Abstract
The pathogenesis of systemic sclerosis is still unknown, although immune cells, mainly macrophages/monocytes, may have an important role in initiating and/or perpetuating the disease. Macrophages and monocytes are often classified as pro-inflammatory M1 phenotype or classic activation and pro-fibrotic/anti-inflammatory M2 phenotype or alternative activation. In this review, we highlighted the most relevant research regarding the involvement of macrophages/monocytes in the pathogenesis of this complex disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a chronic autoimmune disease of unknown etiology characterized by inflammation, vascular injury, and fibrosis. The triggers that initiate and/or perpetuate this complex phenotype remain uncertain. One of the hypotheses is that some of the pro-fibrotic and/or pro-inflammatory factors known to have an important role in the pathogenesis of the disease might be released or be activated by immune cells, mainly monocyte/macrophages. In this review, we will discuss the most recent data regarding the involvement of monocyte/macrophages in the development and in the progression of the SSc disease.
Overview of the M1-M2 Concept: Background and New Paradigms
Macrophages are key regulator and effector cells that based on their activation status can influence a response cascade of the immune system. The classic M1 activated macrophage was originally described in combination of two signals, interferon-gamma (IFNg) and tumor-necrosis factor (TNF), resulting in a macrophage population with strong microbicidal or tumoricidal capacity that secretes high levels of pro-inflammatory cytokines and mediators [1]. On the other extreme are the M2 macrophages or alternatively activated macrophages, firstly described in extracellular parasitic infections with increased interleukin-4 (IL4), a Th2 environment [2].
Nowadays, in a genomic era and with better knowledge of cytokine signaling, we have a much more complex picture regarding monocyte/macrophage activation. Although the purpose of this review is not to describe in detail the M1 and M2 paradigm, it is important to highlight signaling pathways and gene expression singularities between M1 and M2 stimuli. As described below, numerous signals can influence macrophage physiology with the main purpose to preserve homeostasis; however, each of these activations might have dangerous consequences if not appropriately regulated. For example, M1 macrophages can ultimately cause intensive inflammation and tissue damage, or even predispose to neoplastic transformation. On the other hand, M2 macrophages normally involved in wound healing can induce fibrosis, exacerbate allergic processes, and predispose the host to infection [3].
In the most recent review about the M1 and M2 theory by Martinez and Gordon [4••], the authors grouped these two concepts according to relevant receptors and key signaling mediators. In a simplistic way, M1 stimuli could be divided in three subgroups. First, the classic with IFN-gamma as the main cytokine inducing M1 activation through IFNGR-1 and IFNGR-2 that recruits Janus kinase (JAK) 1 and JAK2 adaptors that activate STAT1 and interferon regulatory factors (IRF). The second subgroup involves pattern recognition receptors through Toll-like receptor (TLR) signaling. Lipopolysaccharide (LPS) is the best-studied M1 macrophage signal and is recognized by TLR4. Conventionally, TLR4 activation leads to a strong pro-inflammatory cytokine profile that is controlled by NF-kB, activator protein 1 (AP-1), IRFs, STAT1, and early growth response (EGR). The third group is related to granulocyte macrophage colony-stimulating factor (GM-CSF), which recruits JAK2 to activate STAT5, extracellular signal-regulated kinase (ERK), AKT, NK-kB, and IRF5.
On the other hand, the M2 group is considered even more complex with five subgroups [4••]. An IL-4 stimulus is one of the initial M2 groups of ligands. It interacts with IL-4Ra1 activating JAK1 and JAK3 leading to STAT6 activation. IL-13 signaling is similar to IL-4, although not totally overlapping. The second M2 subgroup involves Fc gamma receptor family leading to spleen tyrosine kinase (Syk) and phosphoinositide 3-kinase (PI3K) activation. The third group includes glucocorticoids stimuli that bind to the glucocorticoid receptor alpha. This complex interacts with transcription factors affecting adherence, spreading, phagocytosis, and apoptosis of monocytes. An IL-10 stimulus is the fourth subgroup of M2 ligands. It binds to the IL-10 receptor leading to activation of STAT3 and inhibiting expression of many pro-inflammatory cytokines. The last subgroup of M2 stimuli is M-CSF that leads to activation of ERK, PI3K, phospholipase C, and SP1 nuclear localization.
