Abstract
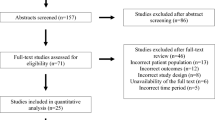
Depression and anxiety during pregnancy are common, and patients and providers are faced with complex decisions regarding various treatment modalities. A structured discussion of the risks and benefits of options with the patient and her support team is recommended to facilitate the decision-making process. This clinically focused review, with emphasis on the last 3 years of published study data, evaluates the major risk categories of medication treatments, namely pregnancy loss, physical malformations, growth impairment, behavioral teratogenicity, and neonatal toxicity. Nonpharmacological treatment options, including neuromodulation and psychotherapy, are also briefly reviewed. Specific recommendations, drawn from the literature and the authors’ clinical experience, are also offered to help guide the clinician in decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During pregnancy, the point prevalence is 11 % for depression and 13 % for anxiety [1]. Given that psychotropic medications are first-line treatments for both depression and anxiety, it is unsurprising that many pregnant women will be prescribed medicine to treat these symptoms; antidepressant prescribing during pregnancy has increased almost fourfold since the 1990s [2]. In a recent study of privately insured Americans, 10 % of pregnant women received a prescription for some psychotropic medication, of which 25 % were diagnosed with depression and 24.4 % anxiety [3].
As a recent New York Times article highlighted, psychiatric illness during pregnancy remains both stigmatized and fraught with complex decisions for the mother-to-be [4]. Furthermore, survey and interview data suggest that depressed pregnant women experience moderate to high levels of decisional conflict about whether to take medication, regardless of socioeconomic status, illness severity, or current treatment with medication [5]. Clinicians also face a large and conflicting body of research on the risk-benefit ratio of medications in pregnancy as well as fear of litigation if the decision to intervene is associated with a negative outcome.
In recognition of the challenges inherent in making treatment decisions in cases of pregnant women with depression, Wisner and colleagues developed a model for risk-benefit decision-making in pregnancy [6]. In addition to guiding the psychiatrist in structuring the presenting problem, the model recommends that risk for each option be discussed with the patient in five major groups: pregnancy loss, physical malformations, growth impairment, behavioral teratogenicity, and neonatal toxicity. The risk of the illness itself is also reviewed. The patient’s active participation, and that of her support team, is imperative, which allows for her values to inform the decision as well as assesses her capacity to give informed consent.
This clinically focused review is intended to support clinicians in shared decision-making and informed consent with patients regarding the treatment of unipolar depression and anxiety during pregnancy. We discuss the most recent evidence on the risks of anxiety and depression in pregnancy. Guideline-supported interventions for depression and anxiety will also be discussed with an emphasis on the risks and benefits of these treatments during pregnancy; treatments reviewed will include psychopharmacology, neuromodulation, and psychotherapy [7–9]. The discussion of risks for medication options will be grouped according to Wisner’s domains, with the addition of mother-specific risks, in order to facilitate collaborative decision-making with patients. Finally, risks and benefits of neuromodulation and psychotherapy will be reviewed more briefly.
Risk of Depression and Anxiety in Pregnancy
In order to fully appreciate the risks and benefits of the treatment options for depression and anxiety during pregnancy, it is essential to consider the risks of depression and anxiety themselves during pregnancy. One such risk is mortality from the illness, such as suicide or infanticide. Relapse is also of concern: although even women who continue medication during pregnancy risk relapse, the risk of depression relapse during pregnancy is increased in women who have had depressive symptoms within the preceding 6 months and discontinue antidepressants, in women with a lifetime history of more than 4 depressive episodes, or a history of moderate to severe pre-pregnancy depressive episodes [10, 11]. Though there is limited evidence that generalized anxiety disorder may actually improve throughout pregnancy [12], pregnancy may be a vulnerable time for development or worsening of other anxiety disorders. For instance, pregnant women have nearly doubled prevalence of obsessive-compulsive disorder (OCD) relative to the general population [13], a third of women with OCD will worsen during pregnancy [14], and 5 % will have onset during pregnancy.
There is also growing evidence that psychiatric illness during pregnancy carries its own somatic risk to the baby and mother. A recent large retrospective cohort study of pregnant veterans found an association between post-traumatic stress disorder (PTSD) and preterm birth [15]. This is consistent with data from another large cohort, this one prospective, that found that PTSD with comorbid depression was as strong a risk factor for preterm birth as a history of previous preterm birth (OR 4.08, 95 % CI 1.27–13.15) [16•]. Preterm birth and low birth weight were also associated with anxiety symptoms at any time in pregnancy in a meta-analysis of studies using interview or questionnaire diagnostic information [17]. Pregnant women with depressive symptoms are more likely to have preterm birth than non-depressed pregnant women, even in the absence of medications, and some, but not all, studies have associated depression with intrauterine growth restriction (IUGR) [18•, 19, 20]. A recent prospective study suggests that high levels of perceived maternal stress at 20 weeks’ gestational age correlates with increased risk for small for gestational age (SGA) at delivery even in babies who had been growing normally when measured at 20 weeks [21]. Additionally, mothers scoring in the highest range of depression and anxiety had an increased risk of SGA, especially with male infants. This study, however, does not address whether any of the patients were taking antidepressants. Several studies have shown that depression is itself a risk factor for preeclampsia, or maternal hypertension with proteinuria, which poses a serious risk to the mother [14, 22], and a recent prospective study revealed a statistically significant increased risk of hypertension during pregnancy in women with comorbid depression and anxiety [23].
There is also evidence that the offspring of mothers who suffer from depression during pregnancy are at increased risk for behavioral and emotional problems. Although maternal depression during pregnancy is a predictor of behavioral and temperament problems in children irrespective of antenatal medication exposure [24], many studies do not control for antidepressant exposure during pregnancy. One study evaluating the risk of depression and behavioral problems at age 5 found that the greatest risk is when children are exposed to high levels of maternal depression during the preschool years, but the risk of these symptoms was also increased in children exposed to depression from pregnancy through early childhood, highlighting the risk of allowing major depression to persist in and past the antenatal phase inadequately treated [25•]. This risk may extend even into adulthood: a retrospective cohort study recently indicated that children exposed to antenatal maternal anxiety, depression, and stress are at increased risk for behavioral problems and depression at age 21, even when adjusted for health habits and life events [26]. Notably, children of mothers with antenatal depression also appear to be at increased risk of maltreatment during childhood, the etiology of which appears to involve interplay between offspring temperamental changes resulting from in utero exposure to maternal depression and the depressed mother’s attachment and caregiving style [27]. In combination, maternal depression and childhood maltreatment significantly increase the risk of offspring adulthood depression.
Treatment Options
Antidepressants
In any discussion of the risks and benefits of medication, it should be noted that few studies examine the benefit of antidepressant treatment to the infant. One notable exception found that antidepressant treatment during pregnancy alleviated a cognitive change referred to as P50 gating in children of mothers with antenatal anxiety [28]. This underscores the need to study the positive as well as negative effects of psychotropic medication use during pregnancy. Further, the literature is complicated by multiple limitations, including lack of access to psychiatric histories of participants and associated poor health habits of pregnant women who take these medications relative to other women [29]. It may be difficult to ascertain the extent to which adverse events are related to the medication, the disease itself, or the health habits of the mother taking the medication.
Pregnancy Loss
In sum, available data suggest that there is a small increased risk of miscarriage for women taking any antidepressant, though this risk becomes less statistically significant when excluding studies of poor quality [29, 30•]. Moreover, most studies do not differentiate between induced and spontaneous abortion, so it could be that depressed women may be more likely to pursue pregnancy termination.
Regarding selective serotonin reuptake inhibitors (SSRIs), a recent large study indicated that SSRI exposure during pregnancy is associated with a very small increased risk of miscarriage in the first trimester (HR 1.08, 1.04–1.13), but not of second-trimester pregnancy loss [31•]. Notably, the risk of first-trimester miscarriage was lower in women who took SSRIs but were not identified as having a diagnosis of depression or anxiety than for women who carried a diagnosis but were not taking an SSRI, suggesting that the association may be due to the mental health disorder itself. Also of note, pregnancies in which an SSRI was used were also associated with unhealthier lifestyle profiles, an important potential confounder. Another large cohort study found that there was a small increased risk of miscarriage (HR 1.27, 1.22–1.33) in women who took SSRIs during the first 35 days of pregnancy, but that this was roughly equivalent to the increased risk of miscarriage in women who discontinued SSRIs 3–12 months prior to pregnancy (HR 1.24, 1.18–1.30); the risk of miscarriage was not related to dosing of SSRIs [32]. Study authors concluded that the risk of miscarriage is likely not to be modified by discontinuing SSRI prior to pregnancy.
