Abstract
The immediate postpartum period is a time of acute vulnerability to mental illness, which presents unique challenges for the psychiatric consultant. Because the postpartum hospital stay is typically brief, the consultant must have a working knowledge of postpartum physiology and the myriad forms of mental illness that may emerge in this vulnerable time, in order to quickly make a diagnosis and formulate a treatment plan. This review aims to characterize the most common reasons for postpartum consultation, review postpartum physiology and psychiatric conditions, and propose an evidence-based, practical approach to treatment. A literature search using the terms “postpartum,” “obstetric,” “consultation,” and “psychiatry” yielded six studies that identified reasons for psychiatric consultation to the obstetrics and gynecology services. These studies informed the structure of the article such that we review the most common reasons for consultation and how to approach each issue. The most common reason for consultation is past psychiatric history, often in the absence of current symptoms. For each clinical situation, including depression, adverse birth events, and psychosis, we present a differential diagnosis, as well as risk factors, clinical signs, and recommended treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The inpatient psychiatric consultant sees a diverse population of patients. Uniquely, consultation to the postpartum obstetric patient must consider two patients, the mother and her infant. Since caring for a newborn requires a substantial level of psychological functioning, the psychiatric assessment of the new mother includes observation of her behavior with the infant. Increased psychiatric vulnerability, maternal capacity, and the choice of psychiatric treatment during breastfeeding are concerns specific to the postpartum woman. The consultant most often only has one visit in which to answer the explicit and implicit questions from the primary team [1], necessitating familiarity with the intricacies of a postpartum obstetric consultation. In this clinical practice article, we translate the most common reasons for obstetric consultation into the potential areas of concern underlying them and provide a practical approach to differential diagnosis and treatment.
Reasons for Consultation
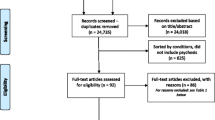
We conducted a search of the literature in PubMed and Ovid and Web of Science, with combinations of the search terms “postpartum,” “obstetric,” “consultation,” and “psychiatry,” excluding articles not written in English. Six retrospective chart reviews list the most commonly stated reasons for inpatient psychiatric consultation to obstetric patients, four of which only included obstetric patients [2–5] and two that included both obstetric and gynecologic patients [6, 7]. In the latter articles, the gynecologic patients were not postpartum women and the authors did not specify what percentage of their population was obstetric. In the former articles, none of the four chart reviews that focused solely on obstetric patients differentiated between antepartum and postpartum patients when listing frequencies of reasons for consultation; however, two of the four [3, 4] indicated that a majority of consultations were for postpartum patients. One other retrospective chart review [8] described diagnoses and interventions, but not reasons for consultation, so it is not included in our table. Because these studies differed in terminology, we provide consolidated groupings of the reasons for consultation (Table 1).
Across studies, as expected, current psychiatric symptoms was a common reason for psychiatric consultation to the obstetrics and gynecology services but, less predictably, so was a past psychiatric history (PPH) without current symptoms. In a retrospective chart review of 96 patients in a Canadian tertiary hospital with a high-risk pregnancy service, the most frequent reason for referral was a report of PPH specifically “because they were deemed to be at risk of postpartum depression” [4]. That study is supported by the results of an abstract (n = 165) which found that 42 % of all psychiatric consultations from the obstetric service were for PPH alone, without current psychiatric symptoms [1]. A retrospective chart review of 90 obstetric patients in an Australian teaching hospital reported “postpartum condition,” depression, and problems coping as the most frequent reasons for consultation [2]. A larger Australian chart review (n = 892) of maternity inpatients at an urban women’s hospital found depression to be the most common reason for consultation (48.7 %), closely followed by PPH (47.9 %) [3]. The same results were found by both reviews of consultations to combined obstetrics and gynecology services, one of which studied 55 Italian inpatients [6], the other of which reported on 111 inpatients in a Taiwanese university hospital [7]—consultation for depression was followed closely by PPH. Only one study of Taiwanese obstetric inpatients (n = 28) found that anxiety was the most common reason for referral [5]. Where a current psychiatric disorder was diagnosed, mood disorders were the most common diagnosis type [1, 3, 4, 7]. Uncommon reasons for consultation included pain [2] and patient request for consultation [2, 6].
Past Psychiatric History and Maternal Capacity
Underlying many of the consults to psychiatry for postpartum mothers, especially those for patients without current symptoms, is the question of maternal capacity, or the ability of the new mother to care for her newborn. Carrying a psychiatric diagnosis may lead others to view a patient’s parental fitness more critically [9]. Assessment of maternal capacity carries the opposing outcomes of putting a vulnerable newborn in harm’s way or of needlessly separating mother and infant. Although there are no published guidelines that address assessment of parental capacity [10], the generally accepted standard is minimal capacity, not optimal parenting [9, 11].
Key to assessment of maternal capacity is the psychiatric consultant’s observation of the mother’s behavior with the child and staff observations of the mother’s behavior. A patient may have a history of schizophrenia and even endorse current hallucinations, but if her behavior is organized and she is appropriately attentive and gentle with her newborn, she may well have the capacity to take care of her baby. Conversely, if the nurses observe the mother handling her infant in a rough or careless fashion, that indicates impaired maternal capacity.
Also, consider the mother’s attitude toward the pregnancy and baby. A positive attitude toward the baby and having prepared for the baby’s arrival are good indicators of motivation to provide care, whereas lack of interest in or hostility toward the baby, especially in the setting of prior abuse, or having other children removed by child welfare authorities, signals a higher risk of a poor outcome [11].
We recommend that the consultant take the following steps [9, 11, 12]: (1) observe the mother’s behavior with her infant; (2) ask her and her partner about her attitude toward the pregnancy; (3) obtain social history, including current stressors and supports; (4) assess the patient’s family, especially for members who could monitor the mother and/or take over primary caretaking of the infant if necessary, and (5) ascertain the mother’s level of insight into her psychiatric illness, as low insight would prompt more intervention. If she is deemed to lack maternal capacity, the state child welfare services should be contacted to arrange for a safe discharge plan for the infant.
Current Depression Symptoms
In evaluating current depressive symptoms, the consultant must differentiate between maternity blues, which occurs in 50–80 % of mothers [13–16], and postpartum depression (PPD), because while the blues is self-limited, untreated PPD can have devastating sequelae. The negative effects of PPD on the child and mother are more thoroughly reviewed elsewhere [17–19] but include adverse birth outcomes [20, 21], impairments in the child’s growth, attachment, and cognitive and emotional development and elevated risk of suicide in the mother. Furthermore, PPD is associated with increased child abuse, neglect, and filicide of the older child [22].
