Abstract
Sleep disturbance is a common clinical problem experienced by patients with a wide range of psychiatric disorders. Accumulating evidence has demonstrated that insomnia is a comorbid process that affects the course and treatment of a number of forms of mental illness. The efficacy and safety of sedative-hypnotic medications have largely been established in patients who do not have comorbid psychiatric disorders, underscoring the need for further research in this sphere. This review summarizes pertinent findings in the recent literature that have examined the role of hypnotic medication in the treatment of psychiatric illness, and highlights potential areas that may prove fruitful avenues of future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disturbance is extremely common among persons with psychiatric disorders. Insomnia, defined as difficulty initiating or maintaining sleep despite adequate opportunity that is associated with significant distress or impairment, is a diagnostic feature of mood and anxiety disorders, and is also frequently experienced by persons with several other forms of psychiatric illness [1]. Insomnia shares a particularly strong bidirectional relationship with mood disorders, as it has been associated with increased risk of incident depression and poorer treatment outcomes, as well as increased suicidal ideation, suicide attempts, and completed suicide [2]. These relationships have led to development of current nosological perspectives that consider sleep difficulties as comorbid with, rather than secondary to, psychiatric disorders [1, 3].
Despite these evolving views on sleep disturbance and psychiatric disorders, there are several important questions that remain unanswered, particularly in regard to the use of sedative-hypnotic medications. First, what evidence supports the use of specific medications in the treatment of insomnia comorbid with psychiatric disorders? Second, does pharmacologic treatment of insomnia impact psychiatric symptoms beyond specific effects on sleep disturbance? Third, how do sedative-hypnotic medications alter the longitudinal course of major mental illnesses? And finally, might agents designed to improve sleep continuity have separate effects on other spheres of neurocognitive functioning, particularly those that have been demonstrated to be altered by sleep?
In this review, we will highlight the recent salient literature that examines these vital areas of inquiry. We will focus our summary predominantly on medications that were initially developed and/or marketed for the purpose of treating insomnia, with inclusion of other agents used off-label to treat sleep disturbance where pertinent. We readily acknowledge the efficacy of non-pharmacologic methods for the treatment of insomnia [4]; however, this review will specifically focus medications and not other cognitive-behavioral approaches. Moreover, because several reviews have detailed the effects and efficacy of the melatonergic antidepressant agomelatine [5–7], this medication is considered beyond the scope of this review. In keeping with the Current Reports format, we will focus primarily on recent developments in the literature, and specifically overview the use of sedative-hypnotic medications in unipolar major depressive disorder, bipolar disorder, schizophrenia, and post-traumatic stress disorder (PTSD). Our goal is to provide a succinct, yet critical assessment of the recent literature on this topic, as well as underscore areas of future research required to advance the field.
Major Depressive Disorder
Insomnia is very common in major depressive disorder (MDD), with up to 90 % of patients experiencing difficulty initiating or maintaining sleep during a mood episode [8]. Since their inception nearly three decades ago, specific serotonin reuptake inhibitors (SSRIs) have become the mainstay of treatment for unipolar depression. As a class, SSRIs tend not to have significant antihistaminergic or anticholinergic effects and thus tend to be less sedating than older tricyclic antidepressant (TCA) medications. In this context, a research design in which patients experiencing a major depressive episode with comorbid insomnia are co-administered an open-label SSRI with a blinded sedative-hypnotic versus placebo has become a useful paradigm to study the effects of sedative hypnotics on both sleep and psychiatric symptoms within the standard of care. Using this study design, Fava et al. [9] previously reported that eszopiclone 3 mg nightly co-administered with fluoxetine in patients with MDD and insomnia not only significantly improved sleep-related symptoms, but also significantly improved depressive symptoms beyond its soporific effects [measured by improvement on the 17-item Hamilton Rating Scale for Depression (HDRS-17) with sleep items omitted]. Building on this work, Fava and colleagues [10•] more recently conducted a post hoc analysis that combined data from this prior study with another randomized placebo-controlled study of patients with generalized anxiety disorder treated with escitalopram and concurrent eszopicone 3 mg nightly versus placebo [11]. For this study, anxious depression was defined as an HDRS-17 score ≥14 (excluding insomnia items) and an anxiety/somatization factor score (derived from six sub-items on the HDRS-17) ≥7 [10•]. Pooled analyses demonstrated eszopiclone co-administration significantly improved insomnia symptoms [assessed by the change mean change from baseline on the Insomnia Severity Index (ISI)] [10•]. Moreover, after 8 weeks of co-therapy with eszopiclone, HDRS-17 scores decreased from baseline, regardless of whether insomnia items were excluded; however, this effect was not observed when specifically examining anxiety/somatization [10•].