Physical Malformations
Major congenital anomalies, especially cardiac defects, are of concern when a fetus is exposed to medication during organogenesis in the first trimester of pregnancy. The baseline against which the relative risk of major congenital malformations in this population must be considered is that of the general population: 2–3 % [33]. Given this, although there is conflicting evidence that there is an increased risk of such malformations with medication treatment, any increase in risk is likely to result in a very small absolute risk change. There is differing data by class of medication, so we will review SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), bupropion, and mirtazapine.
Most studies evaluating rates of congenital malformations overall following SSRI exposure find no elevated risk with medication use [34–36], with one well-controlled study as an exception (OR 1.3, 1.1–1.6) [37]. A recent large Bayesian analysis of registry data considering both specific anomalies and specific medications revealed an equivocally increased risk of neural tube defects following citalopram and ventricular septal defects (VSD) after fluoxetine [38]. More significant were associations between paroxetine and anencephaly, atrial septal defects, right ventricular outflow tract obstruction, gastroschisis, and omphalocele. The study authors were not able to control for maternal depression and noted that if causal, the associations result in a small absolute increased risk.
Older meta-analyses evaluating the risk of cardiovascular malformations have found a small but notable association with SSRI use during pregnancy with paroxetine, fluoxetine, and sertraline specifically implicated [34, 39–42]. More recently, a registry-based study including live births, fetal death after 20 weeks, and termination due to known genetic diagnosis found an increased risk of congenital heart defects, particularly severe defects (OR 1.56, 1.02–1.39), tetralogy of Fallot (OR 3.16, 1.52–6.58), and Ebstein’s anomaly (OR 8.23, 2.92–23.16) following SSRI exposure [43]. Importantly, though women with diabetes or taking anti-epileptic drugs were excluded, there was no adjustment for confounding variables, including psychiatric diagnosis or lifestyle behaviors.
Regarding SNRIs and TCAs, many recent studies show no association between these medications and major congenital malformations [34, 35, 44–46]. One Canadian database study did find an association between venlafaxine and a small number of noncardiac malformations [47], and two large older studies did find an increased association between cardiac malformations and tricyclic antidepressant use, particularly clomipramine [34, 48].
There is less data investigating bupropion and mirtazapine. In one well-controlled study, antenatal exposure to bupropion was associated with a higher risk of VSD relative both to controls and to women taking bupropion in combination with other antidepressants (OR 2.5, 1.3–5.0) [49]. A multicenter prospective cohort study of 357 pregnancies exposed to mirtazapine found no difference between overall rates of congenital anomalies relative to SSRI-exposed pregnancies; though there was an increased rate relative to controls, the rate was nonsignificant when given after the first trimester [50].
As previously indicated, confounders may play an important role in biasing study outcomes, and some of these confounders may be not yet fully identified. For example, a large Scandinavian cohort analysis found that although there was a small increased risk of cardiac and other birth defects in babies exposed to antenatal SSRIs or venlafaxine when controlled for maternal age, diabetes, teratogens, and smoking (OR 1.13, 1.06–1.20), this association disappeared in a sibling-controlled analysis, suggesting that familial and lifestyle factors may be important confounders [51]. Similarly, a large Medicaid data study found that despite an increased risk of cardiac defects across all antidepressant categories in an unadjusted analysis, when restricting to those mothers with depression and adjusting for known cardiac defect risk factors and proxies for depression severity, the increased risk vanished, from OR 1.25 down to 1.06 (0.93–1.22), including for fluoxetine, paroxetine, bupropion, and TCAs [52•].
In sum, there are conflicting data regarding the risk of congenital malformations, and in particular cardiac defects, following early trimester treatment with antidepressants. Importantly, paroxetine has been most consistently associated with major congenital anomalies. However, especially for the SSRIs, this appears to result in a small absolute risk increase and must be weighed against the risk of untreated depression or anxiety, which may be an important confounding factor in most studies and may confer independent risk for such malformations.
Growth Impairment
Being SGA or having IUGR puts the infant at risk for adverse health outcomes, including increased mortality. Low birth weight is defined as <2500 g, but if consistent with the infant’s gestational age, then the infant is not SGA. Being SGA can occur because of genetic programming (i.e., a small parent), but when pathological it is referred to as IUGR. IUGR is diagnosed when (a) an infant is less than the 10th percentile on the basis of gestational age, and (b) the abdominal circumference is less than the 2.5 percentile.
An older, large database study indicates that there is no effect of TCA use on birth weight overall, though the analysis for classification of SGA (i.e., 2 standard deviations below the expected weight) was of borderline significance (OR 1.37, 1.00–1.95) [34]. The same study found significant effects of SNRI use on low birth weight (OR 1.87, 1.37–1.64) and SGA (OR 1.84, 1.20–2.81). More recently, a review of studies with small data pools showed no relation between SGA babies and the use of TCAs during pregnancy [29]. Results have been much more mixed for the SSRIs, but the most rigorously conducted studies controlling for variables like mental health diagnoses find no association between SSRI use and SGA [53–56]. One small study found no association between use of bupropion and birth weight [57].
Of note, in a meta-analysis of antidepressant use during pregnancy, the difference of 74 g between infants exposed and not exposed to antenatal antidepressants was not statistically significant after controlling for mental health diagnoses [30•]. As above, antenatal depression in and of itself has been associated with IUGR, and stress with SGA, again underscoring the importance of exploring the contribution of the depressive or anxiety illness to such findings.
Behavioral Teratogenicity
As discussed previously, offspring of mothers with antenatal depression are at elevated risk for behavioral and emotional problems, even into adulthood. There is also concern that treatment with medication might lead to long-term cognitive and emotional consequences. Some studies have found that SSRI exposure does not affect IQ scores, language development, or behavioral problems [58–60]. A recent large cohort study did find a statistically significant adjusted association between language delay at age 3 and exposure to SSRIs in at least two time periods during pregnancy [61]. However, the same study relied on maternal reports of language competence, was not powered to distinguish between moderate and severe language impairment, and also found an association between language delay and exposure to short- and long-term symptoms of depression and anxiety during pregnancy. As such, and consistent with other similar positive findings concerning language and motor development, the contribution of medication versus illness as well as the clinical impact of findings are uncertain [62, 63].
Regarding behavioral problems, a prospective cohort study demonstrated a significant adjusted association between antenatal use of SSRIs and maternal reports of internalizing and anxious behaviors that was stable at child ages 3 and 6 [64]. Of note, there was no association with externalizing behavior in the same group. A similar association was also found with antenatal exposure to maternal depression and internalizing (especially anxious) and externalizing behavioral problems at child ages 3 and 6. These findings are consistent with another large cohort study, which included matched siblings discordant for antidepressant exposure [65]. In the adjusted, sibling-matched analyses, there was a small increase in the anxiety subscale of internalizing behaviors at 3 years old for children exposed to antenatal antidepressants (beta coefficient 0.64, 0.26–1.02). Of note, a maternal lifetime history of depression (reported at 17 weeks’ gestation) was also associated with internalizing behaviors in offspring in the adjusted, sibling-matched analysis (beta coefficient 0.19, 0.02–0.38). In concert, these data suggest that antidepressants may be associated with a small increase in internalizing, particularly anxiety, behavioral problems in children, but that genetic factors and maternal depression are also important contributors.
There is an emerging and complex database concerning the risk for autism spectrum disorder (ASD) following antenatal antidepressant treatment. Two case–control studies, both well-controlled but relying on retrospective reporting, found that women who took an SSRI during pregnancy were more likely to have a child diagnosed with ASD relative to women who did not take an SSRI during pregnancy [66, 67]. It is important to acknowledge that in their conclusion, the authors of the first study emphasized that the proportion of cases of ASD attributable to SSRIs was less than 3 % in their population, and the second study only found an increase in ASD with normal intellectual ability. Two other studies, both retrospective cohort analyses of registry data [68, 69•] and both controlling for confounders, did not find an association between SSRI use during pregnancy and ASD in children, though the latter did note an association with risk of attention-deficit/hyperactivity disorder (OR 1.81, 1.22–2.70). The mixed literature highlights the importance of considering maternal psychiatric illness as a contributing factor and suggests that if there is an effect of antidepressant treatment, it is likely quite small and relatively mild.