The diagnostic criteria for PPD are the same as major depressive disorder. In the Diagnostic and Statistical Manual of Mental Disorders (DSM)-V, the specifier of “with peripartum onset” is applied “if onset of mood symptoms occurs during pregnancy or in the 4 weeks following delivery” [23]. Previously, in the DSM-IV-TR, this specifier was “with postpartum onset” as defined as “within 4 weeks after childbirth.”[24] This was changed to include pregnancy-onset depressive episodes as it has become more clear that what is called postpartum depression may be a heterogeneous group of biologically distinct entities, only some of which are triggered by parturition.
Accordingly, certain women may be more vulnerable to developing PPD. In a prospective double-blind intervention of euthymic mothers (n = 16), 60 % of women with a history of PPD developed a major depressive episode compared with zero episodes in women without a history when pregnancy hormones were added and withdrawn over a 4-month period [25]. Familial [26, 27] and genotyping [28–30] studies indicate a possible genetic basis for increased risk of depression conferred by childbirth. Finally, the hippocampus is one site where estradiol’s effects on mood are thought to be situated, and a recent study found that DNA methylation modifies the effect of estradiol on certain genes in hippocampal tissue; furthermore, the degree of this methylation is significantly different between PPD and non-depressed mothers [31]. This is likely the first in a line of studies examining the epigenetics of the etiology of PPD.
These differences may underlie a “hormone-sensitive” [32] or “reproductive depression” phenotype, in which some women are more likely to experience depression in context of hormonal changes, be they pre-menstrual, postpartum, or perimenopausal [33]. Late pregnancy and delivery is a time of enormous hormonal flux. Progesterone and estradiol increase up to 8- and 1000-fold respectively during pregnancy [34], then drop to pre-pregnancy levels by day five postpartum [35]. Falling estradiol may affect mood through its effect on serotonin, as it modulates serotonin levels and pre- and postsynaptic serotonin receptor activity [36, 37]. Furthermore, animal studies have demonstrated an inverse relationship between estradiol and MAO-A density [38–40], and, in humans, falling estradiol levels is associated with increased MAO binding in postpartum women [41]. The dramatic hormonal fluctuations that occur in the third trimester and postpartum thus affect neurotransmitter availability, which likely contributes to depressive symptoms before and after delivery. However, since only some women seem to be adversely affected by these typical hormonal changes, future studies should focus on the genetic, hormonal, and neurobiological underpinnings of this putative subtype of PPD.
Because DSM criteria require symptoms to last for at least 2 weeks, the consultant cannot diagnose PPD in those first few days postpartum while the mother is hospitalized, unless a depressive episode began during pregnancy, which happens in one third of PPD cases [42]. However, high-risk women should be identified and monitored. Studies of biomarkers that could predict PPD have produced conflicting results [43–47], so risk assessment must be based on the mother’s clinical presentation and epidemiological risk factors.
Strong risk factors for PPD include a past history of PPD and a history of bipolar disorder, both of which increase the risk of PPD to about 50 %, and a history of pre-menstrual dysphoric disorder [48–53], as well as depressive or anxious symptoms during pregnancy [48]. Moderate risk factors for PPD include primiparity [54], delivering prematurely [52], a family history of depression, stressful life events, perceived lack of social support, unemployment [52], lower education [42], and psychological abuse from the mother’s partner [55], as well as adverse birth outcomes [56].
At the bedside, the consultant should quantify the mother’s degree of depression with a well-validated tool such as the Edinburgh Postnatal Depression Scale (EPDS) [57]. A score of 10 or above is considered at risk for postnatal depression and was noted in days 3–5 postpartum to have a sensitivity of 0.82 for later development of PPD [52, 58]. Apart from the score itself, the presence of depressive symptoms at all should raise concern. One study of postpartum women (n = 594) who completed the EPDS on day 2 postpartum reported that depressive symptoms at 2 days predicted an EPDS score of >9 at 3 months [59].
If the mother does not currently meet criteria for PPD (i.e., did not have onset during pregnancy) but is at increased risk, the consultant should ensure close follow-up. However, giving the patient referral information is not enough. Almost 80 % of women who had screened positive for depression in one study did not show up to their psychiatric follow-up appointment [56], so the psychiatric consultant should ask the outpatient obstetrician to monitor the patient’s mood and encourage psychiatric follow-up. Women with a prior history of PPD should consider beginning an antidepressant preventively, as a randomized controlled trial (RCT) (N = 22) showed the risk of recurrence was 7 % for those taking sertraline vs. 50 % for those taking placebo [60]. PPD risk is also lowered by postpartum home visits by nurses, telephone-based peer support, and interpersonal psychotherapy [61], as well as psychoeducation on modifiable factors associated with PPD (e.g., low social support) and information about how to get help [62].
If the postpartum mother’s symptoms began during pregnancy and she already meets criteria for PPD, the consultant should initiate treatment. Selective serotonin reuptake inhibitors (SSRIs) are first-line but changes in maternal P450 enzyme function necessitate a low starting dose, e.g., the equivalent of sertraline 25 mg daily [63]. Augmentation with benzodiazepines, mood stabilizers, or antipsychotics may be necessary. We do not recommend estrogen therapy at this time, as there is limited current evidence for its use although it may hold promise as a future treatment [64]. Schedule a follow-up appointment with an outpatient psychiatrist, and improve adherence by enlisting the help of the outpatient obstetrician and possibly a family member.
Some psychiatrists base their prescribing decisions for breastfeeding mothers on whether an antidepressant’s milk/plasma ratio is less than 1 and the relative infant dose is under 10 %, in which case the clinician should avoid citalopram, fluoxetine, and venlafaxine [65], unless the patient has a history of positive response to one of these medications. We prefer to base our prescribing decisions on data on in vivo effect of antidepressants on nursing infants, which indicate few adverse outcomes [65, 66]. After medication initiation, the consultant should ask the mother to monitor her infant for irritability, agitation, excessive crying, postfeeding vomiting, or sedation. We recommend against “pumping and dumping” milk, as there is no demonstrated benefit, and this recommendation may send a confusing message about the safety of medication while breastfeeding [63].
Adverse Obstetric Events
Adverse obstetric events and “coping problems” were common reasons for psychiatric consultation. After stillbirth or significant birth injury, shock and numbness is typical, followed by a grief reaction, i.e., bouts of tearfulness, guilt, insomnia, and anxiety. Often, the mother searches for a cause of the death or injury, and anger is mixed with grief in the early weeks of mourning [67]. This presentation is usually not pathologic, but the team may need reassurance that normal grief—either for the baby or for the mother’s expectation of a completely healthy baby—is occurring without need for any intervention beyond an assessment of the mother’s social supports.