It is important to highlight here that the macrophage classification is still a work in progress, as proposed by Guilliams and van de Laar [5], where they suggest a nomenclature system in two levels. First level would be based on a restricted set of names according to their cellular origin that would be applicable across species and across tissues. And a second level would be more flexible depending on the activation state or localization of the cells.
For the purpose of this review, a dichotomized classification based upon M1 and M2 activation will be used to clarify descriptions of the studies. The lists of the most frequently used M1 and M2 macrophage markers and/or cytokines/receptors involved in their activation are provided with citations, below [1, 4••, 6]. The list is not comprehensive nor does include all the currently aspects of the M1-M2 paradigm.
M1 macrophage markers include inducible nitric-oxide synthase (iNOS), suppressor of cytokine signaling (SOCS1), CD64, CD86, TLR2, TLR4, CCR7, interleukin 12 (IL-12), IL-6, CXCL9, CXCL10, and CXCL11.
M2 macrophage markers include mannose receptor C type 1 (MRC1 or CD206), macrophage scavenger receptor 1 (MSR1 or CD204), C-type lectin receptor DCL-1 (DCL-1), membrane-spanning 4-domains, subfamily A, member 4 (MS4A4A), CCR2, IL-10, CCL22, CCL18, CCL13, and CCL17.
Evidence of Macrophage Involvement in the SSc Human Disease
Blood
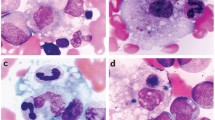
Almost 30 years ago, Andrews and colleagues [7] attempted to better define the level of differentiation and activation of monocytes in the blood of SSc patients. With what nowadays we consider very rudimental tools, enzymatic assays and unspecific cellular markers, the authors were able to show that circulating monocytes are strongly activated in SSc patients. Later on, Hussein et al. [8] showed that mononuclear inflammatory cells (no discriminatory cell markers were used), neutrophils, and eosinophils were significantly higher in the peripheral blood, in the bronchoalveolar lavage (BAL), and in the skin of SSc patients compared to controls. They also observed a higher CD4/CD8 ratios and an increased of TNFa and IL1b in both BAL and blood of these patients. One of the first studies focusing on specific macrophage/monocytes markers involved in the interferon-mediated activation was performed by York et al. [9]. They showed that Siglec-1 (CD169), macrophage marker induced by type I interferon, was increased in circulating SSc monocytes and in the skin macrophages. The authors showed a strong type I interferon signature in SSc patients that was probably through TLR activation with consequently IFN secretion leading to activation of monocyte/macrophages in the blood and skin of SSc patients. Using a more comprehensive panel of markers, Higashi-Kuwata et al. [10•] analyzed simultaneously skin and blood samples from SSc patients in order to explore the monocyte/macrophage population in these organs and their involvement in the pathogenesis of the disease. Fifty-one patients were selected, and the authors observed a higher number of cells positive for CD68 (pan-macrophage marker), CD163, and CD204 in the perivascular regions and also between thickened collagen bundles in the SSc skin compared to controls. CD163 and CD204 are well-accepted markers for activated M2 macrophage [11]. When analyzing the blood, they observed that peripheral blood mononuclear cells (PBMCs) from SSc patients had a significantly greater population of CD14+ cells compared to healthy donors. Interestingly, there was no difference in this population between limited and diffuse SSc subtypes. They further analyzed the CD14+ population revealing that CD14+CD163+ cells were also in higher numbers in PBMCs from SSc patients and the CD163+ cells belonged to the CD204+ population, which the authors suggested that could be the source of the CD163+ and CD204+ macrophages found in the SSc skin [10•]. Multiple reports have described CD163+ being increased in the serum of SSc patients with high levels correlating with the disease severity [12–15].