Neonatal Toxicity
In this domain, we consider the perinatal risks of exposure to medications, including preterm birth, persistent pulmonary hypertension of the newborn (PPHN), and poor neonatal adaptation syndrome (PNAS).
Preterm birth, defined as birth before 37 weeks’ gestational age, is associated with an increased risk of neonatal death and a host of adverse outcomes in child development, including intellectual, behavioral disorders, cerebral palsy as well as respiratory, ophthalmic, and auditory dysfunction; the cost associated with preterm birth in the United States in 2007 was over 26 billion dollars [70]. The baseline preterm birth rate in the United States is approximately 11 % [71]. Large database studies and meta-analyses have demonstrated that the use of TCAs, SSRIs, and SNRIs is associated with preterm birth, the highest risk being with the TCAs and the lowest risk with SSRIs, with no apparent risk difference among SSRIs [30•, 34, 38, 54, 72]. Generally, the literature indicates that prolonged exposure to SSRIs during pregnancy is associated with shorter gestational age. It must be noted that gestational length in many studies is shortened by only a few days and is of questionable clinical significance.
Interestingly, there is evidence from a very small study that SSRI treatment may in fact extend gestational age and raise birth weight relative to women who are not treated for depression; though these findings were significant by ANOVA testing, they were not by χ 2 testing, likely due to the small size of the study [73]. Nevertheless, as above, pregnant women with depressive symptoms are more likely to have preterm birth than are non-depressed women, even in the absence of medications, again highlighting the theme that the risk of medications is confounded by the associated risk of the disease state, which may or may not be mediated with treatment [18•, 20].
PPHN is a life-threatening condition in which pulmonary vascular resistance fails to decrease following delivery, resulting in ineffective oxygenation and potential respiratory failure [29]. Some studies have shown that the rate of PPHN in infants of mothers who took SSRIs after 20 weeks of pregnancy is above the average rate of 1–2 cases per 1000 births [34, 74, 75], most recently as 2.9–3.5 infants per 1000 births following third-trimester exposure to SSRIs [76]. However, not all studies find this association, and many other factors, like obesity, cesarean section, and smoking, all of which have elevated rates in depressed women, might account for an association between PPHN and SSRI use [29]. Most recently, a large Medicaid cohort study found that the odds ratio adjusted for depression for primary PPHN in women taking SSRIs was only slightly elevated and of borderline significance (OR 1.28, 1.01–1.64) and not significantly elevated for non-SSRI antidepressants [77•]. In accordance with this data, the FDA has withdrawn a 2006 black box warning regarding the risk of PPHN and antidepressants [78].
PNAS is marked by a broad constellation of physical and behavioral symptoms observed in 10–30 % of neonates exposed to antidepressants near delivery [79, 80]. Symptoms are most commonly associated with withdrawal from short half-life antidepressants, such as venlafaxine or paroxetine, or toxicity of long half-life medicines, like fluoxetine, but have also been associated with all antidepressants [81]. The risk of PNAS also appears to be dose-related. Specific symptoms include agitation, feeding difficulties, hyperreflexia, hypertonia, jaundice, respiratory distress, tremor, and vomiting [29]. Most of these symptoms are mild in nature and resolve within 2 weeks of delivery, although more severe symptoms may require special care. One recent study found that only 3 % of infants with PNAS demonstrated severe symptoms on a standardized PNAS scale [80]. Tapering the medication near to delivery will decrease the risk of PNAS, but may put the mother at risk for postpartum depression, which may outweigh concern for mild symptoms. Interestingly, there is only one case series evaluating the incidence of PNAS after exposure to mirtazapine; this found a significantly diminishment of PNAS in children who were partially or fully breastfed, raising a question as to whether breastfeeding might reduce risk following exposure to other antidepressants [82].
Maternal Risks
Beyond those risks associated with antidepressant treatment in any given individual, risks identified for the pregnant person include post-partum hemorrhage and gestational hypertension. Acute postpartum hemorrhage is of concern in treatment with SSRIs as these medications may be mild platelet inhibitors [83]. Four studies have examined women exposed to antidepressants proximate to delivery, two of which found an increased risk [34, 84] and two of which did not [85, 86]. As with PNAS, tapering antidepressants before delivery may reduce the risk, but the increased risk of bleeding is controversial, and doing so may lead to a postpartum relapse of depression.
Some studies have indicated an association between gestational hypertension and antidepressants [87, 88]. Currently, however, antidepressants do not appear to “cause” gestational hypertension [89], and a woman’s controlled hypertension is not a contraindication to antidepressant use during pregnancy. As above, depression in and of itself is a risk factor for gestational hypertension and preeclampsia.
Benzodiazepines
Benzodiazepines, which reduce anxiety symptoms through the stimulation of the gamma-Aminobutyric acid (GABA) receptor, are commonly used as treatment strategies for anxiety, including in pregnancy: one study found that 3.9 % of pregnant women were prescribed benzodiazepines, and 1.2 % a combination of antidepressant and anxiolytic [3]. Benzodiazepines also cross the placenta, and one recent study found a higher fetus to mother ratio of diazepam in women with diabetes and hypertension relative to healthy control patients [90]. The authors noted that this ratio did not correlate with change in Apgar scores and postulated that the increased ratio may be due to decreased protein binding and increased placental transfer in diabetes and hypertension.
Pregnancy Loss
Overall, there are very limited data on the risk of pregnancy loss following benzodiazepine exposure. A systematic review of the risks of benzodiazepines in pregnancy found elevated rates of spontaneous abortion in small studies exploring the effect on the fetus of intentional suicidal overdose with high-dose alprazolam, diazepam, medazepam, nitrazepam, and chlordiazepoxide [91]. However, an older small case series of women who were prescribed diazepam for hyperemesis gravidarum did not reveal a higher risk of spontaneous abortion [92].
Physical Malformations
Historically, first-trimester benzodiazepine use was thought to be associated with skeletal and oral cleft abnormalities and central nervous system dysfunction, and clinicians were encouraged to avoid first-trimester benzodiazepine use [93]. More recently, a systematic review identified that alprazolam, clonazepam, and diazepam were not associated with major malformations when recall biases were accounted for, though lorazepam was associated with higher rates of anal atresia in a small number of cases relative to other benzodiazepines [91]. Two large cohort studies, one British and the other Swedish, did not find any increased risk for major congenital malformations following antenatal exposure to benzodiazepines, even in combination with SSRIs [94, 95]. Contrary to physician concern, it is therefore unlikely that benzodiazepines significantly increase the risk of major congenital malformations, and these medications should not be avoided for this reason.
Growth Impairment
There are limited, and no recent, data regarding birth weight following benzodiazepine exposure. An older Swedish registry study found a small increased risk of low birth weight in both early- and late-pregnancy benzodiazepine exposure, though the rate was higher in late-pregnancy exposure (early, OR 1.30, 1.06–1.59; late, 1.89, 1.29–2.76) [96]. While the rates of SGA were also somewhat increased, they did not meet statistical significance, raising questions as to the clinical impact of this growth impairment.
Behavioral Teratogenicity
There have been no recent studies specifically examining the long-term neurodevelopmental consequences of antenatal benzodiazepine exposure. A systematic review published in 2014 did summarize several older studies that revealed mixed data regarding these consequences [97]. However, only one study evaluated children beyond 18 months, and this study did not find any effect on behavior at ages 9 to 10 [98].
Neonatal Toxicity
Swedish registry data suggest that benzodiazepine use during later trimesters does increase the odds of preterm birth (OR 1.87, 1.20–2.89) [99]. When benzodiazepines and SSRIs were both used, odds of preterm birth increased markedly (OR 3.43, 2.33–5.06) after adjustment for year of birth, maternal age, parity, smoking status, BMI, and number of previous miscarriages, but not for severity of mental illness, which may be a serious confounder.
Third trimester exposure to benzodiazepines may be associated with withdrawal symptoms in infants. Symptoms of benzodiazepine withdrawal in the neonate are usually not serious and easily manageable; they include mild sedation, hypotonia, reluctance to suck, apnea, cyanosis, and temperature dysregulation [100]. As with PNAS, discontinuing benzodiazepines during the third trimester may reduce this risk, but could worsen anxiety symptoms in the postpartum period.