Intervention may be needed if a mother is at risk for prolonged symptoms, since adverse obstetric events can be a risk factor for PPD [56], unresolved grief as measured by the Adult Attachment Interview [68], GAD [69], social phobia [69], and posttraumatic stress disorder (PTSD) [70–72]. Unresolved grief for a previous baby, which is sometimes manifested by the maintenance of an ongoing dialogue with the deceased child, was significantly associated with disorganized attachment in a subsequently born child at age 12 months [68]. Risk factors for unresolved grief include lack of social support and low intimacy with the baby’s father [67].
Although acute stress reactions can be seen after an adverse birth outcome, symptoms usually remit. The question of whether the mother should see and hold the stillborn baby’s body has not been firmly answered [73–75]. We recommend presenting the mother with the option of seeing the baby in an unbiased, nonjudgmental fashion [76–78] and to respect the mother’s wishes for how to cope with the loss. If the baby is deformed or anencephalic, warn the mother that seeing the baby may be distressing. If the psychiatric consultant remembers that she is treating a mother who has lost her child, she can avoid common mistakes such as reassuring her that she can have other children or forgetting to ask important questions such as whether the mother is planning on having a service for her child, whether she decided to name her child or whether an autopsy was requested.
There are no clear guidelines for psychiatric intervention [79], but in one RCT of care for parents grieving after pregnancy loss, a 5-week Internet-based cognitive therapy intervention that was originally developed for PTSD but adapted to address pregnancy loss and grief decreased symptoms of depression, anxiety, posttraumatic stress, and grief compared with waitlist controls [80]. The consultant should also be familiar with local perinatal loss support groups.
Lastly, most obstetricians report having felt grief while caring for a mother of a stillborn baby [81, 82], so as a liaison, the psychiatric consultant should evaluate how the obstetric staff is coping. Grief, depression, self-doubt, and self-blame are the most common reactions reported among obstetricians. Brief empathic support provided directly by the psychiatrist, participation in Schwartz Rounds, or a referral to the hospital employee assistance program, especially if junior staff are involved, can be beneficial.
Insomnia
The differential diagnosis for insomnia includes an underlying psychiatric disorder, most likely anxiety, as well as an unusually wakeful rooming-in newborn infant. Interventions for primary insomnia include encouraging the mother to allow the baby to sleep in the nursery as well as medications like diphenhydramine. If the insomnia persists after discharge, cognitive behavioral therapy for insomnia is beneficial [83].
Anxiety
Anxiety is the most frequent comorbidity of PPD [42] but may also be seen in psychosis. If the mother is not depressed, at high risk for PPD, or psychotic, the consultant should screen for obsessive-compulsive disorder (OCD), which can occur for the first time in the postpartum period and can mimic some features of postpartum psychosis, as its associated obsessions may include intrusive thoughts of harming the infant [84, 85]. However, in OCD, these thoughts are ego-dystonic, the mother feels guilty and may avoid the infant, and her affect is not flat. In a prospective cohort study of 491 women who had delivered at a tertiary hospital, 11 % of women screened positive for OCD, but an additional 5.4 % had developed symptoms by 6 months [86]. Postpartum OCD should be treated similarly to non-postpartum OCD, with SSRIs as first-line as well as exposure/response-prevention and/or cognitive behavioral therapy if available.
PTSD, stemming from the mother’s experience of intense fear, helplessness, or horror during birth, occurs in 3.1–15.7 % of postpartum women [87]. A recent meta-analysis found that postpartum depressive symptoms were strongly associated with postpartum PTSD [87]. Other risk factors include unanticipated procedures or interventions, maternal and infant complications, hospitalization or hyperemesis during pregnancy, a previous history of trauma or psychiatric disorder, and low perceived social support [87, 88]. Aside from standard PTSD treatment such as psychotherapy and SSRIs, mothers with PTSD may also benefit from journaling about their birth experience and from reading stories of how other mothers recovered [88].
Anxiety should also prompt the consultant to screen for delirium, as it can be the presenting symptom for limbic encephalitis [89] as well as other medical conditions. If the anxiety is specific to the new baby’s arrival, targeted education, support, and reassurance are warranted. A combination of relaxation techniques, meditation, and short-acting medication such as a benzodiazepine can alleviate the mother’s suffering.
Confusion, Psychosis, “Patient Behavior,” and Organic Disorder: Unusual Behavior in the Mother
The psychiatric consultant must keep a broad differential diagnosis in mind when considering abnormal behavior in the mother, with postpartum psychosis (PPP) and delirium prominent among the diagnostic possibilities.
PPP occurs in 0.1 % of births [90, 91] and clusters in families [92]. It is strongly associated with bipolar disorder, and for some women, PPP is the first manifestation of bipolar disorder [93]. Potential risk factors for PPP in bipolar disorder include primiparity [91, 94, 95], increased maternal age [91], and having had a mood episode during pregnancy [96]. There are conflicting studies on whether delivery complications increase the risk for PPP [94, 95]. A prior history of PPP is a strong risk factor for subsequent episodes, with a risk of recurrence estimated as high as 75-90 % [97–99]. While the underlying pathophysiology is unclear, emerging evidence indicates a possible inflammatory basis for PPP [100–102].
PPP often mimics delirium, as symptoms can include confusion, disorientation, and visual hallucinations, and these may wax and wane [13, 103, 104]. PPP delusions often focus on the identity of the baby and may be accompanied by catalepsy or mania. In one investigation of PPP patients (n = 86) by Rhode et al. [105], the most frequent symptoms were restlessness, paranoid symptoms, catatonic excitement, anxiety, and sleep disturbance. Wisner et al [104] studied 762 women that those with childbearing-related psychosis (i.e., psychosis that emerged during pregnancy or within 3 months postpartum) and found they displayed more disorganization, bizarre behavior, and non-auditory hallucinations than women whose psychosis was not temporally related to childbirth. Therefore, the psychiatric consultant must be aware that PPP can feature both non-auditory hallucinations, which usually accompany delirium or intoxication, and anxiety or depressed mood [93].
PPP is a psychiatric emergency, as harm to the mother or infant may occur. Suicide is the leading cause of death for mothers within the first year after childbirth, usually carried out through violent means [106]. The risk of suicide for women suffering from PPP is estimated at 2 per 1000 [106], and the risk of infanticide in PPP is estimated at 4 % [107–109]. In the previously mentioned study of 86 women with PPP, 16 had died at follow-up 25 years later; five committed suicide by violent methods, and one had committed suicide during the index psychotic episode [105]. In that study, the only observed behavior considered dangerous to the infant occurred during catatonic excitement. In another study, of Indian PPP mothers (n = 108) [110], delusional content increased risk of harm to the infant. The most frequent delusions were “Baby is a devil or is ill fated” and “Someone will kill the baby or harm the baby.” The presence of delusions was associated with increased abusive behavior toward the infant overall, but especially in those mothers who described the baby as a devil, as “ill fated,” or who held the delusion that they had someone else’s baby.