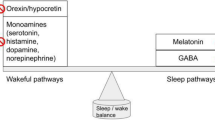
Another recent study examined an open-label SSRI (escitalopram) with co-administration of zolpidem extended-release (ER) 12.5 mg versus placebo in patients with MDD and comorbid insomnia [12•]. Zolpidem ER increased self-reported sleep duration and continuity, as well as next day functioning, but did not augment the antidepressant response of escitalopram assessed by the change in HDRS-17 [12•]. Despite the divergent antidepressant effects observed in zolpidem ER compared to eszopiclone [9, 10•, 12•], there is not currently sufficient evidence to suggest one agent is superior to the other in the treatment of insomnia with comorbid depression, as this would require a direct comparison. However, it does raise important questions regarding how different pharmacologic properties of these agents might lead to particular effects on co-occurring depressive symptoms. In general, although both agents are considered to be non-benzodiazepine benzodiazepine receptor agonists (BZRAs), they do have different affinities for the GABA-A receptor, with zolpidem being highly selective for α1 subtype, while eszopiclone additionally has considerable activity at GABA receptors containing α3 and α5 subunits [13]. Whether the different effects on comorbid depressive symptoms observed in these studies is due to specific neuropharmacologic properties of the drugs, or some other factor, such as inadvertent unblinding in eszopiclone studies due to very high rates of dysgeusia [which can occur in >25 % of participants [10•]] remains to be explained, but may prove a fruitful area of future research.
Another vital area of investigation is how sedative-hypnotics affect suicidal ideation in patients with comorbid depression and insomnia. A sizeable literature has demonstrated that insomnia is an independent risk factor for suicide, raising the possibility that treatment of insomnia with a sedative-hypnotic might reduce suicidal risk [14]. Because prior studies that have examined co-therapy of sedative-hypnotics with SSRIs have excluded people at significant risk of suicide [9, 12•], there is insufficient evidence to determine whether sedative-hypnotics alter the risk of suicide. This is an important area of investigation because clinicians are often unwilling to prescribe sedative-hypnotics to patients with suicidal ideation, possibly out of concern that the agent may be utilized in overdose attempts. Also, a controlled study to examine effects of sedative-hypnotics on suicidal ideation requires a very thoughtful study design to protect the safety of research participants. To help clarify the potential role of sedative-hypnotics in the management of suicidal ideation, a carefully crafted, multi-site randomized clinical trial of open-label SSRI with zolpidem ER versus placebo in depressed adult outpatients with insomnia and suicidal ideation has been developed and is currently recruiting participants with funding from the National Institutes of Mental Health [15]. We eagerly anticipate the results of this Reducing Suicidal Ideation Through Insomnia Treatment (REST-IT) study, as it is very likely to significantly impact the standard of care in psychiatry.
Beyond BZRAs, there has been little recent empiric evaluation of the impact of off-label sedative-hypnotics in the treatment of insomnia with comorbid depressive symptoms. Wichniak and colleagues [16] in an open-label study examined the effects of trazodone continuous-release (CR) 25–150 mg daily in patients with primary insomnia with and without comorbid depressive symptoms, finding that this agent improves clinical symptoms including increased subjective sleep duration and reduced sleep onset latency. Additionally, during the run-out phase, patients with higher depressive symptoms [assessed using the Beck Depression Inventory (BDI)] tended to have a deterioration of symptoms relative to those without depressive symptoms [16]. One other non-controlled study assessed low-dose doxepin (<25 mg/day) in psychiatric inpatients with insomnia and MDD [17]. This retrospective case series failed to demonstrate significant benefit of doxepin on sleep onset or maintenance in these patients [17]. Clearly, because sedating antidepressants are the some of the most commonly prescribed agents for insomnia [18], further research that clarifies the evidence for use of these agents to treat insomnia in psychiatric illness is needed.