Maternal Risks
There do not appear to be risks for the mother associated with benzodiazepine use that is unique to the pregnancy state.
Antipsychotics
Though primarily indicated in psychotic and bipolar disorders, antipsychotics are often prescribed as augmentation agents for difficult to treat depression and anxiety. In one British primary care cohort, not limited to pregnant patients, 57 % of quetiapine prescriptions were coded for diagnoses other than serious mental illness, of which 20 % were for anxiety and 35 % for depression [101]. It is important to note that there has been little systematic investigation into the teratogenic effects of antipsychotic medications on the fetus, and as in depression, many studies do not account for the risk posed by having a serious mental health disorder, which increases risk of a host of adverse outcomes [102]. Further, there are very limited data available on the use of long-acting injectable antipsychotics in pregnancy [103], and data are still emerging on newer second-generation antipsychotics, such as aripiprazole and paliperidone [104, 105].
Pregnancy Loss
There is no current evidence that antipsychotics increase risk of spontaneous abortion or intrauterine fetal death.
Physical Malformations
A comprehensive literature review found no association between use of first- or second-generation antipsychotics during pregnancy and major structural malformations [106]. Some recent studies have shown a small absolute increased risk for major malformations following second-generation antipsychotic exposure when controlling for risk factors for major malformations, but not for psychiatric illness (adjusted OR 2.17, 1.20–3.91, 9.3 % exposed vs. 6.4 % unexposed [107]; adjusted OR 1.44, 0.94–2.22, 6.1 % exposed vs. 4.5 % exposed [108]).
Growth Impairment
Much of the existing data regarding the association between antipsychotics and low birth weight are conflicting and ambiguous [108–112]. Atypical antipsychotics are well known to be linked to metabolic syndrome, which is of special concern in pregnancy in that diabetes during pregnancy is associated with infants who are large for gestational age (LGA). A recent Swedish registry-based study did find an association between antipsychotic use and large head circumference, but not LGA, in a group of patients prescribed either clozapine or olanzapine, after adjusting for risk factors for LGA, including early pregnancy BMI, smoking, and diabetes (OR 3.02, 1.60–5.71) [102].
Behavioral Teratogenicity
Data evaluating the long-term outcomes following antipsychotic exposure in pregnancy is currently lacking. One study indicated that babies exposed to antipsychotics antenatally score lower on a measure of child development at 2 months [109]. Another study suggested that infants exposed to antipsychotics in utero demonstrated impairment on a test of neuromotor development at 6 months [113].
Neonatal Toxicity
As of 2011, the antipsychotics carry an FDA label for risk of neonatal extrapyramidal symptoms at birth and withdrawal symptoms. This caution was based on a small number of safety reports to the FDA. A recent prospective cohort study demonstrated a 15 % rate of withdrawal symptoms, which some babies had for up to 6–8 weeks, and which was associated (though not statistically significant) with higher doses of antipsychotics [114].
Antipsychotics have also been associated with a higher rate of preterm birth and shortened gestational age in multiple studies [104, 108, 115, 116], though a recent large cohort study did not find that the association was statistically significant after adjusting for confounding risk factors [117]. Of note, a prospective cohort study comparing women treated with typical versus atypical antipsychotics with controls found that the rate of preterm birth was increased only for the group treated with typical antipsychotics [107]. The authors did observe, however, that there was a higher incidence of treatment with antidepressants in the typical relative to the atypical antipsychotic cohort, which may confound the results.
That said, a recent large meta-analysis, including 6289 antipsychotic-exposed and 1,618,039 unexposed pregnancies, found an increased rate of preterm birth (absolute risk increase 0.03 %), low birth weight (weighted mean difference of 57.89 g), SGA (absolute risk increase 0.05 %), and no increased risk of LGA [118]. It must be emphasized that the authors noted that limited adjustment was possible given the studies included.
Maternal Risks
As previously indicated, antipsychotic exposure during pregnancy has also been associated gestational diabetes, in addition to cesarean section [102, 108]. The risk of gestational diabetes attributable to antipsychotics is controversial. A recent large matched cohort study did not find an increased risk of gestational diabetes, hypertensive disorders, or venous thromboembolism [117], while a recent descriptive, prospective Australian cohort study found a moderately increased incidence of gestational diabetes and caesarean section in women treated with antipsychotics relative to the national averages, even when adjusted for DSM-IV diagnoses [104].
Neuromodulation
Much of the specific benefit of neuromodulation in pregnancy is the ability to avoid or minimize psychotropic medication and the teratogenic effects thereof. Although ECT does require short-acting sedatives and paralytics [119, 120], hospitalization for initiation of ECT can and should be considered as a treatment option for severe or emergent cases of depression in pregnancy [121]. A recent review suggests that the overall chance of a transient, non-life-threatening adverse event is 10 % for ECT during pregnancy, with the most common events being vaginal bleeding, uterine contractions, abdominal pain, and fetal arrhythmias [122]. Fetal death, major congenital malformations, and preterm birth appear to occur at rates similar to the psychiatric population not receiving ECT.
Vagal nerve stimulation (VNS), the stimulation of the left vagus nerve via surgical placement under anesthesia of a small pulse generator, has been FDA-approved for treatment-resistant depression. A review of case reports suggests that this may be viable alternative to medication, though little is known about the specific risk of VNS during pregnancy [122]. Transcranial magnetic stimulation (TMS) refers to the application of focal magnetic pulses to the dorsolateral prefrontal cortex for 15–45 min a day, 5 days a week, for 4–6 weeks. Case series have shown feasibility and safety in the treatment of depressive symptoms in pregnancy, but randomized controlled trials are needed for efficacy [122]. Supine hypotensive syndrome, occurring when the gravid uterus compresses the inferior vena cava (IVC) as the pregnant woman is supine, may cause symptoms of pallor, dizziness, hypotension, and tachycardia that resolve with position change [123]. For TMS devices that require the patient be in the supine position, the supine hypotensive syndrome may be prevented by positioning the patient with a right-sided wedge cushion to reduce the pressure on the IVC. Other risks of TMS in pregnancy have yet to be elucidated; though in one follow-up study, the offspring of women treated with TMS during pregnancy were perceived by their mothers to have a language delay, no objective delay was documented similar to that observed in the offspring of untreated mothers [124]. Other major drawbacks to TMS include the time and financial costs of treatment, though treatments are now covered by some health insurances.
Psychotherapy
A major appeal of psychotherapy is the ability to avoid pharmacotherapy, and it is perhaps for this reason that perinatal women tend to prefer psychotherapy to medication [125]. Psychotherapy has been recommended as the first-line treatment for women with mild illness during pregnancy and psychotherapy plus medication for women with moderate to severe illness [126]. Interpersonal therapy, a time-limited therapy focusing on relational contributors to mental health, has nearly two decades worth of research supporting its efficacy in the treatment of antepartum depression across a range of sociodemographic groups as well as individual and group settings [127]. More recently, cognitive behavioral therapy has also been identified as effective for both the treatment and prevention of perinatal depression, with individual treatment more effective than group treatment [128]. Commonly cited disadvantages to psychotherapy during pregnancy include time, transportation, and lack of access to childcare, as well as instances in which a woman’s illness is so severe that she is unable to fully participate in and benefit from psychotherapy [129].
Conclusions
In summary, the treatment of depression and/or anxiety during pregnancy requires a careful and collaborative weighing of the risks and benefits of treatment options versus the illness itself by both patient and provider. Medications for depression and anxiety can be prescribed during pregnancy, but may carry with them small risks of pregnancy loss, physical malformations, growth impairment and pre-term birth, neonatal toxicity, behavioral teratogenicity, and risks to the mother unique to pregnancy. Other factors, including the severity of illness, the patient’s functional impairment, the risk of illness relapse, and the patient’s preferences, must also be taken into consideration for what may be the patient’s first parenting decision. To further complicate matters, interpreting the broad and conflicting available database is limited by parsing out the individual contributions of treatment and illness. Although there is an extensive literature on the risks of antidepressants in pregnancy, there are as yet no randomized control trials evaluating the efficacy of these medications in pregnancy, and the data on the risks of antipsychotics and benzodiazepines are globally lacking.
