Abstract
Purpose of Review
This review aims to provide an update on the use of imaging in the assessment of juvenile spondyloarthritis (JSpA) disease manifestations.
Recent Findings
Recent studies have demonstrated superior reliability and specificity of MRI for assessment of sacroiliac joint inflammation compared with radiography. The use of gadolinium contrast may not add incremental value to the assessment of inflammatory sacroiliitis. Sacroiliitis is common at diagnosis of spondyloarthritis. Inflammatory changes of the lumbar spine are not uncommon, and changes over time in the sacroiliac and apophyseal joints may not be concordant. Ultrasonography (US) in turn has been recognized as an excellent imaging technique to visualize the peripheral manifestations of JSpA. US does not only add important information to the clinical assessment but also helps to understand the complexity of the enthesis. Recognition of specific aspects in children is important though. The standardization of image acquisition as well as the establishment of the evidence base are underway.
Summary
MRI and ultrasonography are recognized as increasingly important tools in the diagnosis and management of juvenile spondyloarthritis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spondyloarthritis is a category of juvenile arthritis that encompasses a group of heterogeneous conditions characterized by arthritis, enthesitis (inflammation at tendon insertions), psoriasis, inflammatory bowel disease, acute symptomatic uveitis, and HLA-B27 positivity. The presence of enthesitis, axial (spine or sacroiliac) arthritis, and symptomatic uveitis distinguishes spondyloarthritis from other categories of juvenile arthritis. This article provides an update regarding the use of imaging for assessment of juvenile spondyloarthritis disease manifestations and disease activity. Magnetic resonance imaging (MRI) and ultrasonography including Doppler have increasingly important roles in the assessment of axial and peripheral disease manifestations, respectively.
Classification
Juvenile arthritis is the most common rheumatic condition of childhood, affecting 3–4/1000 children [1]. Spondyloarthritis accounts for 10–15 % of juvenile arthritis cases in North America and Europe, and it is the most common category of juvenile arthritis in Asia [2–7]. The International League of Associations for Rheumatology (ILAR) criteria defines seven mutually exclusive categories of arthritis [8]. Under this terminology, most children with spondyloarthritis are classified as enthesitis-related arthritis, psoriatic arthritis, and undifferentiated arthritis. Conditions traditionally considered under the spondyloarthritis umbrella term that are not specifically considered under the ILAR schema include reactive arthritis, inflammatory bowel disease-related arthropathy, and juvenile ankylosing spondylitis (e.g., isolated sacroiliitis). In addition to the ILAR criteria, the European Spondyloarthropathy Study group (ESSG) [9] and Amor [10] criteria for spondyloarthritis are sometimes also applied to children, though they were developed for use in adults.
Clinical Manifestations
The defining characteristics of spondyloarthritis include male predominance, HLA-B27 positivity, axial arthritis, enthesitis, and painful uveitis. Peak age of onset is early adolescence. The most commonly affected joints are weight-bearing joints including the knees, ankles, and sacroiliac joints [11]. The small joints of the hands and feet are affected in fewer than 10 % of children [11]. Midfoot arthritis is highly suggestive of spondyloarthritis. The majority of children have oligoarticular involvement (<5 joints). Sacroiliitis affects one third to one half of children within several years of disease onset [12–15]. Prevalence of reported sacroiliitis is highly dependent upon the criteria used to define sacroiliitis (clinical, radiographic, or MRI). In one study of unselected children with juvenile spondyloarthritis, 20 % had sacroiliitis, using the Assessment of Spondyloarthritis International Society (ASAS) MRI definitions for active sacroiliitis, within 6 months of diagnosis [16•]. In another study of prevalent disease, more than one third of children had clinical or imaging evidence of sacroiliitis [13]. In this study, children with hip arthritis had increased odds of having sacroiliitis (OR, 11.5).
Most children with spondyloarthritis have at least one tender enthesis. In a prospective study of children newly diagnosed ERA, more than half of children reported pain at six or more entheses [17]. Tenderness was most frequent at the insertions of the patellar ligament and quadriceps on the patella. More than half of children in this study also had enthesitis detectable by ultrasound with Doppler, as defined by the Outcomes Measures in Rheumatology (OMERACT) criteria [18•]. In a study of children with prevalent disease, more than 80 % of children had enthesitis by ultrasound with Doppler, 13 % of which demonstrated chronic changes (enthesophytes, erosion, calcification) [19]. The most frequently affected sites were the insertions of the infrapatellar tendon on the tibial tuberosity, Achilles, and quadriceps.
In contrast to ocular inflammation observed in other categories of juvenile arthritis, uveitis in spondyloarthritis is characteristically painful, red, and recurrent. An estimated 7 % of children with ERA develop uveitis [20]. HLA-B27 positivity is significantly associated with development of uveitis [21]. Screening for uveitis is recommended at a minimum interval of every 12 months. Children with psoriatic arthritis, however, tend to have asymptomatic uveitis that can only be diagnosed through routine ophthalmic screening, recommended at either 3 or 6 months intervals depending on age and antinuclear antibody (ANA) status. The risk of developing uveitis in psoriatic arthritis increases in those with disease onset at before age 7 and ANA positivity [20].
Imaging Evaluation of Axial Disease
Sacroiliac Joint
The sacroiliac joint is a diarthroidal joint between the sacrum and the ilium. In the lower ventral part, the sacral surface is covered with hyaline cartilage while the iliac surface is covered with a thin layer of fibrocartilage. The upper dorsal part is a syndesmosis or fibrous joint in which the bone surfaces are supported by numerous interosseous ligaments. Bony defects most often appear first on the iliac joint margin as the iliac cartilage is thinner as compared with the sacral side [22]. The inferior third of the joint resembles a synovial joint with synovial lining [23]. The transition zone between the proximal 2/3 of the joint and the distal third is characterized by vascular connective tissue and cartilage and subchondral defects [23]. There are several extrinsic liagments that contribute to the stability of the joint and include the ventral and dorsal sacroiliac, sacrospinous and sacrotuberous, and iliolumbar ligaments [22].