Bipolar Disorder
Sleep disturbance, both insomnia and hypersomnolence, is extremely common in bipolar disorder. Insomnia frequently occurs in all phases of the illness, including manic, depressive, and euthymic periods [19, 20]. A sizeable circumstantial literature has suggested sleep disturbance may induce mood switching, particularly to mania [21]. Adding to this literature, Cretu and colleagues recently examined the role of sleep disturbance in a cohort of 89 recovered patients with bipolar disorder followed for over 1 year [22]. Notably, in this cohort, sleep disturbance [assessed with the Pittsburgh Sleep Quality Index (PSQI)] not only correlated significantly with residual mood symptoms, but also predicted earlier mood episode recurrence, even after covarying for residual mood symptoms [22]. Additionally, these findings highlight the potential importance of the treatment of sleep disturbance in bipolar disorder, which theoretically might provide benefit by reducing the occurrence of mood episodes over the longitudinal course of the disorder. However, links between treatment of insomnia and mood stabilization have been highly speculative, and the evidence base regarding the use of specific sedative-hypnotics in bipolar disorder has been quite limited.
McElroy and colleagues assessed the use of ramelteon 8 mg nightly versus placebo in outpatients with bipolar disorder experiencing mild to moderate manic symptoms and insomnia [23]. During the course of the 8-week study, other medications were continued and left unchanged (except in instances in which a medication required dose reduction for side effect management) [23]. In this study, ramelteon did not demonstrate efficacy greater than placebo on the primary outcome measure (change in insomnia assessed by 65-item Pittsburgh Insomnia Rating Scale), nor did it have differential effects on manic symptoms or global severity of illness [23]. However, it did demonstrate improvement in global rating of depressive symptoms, and no serious adverse events were observed [23]. Although this study represents one of the first attempts to conduct a randomized controlled study for insomnia in bipolar disorder, the small sample size (total N = 21), as well as the fact that patients were hypomanic, may limit the power of the study to detect benefit over placebo, as well as the generalizability of results to the management of comorbid insomnia in other phases of bipolar disorder.
Norris and colleagues further extended research on ramelteon in insomnia comorbid with bipolar disorder, examining a larger number of participants (N = 83), who were euthymic at baseline [24•]. Participants in this double-blind investigation were randomized to either ramelteon 8 mg or placebo, in addition to their regular psychiatric medications, and followed for up to 24 weeks or until they experienced a depressive or manic relapse [24•]. Remarkably, participants receiving ramelteon had significantly and roughly twofold lower odds of mood relapse compared to placebo. Also, participants randomized to placebo who had most recently recovered from a mixed or depressive episode had even higher odds (odds ratio 2.67 and 3.75, respectively) of completing the 24-week study compared to participants in the placebo group [24•]. This improved mood stability occurred despite no significant change in the PSQI (last observation carried forward), although trends towards improvement in the PSQI were observed from 8–20 weeks of treatment [24•]. The authors speculated that participants might not have had significant improvement in the PSQI with ramelteon relative to placebo due to a ceiling effect caused by concordant sedating psychotropic medications prescribed for bipolar disorder [24•]. Other study limitations include a relatively small sample size, as well as a duration of mood stability required for study entry of only 1 week, which is shorter than other clinical trials examining mood stability in bipolar disorder [24•]. Despite these limitations, this study suggests that ramelteon, a melatonin type 1- and 2-receptor agonist, may alter the longitudinal course of bipolar disorder, and clearly further research in this sphere is indicated.