We encourage clinicians to adapt Wisner’s model to facilitate this complex and fraught decision-making and informed consent process. We also offer the following specific recommendations regarding treatment informed by this review and our clinical experience:
-
1.
Clinicians should tailor recommendations to the patient’s fears, concerns, preferences, and goals, which should be elicited as part of the history-taking process. Equal weight should be given to the benefit–risk profile of the treatment and that of not treating the illness, including relapse, suicide, and infanticide.
-
2.
If a patient prefers to avoid medication, psychotherapy is most appropriate as primary treatment for mild to moderate illness and neuromodulation for more severe or life-threatening illness.
-
3.
Clinicians may first decide what medication they would recommend if the patient were not pregnant, including medications the patient is currently taking. This helps to clarify the thought and decision making process.
-
4.
It is important to document all exposures to medications and other substances with the potential to impact fetal development as well as to choose medication with the greatest amount of research regarding efficacy and adverse effects in this population [130].
-
5.
Clinicians should aim to prescribe the lowest dose possible while ensuring that the dose is significant enough to achieve a tangible therapeutic effect [131]. Otherwise, the fetus risks exposure to both disease state and medication.
-
6.
Similarly, when possible, monotherapy is preferable to polytherapy [132].
-
7.
The tapering of medication in the weeks prior to delivery is not recommended given the little evidence that it will alleviate the risk of neonatal toxicity or withdrawal and may induce a worsening or relapse of the patient’s symptoms in the postpartum period.
-
8.
Collaboration with an accepting and knowledgeable obstetrician is paramount, particularly as some women may require alternative monitoring during pregnancy.
-
9.
Because pregnant women with psychiatric illnesses have an elevated rate of unhealthy lifestyle behaviors, and these behaviors may influence pregnancy outcomes, a routine part of psychiatric care should also include support, guidance, and counseling on smoking cessation, healthy eating, and exercise.
-
10.
It may be helpful to remind oneself and the patient that no pregnancy is “risk-free,” but an emotionally healthy mother is more resilient and more able and available to deal with any unexpected outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Howard LM, Molyneaux E, Dennis C-L, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384:1775–88.
Peterson I, Gilbert RE, Evans SJ, Man SL, Nazareth I. Pregnancy as a major determinant for discontinuation of antidepressants: an analysis of data from The Health Improvement Network. J Clin Psychiatry. 2011;72:979–85.
Hanley GE, Mintzes B. Patterns of psychotropic medication use in pregnancy in the United States from 2006 to 2011 among women with private insurance. BMC Pregnancy Childbirth. 2014;14:242.
Solomon A. The secret sadness of depression. N Y Times Mag. 2015.
Walton GD, Ross LE, Stewart DE, Grigoriadis S, Dennis C, Vigod S. Decisional conflict among women considering antidepressant medication use in pregnancy. Arch Womens Ment Health. 2014;17:493–501.
Wisner KL, Zarin DA, Holmboe ES, Appelbaum PS, Gelenberg AJ, Leonard HL, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157:1933–40.
American Psychiatric Association: Practice Guideline for the Treatment of Patients with Panic Disorder. 2009. www.psychiatryonline.org/guidelines. Accessed 1 July 2015.
American Psychiatric Association: Practice Guideline for the Treatment of Patients with Obsessive-Compulsive Disorder. 2009. www.psychiatryonline.org/guidelines. Accessed 1 July 2015.
American Psychiatric Association: Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 2009. www.psychiatryonline.org/guidelines. Accessed 1 July 2015.
Cohen LS, Altshuler LL, Harlow BL, Nonacs R, Newport DJ, Viguera AC, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499–507.
Guille C, Epperson CN. Relapse of major depression in women who continue or discontinue antidepressant medication during pregnancy. Am J Psychiatry. 2013;170(5):558.
Buist A, Gotman N, Yonkers KA. Generalized anxiety disorder: course and risk factors in pregnancy. J Affect Disord. 2011;131:277–83.
Russell EJ, Fawcett JM, Mazmanian D. Risk of obsessive-compulsive disorder in pregnant and postpartum women: a meta-analysis. J Clin Psychiatry. 2013;74(4):377–85.
Guglielmi V, Vulink NC, Denys D, Wang Y, Samuels JF, Nestadt G. Obsessive-compulsive disorder and female reproductive cycle events: results from the OCD and reproduction collaborative study. Depress Anxiety. 2014;31(12):979–87.
Shaw JG, Asch SM, Kimerling R, Frayne SM, Shaw KA, Phibbs CS. Posttraumatic stress disorder and risk of spontaneous preterm birth. Obstet Gynecol. 2014;124(6):1111–9.
Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin J, et al. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014;71(8):897–904. A large prospective cohort study finding that PTSD with comorbid depression is as strong a risk factor for preterm birth as a history of previous preterm birth.
Ding X-X, Wu Y-L, Xu S-J, Zhu R-P, Jia X-M, Zhang S-F, et al. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159(20):103–10.
Kim DR, Sockol LE, Sammel MD, Kelly C, Moseley M, Epperson CN. Elevated risk of adverse obstetric outcomes in pregnant women with depression. Arch Womens Ment Health. 2013;16:475–82. Patients who screen positive for depression on the Edinburg Postnatal Depression Scale are at increased risk for preeclampsia, preterm birth, and low birth weight.
Wisner KL, Bogen DL, Sit D, McShea M, Hughes C, Rizzo D, et al. Does fetal exposure to SSRIs or maternal depression impact fetal growth? Am J Psychiatry. 2013;170(5):485–93.
Wisner KL, Sit DK, Hanusa BH, Moses-Kolko EL, Hunker DF, Perel JM, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009;166(5):577–66.
Khashan AS, Everard C, McCowan LME, Dekker G, Moss-Morris R, Baker PN, et al. Second-trimester maternal distress increases the risk of small for gestational age. Psychol Med. 2014;44(13):2799–810.
Zhang S, Ding Z, Liu H, Chen Z, Wu J, Zhang Y, et al. Association between maternal stress and gestational hypertension/preeclampsia: a meta-analysis. Obstet Gynecol Surv. 2013;68(12):825–34.
Winkel S, Einsle F, Pieper L, Höfler M, Wittchen HU, Martini J. Associations of anxiety disorders, depressive disorders, and body weight with hypertension during pregnancy. Arch Womens Ment Health. 2015;18(3):473–83.
Nulman I, Koren G, Rovet J, Barrera M, Pulver A, Streiner D, et al. Neurodevelopment of children following prenatal exposure to venlafaxine, selective serotonin reuptake inhibitors, or untreated maternal depression. Am J Psychiatry. 2012;169(11):1165–74.
Van der Waerden J, Galéra C, Larroque B, Saurel-Cubizolles MJS, Sutter-Dallay AL, Melchior M. Maternal depression trajectories and children’s behavior at age 5 years. J Paediatr. 2015;45(9):1999–2012. The greatest risk of depression and behavioral problems at age 5 occurs when children are exposed to high levels of maternal depression during the preschool years, but the risk of these symptoms is also increased in children exposed to depression from pregnancy through early childhood, highlighting the risk of allowing major depression to persist in and past the antenatal phase inadequately treated.
Betts KS, Williams GM, Najman JM, Alati R. The relationship between maternal depressive, anxious, and stress symptoms during pregnancy and adult offspring behavioral and emotional problems. Depress Anxiety. 2015;32(2):82–90.
Plant DT, Pariante CM, Sharp D, Pawlby S. Maternal depression during pregnancy and offspring depression in adulthood: role of child maltreatment. Br J Psychiatry. 2015.
Hunter SK, Mendoza JH, D’Anna K, Zerbe GO, McCarthly L, Hoffman C, et al. Antidepressants may mitigate the effects of prenatal maternal anxiety on infant auditory sensory gating. Am J Psychiatry. 2012;169(6):616–24.
Yonkers KA, Blackwell KA, Golver J, Forray A. Antidepressant use in pregnant and postpartum women. Annu Rev Clin Psychol. 2014;10:369–92.
Ross LE, Grigoriadis S, Mamisashvili L, Vonderporten EH, Roerecke M, Rehm J, et al. Selected pregnancy and delivery outcomes after exposure to antidepressant medication: a systematic review and meta-analysis. JAMA Psychiatry. 2013;70(4):436–43. Systematic review and meta-analysis finding that there was no significant association between antidepressant medication exposure and spontaneous abortion. There are statistically significant associations between antidepressants and shorter gestational age and preterm delivery (when compared to all unexposed or only depressed mothers without exposure), lower birth weight (but not when compared to unexposed depressed mothers), and lower Apgar scores at 1 and 5 min.