Imaging Technique
MRI is recognized as an increasingly important tool to aid in the diagnosis and management of axial disease in juvenile arthritis. MRI is established as a sensitive imaging modality for detection of synovitis as well as cartilage and bone destruction. MRI has distinct advantages over radiographs for the assessment of axial disease, since bone marrow edema on fluid-sensitive MRI sequences may be visible years prior to radiographic change (Fig. 1). Despite these advantages, radiographs remain the gold standard for diagnosis of ankylosing spondylitis and are required prior to MRI authorization by many insurance companies in the USA. In a study by Jaremko et al., the reliability and specificity of MRI of the pediatric sacroiliac joint were superior to conventional radiography [24•]. Reliability of global diagnosis on MRI was excellent (κ = 0.8) and while reliability for radiographs was poor (κ = 0.3). Authors of this study suggested that MRI should replace conventional radiography in the evaluation of suspected inflammatory sacroiliac disease.
MRI versus radiographs. Sixteen-year-old boy with JSpA, HLA-B27 positive. a AP radiograph of the pelvis demonstrates normal sacroiliac joints without evidence of sclerosis, erosions, joint space widening, or ankylosis. b Coronal oblique STIR image and c axial oblique T2-weighted fat-saturated image of the sacroiliac joints demonstrates bilateral sacroiliitis with bone marrow edema seen along the sacral and iliac aspects of the both joints (arrows). d Coronal oblique T1-weighted image shows corresponding low signal in regions of bone marrow edema without evidence of structural damage
Until recently, the utility of intravenous MRI gadolinium contrast for the evaluation of suspected inflammatory sacroiliitis had not been examined and the use of gadolinium was common. In a study by Weiss et al., the sensitivity and specificity of fluid-sensitive (non-contrast) MRI sequences to detect periarticular bone marrow edema were near perfect, using the study that included post-contrast sequences as the reference standard (Fig. 2) [25•]. This study affirmed that the use of gadolinium contrast was not necessary and that its use added unnecessary cost and risk. These findings were confirmed by a subsequent European study by Herregods et al. [26•]. Use of gadolinium contrast for imaging of the sacroiliac joints should be reserved for when the differential diagnosis includes etiologies such as infection or tumor, in which case contrast enhancement may be helpful. Recommended sequences for routine imaging of the sacroiliac joint with dedicated MR in children have been published and include: coronal oblique (parallel to the long axis of the sacrum) T1-weighted and short tau inversion recovery (STIR), axial oblique (perpendicular to the long axis of the sacrum) T2-weighted fat-saturated, large field-of-view coronal T2-weighted fat-saturated images of the entire pelvis [25•]. Large field-of-view pelvic imaging allows for depiction of pelvic and hip enthesitis as well as hip effusions.
Use of fluid sensitive images (STIR) versus contrast-enhanced images. Six-year-old girl with jSpA, HLA-B27 positive. a Coronal oblique STIR image demonstrates periarticular bone marrow edema within the left sacrum and adjacent ilium (solid arrows). There is edema adjacent to the capsule (dashed arrow). On the coronal oblique T1-weighted post-contrast image (b), there is corresponding enhancement of regions of bone marrow edema (solid arrows) and capsulitis (dashed arrow) in a similar pattern to the STIR image. There is mild synovitis within the inferior aspect of the left sacroiliac joint (arrowhead) which can only be characterized on post-gadolinium imaging. Bilateral iliac bone sclerosis is noted (asterisk)
Lesions indicative of active inflammation are best seen on fluid-sensitive sequences including T2-weighted fat saturated and STIR. Bone marrow edema is essential for defining sacroiliitis according to the ASAS/OMERACT task force [27]. Bone marrow edema is defined as hyperintense signal on fluid-sensitive sequences (T2-weighted fat saturated or STIR). On T1-weighted sequences, marrow edema has corresponding hypointensity (Fig. 3). Other features of active sacroiliitis may include capsulitis, synovitis, enthesitis, and effusion; the presence of any of these features in the absence of bone marrow edema is not sufficient to define active sacroiliitis. Chronic lesions of the sacroiliac joints are best-visualized used T1-weighted sequences. Chronic lesions that may be seen in the pediatric population include erosion, sclerosis, fat metaplasia, backfill, and ankylosis. It is important to note that all lesions with the exception of synovitis can be adequately assessed with non-contrast MRI. In order to evaluate for active synovitis, IV gadolinium contrast must be administered.
Fifteen-year-old boy, HLA-B27 positive, with active sacroiliitis. a Coronal oblique STIR image of the superior aspect of the sacroiliac joints demonstrates bone marrow edema along the sacral and iliac aspects of both joints (arrows) consistent with active inflammation. b Coronal oblique T1-weighted image shows abnormal high signal along the periarticular surface of both joints (dashed arrows) consistent with backfill. c Coronal oblique T1-weighted image slightly more dorsal demonstrates bilateral iliac bone erosions (arrows). d Coronal T2-weighted fat-saturated image of the entire pelvis shows bilateral hip enthesitis with soft tissue edema at the tendon insertions (arrows) and accompanying bone marrow edema
Evaluating the sacroiliac joints in children is challenging due to the age-dependent developmental changes that occur. The sacrum develops from segmental apophyses that become progressively ossified from age 9 to 16 years [22]. This process occurs earlier in girls than boys. Apophyseal fusion occurs between the ages of 16 and 20 years [28]. The lateral apophyses of the sacral wings in skeletal immature children contain cartilaginous margins that demonstrate cartilaginous signal which is relatively hyperintense compared with the adjacent bone and can be misinterpreted as bone marrow edema on MRI fluid-sensitive sequences [28] (Fig. 4). The use of diffusion weighted imaging may be a way to improve reliability of imaging interpretation. Vendhan et al. demonstrated that there was increased diffusion in children with inflammatory sacroiliitis versus controls and that diffusion scores correlated well with STIR [29•]. The incremental value of diffusion sequences over standard MRI imaging protocols has yet to be tested.
