up are needed to draw a conclusion for BS patients.
Conclusions
Similar to other vasculitides, damage in BS is a significant concern that can manifest even in the early stages of the disease and continues to evolve over time, either due to disease-related or treatment-related complications. Among the disease-related complications, mucocutaneous lesions and articular involvement typically have a detrimental impact on the quality of life, and their damage is not usually associated with permanent organ dysfunction or mortality. However, major organ involvement, including ocular, vascular, gastrointestinal, and nervous system complications, can result in permanent damage. The disease often follows a severe course in young individuals and BS patients with permanent damage have to cope with disabilities for the rest of their lives. Treatment-related complications are also common in BS patients. Therefore, early diagnosis, timely recognition of complications, and vigilant monitoring for treatment-related adverse events are essential for preventing permanent damage and enhancing the patients’ overall quality of life.
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hatemi G, Ucar D, Uygunoglu U, Yazici H, Yazici Y. Behcet syndrome. Rheum Dis Clin North Am. 2023;49(3):585–602.
Yazici Y, Hatemi G, Bodaghi B, et al. Behcet syndrome. Nat Rev Dis Primers. 2021;7(1):67.
Yazici H, Seyahi E, Hatemi G, Yazici Y. Behcet syndrome: a contemporary view. Nat Rev Rheumatol. 2018;14(2):119.
Esatoglu SN, Kutlubay Z, Ucar D, et al. Behcet’s syndrome: providing integrated care. J Multidiscip Healthc. 2017;10:309–19.
Senusi AA, Mather J, Ola D, Bergmeier LA, Gokani B, Fortune F. The impact of multifactorial factors on the quality of life of Behcet’s patients over 10 years. Front Med (Lausanne). 2022;9:996571.
Masoumi M, Sharifi A, Rezaei S, et al. Global systematic review and meta-analysis of health-related quality of life in Behcet’s patients. Caspian J Intern Med. 2022;13(3):447–57.
Kural-Seyahi E, Fresko I, Seyahi N, et al. The long-term mortality and morbidity of Behcet syndrome: a 2-decade outcome survey of 387 patients followed at a dedicated center. Medicine (Baltimore). 2003;82(1):60–76.
•• Gurcan M, Esatoglu SN, Hamuryudan V, et al. Long term follow-up of Behcet’s syndrome patients treated with cyclophosphamide. Rheumatology (Oxford). 2020;59(9):2264–71. (This is the largest study regarding the use of cyclophosphamide among BS patients and documents its long-term complications, including infertility and malignancy associated with this agent.)
• David E, Fauvernier M, Saadoun D, et al. Mortality associated with Behcet’s disease in France assessed by multiple-cause-of-death analysis. Clin Rheumatol. 2022;41(6):1749–58. (This is a mortality study from France, which collected data between 1979 and 2016. It indicates that BS patients have a shorter life expectancy than the general population, with infections and cardiovascular complications being the most common causes.)
•• Piga M, Floris A, Espinosa G, et al. Development and preliminary validation of the Behcet’s syndrome overall damage index (BODI). RMD Open. 2020;6(2). https://doi.org/10.1136/rmdopen-2020-001192. (This study outlines the development and validation of BODI, an assessment tool specifically designed for evaluating damage in BS patients.)
•• Floris A, Piga M, Laconi R, et al. Accrual of organ damage in Behcet’s syndrome: trajectory, associated factors, and impact on patients’ quality of life over a 2-year prospective follow-up study. Arthritis Res Ther. 2022;24(1):253. (This study demonstrated that organ damage in BS patients accumulates over time, with glucocorticoid use and flares identified as independent predictor factors of this damage. Immunosuppressive use was found to be protective.)
Musavian S, Farzaneh R, Rahimi M, Mahdavi AM, Gojazadeh M, Khabbazi A. Validity and reliability of the BODI for assessing damage in Behcet’s disease. Ir J Med Sci. 2023;192(5):2549–53.
Yagiz Ozogul Y, Ozguler Y, Ucar D, et al. Validation of Behçet’s disease overall damage index (BODI) for retrospective studies and a proposal for modification [abstract]. Arthritis Rheumatol 2022;74(Suppl 9). https://acrabstracts.org/abstract/validation-of-behcets-disease-overall-damage-index-bodi-for-retrospective-studies-and-a-proposal-for-modification/.