In a different approach, using gene expression analysis of single cell types, Duan et al. [16] were able to demonstrate a pattern of upregulated genes in both monocytes and CD4 lymphocytes populations in the blood of SSc patients. In more detail, the authors analyzed the blood of diffuse and limited SSc patients using a positive selection technique for CD14+ and CD4+ cell types. The gene expression signature of both cell types was enough to distinguish patients from controls. They confirmed the IFN-alpha signature in SSc blood cells in the absence of this cytokine in the plasma, suggesting that monocytes and CD4 lymphocytes respond locally to this cytokine in the vessels. Interestingly, these signatures were similar in both SSc subtypes.
Mathai et al. [17] had a similar hypothesis that monocytes from the blood of patients with SSc-interstitial lung disease (ILD) would also show pro-fibrotic, M2 features. They observed that CD14+ monocytes in SSc-ILD express higher levels of CD163 compared to controls. More importantly, LPS stimulation of these cells increased CD163 expression only in SSc-ILD CD14+ cells compared to controls. In order to address functional differences in these monocytes, CCL18 levels in CD14+-cultured cells were measured showing a substantial increase in both baseline and LPS-stimulated cells compared to controls. Taken together, they revealed a distinct pro-fibrotic phenotype of circulating monocytes in SSc-ILD that might be involved in the pathogenesis of lung fibrosis in SSc disease.
PBMCs of SSc patients have also been extensively analyzed for gene signatures and cytokine profiles in order to better understand the pathogenesis and also used for the development of biomarkers for severe complications, such as pulmonary arterial hypertension (PAH). One of the first studies using microarray gene expression profiling of PBMCs from SSc-PAH and idiopathic PAH and controls was performed by Grigoryev et al. in 2008 [18]. The authors indicated that differential gene expression is detectable in PBMCs from SSc-PAH patients and can be related to severity. More importantly, they observed a strong association of angiogenesis and chemotaxis/inflammation, including CCL3 and CCL4 both chemoattractives for monocytes/macrophages with the severity of PAH in SSc patients. Later on, Pendergrass et al. [19] in a larger group of SSc-PAH patients confirmed the strong expression of vascular markers and again a clear monocyte signature in the blood of SSc-PAH patients. Our group validated the presence of this unique monocyte signature in PBMCs of SSc-PAH patients, and most importantly, we observed that relevant monocyte/macrophage-related genes such as CCR1 and JAK2 were strongly expressed mainly in CD14+ cells of these patients compared to controls [20]. One of the M2 markers, MRC1 (CD206 or mannose receptor 1) was increased exclusively in SSc-PAH patients and strongly correlated with the pulmonary arterial pressure, by catheterization. MRC1 was greatly increased after IL-13 stimulation and with much higher expression in CD14+ cells. We also showed a higher IL-13 concentration in the plasma of SSc-PAH patients, suggesting that the M2 markers found in this severe group of patients might be a reflection of a strong Th2 environment in the blood [20].
Skin
The recruitment of immune cells, including macrophages to the peripheral tissues, depends mostly on chemokine gradients. Skin from SSc patients do have a well-described immune cell infiltration mainly consisted by T cells and macrophages; therefore, a strong expression of chemokines would be highly expected. Following this hypothesis, Mathes et al. performed a very comprehensive analysis of chemokine and chemokine receptor expression in the SSc skin [21•]. They confirmed the upregulation of several chemokines such as CCL2, CCL5, and CXCL9 described before [22–25]. More interestingly, they showed an upregulation of CCL18, CCL19, and CXCL13 in the skin of SSc patients. The source of CCL19 appeared to be from CD163+ macrophages, and its expression was strongly correlated with macrophage markers in the skin, suggesting that this chemokine might have a strong impact in activating skin resident macrophages that eventually will secrete more CCL19 perpetuating this activated loop. CCL19 was also strongly correlated with vascular markers that might suggest a role in the recruitment of macrophages in the SSc skin [21•].