Normal findings in the maturing pelvis. Coronal oblique STIR image of the sacroiliac joints in a healthy 9-year-old girl. The normal sacral apophyseal cartilage (arrows) demonstrates increased signal intensity compared with the adjacent bone marrow (asterisk). The cartilage signal appears symmetric and fairly uniform in thickness along both joints
Whole body MRI has been used as an outcome in a clinical trial of adults with spondyloarthritis [30]. The advantage of whole body MRI over dedicated pelvic MRI is the ability to assess the full range of affected entheses and joints. The disadvantage of this technique for imaging of the axial joints is that the number of slices through the region is fewer and lesions may be missed. There is limited data on the utility of whole body MRI in children with spondyloarthritis but a pediatric protocol has been published [31•]. Preliminary data in children suggest that whole body MRI is more sensitive than clinical examination for detection of arthritis [32, 33].
MRI Evaluation of Axial Involvement
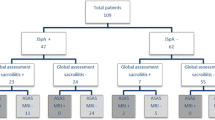
Weiss et al. used MRI in an unselected group of children with spondyloarthritis to assess the prevalence of sacroiliitis at disease onset. Of the 40 children included in this prospective study, 20 % had active sacroiliitis detectable on MR imaging within 6 months of diagnosis [16•]. Children with elevated inflammatory markers and HLA-B27 positivity had the highest predicted probability of having sacroiliitis. The majority of those with active inflammatory lesions also had evidence of erosion or sclerosis, suggesting that the disease was long-standing or rapidly progressive. Only 1/3 of the children had back pain, suggesting that clinicians must maintain a high suspicion for sacroiliitis in this population. Children with an elevated C-reactive protein and HLA-B27 positivity had the highest predicted probability of having sacroiliitis. In a study of children with prevalent disease (median disease duration 15 months), 30 % of children with enthesitis-related arthritis developed both inflammatory back pain and MRI findings of active sacroiliitis [15]. In this cohort, higher active joint tender entheses counts at disease onset were significantly associated with sacroiliitis.
Vendhan et al. evaluated utility of MRI with contrast to assess inflammatory spinal lesions in children [34•]. Synovitis of at least one apophyseal joint was identified in 38 % of children, and end-plate edema was present in 7 %. Sacroiliitis was present in the majority of children with spinal lesions. In a subsequent retrospective study of 31 children with enthesitis-related arthritis who underwent at least two MRIs for clinical suspicion of axial disease, it was rare for there to be apophyseal joint inflammation in the absence of sacroiliitis [35•]. At initial scan, 90 % had sacroiliitis, 68 % had sacroiliitis and apophyseal joint inflammation, and 6 % (two patients) had apophyseal joint inflammation in the absence of sacroiliitis. Interestingly, serial imaging revealed that inflammatory changes over time in the sacroiliac and apophyseal joints were concordant in only approximately one third of cases.
MRI is also useful to assess pelvic enthesitis. In one study, 16 % of children who underwent pelvic MRI for suspected sacroiliitis had pelvic enthesitis [36•]. The most common sites were the entheses around the hip and the retroarticular interosseous ligaments. Three quarters of children with pelvic enthesitis also had sacroiliitis. In several children, the presence of enthesitis on MRI would have enabled them to fulfill ILAR ERA criteria. In a cross-sectional study that used whole-body MRI, the most common site of enthesitis was the insertion of the hip extensor at the greater trochanter [32]. In a prospective study of unselected children with a new diagnosis of juvenile spondyloarthritis, 7/40 (18 %) had hip enthesitis and 1/40 had sacroiliac enthesitis; of those with enthesitis, all but one had concomitant sacroiliitis [16•]. In another study of 11 children with inflammatory back pain for approximately 1 year, all had findings consistent with pelvic enthesitis [37]. The most common sites were the symphysis pubis (82 %) and hip trochanters (55 %).
Imaging Evaluation of Peripheral Disease
Enthesis
The enthesis is a relatively complex structure consisting of several components including the tendon itself, various portions of fibrocartilage, sub-tendinous bursae, fat, and the insertion of tendon fibers into bone through fibrocartilage [38] (Fig. 5). Histologic and molecular analyses suggest that all of these components may play important and distinct roles in the pathogenesis of enthesitis [38, 39] extending the view of the enthesis from a simple insertion of tendon fibers into bone to an entire “enthesis organ.” As all of these structures can be shown very well with ultrasonography [40] (Fig. 5), new and exciting opportunities are opening up for a better understanding of the enthesis in health and disease.
Imaging Technique
Whereas MRI plays a very important role in the imaging of the axial skeleton, most peripheral joints and the enthesis in particular are very accessible for ultrasonography and can be reliably imaged using this technique [41–44]. Ultrasonography has distinct advantages over MRI being much less costly and time consuming [45]. In addition, it has a superior spatial resolution which is especially important in the assessment of smaller entheses like those of the extensor tendons and collateral ligaments of the fingers (Fig. 6). Visualization of these structures has enhanced our understanding of the complexity of the musculoskeletal system in these areas including the associated pathology, for example, in dactylitis [46]. The functional assessment at variable angles of the tendon insertion might offer unique advantages to detect pathology. This also applies to secondary damage, for example, (partial) tendon rupture, which can be detected most reliably by putting different degrees of tension on the tendon. Several entheses can be assessed at the same time, and the exam can also be conducted in younger children without the need for sedation. [17]. The real-time imaging capabilities enable the examiner to directly correlate imaging and clinical findings and also to demonstrate findings to the patient and parents. Finally, the lack of ionizing radiation is particularly important in children.
Imaging Characteristics of the Enthesis Tendon Complex
Normal tendons have a very regular, echogenic, fibrillar appearance on ultrasound. This results from the arrangement of the tendon fascicles formed by the tendon fibers (Fig. 7). On the basic molecular level, collagen molecules aggregate into microfibrils and then into collagen fibrils [47]. A number of collagen fibrils form a collagen fiber, which is the basic unit of a tendon. Within collagen fibers, the structure is much less regular than at the level of the fascicles. The fibrils are oriented longitudinally, transversely, and horizontally allowing adaptation to the various mechanical requirements of the tendon at various angles. Several collagen fibers form a primary fiber bundle (subfascicle), and a group of primary fiber bundles forms a secondary fiber bundle or fascicle. A group of fascicles forms a tertiary bundle, and the tertiary bundles make up the tendon surrounded by the epitenon. The fascicles represent the very regular structure of the tendon seen on ultrasonography.