• Karacayli U, Adesanya A, Aksoy A, et al. The assessment of presenteeism and activity impairment in Behcet’s syndrome and recurrent aphthous stomatitis: a multicentre study. Rheumatology (Oxford). 2022;61(4):1538–47. (This study showed that joint involvement and oral ulcer related pain adversely affect activity impairment in active BS patients compared to inactive patients.)
Senusi AA, Ola D, Mather J, Mather J, Fortune F. Behcet’s syndrome and health-related quality of life: influence of symptoms, lifestyle and employment status. Clin Exp Rheumatol. 2017;35 Suppl 108(6):43–50.
Senusi A, Seoudi N, Bergmeier LA, Fortune F. Genital ulcer severity score and genital health quality of life in Behcet’s disease. Orphanet J Rare Dis. 2015;10:117.
Moses Alder N, Fisher M, Yazici Y. Behcet’s syndrome patients have high levels of functional disability, fatigue and pain as measured by a multi-dimensional health assessment questionnaire (MDHAQ). Clin Exp Rheumatol. 2008;26(4 Suppl 50):S110–3.
Mat MC, Goksugur N, Engin B, Yurdakul S, Yazici H. The frequency of scarring after genital ulcers in Behcet’s syndrome: a prospective study. Int J Dermatol. 2006;45(5):554–6.
Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin Altunbas H, Urgancioglu M. Uveitis in Behcet disease: an analysis of 880 patients. Am J Ophthalmol. 2004;138(3):373–80.
Cingu AK, Onal S, Urgancioglu M, Tugal-Tutkun I. Comparison of presenting features and three-year disease course in Turkish patients with Behcet uveitis who presented in the early 1990s and the early 2000s. Ocul Immunol Inflamm. 2012;20(6):423–8.
Taylor SR, Singh J, Menezo V, Wakefield D, McCluskey P, Lightman S. Behcet disease: visual prognosis and factors influencing the development of visual loss. Am J Ophthalmol. 2011;152(6):1059–66.
Belkhadir K, Boutimzine N, Tachfouti S, Laghmari M, Amazouzi A, Cherkaoui O. Uveitic glaucoma in Behcet’s disease: when everything gets complicated. J Fr Ophtalmol. 2020;43(7):635–41.
Elgin U, Berker N, Batman A. Incidence of secondary glaucoma in Behcet disease. J Glaucoma. 2004;13(6):441–4.
Takahashi T, Ohtani S, Miyata K, Miyata N, Shirato S, Mochizuki M. A clinical evaluation of uveitis-associated secondary glaucoma. Jpn J Ophthalmol. 2002;46(5):556–62.
Tascilar K, Melikoglu M, Ugurlu S, Sut N, Caglar E, Yazici H. Vascular involvement in Behcet’s syndrome: a retrospective analysis of associations and the time course. Rheumatology (Oxford). 2014;53(11):2018–22.
• Aksoy A, Colak S, Yagiz B, et al. Predictors for the risk and severity of post-thrombotic syndrome in vascular Behcet’s disease. J Vasc Surg Venous Lymphat Disord. 2021;9(6):1451–9. (This study showed that BS patients with lower extremity deep vein thrombosis have a high risk of developing severe post thrombotic syndrome.)
Seyahi E, Cakmak OS, Tutar B, et al. Clinical and ultrasonographic evaluation of lower-extremity vein thrombosis in behcet syndrome: an observational study. Medicine (Baltimore). 2015;94(44):e1899.
Ozguler Y, Kutlubay Z, Dikici AS, Melikoglu M, Mat C, Yazici H, Seyahi E. Leg ulcers in Behçet’s syndrome: an observational survey in 24 patients [abstract]. Arthritis Rheumatol. 2018;70(Suppl 9). https://acrabstracts.org/abstract/leg-ulcers-in-behcets-syndrome-an-observational-survey-in-24-patients/.
Seyahi E, Caglar E, Ugurlu S, et al. An outcome survey of 43 patients with Budd-Chiari syndrome due to Behcet’s syndrome followed up at a single, dedicated center. Semin Arthritis Rheum. 2015;44(5):602–9.
Desbois AC, Rautou PE, Biard L, et al. Behcet’s disease in Budd-Chiari syndrome. Orphanet J Rare Dis. 2014;9:104.
Moon H, Lee YJ, Lee SI, Yoo WH. Chylothorax and chylopericardium as the initial clinical manifestation of Behcet’s disease. Rheumatol Int. 2008;28(4):375–7.