Johansen RL, Morensen LH, Andersen AM, Hansen AV, Strandberg-Larsen K. Maternal use of selective serotonin reuptake inhibitors and risk of miscarriage—assessing potential biases. Pediatr Perinat Epidemiol. 2015;29(1):72–81. SSRI exposure during pregnancy is associated with a very small increased risk of miscarriage in the first trimester, but not in the second trimester. The risk of first-trimester miscarriage is lower in women who took SSRIs but are not identified as having a diagnosis of depression or anxiety than for women who carry a diagnosis but were not taking an SSRI, suggesting that the association may be due to the mental health disorder itself. Also of note, pregnancies in which an SSRI was used were also marked by unhealthier lifestyle profiles.
Andersen JT, Andersen NL, Horwitz H, Poulsen HE, Jimenez-Solem E. Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage. Obstet Gynecol. 2014;12(4):655–61.
Cunningham FG, Leveno KJ, Bloom SJ, Hauth JC, Rouse DJ, Spong CY. Teratology and medications that affect the fetus. In: Cunningham FG, Leveno KJ, Bloom SJ, Hauth JC, Rouse DJ, Spong CY, editors. Williams obstetrics. New York: McGraw Hill; 2010.
Reis M, Källén B. Delivery outcome after maternal use of antidepressant drugs in pregnancy: an update using Swedish data. Psychol Med. 2010;40(10):1723–33.
Ban L, Gibson JE, West J, Fiaschi L, Sokal R, Smeeth L, et al. Maternal depression, antidepressant prescriptions, and congenital anomaly risk in offspring: a population-based cohort study. BJOG. 2014;121:1471–81.
Jimenez-Solem E, Andersen JT, Petersen M, Boredbaek K, Jensen JK, Afzal S, et al. Exposure to selective serotonin reuptake inhibitors and the risk of congenital malformations: a nationwide cohort study. BMJ Open. 2012;2(3).
Kornum JB, Nielsen RB, Pedersen L, Mortensen PB, Nørgaard M. Use of selective serotonin reuptake inhibitors during early pregnancy and risk of major congenital malformations: updated analysis. J Clin Epidemiol. 2010;2:29–36.
Reefhuis J, Devine O, Friedman JM, Louik C, Honein MA. Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ. 2015;350:h3190.
Grigoriadis S, VonderPorten EH, Mamisashvili L, Roerecke M, Rehm J, Dennis CL, et al. Antidepressant exposure during pregnancy and congenital malformations is there an association? A systematic review and meta-analysis of the best evidence. J Clin Psychiatry. 2013;74(4):e293–308.
Wurst KE, Pool C, Ephross SA, Olshan AF. First trimester paroxetine use and the prevalence of congenital, specifically cardiac, defects: a meta-analysis of epidemiological studies. Birth Defects Res A Clin Mol Teratol. 2010;88(3):159–70.
Malm H, Artama M, Gissler M, Ritvanen A. Selective serotonin reuptake inhibitors and risk for major congenital anomalies. Obstet Gynecol. 2011;118(1):111–20.
Bérard A, Zhao J-P, Sheehy O. Sertraline use during pregnancy and the risk of major malformations. Am J Obstet Gynecol. 2015;212:795.e1–12.
Wemakor A, Casson K, Garne E, Bakker M, Addor MC, Arriola L, et al. Selective serotonin reuptake inhibitor antidepressant use in first trimester pregnancy and risk of specific congenital anomalies: a European register-based study. Eur J Epidemiol. 2015.
Davis RL, Rubanowice D, McPhillips H, Raebel MA, Andrade SE, Smith D, et al. Risks of congenital malformations and perinatal events among infants exposed to antidepressant medications during pregnancy. Pharmacoepidemiol Drug Saf. 2007;16(10):1086–94.
Bellantouno C, Marini A, Lucarelli C. Infant health and neurodevelopmental outcomes following prenatal exposure to duloxetine. Clin Drug Investig. 2013;33(9):685–8.
Hoog SL, Cheng Y, Elpers J, Dowsett SA. Duloxetine and pregnancy outcomes: safety surveillance findings. Int J Med Sci. 2013;10(4):413–9.
Polen KN, Rasmussen SA, Riehle-Colarusso T, Reefhuis J, the National Birth Defects Prevention Study. The association between reported venlafaxine use in early pregnancy and birth defects, national birth defects prevention study, 1997–2007. Birth Defects Res A Clin Mol Teratol. 2013;97(1):28–35.
Källen B, Otterblad Olausson P. Antidepressant drugs during pregnancy and infant congenital heart defect. Reprod Toxicol. 2006;21(3):221–2.
Louik C, Kerr S, Mitchell AA. First-trimester exposure to bupropion and risk of cardiac malformations. Pharmacoepidemiol Drug Saf. 2014;23:1066–75.
Winterfeld U, Klinger G, Panchaud A, Stephens S, Arnon J, Malm H, et al. Pregnancy outcome following maternal exposure to mirtazapine: a multicenter, prospective study. J Clin Psychopharmacol. 2015;35(3):250–9. doi:10.1097/JCP.0000000000000309.
Furu K, Kieler H, Haglund B, Engeland A, Selmer R, Stephansson O, et al. Selective serotonin reuptake inhibitors and venlafaxine in early pregnancy and risk of birth defects: population based cohort study and sibling design. BMJ. 2015;350:h1798.
Huybrechts KF, Palmsten K, Avorn J, Cohen LS, Holmes LB, Franklin JM, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370:2397–407. A large Medicaid data study, finding that the increased risk of cardiac defects following antidepressant exposure vanishes when restricting to mothers with depressive diagnosis and adjusting for known cardiac defect risk factors and proxies for depression severity, including for fluoxetine, paroxetine, bupropion, and TCAs.
Hayes RM, Wu P, Shelton RC, Cooper WO, Dupont WD, Mitchel E, et al. Maternal antidepressant use and adverse outcomes: a cohort study of 228,876 pregnancies. Am J Obstet Gynecol. 2012;207(1):49.e1–9.
Nordeng H, Spigset O. Treatment with selective serotonin reuptake inhibitors in the third trimester of pregnancy: effects on the infant. Drug Saf. 2005;28(7):565–81.
Oberlander TF, Warburton W, Misri S, Riggs W, Aghajanian J, Hertzman C. Major congenital malformations following prenatal exposure to serotonin reuptake inhibitors and benzodiazepines using population-based health data. Birth Defects Res B Dev Reprod Toxicol. 2008;83(1):68–76.
Ramos E, St-André M, Bérard A. Association between antidepressant use during pregnancy and infants born small for gestational age. Can J Psychiatry. 2010;55(10):643–52.
Chun-Fai-Chan B, Joren G, Fayez I, Kalra S, Voyer-Lavigne S, Boshier A, et al. Pregnancy outcomes of women exposed to bupropion during pregnancy: a prospective outcome study. Am J Obstet Gynecol. 2005;192(3):932–6.
Austin MP, Karatas JC, Mishra P, Christl B, Kennedy D, Oei J. Infant neurodevelopment following in utero exposure to antidepressant medication. Actual Pediatr. 2013;102(11):1054–9.
Nulman I, Rovet J, Stewart DE, Wolpin J, Gardner HA, Theis JG, et al. Neurodevelopment of children exposed in utero to antidepressant drugs. N Engl J Med. 1997;336(4):258–62.
Nulman I, Rovet J, Stewart DE, Wolpin J, Pace-Asciak P, Shuhaiber S, et al. Child development following exposure to tricyclic antidepressants or fluoxetine throughout fetal life: a prospective, controlled study. Am J Psychiatry. 2002;159(11):1889–95.
Skurtveit S, Selmer R, Roth C, Hernandez-Diaz S, Handal M. Prenatal exposure to antidepressants and language competence at age three: results from a large population-based pregnancy cohort in Norway. BJOG. 2014;121:1621–32.
Suri R, Lin AS, Cohen LS, Altshuler LL. Acute and long-term behavioral outcomes of infants and children exposed in utero to either maternal depression or antidepressants: a review of the literature. J Clin Psychiatry. 2014;75(10):e1142–52.