Other than the two aforementioned randomized-controlled studies of ramelteon in bipolar disorder [23, 24•], the remaining evidence base to guide the choice of sedative hypnotic medication in bipolar disorder is largely uncontrolled. Schaffer and colleagues performed a chart review assessing the efficacy and safety of zolpidem (immediate and extended release), eszopiclone, zaleplon, and ramelteon in 361 consecutive patients with bipolar disorder [25]. In general, they noted about half of their of their patients required chronic daily sedative-hypnotics, and that BZRAs had success rates (defined as much or very much improved on the Clinical Global Impression Scale-Bipolar Version) of 36–60 %, with more limited success for ramelteon (15 %). These agents were all generally well tolerated, and chronic sedative-hypnotic users had not experienced unacceptable untoward events [25]. Although these uncontrolled data must be interpreted with caution, they do provide some evidence that these agents may be reasonable choices for the treatment of insomnia associated with bipolar disorder, including chronic use.
Another class of agents, sedating antidepressants, is frequently used to treat insomnia in patients with bipolar disorder; however, the evidence base for these medications is limited, despite their widespread use [18]. Because previous studies have suggested that TCAs and trazodone might increase the risk of mood switching, particularly to the manic phase [26, 27], clarification of the safety and efficacy of these agents in persons with bipolar disorder is an important area of study. In the absence of controlled data, Wichniak and colleagues recently reviewed the literature to identify case reports of sedating antidepressants (trazodone and mirtazapine, as well as agomelatine) inducing manic symptoms [28]. Although the risk of bias in this approach is substantial, they found that trazodone and mirtazapine tended to cause mania in patients with other risk factors for manic switching (e.g., not being on a concomitant mood stabilizer) and tended to occur at antidepressant (i.e., higher) doses than the lower doses typically prescribed off-label for insomnia [28]. Thus, if these agents are used to treat insomnia comorbid with bipolar disorder, it would seem most prudent to utilize these agents only in patients concurrently maintained on a mood-stabilizing medication, and with careful monitoring for increased mood switching. Ideally, further controlled research would shed light on the efficacy and safety of sedating antidepressants in bipolar disorder; however, there are likely economic and ethical reasons that such studies are not likely to be conducted in the near future.
Beyond treating insomnia and potentially altering the longitudinal course of bipolar disorder, the use of sedative-hypnotics may also provide benefit in the management of other negative health behaviors such as smoking, which is 3.5-fold more common among patients with bipolar disorder than the general population [29]. Since insomnia preceding and during attempts to quit smoking have been associated with cessation failure [30, 31], the use of adjunctive sleep-promoting agents in patients attempting to quit smoking, particularly among high-risk patients such as those with major mental illness, is a potentially promising line of investigation. Forrest and colleagues performed a secondary analysis of an RCT that examined varenicline versus placebo in patients with bipolar disorder desirous of quitting smoking, finding the use of concomitant hypnotic agents was associated with a greater likelihood of cessation in these patients [32]. Despite limitations including a small sample size (N = 60), and open-label use of hypnotic use limiting cause and effect inferences, these results suggest future larger controlled studies that include patients with bipolar disorder, as well as other psychiatric disorders associated with increased rates of smoking, such as schizophrenia, are indicated.
Schizophrenia
Schizophrenia is the quintessential psychotic illness, with symptoms that fall into three broad categories: positive, negative, and cognitive; all of which are can negatively impact social and occupational functioning. Cognitive symptoms, which can include poor executive functioning, attentional difficulties, and difficulty with working memory, can be particularly impairing for patients with the disorder [33]. The most consistently identified sleep-related difficulties endured by patients with schizophrenia include difficulties falling and staying asleep [34, 35]. Since insomnia and sleep restriction are associated with cognitive impairment in a number of domains [36, 37], treating sleep initiation and continuity difficulties could theoretically result in improved cognition in these patients.