Gokturk A, Esatoglu SN, Atahan E, Hamuryudan V, Yazici H, Seyahi E. Increased frequency of obstructive sleep apnea syndrome in Behcet’s syndrome patients with superior vena cava syndrome. Clin Exp Rheumatol. 2019;37 Suppl 121(6):132–6.
Saadoun D, Asli B, Wechsler B, et al. Long-term outcome of arterial lesions in Behcet disease: a series of 101 patients. Medicine (Baltimore). 2012;91(1):18–24.
Seyahi E, Melikoglu M, Akman C, et al. Pulmonary artery involvement and associated lung disease in Behcet disease: a series of 47 patients. Medicine (Baltimore). 2012;91(1):35–48.
Hamuryudan V, Er T, Seyahi E, et al. Pulmonary artery aneurysms in Behcet syndrome. Am J Med. 2004;117(11):867–70.
Hamuryudan V, Yurdakul S, Moral F, et al. Pulmonary arterial aneurysms in Behcet’s syndrome: a report of 24 cases. Br J Rheumatol. 1994;33(1):48–51.
Esatoglu SN, Seyahi E, Ugurlu S, et al. Bronchial artery enlargement may be the cause of recurrent haemoptysis in Behcet’s syndrome patients with pulmonary artery involvement during follow-up. Clin Exp Rheumatol. 2016;34(6 Suppl 102):92–6.
Yildizeli SO, Yanartas M, Tas S, et al. Outcomes of patients with Behcet’s syndrome after pulmonary endarterectomy. Thorac Cardiovasc Surg. 2018;66(2):187–92.
Uygunoglu U, Siva A. An uncommon disease included commonly in the differential diagnosis of neurological diseases: neuro-Behcet’s syndrome. J Neurol Sci. 2021;426:117436.
Siva A, Kantarci OH, Saip S, et al. Behcet’s disease: diagnostic and prognostic aspects of neurological involvement. J Neurol. 2001;248(2):95–103.
Akman-Demir G, Serdaroglu P, Tasci B. Clinical patterns of neurological involvement in Behcet’s disease: evaluation of 200 patients. Neuro-Behcet Study Group Brain. 1999;122(Pt 11):2171–82.
Noel N, Bernard R, Wechsler B, et al. Long-term outcome of neuro-Behcet’s disease. Arthritis Rheumatol. 2014;66(5):1306–14.
Saadoun D, Wechsler B, Resche-Rigon M, et al. Cerebral venous thrombosis in Behcet’s disease. Arthritis Rheum. 2009;61(4):518–26.
Hatemi I, Esatoglu SN, Hatemi G, Erzin Y, Yazici H, Celik AF. Characteristics, treatment, and long-term outcome of gastrointestinal involvement in Behcet’s syndrome: a strobe-compliant observational study from a dedicated multidisciplinary center. Medicine (Baltimore). 2016;95(16):e3348.
Jung YS, Cheon JH, Park SJ, Hong SP, Kim TI, Kim WH. Clinical course of intestinal Behcet’s disease during the first five years. Dig Dis Sci. 2013;58(2):496–503.
Cheon JH, Kim WH. An update on the diagnosis, treatment, and prognosis of intestinal Behcet’s disease. Curr Opin Rheumatol. 2015;27(1):24–31.
Jung YS, Yoon JY, Hong SP, Kim TI, Kim WH, Cheon JH. Influence of age at diagnosis and sex on clinical course and long-term prognosis of intestinal Behcet’s disease. Inflamm Bowel Dis. 2012;18(6):1064–71.
• Karatemiz G, Esatoglu SN, Gurcan M, et al. Frequency of AA amyloidosis has decreased in Behcet’s syndrome: a retrospective study with long-term follow-up and a systematic review. Rheumatology (Oxford). 2022;62(1):9–18. (This study identifies BS patients who are at a high risk of developing AA amyloidosis and reports a decreasing frequency of AA amyloidosis among BS patients over time.)
Esatoglu SN, Hatemi G, Salihoglu A, Hatemi I, Soysal T, Celik AF. A reappraisal of the association between Behcet’s disease, myelodysplastic syndrome and the presence of trisomy 8: a systematic literature review. Clin Exp Rheumatol. 2015;33(6 Suppl 94):S145–51.
• Yilmaz U, Ar MC, Esatoglu SN, et al. How to treat myelodysplastic syndrome with clinical features resembling Behcet syndrome: a case-based systematic review. Ann Hematol. 2020;99(6):1193–203. (This case-based systematic review summarizes the clinical characteristics and treatment approaches for patients with myelodysplastic syndrome presenting with gastrointestinal involvement resembling BS.)