CCL2 has been long recognized as a key player in the SSc pathogenesis being shown to be upregulated in the skin [22, 23, 26, 27] of SSc patients and strongly correlated with the modified Rodnan skin score (MRSS) [28, 29], a clinical skin fibrotic score [30]. Serum levels of CCL2 are also higher in SSc patients as shown by several groups; more importantly, serum CCL2 was correlated with the MRSS strongly suggesting that CCL2, and consequently the macrophage recruitment, might be involved in the pathogenesis of the skin fibrosis [27, 28, 31–34]. Another important piece of evidence is that the involvement of CCL2 might not be restricted only to the skin. As was nicely shown by Assassi et al., skin gene expression and plasma levels of CCL2 were strongly correlated with the severity of lung fibrosis in SSc patients [35].
In terms of biomarker development, Stifano et al. [36] observed an overexpression of TLR4 and its co-receptors, CD14 and MD2, in the skin of diffuse SSc patients. Most importantly, CD14 correlated with progressive skin disease assessed by the change in MRSS 6 months after the skin biopsy. It was considered the first prognostic biomarker identified in SSc skin disease. CD14 is mainly expressed by macrophages, although it can also be found in lower levels in neutrophils and dendritic cells, and more recently, CD14 has been recognized to be expressed by many non-myeloid cells including endothelial, epithelial cells, and fibroblasts [37]. Additional evidence of the macrophage involvement in SSc skin disease progression was observed by Rice et al. using a novel skin biomarker [38]. The main goal of the study was the development of a pharmacodynamic biomarker based on skin gene expression, but it revealed in two separate models that macrophage markers such as MS4A4A, CD163, and CCL2 are strongly correlated with the MRSS and can be used to monitor skin disease activity longitudinally.
In order to identify the consensus genes present in three independent cohorts of SSc skin biopsies, Mahoney et al. [39] developed a computational tool that was able to perform a meta-analysis of these genome-wide gene expression datasets. In a simplistic way, the authors created a gene-gene interaction network of conserved molecular features across the intrinsic subsets (inflammatory, fibroproliferative, normal-like, and limited) and analyzed their connections with SSc-associated genetic polymorphisms. The network shows five main components interconnected with the first subnetwork related to interferon activation, a second network containing genes characteristic of M2 macrophage activation, and a third molecular subnetwork containing genes involved in adaptive immunity. The fourth molecular subnetwork contained TGFb pathway and extra cellular (ECM) structural proteins, and the fifth molecular subnetwork was related to cell cycle/cell proliferation [39].
Lung
Interstitial lung disease (SSc-ILD) is one of the leading causes of mortality in patients with SSc. Lung tissue from SSc-ILD patients is not frequently available, and currently, biopsies come mostly from lung transplantation patients. In a very elegant study, Hsu et al. [40] showed using microarray analysis of lung tissue from patients with idiopathic pulmonary fibrosis (IPF), SSc-ILD, pulmonary arterial hypertension (SSc-PAH), and idiopathic PAH (IPAH) that unique molecular signatures are present as disease specific (SSc or IPF) and phenotype specific (ILD or PAH). These molecular signatures provided new insights into the pathogenesis of these two severe complications of SSc; many genes in these signatures are markers of alveolar macrophage activation and of fibrosis [40, 41]. Using a similar microarray analysis, our group examined gene signatures in lung tissue from SSc-ILD patients on whom two prospective clinical parameters were available; therefore, the progression of the lung disease could be measured and correlated with the lung gene expression [42•]. We confirmed Hsu’s data showing a strong fibrotic TGFb signature in SSc-ILD lungs. More importantly, we observed three main lung gene signatures strongly correlated with the progression of the disease, based on clinical parameters. The largest lung gene signature strongly related to progressive lung disease was the macrophage emigration and activation, with CCL18 and CD163 expression also confirmed at the protein level. The fibrotic TGFb and the interferon signatures were also correlated with progressive SSc-ILD [43]. Taken together, these studies revealed molecular signatures in SSc-ILD lung tissue, highlighted the major pathogenic pathways involved in the pathogenesis and/or progression of lung fibrosis, and indicated that macrophages are key players.