Following this line of inquiry, Tek and colleagues examined the use of eszopiclone 3 mg nightly versus placebo in 39 clinically stable outpatients with schizophrenia or schizoaffective disorder and comorbid insomnia [38•]. The study included an 8-week randomized period, followed by a single-blind 2-week placebo phase to assess durability of drug effects. Eszopiclone demonstrated significant efficacy over placebo on the primary outcome measure of change in ISI score, with a between group difference of nearly four points on the scale [38•]. During the discontinuation period, there was no difference between eszopiclone and placebo in the change in ISI score [38•]. Despite improvements in insomnia, eszopiclone did not demonstrate benefit on the secondary outcome of change in Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Consensus Cognitive Battery, which assesses processing speed, attention, verbal and non-verbal working memory, verbal and visual learning, reasoning/ problem solving, and social cognition [38•]. Exploratory analysis suggested subscale improvement with eszopiclone on a working memory test, the letter number span component of MATRICS, for participants with schizophrenia (but not schizoaffective disorder), which correlated with the change in ISI score [38•]. However, improvements in working memory observed during the double-blind phase with eszopiclone did not persist into the single-blind placebo phase, suggesting such changes were not durable [38•].
In addition to changes in working memory, it has been posited that eszopiclone might lead to improved sleep-dependent procedural memory consolidation in persons with schizophrenia. Patients with schizophrenia have demonstrated impairments in overnight improvement on a well-established finger-tapping motor sequence task (MST) [39]. Because patients with schizophrenia demonstrate reductions in sleep spindles [40] and sleep-dependent improvement on the MST correlates with these waxing-waning electroencephalographic oscillations characteristic of non-rapid eye movement sleep [41], examining the effects of agents such as eszopiclone, which may increase sleep spindles through potentiation of the GABAergic thalamic reticular nucleus (the primary site of sleep spindle generation), is a promising line of inquiry. Wamsley and colleagues examined both the ability of eszopiclone to generate sleep spindles as well as its associative effects on overnight MST performance [42•]. After screening, 21 patients with schizophrenia completed in laboratory baseline visits, which consisted of two consecutive nights of polysomnography, with the MST performed during the second night of sleep. One week later, participants completed a similar treatment visit; however, patients were randomized to either eszopiclone 3 mg or placebo and completed the MST using an alternate sequence compared to baseline. Eszopiclone significantly increased the number and density of spindles relative to baseline compared to placebo, but did not significantly enhance overnight MST improvement [42•]. When eszopiclone and placebo groups were combined, sleep spindle number and density correlated with overnight MST improvement [42•]. These findings support the notion that pharmacologic enhancement of sleep spindles may have some benefit in patients with schizophrenia; however, further research is indicated to determine what domains may be impacted and whether such improvements have demonstrable clinical impact on the disorder.
Post-Traumatic Stress Disorder
PTSD is among the most common psychiatric conditions, with an overall lifetime prevalence in the USA of roughly 7 % [43]. Sleep disturbance is a core feature of PTSD, with insomnia and nightmares both components of the diagnostic criteria for the disorder [1]. Additionally, insomnia and nightmares may play a role in the morbidity of the disorder, and thus be an important target of therapy [44]. Despite this, the evidence base for treatment of sleep disturbance in PTSD is relatively scant. Recent review of the literature supports the use of prazosin as a first-line agent for both insomnia and nightmares in PTSD [45].
There is also recent evidence that suggests that eszopiclone may provide benefit as an adjunctive agent in the treatment of sleep disturbance in PTSD. Pollack and colleagues examined the use of eszopiclone 3 mg nightly in patients with PTSD and co-occurring sleep disturbance, using a randomized, double-blind, placebo-controlled crossover design [46•]. Three weeks of eszopiclone compared to placebo was associated with significantly reduced sleep onset latency and improvement in sleep quality (measured by the PSQI). Additionally, similar to benefits of co-therapy in major depression [9, 10•], eszopiclone also significantly improved PTSD symptoms [assessed with the clinician-administered short PTSD rating interview (SPRINT) and the clinician-administered PTSD scale (CAPS)], even when sleep-related items were excluded [46•]. Although these results are promising, the study was relatively small (N = 23), and future work replicating such results as well as evaluating longitudinal effects beyond short-term use are indicated. In addition, comparative effectiveness studies would be helpful in determining whether sedative-hypnotics provide benefit above other agents frequently used off-label to treat insomnia in PSTD. In particular, atypical antipsychotics, which are commonly prescribed largely for their sedative-hypnotic properties in patients with PTSD [47], should be compared both in efficacy on sleep and PTSD symptoms, as well as side-effect profile, given the negative health consequences (e.g., weight gain, metabolic syndrome, etc.) associated with second generation antipsychotics.