Regular tendon structure on ultrasonography and anisotropy. Longitudinal view of a peroneus tendon running along the fibula and showing the very regular fibrillar pattern of a tendon on ultrasonography. At the right side of the image, the tendon turns very dark due to a change of direction and the occurrence of anisotropy (white arrows). This artifact should not be mistaken for pathology. The bone of the fibula does show an interruption representing the growth plate with the subsequent bone representing the epiphysis
Many tendons are surrounded by connective tissue called paratenon (for example, the Achilles tendon) providing an elastic sleeve for the tendon [47]. The paratenon is lined on its inner surface by synovial cells [47–49]. Other tendons have synovial sheaths [47]. Under a fibrous layer two thin and serous sheets, the parietal and visceral sheet, are found and they are lined with synovial cells as well.
Fluid within the synovial sheath appears as an anechoic halo surrounding the tendon while synovial thickening appears as a hypoechoic thickening around the tendon. Fluid accumulating in the paratenon can also be shown as a thin anechoic structure surrounding the tendon. Vascular anatomy can be assessed by Doppler. Synovial hyperemia, for example, leads to increased Doppler signals in the tendon sheath. Increased blood flow can also be demonstrated by Doppler sonography in the peritendinous area of tendons having a paratenon.
As the tendon inserts into bone, it will transition through a layer of fibrocartilage, which has essential mechanical functions of stress dissipation [38, 39]. The fibrocartilage can be visualized as a thin anechoic layer between the tendon fibers and the echoic surface of the bone [40] (Fig. 5). Other relevant structures of the entheseal complex that can be seen on ultrasonography are subtendinous fat pads (Fig. 5) as well as bursae surrounding the enthesis which are often not visible in healthy conditions but will appear as hypoechoic structures with increasing dimensions in the case of bursitis.
Technical Aspects
Due to the superficial location of most entheses, high-frequency transducers are typically being used in B-mode [18•]. With regard to Doppler imaging, low flow settings with a low pulse-repetition frequency and low wall filter are preferred in order to maximize sensitivity [18•]. The Doppler box as well as the gain need to be adjusted to allow maximum sensitivity without creating artifacts. It is important to avoid Doppler artifacts which will especially occur close to the bone cortex as they can easily be misinterpreted as signals suggestive of enthesitis. Tendons, due to the very regular structure of their fascicles, are prone to an artifact called “anisotropy” (Fig. 7). This can be avoided by changing the angle of the probe relative to the tendon during the exam in order to visualize all areas of the tendon correctly and not to misinterpret areas of anisotropy as pathologic.
Several other factors will influence findings as well. For example, in adult runners with asymptomatic knees, a high percentage showed fluid accumulation around the iliotibial band [50•]. These findings were very position dependent. When examined in full extension with the subject supine, fluid was seen in 67.5 % of knees (n = 40) compared with 95 % of the knees when standing. When examined in 30° of flexion, the presence of fluid decreased to 30 % when supine and 22.5 % when standing. With regard to Doppler signals at the enthesis, it has also been known for some time that in addition to the joint position [51], the time of the day as well as the activity level preceding the assessment will influence Doppler findings in particular. This as well as the inherent dependence of ultrasonography on the operator has led to concerns about the reliability of ultrasound assessments. Pediatric data are limited at this point, but several studies on the pediatric enthesis have included interrater reliability assessments with good results [17, 52, 53 54•, 55•]. These assessments have nevertheless not determined the reliability of assessing the same healthy control person or patient by various sonographers on the same day or assessing the same person at different time points. One pediatric study has assessed the same enthesis in healthy children at different degrees of flexion of the associated joint [54•]. The authors did not find a consistent pattern of sensitivity for Doppler signals associated with either the neutral position of the joint (relaxed tendon) or a flexed position of the joint (tendon under tension). More data on these latter aspects especially in children and adolescents will be desirable in order to validate ultrasonography of the enthesis further. In the clinical setting, as well as for research, it is probably important to assess entheses at various positions and to interpret pathologic findings on the background of findings in healthy children and adolescents at various ages.
Pediatric Enthesis
Knowledge of entheseal development in children as well as consideration of vascularization is important in order to differentiate pathologic from normal findings. From an imaging point of view, it is also important to remember that depending on the age of the child, a significant part of what later becomes the osseous insertion is still composed of hyaline cartilage as well as fibrocartilage and will therefore appear hypo- or anechoic on ultrasonography (US; illustrated schematically in Fig. 8). There are no detailed sono-anatomic descriptions for all regions, but, for example, the development of the Achilles tendon insertion has nicely been described by Fornage and Grechenig as follows: (1) from 2 months to 3 years, no ossification of the secondary center of calcaneus is visible, (2) from 4 to 6 years, early signs of the secondary ossification center appear, (3) from 7 to 11 years, the posterior bony contour of the primary ossification center of the calcaneus has got a wavy appearance, and (4) from 12 to 18 years, the secondary ossification center then appears and full ossification of the apophyseal cartilage occurs [56, 57]. Ogden has published a series of anatomic studies on ossification including entheseal/apophyseal sites which can serve as a reference to understand progression of ossification and correlate it with the sonographic images [58–61].