As a surrogate for lung tissue, alveolar macrophages (AM) have also been extensively studied in BAL from lungs of SSc patients. The indication and the interpretation of this analysis are not the focus of this review, but some of the functional studies of these cells are relevant and should be mentioned. White et al. [44] compared the gene expression profiles of BAL cells from SSc patients with lung inflammation and patients without inflammation with the hypothesis that this could reflect the cellular activation involved in the development of lung fibrosis in SSc. Using DNA array technology, the authors showed striking differences in gene expression of BAL cells from SSc patients with inflammation. Of particular interest was the increase in expression of CCL18 (PARC) and CXCR4 genes. CCL18 is a monocyte (M2)-derived chemokine that induces T cell migration and collagen production by fibroblasts [45]. The authors were also able to show an increase of CCL18 levels in BAL fluids from SSc patients with lung inflammation, along with another important macrophage chemoattractive chemokine CCL2. High levels of CCL18 in SSc patients, mainly related to pulmonary fibrosis, were later on confirmed by several groups, and it has been proposed for use as a biomarker for pulmonary fibrotic activity in idiopathic interstitial pneumonia and SSc-ILD [46–48].
Another very interesting study led by Hamilton et al. [49] showed that AM from SSc-ILD patients responded more strongly to LPS stimulation than controls, in agreement with Mathai’s data showing an intense response of circulating SSc-ILD monocytes after stimulation with LPS [17]. In addition, markers of AM activation were significantly elevated in SSc BAL samples compared to normal BAL. These phenotypical changes in SSc AM were observed only in normal AM stimulated with IL-4, but not after stimulation with INFg, IL-3, IL-10, nor IL-12. The authors suggested that a more Th2 environment might be responsible for the activation of AM in SSc-ILD patients [49]. See Table 1 for a summary of the references regarding markers.
Conclusions
More than thirty years of research have revealed strong evidence that macrophages/monocytes are involved in the pathogenesis of SSc, but their precise role in the disease is still unclear. Furthermore, we have not yet identified which specific subset of macrophages is implicated in the development and/or in the progression of this lethal chronic disease. The presence of both M1 and strong M2 signatures observed in the skin, blood, and lungs of SSc patients is very clear. Our main challenge for future research is to better define the mechanisms and how relevant these cells are in perpetuating the fibrotic loop. In order to solve this puzzle, we need better tools both in animal models and in humans that will characterize at the cellular level the contribution of specific monocyte/macrophage in the development of the disease. Currently, characterization of macrophages is an area of intense research that with novel genetic tools will allow us to define specific subsets that could potentially be targets for drug development.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8(12):958–69.
Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3(1):23–35.
Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol. 2011;11(11):723–37.
Martinez FO, Gordon S. The M1 and M2 paradigm of macrophage activation: time for reassessment. F1000Prime Rep. 2014;6:13. The authors reassessed the current macrophage activation classification stratifying M1 and M2 in several subsets based on downstream signaling.
Guilliams M, van de Laar L. A Hitchhiker’s guide to myeloid cell subsets: practical implementation of a novel mononuclear phagocyte classification system. Front Immunol. 2015;6:406.
Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25(12):677–86.
Andrews BS, Friou GJ, Berman MA, Sandborg CI, Mirick GR, Cesario TC. Changes in circulating monocytes in patients with progressive systemic sclerosis. J Rheumatol. 1987;14(5):930–5.
Hussein MR, Hassan HI, Hofny ER, Elkholy M, Fatehy NA, Abd Elmoniem AE, et al. Alterations of mononuclear inflammatory cells, CD4/CD8+ T cells, interleukin 1beta, and tumour necrosis factor alpha in the bronchoalveolar lavage fluid, peripheral blood, and skin of patients with systemic sclerosis. J Clin Pathol. 2005;58(2):178–84.
York MR, Nagai T, Mangini AJ, Lemaire R, van Seventer JM, Lafyatis R. A macrophage marker, Siglec-1, is increased on circulating monocytes in patients with systemic sclerosis and induced by type I interferons and toll-like receptor agonists. Arthritis Rheum. 2007;56(3):1010–20.