Conclusions
Because sleep plays an integral role in the presentation and course of many psychiatric disorders, research that examines the use of sedative-hypnotics in mental illness is likely to significantly impact the delivery of care in clinical psychopharmacology. However, despite recent inroads made by the investigations described in this review, the evidence base for the use of hypnotic medications in psychiatric illness remains relatively limited. There are myriad factors that influence the use of sedative-hypnotics by both primary care and behavioral health providers, and their optimal use remains controversial [48, 49]. However, it is crucial that the field overcomes the stigma surrounding these medications to empirically determine how and under what circumstances these agents can be most helpful for patients with psychiatric illness. Such inquiry is particularly important since management of sleep disturbance has the potential to reduce the morbidity and mortality associated with psychiatric disorders, as well as prevent major illness episodes, which are principal goals in the care of patients with mental illness.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Krystal AD. Psychiatric disorders and sleep. Neurol Clin. 2012;30(4):1389–413.
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien: American Academy of Sleep Medicine; 2014.
Wu JQ, Appleman ER, Salazar RD, Ong JC. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Intern Med. 2015;175(9):1461–72.
Quera-Salva MA, Lemoine P, Guilleminault C. Impact of the novel antidepressant agomelatine on disturbed sleep-wake cycles in depressed patients. Hum Psychopharmacol. 2010;25(3):222–9.
Taylor D, Sparshatt A, Varma S, Olofinjana O. Antidepressant efficacy of agomelatine: meta-analysis of published and unpublished studies. BMJ. 2014;348:g1888.
Guaiana G, Gupta S, Chiodo D, Davies SJ, Haederle K, Koesters M. Agomelatine versus other antidepressive agents for major depression. Cochrane Database Syst Rev. 2013;12, CD008851.
Ohayon MM, Caulet M, Lemoine P. Comorbidity of mental and insomnia disorders in the general population. Compr Psychiatry. 1998;39(4):185–97.
Fava M, McCall WV, Krystal A, Wessel T, Rubens R, Caron J, et al. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biol Psychiatry. 2006;59(11):1052–60.
Fava M, Schaefer K, Huang H, Wilson A, Iosifescu DV, Mischoulon D, et al. A post hoc analysis of the effect of nightly administration of eszopiclone and a selective serotonin reuptake inhibitor in patients with insomnia and anxious depression. J Clin Psychiatry. 2011;72(4):473–9. Randomized study demonstrating efficacy of eszopiclone in the treatment of insomnia in patients with anxious depression as well as improvement in mood symptoms.
Pollack M, Kinrys G, Krystal A, McCall WV, Roth T, Schaefer K, et al. Eszopiclone coadministered with escitalopram in patients with insomnia and comorbid generalized anxiety disorder. Arch Gen Psychiatry. 2008;65(5):551–62.
Fava M, Asnis GM, Shrivastava RK, Lydiard B, Bastani B, Sheehan DV, et al. Improved insomnia symptoms and sleep-related next-day functioning in patients with comorbid major depressive disorder and insomnia following concomitant zolpidem extended-release 12.5 mg and escitalopram treatment: a randomized controlled trial. J Clin Psychiatry. 2011;72(7):914–28. Randomized study demonstrating efficacy of zolpidem extended-release in the treatment of insomnia in patients with major depressive disorder.
Xi M, Chase MH. Effects of eszopiclone and zolpidem on sleep and waking states in the adult guinea pig. Sleep. 2008;31(7):1043–51.
McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatr Rep. 2013;15(9):389.