Yurdakul S, Mat C, Tuzun Y, et al. A double-blind trial of colchicine in Behcet’s syndrome. Arthritis Rheum. 2001;44(11):2686–92.
Calguneri M, Kiraz S, Ertenli I, Benekli M, Karaarslan Y, Celik I. The effect of prophylactic penicillin treatment on the course of arthritis episodes in patients with Behcet’s disease. A randomized clinical trial. Arthritis Rheum. 1996;39(12):2062–5.
Haimov-Kochman R, Ben-Chetrit E. The effect of colchicine treatment on sperm production and function: a review. Hum Reprod. 1998;13(2):360–2.
Kim JB, Kim S, Lee T, et al. Colchicine-induced rhabdomyolysis caused by interaction with clarithromycin in a patient with Behcet disease. J Clin Rheumatol. 2013;19(2):108–9.
Yazici H, Pazarli H, Barnes CG, et al. A controlled trial of azathioprine in Behcet’s syndrome. N Engl J Med. 1990;322(5):281–5.
Jung YS, Cheon JH, Hong SP, Kim TI, Kim WH. Clinical outcomes and prognostic factors for thiopurine maintenance therapy in patients with intestinal Behcet’s disease. Inflamm Bowel Dis. 2012;18(4):750–7.
Girgin S, Yurumez S, Omma A, et al. Comparison of relapse rates in Behcet’s disease with venous involvement on different doses of azathioprine therapy, a retrospective observational study. Int J Rheum Dis. 2021;24(4):562–6.
Teich N, Mohl W, Bokemeyer B, et al. Azathioprine-induced acute pancreatitis in patients with inflammatory bowel diseases—a prospective study on incidence and severity. J Crohns Colitis. 2016;10(1):61–8.
Huang MX, Wang CY, Guo JY, et al. Pharmacotherapy for Behcet’s disease and the risk of malignancy. Front Pharmacol. 2021;12:661150.
Wang X, Peng Y, Gao J, Han S, Li Y. Risk of malignancy in Behcet disease: a meta-analysis with systematic review. Medicine (Baltimore). 2019;98(44):e17735.
Masuda K, Nakajima A, Urayama A, Nakae K, Kogure M, Inaba G. Double-masked trial of cyclosporin versus colchicine and long-term open study of cyclosporin in Behcet’s disease. Lancet. 1989;1(8647):1093–6.
BenEzra D, Cohen E, Chajek T, et al. Evaluation of conventional therapy versus cyclosporine A in Behcet’s syndrome. Transplant Proc. 1988;20(3 Suppl 4):136–43.
Ozyazgan Y, Yurdakul S, Yazici H, et al. Low dose cyclosporin A versus pulsed cyclophosphamide in Behcet’s syndrome: a single masked trial. Br J Ophthalmol. 1992;76(4):241–3.
Qian Y, Qu Y, Gao F, et al. Comparison of the safety and efficacy of interferon alpha-2a and cyclosporine-A when combined with glucocorticoid in the treatment of refractory Behcet’s uveitis: a randomized controlled prospective study. Front Pharmacol. 2021;12:699903.
Akman-Demir G, Ayranci O, Kurtuncu M, Vanli EN, Mutlu M, Tugal-Tutkun I. Cyclosporine for Behcet’s uveitis: is it associated with an increased risk of neurological involvement? Clin Exp Rheumatol. 2008;26(4 Suppl 50):S84-90.
Adler YD, Mansmann U, Zouboulis CC. Mycophenolate mofetil is ineffective in the treatment of mucocutaneous Adamantiades-Behcet’s disease. Dermatology (Basel, Switzerland). 2001;203(4):322–4.
Kose O, Simsek I, Pay S. Mycophenolate sodium in the treatment of mucocutaneous Behcet’s diseases. Int J Dermatol. 2011;50(7):895–6.
Ucar D, Esatoglu SN, Cerme E, et al. Mycophenolate mofetil may be an alternative for maintenance therapy of Behcet syndrome uveitis: a single-center retrospective analysis. Rheumatol Int. 2023;43(11):2099–106.
Ozguler Y, Esatoglu SN, Hatemi G. Current pharmacological solutions for Behcet’s syndrome. Expert Opin Pharmacother. 2023;24(2):221–31.
Alpsoy E, Durusoy C, Yilmaz E, et al. Interferon alfa-2a in the treatment of Behcet disease: a randomized placebo-controlled and double-blind study. Arch Dermatol. 2002;138(4):467–71.