For asymptomatic patients with a history of psychosis, the consultant should conduct a maternal capacity assessment, watching for psychotic neglect, including persecutory delusions, mistrust of healthcare providers, and especially delusions about the baby [108]. The mother’s family or outpatient team can provide valuable history, including any history of violence, impulsivity, or nonadherence to care, as well as more recent functioning. Consider prevention in high-risk mothers; if the mother has a history of psychosis only in the postpartum period, Bergink et al. [96] recommend prophylactic initiation of medication immediately postpartum, as they found that none of the women with a history of PPP relapsed with medication, while 44 % of women off medication relapsed [96]. Several case series and open trials have suggested efficacy for lithium [111, 112], divalproex sodium [113], and olanzapine [114]. Although there have been no RCTs of PPP prevention [115], we recommend initiating prophylaxis soon after delivery with the psychotropic that has historically been most effective for the patient. Furthermore, since the median onset for PPP is 8 days postpartum [95], we recommend close follow-up in high-risk patients, e.g., an obstetrics appointment or a nurse visit at home 1–2 weeks postpartum.
Psychotic symptoms observed in-house should be treated similarly to non-postpartum psychosis, with antipsychotics, mood stabilizers, and benzodiazepines as clinically indicated [116], and possible transfer to inpatient psychiatric care. For the first several weeks postdischarge, Sit et al. recommend intensive outpatient therapy or a day program [93]. The consultant can talk to the family, assuage guilt, and educate them about PPP as well as how to monitor for relapse [117].
If the mother plans to breastfeed, the consultant should discuss the risks of medication treatment versus the risks of untreated illness and balance those with the benefits of breastfeeding. For women that become ill with disrupted sleep, nursing should be discouraged at night. For nursing mothers taking anti-epileptic drugs like carbamazepine or valproate, the infant’s liver functions, complete blood count, and anticonvulsant level should be monitored at six weeks of age [118]. For mothers taking lithium, the infant’s lithium level, blood urea nitrogen, creatinine, and thyroid stimulating hormone should be measured at 4 to 6 weeks, and again every 8–12 weeks or as clinically indicated while the nursing mother is taking lithium [118, 119]. For mothers taking antipsychotics, the infants’ clinical status should be monitored, but most cases of infant exposure have documented no adverse effects [120, 121].
Medical causes of postpartum mental status change are rarer than PPP, but it is essential to consider them in the differential diagnosis. The medical causes of mental status changes that have been reported postpartum include Sheehan syndrome, urea cycle disorders, autoimmune thyroiditis, stroke, meningitis, meningioma, and multiple sclerosis [13, 122–125]. In Sheehan syndrome, or pituitary necrosis following postpartum hemorrhage, patients may have early hyponatremia or hypoglycemia, manifesting as weakness, apathy, mental slowing, confusion, and failure to lactate [126–128]. Urea cycle disorders begin with disorientation and confusion, appearing from one day antepartum to three days postpartum and progressing to coma; case reports describe hyperammonemia and hyperglutaminemia with normal liver transaminases [129–132]. Most cases occur in previously asymptomatic patients, but the patient or family may endorse a history of nausea after high-protein meals, episodes of irritability, lethargy, and vomiting, or growth delays [133]. Autoimmune thyroiditis has been associated with PPP, though it is unclear whether it is an incidental finding or a cause of psychosis [124]. Other reported causes of postpartum mental status change include epilepsy, alcohol withdrawal, and water intoxication from overhydration during labor [134, 135].
If the patient’s level of consciousness is fluctuating, or if her neurologic exam is revealing, obtain head imaging and ammonia levels as well as a complete blood count and comprehensive metabolic panel. Further workup may require neurology consult, lumbar puncture, electroencephalogram, or thyroperoxidase antibodies to avoid missing a reversible and potentially fatal cause of mental status change.
Besides PPP and medical causes, a personality disorder may lead to abnormal patient behavior. If this is the case, educate the primary obstetric team about the importance of consistent and frequent team communication to avoid splitting and milieu disruption [2, 136]. The importance of the consultant, in this case, is to determine maternal capacity as described above.
Substance Abuse
The consult for a mother abusing substances is sometimes a consult to determine maternal capacity. Often, this determination is out of the consultants’ hands, as state child welfare agencies may mandate reporting of patients with positive drug screens [137]. The psychiatrist’s main intervention may be to discuss the substance use with the mother non-judgmentally and to determine the appropriate level of referral to addiction services [138].
Medication Review
Consideration of medication during breastfeeding requires balancing potential risks and benefits to the mother and baby, but in general, the benefit of a mentally healthy mother should outweigh the risk of medication exposure to the infant, especially when the mother is at risk for such serious disorders as PPD or PPP. Studies indicate that most psychotropic medications are present in low amounts in infant serum and are well tolerated [119, 139, 140]. Generally, we recommend first deciding on proper psychiatric treatment for the mother as if she were not breastfeeding, and then modifying treatment as necessary depending on nursing status. The specific pharmacokinetics for each psychotropic in breastfeeding is beyond the scope of this article. For up to date information on the relative risks and benefits of psychotropics in nursing, several websites are useful, including reprotox.org and mothertobaby.org, as well as recent reviews by Molyneaux [141], Yonkers [142], Fortinguerra [143], and Klinger [139].
The Consultant’s Approach
We recommend the following approach for psychiatric consultation to a postpartum mother:
-
1.
Clarify the consult request. The primary team may have further concerns beyond the initial consultation question, and directly addressing these concerns enhances the consultation’s impact.
-
2.
Assess current symptoms, focusing on early signs of PPD, postpartum anxiety or PPP, and assess the patient’s level of coping.
-
3.
Observe maternal behavior with her infant and obtain staff input, paying special attention to safety concerns.
-
4.
Engage the patient, significant other, and family by providing education about the diagnosis and crafting a plan for symptom monitoring, management and follow-up, including how to access emergent psychiatric care if needed. Identify social supports and encourage increased involvement during the postpartum.
-
5.
If medication treatment is indicated, choose the appropriate medication for the patient’s symptoms regardless of her breastfeeding status, then modify the treatment plan as needed if she is nursing. Document a discussion of the risks to the infant’s health of untreated illness as well as of medication exposure.
-
6.
If the patient is high risk for PPD or PPP, or if treatment was started, obtain a postdischarge psychiatric appointment.