Higashi-Kuwata N, Jinnin M, Makino T, Fukushima S, Inoue Y, Muchemwa FC, et al. Characterization of monocyte/macrophage subsets in the skin and peripheral blood derived from patients with systemic sclerosis. Arthritis Res Ther. 2010;12(4):R128. Skin and blood analysis of macrophage markers in SSc compared to controls. It showed an increased of CD163 + CD204+ population in both tissues.
Martinez FO, Gordon S, Locati M, Mantovani A. Transcriptional profiling of the human monocyte-to-macrophage differentiation and polarization: new molecules and patterns of gene expression. J Immunol. 2006;177(10):7303–11.
Bielecki M, Kowal K, Lapinska A, Chyczewski L, Kowal-Bielecka O. Increased release of soluble CD163 by the peripheral blood mononuclear cells is associated with worse prognosis in patients with systemic sclerosis. Adv Med Sci. 2013;58(1):126–33.
Nakayama W, Jinnin M, Makino K, Kajihara I, Makino T, Fukushima S, et al. Serum levels of soluble CD163 in patients with systemic sclerosis. Rheumatol Int. 2012;32(2):403–7.
Shimizu K, Ogawa F, Yoshizaki A, Akiyama Y, Kuwatsuka Y, Okazaki S, et al. Increased serum levels of soluble CD163 in patients with scleroderma. Clin Rheumatol. 2012;31(7):1059–64.
Kowal-Bielecka O, Bielecki M, Guiducci S, Trzcinska-Butkiewicz B, Michalska-Jakubus M, Matucci-Cerinic M, et al. High serum sCD163/sTWEAK ratio is associated with lower risk of digital ulcers but more severe skin disease in patients with systemic sclerosis. Arthritis Res Ther. 2013;15(3):R69.
Duan H, Fleming J, Pritchard DK, Amon LM, Xue J, Arnett HA, et al. Combined analysis of monocyte and lymphocyte messenger RNA expression with serum protein profiles in patients with scleroderma. Arthritis Rheum. 2008;58(5):1465–74.
Mathai SK, Gulati M, Peng X, Russell TR, Shaw AC, Rubinowitz AN, et al. Circulating monocytes from systemic sclerosis patients with interstitial lung disease show an enhanced profibrotic phenotype. Lab Invest. 2010;90(6):812–23.
Grigoryev DN, Mathai SC, Fisher MR, Girgis RE, Zaiman AL, Housten-Harris T, et al. Identification of candidate genes in scleroderma-related pulmonary arterial hypertension. Transl Res. 2008;151(4):197–207.
Pendergrass SA, Hayes E, Farina G, Lemaire R, Farber HW, Whitfield ML, et al. Limited systemic sclerosis patients with pulmonary arterial hypertension show biomarkers of inflammation and vascular injury. PLoS One. 2010;5(8):e12106.
Christmann RB, Hayes E, Pendergrass S, Padilla C, Farina G, Affandi AJ, et al. Interferon and alternative activation of monocyte/macrophages in systemic sclerosis-associated pulmonary arterial hypertension. Arthritis Rheum. 2011;63(6):1718–28.
Mathes AL, Christmann RB, Stifano G, Affandi AJ, Radstake TR, Farina GA, et al. Global chemokine expression in systemic sclerosis (SSc): CCL19 expression correlates with vascular inflammation in SSc skin. Ann Rheum Dis. 2014;73(10):1864–72. Human study analyzing a broad panel of chemokine expression in the skin of normal and SSc patients. It demonstrated a strong correlation between CD163+ macrophages and perivascular inflammation.
Distler O, Pap T, Kowal-Bielecka O, Meyringer R, Guiducci S, Landthaler M, et al. Overexpression of monocyte chemoattractant protein 1 in systemic sclerosis: role of platelet-derived growth factor and effects on monocyte chemotaxis and collagen synthesis. Arthritis Rheum. 2001;44(11):2665–78.