Schematic depiction of the enthesis in children. The three consecutive schemas show the enthesis into cartilage in the young child (top image), the insertion into cartilage through fibrocartilage with the formation of epiphyseal, as well as apophyseal ossification centers in the older child (middle image) and the mature situation with insertion of the tendon into bone through fibrocartilage (bottom image)
It is equally important to recognize physiologic blood flow which can be shown on Doppler sonography. In the case of the tendon and its enthesis, blood flow will occur within the cartilage into which the tendon inserts [52], along the tendon (peri-tendinous blood flow) as well as inside the tendon itself at various distances from its insertion (intra-entheseal vascularity) [55•]. In healthy children, intra-entheseal vascularity was shown in the very young children, mostly in the quadriceps tendon (12 %, 7 out of 60 children) and mostly of a mild degree with only two of the seven children reporting tenderness in the area. There were no findings in any Achilles, patellar, plantar, or elbow tendons [55•]. Peri-tendinous blood flow in contrast was found mostly in the middle age group, 3.3 % (2/60) of patellar entheses, 6.7 % (4/60) of quadriceps entheses, and 1.7 % (1/60) of the common flexor tendon were positive all of them with mild vascularity and none of them tender on examination [55•]. Another publication only found Doppler signals within the cartilage in the younger children [52]. In contrast, Roth and diGeso have shown intra-entheseal Doppler signals in up to 20 % of children in a 12–14-year age group within 2 mm of the enthesis of the quadriceps and distal patella tendon insertion [54•]. No signals were seen at the insertion of the proximal patella tendon and the Achilles tendon, and the findings were independent of the degree of flexion of the knee joint [54•]. Almost all of the signals were mild but some, especially at the quadriceps insertion, were actually more significant.
All of these findings illustrate the need to interpret Doppler signals carefully in terms of their precise location and also to distinguish various entheses in terms of their sensitivity versus specificity for Doppler findings. These might need to be differentiated further according to various age groups. More date on healthy children is clearly needed but even at the present time ultrasonography can be used reliably in patients when exerting caution in not over-interpreting mild signals and considering the possibility of physiologic signals especially in regions like the quadriceps insertion and the tibial tuberosity. Studies comparing patients and healthy controls [17, 53] have shown that Doppler findings are much more prevalent in patients. In addition, ultrasonography is often most helpful in the context of the clinical history and exam and also has great value in longitudinal assessments. At times, the isolated interpretation of a cross-sectional ultrasound exam out of the clinical context might not be enough to come to a meaningful conclusion.
Apophysitis
Traction apophysitis is a term used to describe the occurrence of insertional tendinopathy at an apophyseal site and possible avulsion of osteochondral fragments [61]. It needs to be differentiated from enthesitis as a manifestation of jSpA. The most common examples are Osgood-Schlatter’s disease at the site of the patellar tendon’s insertion into the proximal tibia and Sever’s disease at the insertion of the Achilles tendon into the calcaneus. The inflammation and injury result from chronic repetitive traction exceeding the resistance to tensile forces at the insertion site of the tendon. It will typically occur during a period of rapid growth, especially in physically very active children. This period coincides with the ossification of the previously cartilaginous insertion of the tendon. The differentiation of apophysitis from enthesitis as in enthesitis-related arthritis can be achieved through history and clinical exam as well as the imaging characteristics.
Apophysitis tends to present more in single locations and in characteristic age groups (Severs disease around the age of 10 in contrast to Osgood Schlatters around the age of 13–15). Symptomatology will be worse with exercise as opposed to the morning symptomatology in enthesitis-related arthritis. ERA will often involve multiple locations and include synovitis as well. Finally, the fragmentation of the apophyseal bone is a feature seen more with apophysitis than with ERA. The two conditions are another excellent example of how ultrasound imaging can provide a very detailed assessment enhancing the clinical assessment but at the same time becomes most powerful when interpreted in light of clinical findings.
Spondylarthritis and Enthesitis-Related JIA
In adults, a significant amount of work on the ultrasound imaging of the enthesis has been completed by various authors and the Outcome Measures in Rheumatology (OMERACT) group [18•, 62–66]. The main entheseal abnormalities that can be detected by US include tendon edema, loss of fibrillar echotexture, tendon thickening, tendon tear, calcifications, bone erosions, enthesophytes, adjacent bursitis, and increased blood perfusion (intraentheseal and/or perientheseal). OMERACT defines enthesopathy on ultrasonography as an “abnormally hypoechoic (loss of normal fibrillar architecture) and/or thickened tendon or ligament at its bony attachment that may occasionally contain hyperechoic foci consistent with calcification, that should be assessed in 2 perpendicular planes and may exhibit Doppler signal, and/or bony changes including enthesophytes, erosion, or irregularity” [62]. Scoring systems have been established with the Glasgow Ultrasound Enthesitis Scoring System (GUESS) and the Madrid Sonographic Enthesis Index (MASEI) [63, 66]. In an OMERACT interrater exercise, the interobserver reliability was highest with a kappa of 0.63 for Doppler signals near the bony cortex [18•].
Entheseal inflammation can be asymptomatic and may be overlooked on clinical examination. In a study of 35 adult patients with SpA, clinical examination identified enthesitis in 22 % (75/348) of sites as compared with 56 % (195/348) of sites on ultrasound examination [63]. Similar data have been reported in pediatric studies demonstrating Doppler signals in a high percentage of asymptomatic entheseal sites. Weiss et al. [17] found that US-confirmed enthesitis is common in children with ERA, particularly at the insertions of the quadriceps, the common extensor and the Achilles tendons.
It is important to note that no uniform definition for the diagnosis and grading of enthesitis in children exists in ultrasonography. Secondary changes (calcifications, enthesophytes) have been observed much less in children compared with adults [17, 53]. The specificity of Doppler signals close to the enthesis for spondylarthritis is not uniform either. Signals at the enthesis <2 mm of the bony cortex are thought to be very specific for spondylarthropathies [67] but can be observed in sports’ lesions as well. The careful interpretation of findings in the clinical context and the differentiation of various entheses therefore seems to be mandatory [54•]. For example, the quadriceps and distal patella tendon insertion may not be as specific than other sites for findings of enthesitis especially when it comes to Doppler ultrasonography [54•] (Fig. 9). Further work is needed in order to precisely define the various grades on semiquantitative scoring methods as well as the definition of a threshold suggesting pathologic Doppler signals.