-
7.
Inform the outpatient obstetrician of the consultation outcome so she can monitor symptoms and encourage psychiatric follow-up.
-
8.
In complicated cases, consider a second opinion from a perinatal psychiatrist.
Conclusions
In this article, we have reviewed the reasons for psychiatric consultation to the obstetrics service and have outlined important steps for evaluation, diagnosis, and treatment of the most common conditions encountered postpartum. A major consideration in almost all consults is assessment of maternal capacity. Identifying as a mother can increase a patient’s motivation to adhere to treatment, and this may be harnessed effectively at the bedside, improving outcomes for all involved. Further research is needed into biomarkers for PPP and PPD. Because of potentially devastating effects of maternal psychiatric illness on the infant as well as the mother and other family members, consultants to the obstetric ward must be familiar with assessment and proper treatment of the psychiatric concerns of the postpartum.
References
Hutner L, Sacks A, Segal C. Characteristics of the population of patients on an obstetrics-gynecology consultation-liaison service. Paris, France: Marce Society; 2012.
Dunsis A, Smith GC. Consultation-liaison psychiatry in an obstetric service. Aust N Z J Psychiatry. 1996;30(1):63–73.
Judd F, Stafford L, Handrinos D, Laios L, Breadon C, Cornthwaite L, et al. Consultation-liaison psychiatry in a maternity hospital. Australas Psychiatry. 2010;18(2):120–4.
Sloan EP, Kirsh S. Characteristics of obstetrical inpatients referred to a consultation-liaison psychiatry service in a tertiary-level university hospital. Arch Womens Ment Health. 2008;11(5–6):327–33.
Tsai SJ, Lee YC, Yang CH, Sim CB. Psychiatric consultations in obstetric inpatients. J Obstet Gynaecol Res. 1996;22(6):603–7.
Rigatelli M, Galeazzi GM, Palmieri G. Consultation-liaison psychiatry in obstetrics and gynecology. J Psychosom Obstet Gynaecol. 2002;23(3):165–72.
Lin HL, Chou HH, Liu CY, Hsu SC, Hsiao MC, Juang YY. The role of consulting psychiatrists for obstetric and gynecologic inpatients. Chang Gung Med J. 2011;34(1):57–64.
Mourikis I, Kouzoupis AV, Antoniou M, Spyropoulou A, Leonardou A, Vogiatzi M, et al. Consultation-liaison psychiatry service in obstetrics and gynecology, in Athens, Greece. Eur Neuropsychopharmacol. 2009;19:S697.
Benjet C, Azar ST, Kuersten-Hogan R. Evaluating the parental fitness of psychiatrically diagnosed individuals: advocating a functional-contextual analysis of parenting. J Fam Psychol. 2003;17(2):238–51.
Rutherford SJ, Keeley P. Assessing parenting capacity: are mental health nurses prepared for this role? J Psychiatr Ment Health Nurs. 2009;16(4):363–7.
Nair S, Morrison MF. The evaluation of maternal competency. Psychosomatics. 2000;41(6):523–30.
Oyserman D, Mowbray CT, Meares PA, Firminger KB. Parenting among mothers with a serious mental illness. Am J Orthopsychiatry. 2000;70(3):296–315.
Brockington I. Motherhood and mental health. Oxford, England: Oxford University Press; 1996.
Beck CT, Reynolds MA, Rutowski P. Maternity blues and postpartum depression. J Obstet Gynecol Neonatal Nurs. 1992;21(4):287–93.
O'Hara MW. Postpartum depression: what we know. J Clin Psychol. 2009;65(12):1258–69.
O'Hara MW, Zekoski EM, Philipps LH, Wright EJ. Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol. 1990;99(1):3–15.
Murray L, Cooper P. Effects of postnatal depression on infant development. Arch Dis Child. 1997;77(2):99–101.
Whiffen VE, Gotlib IH. Infants of postpartum depressed mothers: temperament and cognitive status. J Abnorm Psychol. 1989;98(3):274–9.
Wrate RM, Rooney AC, Thomas PF, Cox JL. Postnatal depression and child development. A three-year follow-up study. Br J Psychiatry. 1985;146:622–7.
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–24.
Kim DR, Sockol LE, Sammel MD, Kelly C, Moseley M, Epperson CN. Elevated risk of adverse obstetric outcomes in pregnant women with depression. Arch Womens Ment Health. 2013;16(6):475–82.
Kim JH, Choi SS, Ha K. A closer look at depression in mothers who kill their children: is it unipolar or bipolar depression? J Clin Psychiatry. 2008;69(10):1625–31.
American Psychiatric Association. Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed.; 2013. pp. 186–7
American Psychiatric Association. Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition, Text Revision ed.; 2000. pp. 422–3.
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000;157(6):924–30.
Forty L, Jones L, Macgregor S, Caesar S, Cooper C, Hough A, et al. Familiality of postpartum depression in unipolar disorder: results of a family study. Am J Psychiatry. 2006;163(9):1549–53.
Murphy-Eberenz K, Zandi PP, March D, Crowe RR, Scheftner WA, Alexander M, et al. Is perinatal depression familial? J Affect Disord. 2006;90(1):49–55.
El-Ibiary SY, Hamilton SP, Abel R, Erdman CA, Robertson PA, Finley PR. A pilot study evaluating genetic and environmental factors for postpartum depression. Innov Clin Neurosci. 2013;10(9–10):15–22.
Costas J, Gratacos M, Escaramis G, Martin-Santos R, de Diego Y, Baca-Garcia E, et al. Association study of 44 candidate genes with depressive and anxiety symptoms in post-partum women. J Psychiatr Res. 2010;44(11):717–24.
Doornbos B, Dijck-Brouwer DA, Kema IP, Tanke MA, van Goor SA, Muskiet FA, et al. The development of peripartum depressive symptoms is associated with gene polymorphisms of MAOA, 5-HTT and COMT. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(7):1250–4.
Guintivano J, Arad M, Gould TD, Payne JL, Kaminsky ZA. Antenatal prediction of postpartum depression with blood DNA methylation biomarkers. Mol Psychiatry. 2014;19(5):560–7.
Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectr. 2014;29:1–12.
Payne JL, Palmer JT, Joffe H. A reproductive subtype of depression: conceptualizing models and moving toward etiology. Harv Rev Psychiatry. 2009;17(2):72–86.
Brett M, Baxendale S. Motherhood and memory: a review. Psychoneuroendocrinology. 2001;26(4):339–62.
Hendrick V, Altshuler LL, Suri R. Hormonal changes in the postpartum and implications for postpartum depression. Psychosomatics. 1998;39(2):93–101.