Santucci AK, Singer LT, Wisniewski SR, Luther JF, Eng HF, Dills JL, et al. Impact of prenatal exposure to serotonin reuptake inhibitors or maternal major depressive disorder on infant development outcomes. J Clin Psychiatry. 2014;75(10):1088–95.
Hanley GE, Brain U, Oberlander TF. Prenatal exposure to serotonin reuptake inhibitor antidepressants and childhood behavior. Pediatr Res. 2015. doi:10.1038/pr.2015.77.
Brandlistuen RE, Ystrom E, Eberhard-Gran M, Nulman I, Koren G, Nordeng H. Behavioural effects of fetal antidepressant exposure in a Norwegian cohort of discordant siblings. Int J Epidemiol. 2015.
Croen LA, Grether JK, Yoshida CK, Odouli R, Hendrick V. Antidepressant use during pregnancy and childhood autism spectrum disorders. Arch Gen Psychiatry. 2011;68(11):1104–12.
Rai D, Lee BK, Dalman C, Golding J, Lewis G, Magnusson C. Prenatal depression, maternal antidepressant use during pregnancy, and risk of autism spectrum disorders: population based case–control study. BMJ. 2013;346:f2059.
Sørensen MJ, Grønborg TK, Christensen J, Parner ET, Vestergaard M, Schendel D, et al. Antidepressant exposure in pregnancy and risk of autism spectrum disorders. J Clin Epidemiol. 2013;5:449–59.
Clements CC, Castro VM, Blumenthal SR, Rosenfield HR, Murphy SN, Fava M, et al. Prenatal antidepressant exposure is associated with risk for attention-deficit hyperactivity disorder but not autism spectrum disorder in a large health system. Mol Psychiatry. 2015;20(6):727–34. Large retrospective cohort study which did not find an association with prenatal antidepressants and autism spectrum disorder, but did indicate an increased risk of attention-deficit/hyperactivity disorder.
March of Dimes. www.marchofdimes.org. Accessed 3 August 2015.
Center for Disease Control. 2014. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.html. Accessed 1 July 2015.
Colvin L, Slack-Smith L, Stanley FJ, Bower C. Dispensing patterns and pregnancy outcomes for women dispensed selective serotonin reuptake inhibitors in pregnancy. Birth Defects Res A Clin Mol Teratol. 2011;91(3):142–52.
Sahingöz M, Yuskel G, Karsidag C, Uguz F, Sonmez E, Annagur BB, et al. Birth weight and preterm birth in babies of pregnant women with major depression in relation to treatment with antidepressants. J Clin Psychopharmacol. 2014;34:226–9.
Chambers CD, Hernandez-Diaz S, Van Marter LJ, Werler MM, Louik C, Jones KL, et al. Selective serotonin-reuptake inhibitors and risk of persistent pulmonary hypertension of the newborn. N Engl J Med. 2006;9(6):579–87.
Walsh-Sukys MC, Tyson JE, Wright LL, Bauer CR, Korones SB, Stevenson DK, et al. Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics. 2000;105(1 Pt 1):14–20.
Grigoriadis S, Vonderporten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, et al. Prenatal exposure to antidepressants and persistent pulmonary hypertension of the newborn: systematic review and meta-analysis. BMJ. 2014;348:f6932.
Huybrechts KF, Bateman BT, Palmsten K, Desai RJ, Patorno E, Gopalakrishnan C, et al. Antidepressant use late in pregnancy and risk of persistent pulmonary hypertension of the newborn. JAMA. 2015;313(21):2142–51. Large Medicaid cohort study finding that the odds ratio adjusted for depression for primary PPHN for women taking SSRIs is only slightly elevated and of borderline significance (OR = 1.28, 1.01–1.64) relative to unexposed pregnancies and is not significantly elevated for non-SSRI antidepressants.
Food and Drug Administration. FDA Drug Safety Communication: selective serotonin reuptake inhibitor (SSRI) antidepressant use during pregnancy and reports of a rare heart and lung condition in newborn babies. 2011. http://www.fda.gov/Drugs/DrugSafety/ucm283375.htm. Accessed 13 August 2015.
Koren G, Finkelstein Y, Matsui D, Berkovich M. Diagnosis and management of poor neonatal adaptation syndrome in newborns exposed in utero to selective serotonin/norepinephrine reuptake inhibitors. J Obstet Gynaecol Can. 2009;31(4):348–50.
Forsberg L, Navér L, Gustafsson LL, Wide K. Neonatal adaptation in infants prenatally exposed to antidepressants—clinical monitoring using neonatal abstinence score. PLoS ONE. 2014;2014(9):11–e111327. doi:10.1371/journal.pone.0111327.
Kieviet N, Dolman KM, Honig A. The use of psychotropic medication during pregnancy: how about the newborn? Neuropsychiatr Dis Treat. 2013;9:1257–66.
Smit M, Wennik HJMB, Heres MMHB, Dolman KKM, Honig A. Mirtazapine in pregnancy and lactation: data from a case series. J Clin Psychopharmacol. 2015;35:163–7.
Javors MA, Houston JP, Tekell JL, Brannan SK, Frazer A. Reduction of platelet serotonin content in depressed patients treated with either paroxetine or desipramine. Int J Neuropsychopharmacol. 2000;3(3):229–35.
Palmsten K, Hernández-Díaz S, Huybrechts KF, Willams PL, Michels KB, Achtyes ED, et al. Use of antidepressants near delivery and risk of postpartum hemorrhage: cohort study of low income women in the United States. BMJ. 2013;347:f4877.
Lupattelli A, Spigset O, Koren G, Nordeng H. Risk of vaginal bleeding and postpartum hemorrhage after use of antidepressants in pregnancy: a study from the Norwegian Mother and Child Cohort Study. J Clin Psychopharmacol. 2014;34(1):143–8.
Salkeld E, Ferris LE, Juurlink DN. The risk of postpartum hemorrhage with selective serotonin reuptake inhibitors and other antidepressants. J Clin Psychopharmacol. 2008;28(2):230–4.
De Vera MA, Bérard A. Antidepressant use during pregnancy and the risk of pregnancy-induced hypertension. Br J Clin Pharmacol. 2012;74(2):362–9.
Toh S, Mitchell AA, Louik C, Werler MM, Chambers CD, Hernández-Díaz S. Antidepressant use during pregnancy and the risk of preterm delivery and fetal growth restriction. J Clin Psychopharmacol. 2009;29(6):555–60.
Grzeskowiak LE, Pedersen LH, Morrison JL. Antidepressant use and gestational hypertension: does evidence support causality? Br J Clin Pharmacol. 2013;75(5):1373–4.
Lalic-Popovic M, Paunkovic J, Grujic Z, Golocorbin-Kon S, Al-Salami H, Mikov M. Diabetes and hypertension increase the placental and transcellular permeation of the lipophilic drug diazepam in pregnant women. BMC Pregnancy Childbirth. 2013;13:188.
Bellantuono C, Tofani S, Di Sciascio G, Santone G. Benzodiazepine exposure in pregnancy and risk of major malformations: a critical overview. Gen Hosp Psychiatry. 2013;35(1):3–8.
Tasci Y, Demir B, Dilbaz S, Haberal A. Use of diazepam for hyperemesis gravidarum. J Matern Fetal Neonatal Med. 2009;22(4):353–6.
Dolovich LR, Addis A, Vaillancourt JM, Power JD, Joren G, Einarson TR. Benzodiazepine use in pregnancy and major malformations or oral cleft: meta-analysis of cohort and case–control studies. BMJ. 1998;317(7162):839–43.
Reis M, Källén B. Combined use of selective serotonin reuptake inhibitors and sedatives/hypnotics during pregnancy: risk of relatively severe congenital malformations or cardiac defects. A register study. BMJ Open. 2013;3(2).
Ban L, West J, Gibson JE, Fiaschi L, Sokal R, Doyle P, et al. First trimester exposure to anxiolytic and hypnotic drugs and the risks of major congenital anomalies: a United Kingdom population-based cohort study. PLoS ONE. 2014;9(6), e100996. doi:10.1371/journal.pone.0100996.