McCall WV, Benca RM, Rosenquist PB, Riley MA, Hodges C, Gubosh B, et al. A multi-site randomized clinical trial to reduce suicidal ideation in suicidal adult outpatients with major depressive disorder: development of a methodology to enhance safety. Clin Trials. 2015;12(3):189–98.
Wichniak A, Wierzbicka A, Jernajczyk W. Patients with insomnia and subthreshold depression show marked worsening of insomnia after discontinuation of sleep promoting medication. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(7):1671–6.
Mews MR, Rombold F, Quante A. Efficacy and safety of low-dose doxepin in depressed patients suffering from insomnia: a retrospective, naturalistic case series analysis. Prim Care Companion CNS Disord. 2014;16(1).
Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999-2010. Sleep. 2014;37(2):343–9.
Ng TH, Chung KF, Ho FY, Yeung WF, Yung KP, Lam TH. Sleep-wake disturbance in interepisode bipolar disorder and high-risk individuals: a systematic review and meta-analysis. Sleep Med Rev. 2015;20:46–58.
Robillard R, Naismith SL, Hickie IB. Recent advances in sleep-wake cycle and biological rhythms in bipolar disorder. Curr Psychiatr Rep. 2013;15(10):402.
Plante DT, Winkelman JW. Sleep disturbance in bipolar disorder: therapeutic implications. Am J Psychiatry. 2008;165(7):830–43.
Cretu JB, Culver JL, Goffin KC, Shah S, Ketter TA. Sleep, residual mood symptoms, and time to relapse in recovered patients with bipolar disorder. J Affect Disord. 2016;190:162–6.
McElroy SL, Winstanley EL, Martens B, Patel NC, Mori N, Moeller D, et al. A randomized, placebo-controlled study of adjunctive ramelteon in ambulatory bipolar I disorder with manic symptoms and sleep disturbance. Int Clin Psychopharmacol. 2011;26(1):48–53.
Norris ER, Karen B, Correll JR, Zemanek KJ, Lerman J, Primelo RA, et al. A double-blind, randomized, placebo-controlled trial of adjunctive ramelteon for the treatment of insomnia and mood stability in patients with euthymic bipolar disorder. J Affect Disord. 2013;144(1-2):141–7. Randomized study demonstrating mood stabilizing properties of adjunctive ramelteon in the treatment of bipolar disorder.
Schaffer CB, Schaffer LC, Miller AR, Hang E, Nordahl TE. Efficacy and safety of nonbenzodiazepine hypnotics for chronic insomnia in patients with bipolar disorder. J Affect Disord. 2011;128(3):305–8.
Terao T. Comparison of manic switch onset during fluoxetine and trazodone treatment. Biol Psychiatry. 1993;33(6):477–8.
Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164(4):549–50.
Wichniak A, Jarkiewicz M, Okruszek Ł, Wierzbicka A, Holka-Pokorska J, Rybakowski JK. Low risk for switch to mania during treatment with sleep promoting antidepressants. Pharmacopsychiatry. 2015;48(3):83–8.
Jackson JG, Diaz FJ, Lopez L, de Leon J. A combined analysis of worldwide studies demonstrates an association between bipolar disorder and tobacco smoking behaviors in adults. Bipolar Disord. 2015;17(6):575–97.
Augustson EM, Wanke KL, Rogers S, Bergen AW, Chatterjee N, Synder K, et al. Predictors of sustained smoking cessation: a prospective analysis of chronic smokers from the alpha-tocopherol beta-carotene cancer prevention study. Am J Public Health. 2008;98(3):549–55.
Boutou AK, Tsiata EA, Pataka A, Kontou PK, Pitsiou GG, Argyropoulou P. Smoking cessation in clinical practice: predictors of six-month continuous abstinence in a sample of Greek smokers. Prim Care Respir J. 2008;17(1):32–8.
Forrest PE, Brinson AJ, Gannon JM, George TP, Perkins KA, Chengappa KN. An association between the use of hypnotics and quit status in the treatment of nicotine dependence with varenicline in bipolar disorder. J Clin Psychopharmacol. 2015;35(2):199–200.