Osterlund MK. Underlying mechanisms mediating the antidepressant effects of estrogens. Biochim Biophys Acta. 2010;1800(10):1136–44.
Rubinow DR, Schmidt PJ, Roca CA. Estrogen-serotonin interactions: implications for affective regulation. Biol Psychiatry. 1998;44(9):839–50.
Chevillard C, Barden N, Saavedra JM. Estradiol treatment decreases type A and increases type B monoamine oxidase in specific brain stem areas and cerebellum of ovariectomized rats. Brain Res. 1981;222(1):177–81.
Ma ZQ, Bondiolotti GP, Olasmaa M, Violani E, Patrone C, Picotti GB, et al. Estrogen modulation of catecholamine synthesis and monoamine oxidase A activity in the human neuroblastoma cell line SK-ER3. J Steroid Biochem Mol Biol. 1993;47(1–6):207–11.
Ma ZQ, Violani E, Villa F, Picotti GB, Maggi A. Estrogenic control of monoamine oxidase A activity in human neuroblastoma cells expressing physiological concentrations of estrogen receptor. Eur J Pharmacol. 1995;284(1–2):171–6.
Sacher J, Wilson AA, Houle S, Rusjan P, Hassan S, Bloomfield PM, et al. Elevated brain monoamine oxidase A binding in the early postpartum period. Arch Gen Psychiatry. 2010;67(5):468–74.
Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–8.
Harris B, Johns S, Fung H, Thomas R, Walker R, Read G, et al. The hormonal environment of post-natal depression. Br J Psychiatry. 1989;154:660–7.
Harris B. Biological and hormonal aspects of postpartum depressed mood. Br J Psychiatry. 1994;164(3):288–92.
Yim IS, Glynn LM, Dunkel-Schetter C, Hobel CJ, Chicz-DeMet A, Sandman CA. Risk of postpartum depressive symptoms with elevated corticotropin-releasing hormone in human pregnancy. Arch Gen Psychiatry. 2009;66(2):162–9.
Rich-Edwards JW, Mohllajee AP, Kleinman K, Hacker MR, Majzoub J, Wright RJ, et al. Elevated midpregnancy corticotropin-releasing hormone is associated with prenatal, but not postpartum, maternal depression. J Clin Endocrinol Metab. 2008;93(5):1946–51.
Meltzer-Brody S, Stuebe A, Dole N, Savitz D, Rubinow D, Thorp J. Elevated corticotropin releasing hormone (CRH) during pregnancy and risk of postpartum depression (PPD). J Clin Endocrinol Metab. 2011;96(1):E40–7.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95.
Glynn LM, Davis EP, Sandman CA. New insights into the role of perinatal HPA-axis dysregulation in postpartum depression. Neuropeptides. 2013;47(6):363–70.
Bloch M, Rotenberg N, Koren D, Klein E. Risk factors associated with the development of postpartum mood disorders. J Affect Disord. 2005;88(1):9–18.
Bloch M, Rotenberg N, Koren D, Klein E. Risk factors for early postpartum depressive symptoms. Gen Hosp Psychiatry. 2006;28(1):3–8.
Jardri R, Pelta J, Maron M, Thomas P, Delion P, Codaccioni X, et al. Predictive validation study of the edinburgh postnatal depression scale in the first week after delivery and risk analysis for postnatal depression. J Affect Disord. 2006;93(1–3):169–76.
Buttner MM, Mott SL, Pearlstein T, Stuart S, Zlotnick C, O'Hara MW. Examination of premenstrual symptoms as a risk factor for depression in postpartum women. Arch Womens Ment Health. 2013;16(3):219–25.
Di Florio A, Jones L, Forty L, Gordon-Smith K, Blackmore ER, Heron J, et al. Mood disorders and parity—a clue to the aetiology of the postpartum trigger. J Affect Disord. 2014;152–154:334–9.
Ludermir AB, Lewis G, Valongueiro SA, de Araujo TV, Araya R. Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet. 2010;376(9744):903–10.
Nelson DB, Freeman MP, Johnson NL, McIntire DD, Leveno KJ. A prospective study of postpartum depression in 17 648 parturients. J Matern Fetal Neonatal Med. 2013;26(12):1155–61.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–6.
Evins GG, Theofrastous JP, Galvin SL. Postpartum depression: a comparison of screening and routine clinical evaluation. Am J Obstet Gynecol. 2000;182(5):1080–2.
Petrozzi A, Gagliardi L. Anxious and depressive components of Edinburgh postnatal depression scale in maternal postpartum psychological problems. J Perinat Med. 2013;41(4):343–8.
Wisner KL, Perel JM, Peindl KS, Hanusa BH, Piontek CM, Findling RL. Prevention of postpartum depression: a pilot randomized clinical trial. Am J Psychiatry. 2004;161(7):1290–2.
Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2013;CD001134.
Howell EA, Balbierz A, Wang J, Parides M, Zlotnick C, Leventhal H. Reducing postpartum depressive symptoms among black and Latina mothers: a randomized controlled trial. Obstet Gynecol. 2012;119(5):942–9.
Kim DR, Epperson CN, Weiss AR, Wisner KL. Pharmacotherapy of postpartum depression: an update. Expert Opin Pharmacother. 2014;15(9):1223–34.
Moses-Kolko EL, Berga SL, Kalro B, Sit DK, Wisner KL. Transdermal estradiol for postpartum depression: a promising treatment option. Clin Obstet Gynecol. 2009;52(3):516–29.
Davanzo R, Copertino M, De Cunto A, Minen F, Amaddeo A. Antidepressant drugs and breastfeeding: a review of the literature. Breastfeed Med. 2011;6(2):89–98.
Lanza di Scalea T, Wisner KL. Antidepressant medication use during breastfeeding. Clin Obstet Gynecol. 2009;52(3):483–97.
Forrest GC, Standish E, Baum JD. Support after perinatal death: a study of support and counselling after perinatal bereavement. Br Med J (Clin Res Ed). 1982;285(6353):1475–9.
Hughes P, Turton P, Hopper E, McGauley GA, Fonagy P. Disorganised attachment behaviour among infants born subsequent to stillbirth. J Child Psychol Psychiatry. 2001;42(6):791–801.
Gold KJ, Boggs ME, Muzik M, Sen A. Anxiety disorders and obsessive compulsive disorder 9 months after perinatal loss. Gen Hosp Psychiatry. 2014.
Gold KJ, Johnson TR. Mothers at risk: maternal mental health outcomes after perinatal death. Obstet Gynecol. 2014;123(1):6S.
Engelhard IM, van den Hout MA, Arntz A. Posttraumatic stress disorder after pregnancy loss. Gen Hosp Psychiatry. 2001;23(2):62–6.