Ultrasound images of enthesitis-related JIA before and after treatment. Images showing findings in a 10-year-old patient with enthesitis-related JIA with increased Doppler signals at the quadriceps insertion pre-treatment (top left) as well as proximal patella tendon insertion pre-treatment (top right) as well as post-treatment for the quadriceps tendon (bottom left) and proximal patella tendon (bottom right). Note the persistence of some Doppler signals in the quadriceps tendon post-treatment which may well be physiologic whereas signals in the proximal patella tendon disappear completely
Another way to avoid some of the dilemmas of cross-sectional assessments is to use Doppler sonography in longitudinal assessments. Tse and colleagues [68] demonstrated the ability of color Doppler sonography to show improvement in increased vascularity at the cortical bone insertion of enthesis and along the adjacent synovium in children with enthesitis-related arthritis. Longitudinal studies on adult patients with SpA have also highlighted the role of the perientheseal structures by showing excellent responsiveness of imaging findings following treatment [64]. These structures, which are very important demonstrating the complexity of the enthesis organ (detailed above), should therefore be part of the assessment both for diagnosis as well as therapeutic monitoring and will add further value to the addition of ultrasound imaging as they cannot be assessed in detail on clinical exam.
Recent publications have also demonstrated the value of assessing entheses which are less commonly studied. For example, Fasth et al. have published a detailed assessment of the proximal gluteal enthesis carefully distinguishing findings in healthy children from pathology in order to allow a reliable assessment with ultrasonography [69]. This publication provides an excellent blue print on how to study a pediatric enthesis including blood flow at various ages in health and disease.
Conclusions
MRI and ultrasonography have already enhanced our understanding of pathologic processes in jSpA tremendously and provide a more comprehensive assessment than the clinical exam alone.
More studies on healthy children as well as prospective trials on patients will nevertheless be beneficial to provide a solid evidence base for its use. In ultrasonography, further standardization including the development of pediatric scoring systems for B-mode and Doppler findings will be important next steps.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Petty RE, Laxer RM, Lindsley CB, Wedderburn LR. Textbook of pediatric rheumatology, 7th edition: Elsevier; 2016.
Minden K, Niewerth M, Listing J, Biedermann T, Bollow M, Schontube M, et al. Long-term outcome in patients with juvenile idiopathic arthritis. Arthritis Rheum. 2002;46(9):2392–401.
Kunjir V, Venugopalan A, Chopra A. Profile of Indian patients with juvenile onset chronic inflammatory joint disease using the ILAR classification criteria for JIA: a community-based cohort study. J Rheumatol. 2010;37(8):1756–62.
Oen K, Duffy CM, Tse SM, Ramsey S, Ellsworth J, Chedeville G, et al. Early outcomes and improvement of patients with juvenile idiopathic arthritis enrolled in a Canadian multicenter inception cohort. Arthritis Care Res. 2010;62(4):527–36.
Nordal E, Zak M, Aalto K, Berntson L, Fasth A, Herlin T, et al. Ongoing disease activity and changing categories in a long-term nordic cohort study of juvenile idiopathic arthritis. Arthritis Rheum. 2011;63(9):2809–18.
Modesto C, Anton J, Rodriguez B, Bou R, Arnal C, Ros J, et al. Incidence and prevalence of juvenile idiopathic arthritis in Catalonia (Spain). Scand J Rheumatol. 2010;39(6):472–9.
Davies R, Carrasco R, Foster HE, Baildam EM, Chieng SE, Davidson JE, et al. Treatment prescribing patterns in patients with juvenile idiopathic arthritis (JIA): analysis from the UK Childhood Arthritis Prospective Study (CAPS). Semin Arthritis Rheum. 2016.
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31(2):390–2.
Dougados M, van der Linden S, Juhlin R, Huitfeldt B, Amor B, Calin A, et al. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991;34(10):1218–27.
Amor B, Dougados M, Mijiyawa M. Criteria of the classification of spondylarthropathies. Rev Rhum Mal Osteoartic. 1990;57(2):85–9.
Weiss PF, Klink AJ, Behrens EM, Sherry DD, Finkel TH, Feudtner C, et al. Enthesitis in an inception cohort of enthesitis-related arthritis. Arthritis Care Res. 2011;63(9):1307–12.
Bollow M, Braun J, Biedermann T, Mutze S, Paris S, Schauer-Petrowskaja C, et al. Use of contrast-enhanced MR imaging to detect sacroiliitis in children. Skeletal Radiol. 1998;27(11):606–16.
Stoll ML, Bhore R, Dempsey-Robertson M, Punaro M. Spondyloarthritis in a pediatric population: risk factors for sacroiliitis. J Rheumatol. 2010;37(11):2402–8.
Flato B, Hoffmann-Vold AM, Reiff A, Forre O, Lien G, Vinje O. Long-term outcome and prognostic factors in enthesitis-related arthritis: a case-control study. Arthritis Rheum. 2006;54(11):3573–82.
Pagnini I, Savelli S, Matucci-Cerinic M, Fonda C, Cimaz R, Simonini G. Early predictors of juvenile sacroiliitis in enthesitis-related arthritis. J Rheumatol. 2010;37(11):2395–401.
• Weiss PF, Xiao R, Biko DM, Chauvin NA. Assessment of sacroiliitis at diagnosis of juvenile spondyloarthritis by radiography, magnetic resonance imaging, and clinical examination. Arthritis Care Res. 2016;68(2):187–94. Important contribution to the prevalence of sacroiliitis at disease onset.
Weiss PF, Chauvin NA, Klink AJ, Localio R, Feudtner C, Jaramillo D, et al. Detection of enthesitis in children with enthesitis-related arthritis: dolorimetry compared to ultrasonography. Arthritis Rheumatol. 2014;66(1):218–27.
• Terslev L, Naredo E, Iagnocco A, Balint PV, Wakefield RJ, Aegerter P, et al. Defining enthesitis in spondyloarthritis by ultrasound: results of a Delphi process and of a reliability reading exercise. Arthritis Care Res. 2013. Important contribution to the reliability of ultrasound assessments of enthesopathy.
Shenoy S, Aggarwal A. Sonologic enthesitis in children with enthesitis-related arthritis. Clin Exp Rheumatol. 2016;34(1):143–7.
Heiligenhaus A, Niewerth M, Ganser G, Heinz C, Minden K, German Uveitis in Childhood Study Group. Prevalence and complications of uveitis in juvenile idiopathic arthritis in a population-based nation-wide study in Germany: suggested modification of the current screening guidelines. Rheumatology (Oxford). 2007;46(6):1015–9.