Wikner BN, Stiller C-O, Bergman U, Asker C, Källén B. Use of benzodiazepines and benzodiazepine receptor antagonists during pregnancy: neonatal outcome and congenital malformations. Pharmacoepidemiol Drug Saf. 2007;166:1203–10.
Marroun HE, White T, Verhulst FC, Tiemeier H. Maternal use of antidepressant or anxiolytic medication during pregnancy and childhood neurodevelopmental outcomes: a systematic review. Eur Child Adolesc Psychiatry. 2014;23:973–92.
Stika L, Elisova K, Honzakova L, Hrochova H, Pelchatova H, Strnadova J, et al. Effects of drug administration in pregnancy on children’s school behavior. Pharm Weekbl Sci. 1990;12:252–5.
Källén B, Reis M. Neonatal complications after maternal concomitant use of SSRI and other central nervous system active drugs during the second or third trimester of pregnancy. J Clin Psychopharmacol. 2012;32(5):608–14.
March D, Yonkers KA. Panic disorder. In: Yonkers KA, Little BB, editors. Management of psychiatric disorders in pregnancy. London: Arnold; 2001. p. 134–48.
Marston L, Nazareth I, Petersen I, et al. Prescribing of antipsychotics in UK primary care: a cohort study. BMJ Open. 2014;4, e006135. doi:10.1136/bmjopen-2014-006135.
Bodén R, Lundgren M, Brandt L, Reutfors J, Kieler H. Antipsychotics during pregnancy: relation to fetal and maternal metabolic effects. Arch Gen Psychiatry. 2012;69(7):715–21.
Kim SW, Kim KM, Kim JM, Shin IS, Shin HY, Yang SJ, et al. Use of long-acting injectable risperidone before and throughout pregnancy in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(2):543–5.
Windhager E, Kim SW, Saria A, Zauner K, Amminger PG, Klier CM. Perinatal use of aripiprazole: plasma levels, placenta transfer, and child outcome in 3 new cases. J Clin Psychopharmacol. 2014;34:637–41.
Özdemir A, Pak S, Canan F, Geçici Ö, Kuloglu M, Gücer M. Paliperidone palmitate use in pregnancy in a woman with schizophrenia. Arch Womens Ment Health. 2015. doi:10.1007/s00737-014-0496-6.
Einarson A, Boskovic R. Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract. 2009;15(3):183–92.
Habermann F, Fritzsche J, Fuhlbrück F, Wacker E, Allignol A, Weber-Schoendorfer C, et al. Atypical antipsychotic drugs and pregnancy outcome: a prospective, cohort study. J Clin Psychopharmacol. 2013;33(4):453–62.
Reis M, Källén B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J Clin Psychopharmacol. 2008;28(3):279–88.
Peng M, Gao K, Ding Y, Ou J, Calabrese JR, Wu R, et al. Effects of prenatal exposure to atypical antipsychotics on postnatal development and growth of infants: a case-controlled, prospective study. Psychopharmacology (Berlin). 2013;228(4):577–84.
Babu GN, Desai G, Tippeswamy H, Chandra PS. Birth weight and use of olanzapine in pregnancy: a prospective comparative study. J Clin Psychopharmacol. 2010;30(3):331–2.
Lin HC, Chen IJ, Chen YH, Lee HC, Wu FJ. Maternal schizophrenia and pregnancy outcome: does the use of antipsychotics make a difference? Schizophr Res. 2010;116(1):55–60.
Sutter-Dallay A-L, Bales M, Pambrun E, Glangeaud-Freudenthal NM-C, Wisner KL, Verdoux H. Impact of prenatal exposure to psychotropic drugs on neonatal outcome in infants of mothers with serious psychiatric illnesses. J Clin Psychiatry. 2015;76(7):967–73.
Johnson KC, LaPrairie JL, Brennan PA, Stowe ZN, Newport DJ. Prenatal antipsychotic exposure and neuromotor performance during infancy. Arch Gen Psychiatry. 2012;69(8):787–94.
Kulkarni J, Worsley R, Gilbert H, Gavrilidis E, Van Rheenen TE, Wang W, et al. A prospective cohort study of antipsychotic medications in pregnancy: the first 147 pregnancies and 100 one year old babies. PLoS ONE. 2014;9(5), e94788. doi:10.1371/journal.pone.0094788.
Wichman CL. Atypical antipsychotic use in pregnancy: a retrospective review. Arch Womens Ment Health. 2009;12(1):53–7.
Sadowski A, Todorow M, Yazdani Brojeni P, Koren G, Nulman I. Pregnancy outcomes following maternal exposure to second-generation antipsychotics given with other psychotropic drugs: a cohort study. BMJ Open. 2013;3, e003062. doi:10.1136/bmjopen-2013-003062.
Vigod SN, Gomes T, Wilton AS, Taylor VH, Ray JG. Antipsychotic drug use in pregnancy: high dimensional, propensity matched, population based cohort study. BMJ. 2015;350:h2298.
Coughlin CG, Blackwell KA, Barley C, Hay M, Yonkers KA, Bloch MH. Obstetric and neonatal outcomes after antipsychotic medication exposure in pregnancy. Obstet Gynecol. 2015;125(5):1224–35.
Lihua P, Su M, Ke W, Ziemann-Gimmel P. Different regimens of intravenous sedatives or hypnotics for electroconvulsive therapy (ECT) in adult patients with depression. Cochrane Database Syst Rev. 2014;4, CD009763.
Mizrakhani H, Welch CA, Eikermann M, Nozari A. Neuromuscular blocking agents for electroconvulsive therapy: a systematic review. Acta Aneaesthesiol Scand. 2012;56(1):3–16.
O’Reardon JP, Cristancho MA, von Andreae CV, Cristancho P, Weiss D. Acute and maintenance electroconvulsive therapy for treatment of severe major depression during the second and third trimesters of pregnancy with infant follow-up to 18 months: case report and review of the literature. J ECT. 2011;27:e23–6.
Kim DR, Snell JL, Ewing GC, O’Reardon J. Neuromodulation and antenatal depression: a review. Neuropsychiatr Dis Treat. 2015;11:975–82.
Kim DR, Wang W. Prevention of supine hypotensive syndrome in pregnant women treated with transcranial magnetic stimulation. Psychiatry Res. 2014;218(1–2):247–8.
Eryilmaz G, Hizli Sayar G, Ozten E, Gogcegoz Gul I, Yorbik O, Isiten N, et al. Follow-up study of children whose mothers were treated with transcranial magnetic stimulation during pregnancy: preliminary results. Neuromodulation. 2015;18(4):255–60.
Pearlstein TB, Zlotnick C, Battle CL, Stuart S, O’Hara MW, Price AB, et al. Patient choice of treatment for postpartum depression: a pilot study. Arch Womens Ment Health. 2006;9:303–8.
Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, et al. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen Hosp Psychiatry. 2009;31(5):403–13.
Wenzel A, Stuart S, Koleva H. Psychotherapy for psychopathology during pregnancy and the postpartum period. . 2015.
Sockol LE. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J Affect Disord. 2015;177:7–21.
Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36(1):60–9.
Nonacs RM, Cohen LS, Viguera AC, Mogielnick J. Diagnosis and treatment of mood and anxiety disorders in pregnancy. In: Cohen LS, Nonacs RM, editors. Mood and anxiety disorders during pregnancy and postpartum, Review of psychiatry, vol. 24. 4th ed. Washington DC: American Psychiatric Publishing; 2005. p. 17–51.
Galbally M, Snellen M, Power J. Antipsychotic drugs in pregnancy: a review of their maternal and fetal effects. Ther Adv Drug Saf. 2014;5(2):100–9.
Birndorf CA, Sacks AC. To medicate or not: the dilemma of pregnancy and psychiatric illness. In: Stone SD, Menken AE, editors. Perinatal and postpartum mood disorders: perspectives and treatment guide for the health care practitioner. New York: Springer; 2008. p. 237–65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Katharine Baratz Dalke, Amy Wenzel, and Deborah R. Kim declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Women’s Mental Health
Rights and permissions
About this article
Cite this article
Dalke, K.B., Wenzel, A. & Kim, D.R. Depression and Anxiety During Pregnancy: Evaluating the Literature in Support of Clinical Risk-Benefit Decision-Making. Curr Psychiatry Rep 18, 59 (2016). https://doi.org/10.1007/s11920-016-0698-x
Published:
DOI: https://doi.org/10.1007/s11920-016-0698-x