Yamamoto T, Eckes B, Hartmann K, Krieg T. Expression of monocyte chemoattractant protein-1 in the lesional skin of systemic sclerosis. J Dermatol Sci. 2001;26(2):133–9.
Ong VH, Evans LA, Shiwen X, Fisher IB, Rajkumar V, Abraham DJ, et al. Monocyte chemoattractant protein 3 as a mediator of fibrosis: overexpression in systemic sclerosis and the type 1 tight-skin mouse. Arthritis Rheum. 2003;48(7):1979–91.
Distler O, Rinkes B, Hohenleutner U, Scholmerich J, Landthaler M, Lang B, et al. Expression of RANTES in biopsies of skin and upper gastrointestinal tract from patients with systemic sclerosis. Rheumatol Int. 1999;19(1–2):39–46.
Galindo M, Santiago B, Rivero M, Rullas J, Alcami J, Pablos JL. Chemokine expression by systemic sclerosis fibroblasts: abnormal regulation of monocyte chemoattractant protein 1 expression. Arthritis Rheum. 2001;44(6):1382–6.
Hasegawa M, Sato S, Takehara K. Augmented production of chemokines (monocyte chemotactic protein-1 (MCP-1), macrophage inflammatory protein-1alpha (MIP-1alpha) and MIP-1beta) in patients with systemic sclerosis: MCP-1 and MIP-1alpha may be involved in the development of pulmonary fibrosis. Clin Exp Immunol. 1999;117(1):159–65.
Bandinelli F, Del Rosso A, Gabrielli A, Giacomelli R, Bartoli F, Guiducci S, et al. CCL2, CCL3 and CCL5 chemokines in systemic sclerosis: the correlation with SSc clinical features and the effect of prostaglandin E1 treatment. Clin Exp Rheumatol. 2012;30(2 Suppl 71):S44–9.
Greenblatt MB, Sargent JL, Farina G, Tsang K, Lafyatis R, Glimcher LH, et al. Interspecies comparison of human and murine scleroderma reveals IL-13 and CCL2 as disease subset-specific targets. Am J Pathol. 2012;180(3):1080–94.
Clements PJ, Lachenbruch PA, Seibold JR, Zee B, Steen VD, Brennan P, et al. Skin thickness score in systemic sclerosis: an assessment of interobserver variability in 3 independent studies. J Rheumatol. 1993;20(11):1892–6.
Peterlana D, Puccetti A, Caramaschi P, Biasi D, Beri R, Simeoni S, et al. Endothelin-1 serum levels correlate with MCP-1 but not with homocysteine plasma concentration in patients with systemic sclerosis. Scand J Rheumatol. 2006;35(2):133–7.
Antonelli A, Ferri C, Fallahi P, Ferrari SM, Giuggioli D, Colaci M, et al. CXCL10 (alpha) and CCL2 (beta) chemokines in systemic sclerosis--a longitudinal study. Rheumatology (Oxford). 2008;47(1):45–9.
Carulli MT, Handler C, Coghlan JG, Black CM, Denton CP. Can CCL2 serum levels be used in risk stratification or to monitor treatment response in systemic sclerosis? Ann Rheum Dis. 2008;67(1):105–9.
Scala E, Pallotta S, Frezzolini A, Abeni D, Barbieri C, Sampogna F, et al. Cytokine and chemokine levels in systemic sclerosis: relationship with cutaneous and internal organ involvement. Clin Exp Immunol. 2004;138(3):540–6.
Assassi S, Wu M, Tan FK, Chang J, Graham TA, Furst DE, et al. Skin gene expression correlates of severity of interstitial lung disease in systemic sclerosis. Arthritis Rheum. 2013;65(11):2917–27.
Stifano G, Affandi AJ, Mathes AL, Rice LM, Nakerakanti S, Nazari B, et al. Chronic Toll-like receptor 4 stimulation in skin induces inflammation, macrophage activation, transforming growth factor beta signature gene expression, and fibrosis. Arthritis Res Ther. 2014;16(4):R136.