Gmuca S, Brandon T, Xiao R, Pagnini I, Wright T, Beukelman T, et al. Phenotypic differences between HLA-B27 positive and negative children with enthesitis-related arthritis [Abstract]. Arthritis Rheumatol. 2015;67(S10):1582.
Navallas M, Ares J, Beltran B, Lisbona MP, Maymo J, Solano A. Sacroiliitis associated with axial spondyloarthropathy: new concepts and latest trends. Radiographics: a review publication of the Radiological Society of North America, Inc. 2013;33(4):933–56.
Puhakka KB, Melsen F, Jurik AG, Boel LW, Vesterby A, Egund N. MR imaging of the normal sacroiliac joint with correlation to histology. Skeletal Radiol. 2004;33(1):15–28.
• Jaremko JL, Liu L, Winn NJ, Ellsworth JE, Lambert RG. Diagnostic utility of magnetic resonance imaging and radiography in juvenile spondyloarthritis: evaluation of the sacroiliac joints in controls and affected subjects. J Rheumatol. 2014;41(5):963–70. Important contribution that highlights the limitations of radiography versus MRI in the evaluation of inflammatory sacroiliitis.
• Weiss PF, Xiao R, Biko DM, Johnson AM, Chauvin NA. Detection of inflammatory sacroiliitis in children with magnetic resonance imaging: is gadolinium contrast enhancement necessary? Arthritis Rheumatol. 2015;67(8):2250–6. Important contribution highlighting that the use of contrast for the evaluation of inflammatory sacroiliitis is not necessary.
• Herregods N, Jaremko JL, Baraliakos X, Dehoorne J, Leus A, Verstraete K, et al. Limited role of gadolinium to detect active sacroiliitis on MRI in juvenile spondyloarthritis. Skeletal Radiol. 2015;44(11):1637–46. Important contribution highlighting that the use of contrast for the evaluation of sacroiliitis is of limited utility.
Rudwaleit M, Jurik AG, Hermann KG, Landewe R, van der Heijde D, Baraliakos X, et al. Defining active sacroiliitis on magnetic resonance imaging (MRI) for classification of axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI group. Ann Rheum Dis. 2009;68(10):1520–7.
Bray TJ, Vendhan K, Roberts J, Atkinson D, Punwani S, Sen D, et al. Association of the apparent diffusion coefficient with maturity in adolescent sacroiliac joints. J Magn Reson Imaging. 2016;44(3):556–64.
• Vendhan K, Bray TJ, Atkinson D, Punwani S, Fisher C, Sen D, et al. A diffusion-based quantification technique for assessment of sacroiliitis in adolescents with enthesitis-related arthritis. Br J Radiol. 2016;89(1059):20150775. Important paper highlighting the potential use of a novel technique to evaluate sacroiliitis.
Song IH, Hermann K, Haibel H, Althoff CE, Listing J, Burmester G, et al. Effects of etanercept versus sulfasalazine in early axial spondyloarthritis on active inflammatory lesions as detected by whole-body MRI (ESTHER): a 48-week randomised controlled trial. Ann Rheum Dis. 2011;70(4):590–6.
• Aquino MR, Tse SM, Gupta S, Rachlis AC, Stimec J. Whole-body MRI of juvenile spondyloarthritis: protocols and pictorial review of characteristic patterns. Pediatr Radiol. 2015;45(5):754–62. Important contribution as it gives a WB imaging protocol for children.
Rachlis AC, Babyn PS, Lobo-Mueller E, Tse SM. Whole body magnetic resonance imaging in juvenile spondylarthritis: will it provide cital information compared to clinical exam alone? Arthritis Rheum. 2011;63:S292.
Srinivasalu H, Hill SC, Montealegre Sanchez G, Colbert RA. Whole body magnetic resonance imaging in evaluation of enthesitis in spondyloarthropathy. Arthritis Rheum. 2012;64 Suppl 10:S848.
• Vendhan K, Sen D, Fisher C, Ioannou Y, Hall-Craggs MA. Inflammatory changes of the lumbar spine in children and adolescents with enthesitis-related arthritis: magnetic resonance imaging findings. Arthritis Care Res. 2014;66(1):40–6. This paper highlights that apophyseal joint arthritis and end plate edema is not uncommon in children with ERA.
• Bray TJ, Amies T, Vendhan K, Humphries P, Sen D, Ioannou Y, et al. Discordant inflammatory changes in the apophyseal and sacroiliac joints: serial observations in enthesitis-related arthritis. Br J Radiol. 2016;89(1065):20160353. This paper demonstrates that apophyseal joint arthritis is uncommon in the absence of sacroiliitis.
• Herregods N, Dehoorne J, Pattyn E, Jaremko JL, Baraliakos X, Elewaut D, et al. Diagnositic value of pelvic enthesitis on MRI of the sacroiliac joints in enthesitis related arthritis. Pediatr Rheumatol Online J. 2015;13(1):46. This is an interesting paper highlighting the prevalence and distribution of pelvic enthesitis in children with ERA.
Yilmaz MH, Ozbayrak M, Kasapcopur O, Kurugoglu S, Kanberoglu K. Pelvic MRI findings of juvenile-onset ankylosing spondylitis. Clin Rheumatol. 2010;29(9):1007–13.
Benjamin M, Moriggl B, Brenner E, Emery P, McGonagle D, Redman S. The “enthesis organ” concept: why enthesopathies may not present as focal insertional disorders. Arthritis Rheum. 2004;50(10):3306–13.
Benjamin M, McGonagle D. The enthesis organ concept and its relevance to the spondyloarthropathies. Adv Exp Med Biol. 2009;649:57–70. Review.
Aydin SZ, Bas E, Basci O, Filippucci E, Wakefield RJ, Celikel C, et al. Validation of ultrasound imaging for Achilles entheseal fibrocartilage in bovines and description of changes in humans with spondyloarthritis. Ann Rheum Dis. 2010;69(12):2165–8.
Lamer S, Sebag GH. MRI and ultrasound in children with juvenile chronic arthritis. Eur J Radiol. 2000;33:85–93.
Daldrup-Link HE, Steinbach L. MRI imaging of pediatric arthritis. Magn Reson Imaging Clin N Am. 2009;17:451–67.