Christiansen DM, Elklit A, Olff M. Parents bereaved by infant death: PTSD symptoms up to 18 years after the loss. Gen Hosp Psychiatry. 2013;35(6):605–11.
Cacciatore J, Radestad I, Frederik Froen J. Effects of contact with stillborn babies on maternal anxiety and depression. Birth. 2008;35(4):313–20.
Erlandsson K, Warland J, Cacciatore J, Radestad I. Seeing and holding a stillborn baby: mothers’ feelings in relation to how their babies were presented to them after birth—findings from an online questionnaire. Midwifery. 2013;29(3):246–50.
Hughes P, Turton P, Hopper E, Evans CD. Assessment of guidelines for good practice in psychosocial care of mothers after stillbirth: a cohort study. Lancet. 2002;360(9327):114–8.
Gold KJ, Dalton VK, Schwenk TL. Hospital care for parents after perinatal death. Obstet Gynecol. 2007;109(5):1156–66.
Hughes P, Riches S. Psychological aspects of perinatal loss. Curr Opin Obstet Gynecol. 2003;15(2):107–11.
Cunningham KA. Holding a stillborn baby: does the existing evidence help us provide guidance? Med J Aust. 2012;196(9):558–60.
Koopmans L, Wilson T, Cacciatore J, Flenady V. Support for mothers, fathers and families after perinatal death. Cochrane Database Syst Rev. 2013;6:CD000452.
Kersting A, Dolemeyer R, Steinig J, Walter F, Kroker K, Baust K, et al. Brief internet-based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: a randomized controlled trial. Psychother Psychosom. 2013;82(6):372–81.
Gold KJ, Kuznia AL, Hayward RA. How physicians cope with stillbirth or neonatal death: a national survey of obstetricians. Obstet Gynecol. 2008;112(1):29–34.
Farrow VA, Goldenberg RL, Fretts R, Schulkin J. Psychological impact of stillbirths on obstetricians. J Matern Fetal Neonatal Med. 2013;26(8):748–52.
Swanson LM, Flynn H, Adams-Mundy JD, Armitage R, Arnedt JT. An open pilot of cognitive-behavioral therapy for insomnia in women with postpartum depression. Behav Sleep Med. 2013;11(4):297–307.
Hudak R, Wisner KL. Diagnosis and treatment of postpartum obsessions and compulsions that involve infant harm. Am J Psychiatry. 2012;169(4):360–3.
Abramowitz JS, Meltzer-Brody S, Leserman J, Killenberg S, Rinaldi K, Mahaffey BL, et al. Obsessional thoughts and compulsive behaviors in a sample of women with postpartum mood symptoms. Arch Womens Ment Health. 2010;13(6):523–30.
Miller ES, Chu C, Gollan J, Gossett DR. Obsessive-compulsive symptoms during the postpartum period. A prospective cohort. J Reprod Med. 2013;58(3-4):115–22.
Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 2014;34(5):389–401.
Beck CT, Gable RK, Sakala C, Declercq ER. Posttraumatic stress disorder in new mothers: results from a two-stage U.S. national survey. Birth. 2011;38(3):216–27.
Gotkine M, Ben-Hur T, Vincent A, Vaknin-Dembinsky A. Limbic encephalitis presenting as a post-partum psychiatric condition. J Neurol Sci. 2011;308(1–2):152–4.
Munk-Olsen T, Laursen TM, Mendelson T, Pedersen CB, Mors O, Mortensen PB. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66(2):189–95.
Valdimarsdottir U, Hultman CM, Harlow B, Cnattingius S, Sparen P. Psychotic illness in first-time mothers with no previous psychiatric hospitalizations: a population-based study. PLoS Med. 2009;6(2):e13.
Jones I, Craddock N. Familiality of the puerperal trigger in bipolar disorder: results of a family study. Am J Psychiatry. 2001;158(6):913–7.
Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Womens Health (Larchmt). 2006;15(4):352–68.
Blackmore ER, Jones I, Doshi M, Haque S, Holder R, Brockington I, et al. Obstetric variables associated with bipolar affective puerperal psychosis. Br J Psychiatry. 2006;188:32–6.
Bergink V, Lambregtse-van den Berg MP, Koorengevel KM, Kupka R, Kushner SA. First-onset psychosis occurring in the postpartum period: a prospective cohort study. J Clin Psychiatry. 2011;72(11):1531–7.
Bergink V, Bouvy PF, Vervoort JS, Koorengevel KM, Steegers EA, Kushner SA. Prevention of postpartum psychosis and mania in women at high risk. Am J Psychiatry. 2012;169(6):609–15.
Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662–73.
Altshuler LL, Hendrick V, Cohen LS. Course of mood and anxiety disorders during pregnancy and the postpartum period. J Clin Psychiatry. 1998;59 Suppl 2:29–33.
Blackmore ER, Rubinow DR, O’Connor TG, Liu X, Tang W, Craddock N, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar Disord. 2013;15(4):394–404.
Bergink V, Burgerhout KM, Weigelt K, Pop VJ, de Wit H, Drexhage RC, et al. Immune system dysregulation in first-onset postpartum psychosis. Biol Psychiatry. 2013;73(10):1000–7.
Weigelt K, Bergink V, Burgerhout KM, Pescatori M, Wijkhuijs A, Drexhage HA. Down-regulation of inflammation-protective microRNAs 146a and 212 in monocytes of patients with postpartum psychosis. Brain Behav Immun. 2013;29:147–55.
Bergink V, Gibney SM, Drexhage HA. Autoimmunity, inflammation, and psychosis: a search for peripheral markers. Biol Psychiatry. 2014;75(4):324–31.
Viguera AC, Emmerich AD, Cohen LS. Case records of the Massachusetts General Hospital. Case 24-2008. A 35-year-old woman with postpartum confusion, agitation, and delusions. N Engl J Med. 2008;359(5):509–15.
Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77–87.
Rhode A, Marneros A. Postpartum psychoses: onset and long-term course. jPsychopharmacology. 1993;26(3–4):203–9.
Oates M. Suicide: the leading cause of maternal death. Br J Psychiatry. 2003;183:279–81.
Porter T, Gavin H. Infanticide and neonaticide: a review of 40 years of research literature on incidence and causes. Trauma Violence Abuse. 2010;11(3):99–112.
Rahman T, Grellner KA, Harry B, Beck N, Lauriello J. Infanticide in a case of folie a deux. Am J Psychiatry. 2013;170(10):1110–2.
Nonacs R, Cohen LS. Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59 Suppl 2:34–40.