Jersmann HP. Time to abandon dogma: CD14 is expressed by non-myeloid lineage cells. Immunol Cell Biol. 2005;83(5):462–7.
Rice LM, Ziemek J, Stratton EA, McLaughlin SR, Padilla CM, Mathes AL, et al. A longitudinal biomarker for the extent of skin disease in patients with diffuse cutaneous systemic sclerosis. Arthritis Rheumatol. 2015;67:3004–15.
Mahoney JM, Taroni J, Martyanov V, Wood TA, Greene CS, Pioli PA, et al. Systems level analysis of systemic sclerosis shows a network of immune and profibrotic pathways connected with genetic polymorphisms. PLoS Comput Biol. 2015;11(1):e1004005.
Hsu E, Shi H, Jordan RM, Lyons-Weiler J, Pilewski JM, Feghali-Bostwick CA. Lung tissues in patients with systemic sclerosis have gene expression patterns unique to pulmonary fibrosis and pulmonary hypertension. Arthritis Rheum. 2011;63(3):783–94.
Silver RM, Feghali-Bostwick CA. Editorial: molecular insights into systemic sclerosis-associated interstitial lung disease. Arthritis Rheumatol. 2014;66(3):485–7.
Christmann RB, Sampaio-Barros P, Stifano G, Borges CL, de Carvalho CR, Kairalla R, et al. Association of Interferon- and transforming growth factor beta-regulated genes and macrophage activation with systemic sclerosis-related progressive lung fibrosis. Arthritis Rheumatol. 2014;66(3):714–25. Microarray analysis of human lung biopsies from SSc-ILD patients compared to controls. It identified a correlation between progressive lung disease with three main molecular signaling: macrophage activation, interferon and fibrotic-TGF-beta signatures.
Farina G, Lafyatis D, Lemaire R, Lafyatis R. A four-gene biomarker predicts skin disease in patients with diffuse cutaneous systemic sclerosis. Arthritis Rheum. 2010;62(2):580–8.
Luzina IG, Atamas SP, Wise R, Wigley FM, Xiao HQ, White B. Gene expression in bronchoalveolar lavage cells from scleroderma patients. Am J Respir Cell Mol Biol. 2002;26(5):549–57.
Hieshima K, Imai T, Baba M, Shoudai K, Ishizuka K, Nakagawa T, et al. A novel human CC chemokine PARC that is most homologous to macrophage-inflammatory protein-1 alpha/LD78 alpha and chemotactic for T lymphocytes, but not for monocytes. J Immunol. 1997;159(3):1140–9.
Prasse A, Pechkovsky DV, Toews GB, Schafer M, Eggeling S, Ludwig C, et al. CCL18 as an indicator of pulmonary fibrotic activity in idiopathic interstitial pneumonias and systemic sclerosis. Arthritis Rheum. 2007;56(5):1685–93.
Schupp J, Becker M, Gunther J, Muller-Quernheim J, Riemekasten G, Prasse A. Serum CCL18 is predictive for lung disease progression and mortality in systemic sclerosis. Eur Respir J. 2014;43(5):1530–2.
Tiev KP, Hua-Huy T, Kettaneh A, Gain M, Duong-Quy S, Toledano C, et al. Serum CC chemokine ligand-18 predicts lung disease worsening in systemic sclerosis. Eur Respir J. 2011;38(6):1355–60.
Hamilton Jr RF, Parsley E, Holian A. Alveolar macrophages from systemic sclerosis patients: evidence for IL-4-mediated phenotype changes. Am J Physiol Lung Cell Mol Physiol. 2004;286(6):L1202–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Scleroderma
Rights and permissions
About this article
Cite this article
Stifano, G., Christmann, R.B. Macrophage Involvement in Systemic Sclerosis: Do We Need More Evidence?. Curr Rheumatol Rep 18, 2 (2016). https://doi.org/10.1007/s11926-015-0554-8
Published:
DOI: https://doi.org/10.1007/s11926-015-0554-8