Keskin Y, Seyahi E, Poyraz C, Ugurlu S, Ozyazgan Y, Yazici H. Interferon alfa-associated depression in patients with Behcet’s syndrome: a prospective controlled study. Clin Exp Rheumatol. 2014;32(4 Suppl 84):S175.
Hamuryudan V, Ozyazgan Y, Fresko Y, Mat C, Yurdakul S, Yazici H. Interferon alfa combined with azathioprine for the uveitis of Behcet’s disease: an open study. Isr Med Assoc J. 2002;4(11 Suppl):928–30.
Akeno N, Smith EP, Stefan M, et al. IFN-alpha mediates the development of autoimmunity both by direct tissue toxicity and through immune cell recruitment mechanisms. J Immunol. 2011;186(8):4693–706.
•• Hatemi G, Tukek NB, Esatoglu SN, et al. Infliximab for vascular involvement in Behcet’s syndrome. Clin Immunol. 2023;253:109682. (This is the largest single-center study with long-term follow-up, reporting on the efficacy and safety of infliximab among patients with vascular involvement.)
Sener H, Evereklioglu C, Horozoglu F, Gunay Sener AB. Efficacy and safety of adalimumab in patients with Behcet uveitis: a systematic review and meta-analysis. Ocul Immunol Inflamm. 2023;10:1–9. https://doi.org/10.1080/09273948.2022.2157288.
Zhang Q, Ma C, Dong R, et al. Efficacy and safety of anti-tumor necrosis factor-alpha agents for patients with intestinal Behcet’s disease: a systematic review and meta-analysis. Yonsei Med J. 2022;63(2):148–57.
• Gazel U, Kocakaya D, Hicret Topcu I, et al. Risk of tuberculosis is increased in Behcet’s disease compared to other rheumatological disorders after anti-TNFalpha treatments: a case series and review of the literature. Turk J Med Sci. 2021;51(4):1689–94. (This study underscores the elevated risk of tuberculosis among BS patients when compared to those with other rheumatic diseases.)
Gabriel SE. Tumor necrosis factor inhibition: a part of the solution or a part of the problem of heart failure in rheumatoid arthritis? Arthritis Rheum. 2008;58(3):637–40.
Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL, Montori V. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA. 2006;295(19):2275–85.
The Lenercept Multiple Sclerosis Study Group and The University of British Columbia MS/MRI Analysis Group. TNF neutralization in MS: results of a randomized, placebo-controlled multicenter study. Neurology. 1999;53(3):457–65.
Diamantopoulos AP, Hatemi G. Lack of efficacy of tocilizumab in mucocutaneous Behcet’s syndrome: report of two cases. Rheumatology (Oxford). 2013;52(10):1923–4.
Emmi G, Silvestri E, Squatrito D, Emmi L, Cantarini L, Prisco D. Tocilizumab-induced exacerbation of mucosal ulcers in a patient with multi-refractory Behcets disease. Semin Arthritis Rheum. 2016;46(1):e1-2.
• Akiyama M, Kaneko Y, Takeuchi T. Effectiveness of tocilizumab in Behcet’s disease: a systematic literature review. Semin Arthritis Rheum. 2020;50(4):797–804. (This systematic review reported the effectiveness of tocilizumab among BS patients and also noted exacerbations of mucocutaneous lesions with this agent.)
Barroso-Garcia N, Atienza-Mateo B, Ferraz-Amaro I, et al. Anti-TNF vs tocilizumab in refractory uveitic cystoid macular edema due to Behcet’s disease. Multicenter study of 49 patients. Semin Arthritis Rheum. 2023;58:152153.
Khitri MY, Bartoli A, Maalouf G, et al. Tocilizumab in Behcet disease: a multicenter study of 30 patients. J Rheumatol. 2023;50(7):916–23.
Arnold DD, Yalamanoglu A, Boyman O. Systematic review of safety and efficacy of IL-1-targeted biologics in treating immune-mediated disorders. Front Immunol. 2022;13:888392.
Bettiol A, Silvestri E, Di Scala G, et al. The right place of interleukin-1 inhibitors in the treatment of Behcet’s syndrome: a systematic review. Rheumatol Int. 2019;39(6):971–90.
Dick AD, Tugal-Tutkun I, Foster S, et al. Secukinumab in the treatment of noninfectious uveitis: results of three randomized, controlled clinical trials. Ophthalmology. 2013;120(4):777–87.