Chandra PS, Bhargavaraman RP, Raghunandan VN, Shaligram D. Delusions related to infant and their association with mother–infant interactions in postpartum psychotic disorders. Arch Womens Ment Health. 2006;9(5):285–8.
Stewart DE, Klompenhouwer JL, Kendell RE, van Hulst AM. Prophylactic lithium in puerperal psychosis. The experience of three centres. Br J Psychiatry. 1991;158:393–7.
Austin MP. Puerperal affective psychosis: is there a case for lithium prophylaxis? Br J Psychiatry. 1992;161:692–4.
Wisner KL, Hanusa BH, Peindl KS, Perel JM. Prevention of postpartum episodes in women with bipolar disorder. Biol Psychiatry. 2004;56(8):592–6.
Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400–4.
Essali A, Alabed S, Guul A, Essali N. Preventive interventions for postnatal psychosis. Cochrane Database Syst Rev. 2013;6:CD009991.
Sharma V. Pharmacotherapy of postpartum psychosis. Expert Opin Pharmacother. 2003;4(10):1651–8.
Engqvist I, Nilsson K. Involving the family in the care and treatment of women with postpartum psychosis: Swedish psychiatrists’ experiences. Psychiatry J. 2013;2013:897084.
Marsh W, Viguera A. Bipolar disorder through pregnancy and postpartum. Psychiatr Ann. 2012;42(5):184–9.
Viguera AC, Newport DJ, Ritchie J, Stowe Z, Whitfield T, Mogielnicki J, et al. Lithium in breast milk and nursing infants: clinical implications. Am J Psychiatry. 2007;164(2):342–5.
Yonkers KA, Wisner KL, Stowe Z, Leibenluft E, Cohen L, Miller L, et al. Management of bipolar disorder during pregnancy and the postpartum period. Am J Psychiatry. 2004;161(4):608–20.
Gardiner SJ, Kristensen JH, Begg EJ, Hackett LP, Wilson DA, Ilett KF, et al. Transfer of olanzapine into breast milk, calculation of infant drug dose, and effect on breast-fed infants. Am J Psychiatry. 2003;160(8):1428–31.
Brockington IF. Cerebral vascular disease as a cause of postpartum psychosis. Arch Womens Ment Health. 2007;10(4):177–8.
Brockington IF. Eclamptic psychosis. Arch Womens Ment Health. 2007;10(2):87–8.
Bergink V, Kushner SA, Pop V, Kuijpens H, Lambregtse-van den Berg MP, Drexhage RC, et al. Prevalence of autoimmune thyroid dysfunction in postpartum psychosis. Br J Psychiatry. 2011;198(4):264–8.
Castro J, Billick S, Kleiman A, Chiechi M, Al-Rashdan M. Confounding psychosis in the postpartum period. Psychiatr Q. 2014;85(1):91–6.
Boulanger E, Pagniez D, Roueff S, Binaut R, Valat AS, Provost N, et al. Sheehan syndrome presenting as early post-partum hyponatraemia. Nephrol Dial Transplant. 1999;14(11):2714–5.
Kovacs K. Sheehan syndrome. Lancet. 2003;361(9356):520–2.
Shoib S, Dar MM, Arif T, Bashir H, Bhat MH, Ahmed J. Sheehan's syndrome presenting as psychosis: a rare clinical presentation. Med J Islam Repub Iran. 2013;27(1):35–7.
Peterson DE. Acute postpartum mental status change and coma caused by previously undiagnosed ornithine transcarbamylase deficiency. Obstet Gynecol. 2003;102(5 Pt 2):1212–5.
Enns GM, O'Brien WE, Kobayashi K, Shinzawa H, Pellegrino JE. Postpartum “psychosis” in mild argininosuccinate synthetase deficiency. Obstet Gynecol. 2005;105(5 Pt 2):1244–6.
Wong LJ, Craigen WJ, O'Brien WE. Postpartum coma and death due to carbamoyl-phosphate synthetase I deficiency. Ann Intern Med. 1994;120(3):216–7.
Cordero DR, Baker J, Dorinzi D, Toffle R. Ornithine transcarbamylase deficiency in pregnancy. J Inherit Metab Dis. 2005;28(2):237–40.
Leonis MA, Balistreri WF. Ch. 76: other inherited metabolic disorders of the liver. In: Feldman M, Friedman LS, Brandt LJ, editors. Sleisinger and Fordtran’s gastrointestinal and liver disease. 9th ed. Saunders Elsevier: Philadelphia, PA, USA; 2010. p. 1271–4.
Brockington IF. The present importance of the organic psychoses of pregnancy, parturition and the puerperium. Arch Womens Ment Health. 2007;10(6):305–6.
Brockington IF. Postpartum psychoses due to other diseases with a specific link to childbirth. Arch Womens Ment Health. 2007;10(5):241–2.
Groves JE. Management of the borderline patient on a medical or surgical ward: the psychiatric consultant's role. Int J Psychiatry Med. 1975;6(3):337–48.
Miller C, Lanham A, Welsh C, Ramanadhan S, Terplan M. Screening, testing, and reporting for drug and alcohol use on labor and delivery: a survey of Maryland birthing hospitals. Soc Work Health Care. 2014;53(7):659–69.
Gopman S. Prenatal and postpartum care of women with substance use disorders. Obstet Gynecol Clin North Am. 2014;41(2):213–28.
Klinger G, Stahl B, Fusar-Poli P, Merlob P. Antipsychotic drugs and breastfeeding. Pediatr Endocrinol Rev. 2013;10(3):308–17.
Stowe ZN. The use of mood stabilizers during breastfeeding. J Clin Psychiatry. 2007;68 Suppl 9:22–8.
Molyneaux E, Howard LM, McGeown HR, Karia AM, Trevillion K. Antidepressant treatment for postnatal depression. Cochrane Database Syst Rev. 2014;9:CD002018.
Yonkers KA, Vigod S, Ross LE. Diagnosis, pathophysiology, and management of mood disorders in pregnant and postpartum women. Obstet Gynecol. 2011;117(4):961–77.
Fortinguerra F, Clavenna A, Bonati M. Psychotropic drug use during breastfeeding: a review of the evidence. Pediatrics. 2009;124(4):e547–56.
Acknowledgments
This manuscript was supported by NIMH grant K23 MH092399 (P.I. DRK).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Neither Dr. Anderson nor Dr. Kim have any conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Women's Mental Health
Rights and permissions
About this article
Cite this article
Anderson, E.A., Kim, D.R. Psychiatric Consultation to the Postpartum Mother. Curr Psychiatry Rep 17, 26 (2015). https://doi.org/10.1007/s11920-015-0561-5
Published:
DOI: https://doi.org/10.1007/s11920-015-0561-5