Lin CY, Tsai GE, Lane HY. Assessing and treating cognitive impairment in schizophrenia: current and future. Curr Pharm Des. 2014;20(32):5127–38.
Chouinard S, Poulin J, Stip E, Godbout R. Sleep in untreated patients with schizophrenia: a meta-analysis. Schizophr Bull. 2004;30(4):957–67.
Palmese LB, DeGeorge PC, Ratliff JC, Srihari VH, Wexler BE, Krystal AD, et al. Insomnia is frequent in schizophrenia and associated with night eating and obesity. Schizophr Res. 2011;133(1-3):238–43.
Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin CM. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev. 2012;16(1):83–94.
Goel N, Rao H, Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2009;29(4):320–39.
Tek C, Palmese LB, Krystal AD, Srihari VH, DeGeorge PC, Reutenauer EL, et al. The impact of eszopiclone on sleep and cognition in patients with schizophrenia and insomnia: a double-blind, randomized, placebo-controlled trial. Schizophr Res. 2014;160(1-3):180–5. Randomized study demonstrating efficacy of eszopiclone in the treatment of insomnia in patients with schizophrenia.
Manoach DS, Cain MS, Vangel MG, Khurana A, Goff DC, Stickgold R. A failure of sleep-dependent procedural learning in chronic, medicated schizophrenia. Biol Psychiatry. 2004;56(12):951–6.
Manoach DS, Pan JQ, Purcell SM, Stickgold R. Reduced sleep spindles in schizophrenia: a treatable endophenotype that links risk genes to impaired cognition? Biol Psychiatry. 2015.
Morin A, Doyon J, Dostie V, Barakat M, Hadj Tahar A, Korman M, et al. Motor sequence learning increases sleep spindles and fast frequencies in post-training sleep. Sleep. 2008;31(8):1149–56.
Wamsley EJ, Shinn AK, Tucker MA, Ono KE, McKinley SK, Ely AV, et al. The effects of eszopiclone on sleep spindles and memory consolidation in schizophrenia: a randomized placebo-controlled trial. Sleep. 2013;36(9):1369–76. Controlled study that demonstrates eszopiclone may impact sleep-dependent procedural memory consolidation in patients with schizophrenia via enhancement of sleep spindles.
Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–23.
Pigeon WR, Gallegos AM. Posttraumatic stress disorder and sleep. Sleep Med Clin. 2015;10(1):41–8.
Lipinska G, Baldwin DS, Thomas KG. Pharmacology for sleep disturbance in PTSD. Hum Psychopharmacol. 2016;31(2):156–63.
Pollack MH, Hoge EA, Worthington JJ, Moshier SJ, Wechsler RS, Brandes M, et al. Eszopiclone for the treatment of posttraumatic stress disorder and associated insomnia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(7):892–7. Randomized study demonstrating efficacy of eszopiclone in the treatment of insomnia in patients with PTSD.
Hermes ED, Sernyak M, Rosenheck R. Use of second-generation antipsychotic agents for sleep and sedation: a provider survey. Sleep. 2013;36(4):597–600.
Sivertsen B, Nordhus IH, Bjorvatn B, Pallesen S. Sleep problems in general practice: a national survey of assessment and treatment routines of general practitioners in Norway. J Sleep Res. 2010;19(1 Pt 1):36–41.
MacDonald J, Garvie C, Gordon S, Huthwaite M, Mathieson F, Wood AJ, et al. 'Is it the crime of the century?': factors for psychiatrists and service users that influence the long-term prescription of hypnosedatives. Int Clin Psychopharmacol. 2015;30(4):193–201.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Shane Creado declares no conflict of interest.
David T. Plante has received and is supported by grants from the National Institute of Mental Health (K23MH099234), Brain and Behavior Research Foundation and American Sleep Medicine Foundation.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Creado, S., Plante, D.T. An Update on the Use of Sedative-Hypnotic Medications in Psychiatric Disorders. Curr Psychiatry Rep 18, 78 (2016). https://doi.org/10.1007/s11920-016-0717-y
Published:
DOI: https://doi.org/10.1007/s11920-016-0717-y