Grassi W, Filippucci E, Busilacchi P. Musculoskeletal ultrasound. Best Pract Res Clin Rheumatol. 2004;18:813–26.
Ostergaard M, Duer A, Ejbjerg B. Magnetic resonance imaging of peripheral joints in rheumatic diseases. Best Pract Res Clin Rheumatol. 2004;18:861–79.
Damasio MB, Malattia C, Martini A, Toma P. Synovial and inflammatory diseases in childhood: role of new imaging modalities in the assessment of patients with juvenile idiopathic arthritis. Pediatr Radiol. 2010;40(6):985–98.
Kaeley GS. Review of the use of ultrasound for the diagnosis and monitoring of enthesitis in psoriatic arthritis. Curr Rheumatol Rep. 2011;13(4):338–45.
Kannus P. Structure of the tendon connective tissue. Scand J Med Sci Sports. 2000;10(6):312–20. Review.
Jozsa L, Balint BJ. The architecture of human tendons and so-called surface phenomenon. Traumatologia. 1978;21:293–7.
Williams JGP. Achilles tendon lesions insport. Sports Med. 1986;3:114–35.
• Jelsing EJ, Finnoff J, Levy B, Smith J. The prevalence of fluid associated with the Iliotibial band in asymptomatic recreational runners: an ultrasonographic study. PM R. 2013;5(7):563–7. Interesting approach showing the variability of ultrasound findings in different scan positions.
Gutierrez M, Filippucci E, Grassi W, Rosemffet M. Intratendinous power Doppler changes related to patient position in seronegative spondyloarthritis. J Rheumatol. 2010;37:1057–9.
Jousse-Joulin S, Cangemi C, Gerard S, Gestin S, Bressollette L, de Parscau L, et al. Normal sonoanatomy of the paediatric entheses including echostructure and vascularisation changes during growth. Eur Radiol. 2015;25(7):2143–52.
Jousse-Joulin S, Breton S, Cangemi C, Fenoll B, Bressolette L, de Parscau L, et al. Ultrasonography for detecting enthesitis in juvenile idiopathic arthritis. Arthritis Care Res. 2011;63(6):849–55.
• Roth J, diGeso L. Power and Colour Doppler Findings in lower extremity entheses of healthy children—effect of measurement distance from insertion and joint position. Arthritis Rheumatol. 2014; 66(S45). A differential pattern of ultrasound signals at various entheses in healthy children is shown.
• Chauvin NA, Ho-Fung V, Jaramillo D, Edgar JC, Weiss PF. Ultrasound of the joints and entheses in healthy children. Pediatr Radiol. 2015;45(9):1344–54. Detailed description of the Doppler signals in various locations in relation to the tendon and enthesis.
Grechenig W, Mayr JM, Peicha G, Hammerl R, Schatz B, Grechenig S. Sonoanatomy of the Achilles tendon insertion in children. J Clin Ultrasound. 2004;32(7):338–43.
Doria S, Roth J, Babyn P. Imaging in pediatric rheumatic diseases. In: Petty R, Laxer R, Lindsley CB, Wedderburn L, editors. Textbook of pediatric rheumatology, 7th edition. Saunders; 2015.
Ogden JA, Hempton RF, Southwick WO. Development of the tibial tuberosity. Anat Rec. 1974;182:431–46.
McCarthy SM, Ogden JA. Radiology of postnatal skeletal development. V. Distal humerus. Skeletal Radiol. 1982;7(4):239–49.
Ogden JA. Radiology of postnatal skeletal development. X. Patella and tibial tuberosity. Skeletal Radiol. 1984;11(4):246–57N.
Ogden JA, Southwick WO. Osgood-Schlatter’s disease and tibial tuberosity development. Clin Orthop Relat Res. 1976;116:180–9.
Wakefield RJ, Balint P, Szkudlarek M, Filippucci E, Backhaus M, Scheel AK, et al. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol. 2005;32:2485–7.
Balint PV, Kane D, Wilson H, McInnes IB, Sturrock RD. Ultrasonography of entheseal insertions in the lower limb in spondyloarthropathy. Ann Rheum Dis. 2002;61:905–10.
Naredo E, Batle-Gualda E, Garcìa-Vivar ML, Garcìa-Aparicio AM, Fernandez-Sueiro JL, Fernandez-Prada M, et al. Power Doppler ultrasonographic assessment of entheses in spondyloarthropathies: response to therapy of entheseal abnormalities. J Rheumatol. 2010;37:2110–7.
Grassi W, Gutierrez M, Filippucci E. The sound of enthesis. J Rheumatol. 2010;37(10):1986–8.
De Miguel E, Cobo T, Muñoz-Fernández S, Naredo E, Usón J, Acebes JC, et al. Validity of enthesis ultrasound assessment in spondylarthropathy. Ann Rheum Dis. 2009;68:169–74.
D’Agostino MA, Said-Nahal R, Hacquard-Bouder C, et al. Assessment of peripheral enthesitis in the spondyloarthropathies by ultrasonography combined with power Doppler: a cross-sectional study. Arthritis Rheum. 2003;48:523–33.
Tse SM, Laxer R, Babyn P, et al. Radiologic improvement of juvenile idiopathic: arthritis-enthesitis-related arthritis following anti-tumor necrosis factor-alpha blockade with etanercept. J Rheumatol. 2006;33:1186–8.
Laurell L, Court-Payen M, Nielsen S, Zak M, Thomsen C, Miguel-Pérez M, et al. Ultrasonography and color Doppler of proximal gluteal enthesitis in juvenile idiopathic arthritis: a descriptive study. Pediatr Rheumatol Online J. 2011;9(1):22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Pamela F. Weiss, Nancy A. Chauvin, and Johannes Roth declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Spondyloarthritis
Rights and permissions
About this article
Cite this article
Weiss, P.F., Chauvin, N.A. & Roth, J. Imaging in Juvenile Spondyloarthritis. Curr Rheumatol Rep 18, 75 (2016). https://doi.org/10.1007/s11926-016-0624-6
Published:
DOI: https://doi.org/10.1007/s11926-016-0624-6