Di Scala G, Bettiol A, Cojan RD, Finocchi M, Silvestri E, Emmi G. Efficacy of the anti-IL 17 secukinumab in refractory Behcet’s syndrome: a preliminary study. J Autoimmun. 2019;97:108–13.
Dincses E, Yurttas B, Esatoglu SN, Melikoglu M, Hamuryudan V, Seyahi E. Secukinumab induced Behcet’s syndrome: a report of two cases. Oxf Med Case Rep. 2019;2019(5):omz041.
Barrado-Solis N, Rodrigo-Nicolas B, De la Morena-Barrio I, et al. Report of two cases of Behcet’s disease developed during treatment with secukinumab. J Eur Acad Dermatol Venereol. 2020;34(10):e587–9.
Calleja Algarra A, Aragon Miguel R, Andres Lencina JJ, et al. Behcet’s-like disease during secukinumab treatment: new paradoxical reaction? J Dtsch Dermatol Ges. 2021;19(1):116–8.
Sun FSK, Chiu NSY, Chung HY. Potential gastrointestinal Behcet’s disease flare after treatment with anti-interleukin 17a therapy. BMC Rheumatol. 2023;7(1):25.
Avci C, Akin G, Akarsu S, Lebe B. Pyoderma gangrenosum and Behcet’s-like disease induced by secukinumab: a paradoxical drug reaction. J Dermatolog Treat. 2023;34(1):2235040.
Hatemi G, Mahr A, Ishigatsubo Y, et al. Trial of apremilast for oral ulcers in Behcet’s syndrome. N Engl J Med. 2019;381(20):1918–28.
Hatemi G, Melikoglu M, Tunc R, et al. Apremilast for Behcet’s syndrome—a phase 2, placebo-controlled study. N Engl J Med. 2015;372(16):1510–8.
•• Mease PJ, Hatemi G, Paris M, et al. Apremilast long-term safety up to 5 years from 15 pooled randomized, placebo-controlled studies of psoriasis, psoriatic arthritis, and Behcet’s syndrome. Am J Clin Dermatol. 2023;24(5):809–20. (This systematic review provides support for the long-term safety of apremilast therapy.)
Liu J, Yu X, Wang Z, et al. Baricitinib for the treatment of intestinal Behcet’s disease: a pilot study. Clin Immunol. 2023;247:109241.
Zou J, Lin CH, Wang Y, Shen Y, Guan JL. Correspondence on ‘A pilot study of tofacitinib for refractory Behcet’s syndrome’. Ann Rheum Dis. 2023;82(4):e100. https://doi.org/10.1136/annrheumdis-2020-219810.
Liu J, Hou Y, Sun L, et al. A pilot study of tofacitinib for refractory Behcet’s syndrome. Ann Rheum Dis. 2020;79(11):1517–20.
Wang Z, Wang X, Liu W, et al. Baricitinib for the treatment of refractory vascular Behcet’s disease. Clin Immunol. 2023;250:109298.
Author information
Authors and Affiliations
Contributions
S.N.E. wrote the manuscript and prepared table 2. Y.O. wrote the manuscript and prepared table 1. G.H. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Sinem Nihal Esatoglu has received honorariums for presentations from UCB Pharma, Roche, Pfizer, and Merck Sharp Dohme. Yesim Ozguler has received honorariums for presentations from UCB Pharma, Novartis, and Pfizer. Prof Hatemi has received research grant, lecture fees and fees for serving on an advisory board from Celgene, receiving consulting fees from UCB Pharma, Bayer, Johnson & Johnson, lecture fees from Novartis, Abbvie, Amgen, and UCB Pharma.
Conflict of Interest
Sinem Nihal Esatoglu has received honorariums for presentations from UCB Pharma, Roche, Pfizer, and Merck Sharp Dohme. Yesim Ozguler has received honorariums for presentations from UCB Pharma, Novartis, and Pfizer. Prof Hatemi has received research grant, lecture fees, and fees for serving on an advisory board from Celgene; consulting fees from UCB Pharma, Bayer, and Johnson & Johnson; and lecture fees from Novartis, Abbvie, Amgen, and UCB Pharma.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Esatoglu, S.N., Ozguler, Y. & Hatemi, G. Disease and Treatment-Specific Complications of Behçet Syndrome. Curr Rheumatol Rep 26, 1–11 (2024). https://doi.org/10.1007/s11926-023-01124-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-023-01124-7