Abstract
The menopause transition is associated with a two to fourfold increased risk in major depressive disorder (MDD) and clinical elevations in depressive symptoms. While the pathophysiological mechanisms underlying this increased risk remain uncertain, ovarian hormone fluctuation is believed to play a role. To the extent that this is the case, hormone replacement therapy (HRT), through its hormone-stabilizing effects, represents a viable antidepressant treatment. The current review summarizes the most recent literature evaluating the efficacy of HRT in treating MDD in peri- and postmenopausal women. In addition, to provide a clinical context in which to interpret this research, the endocrinology and clinical phenomenology related to depression with onset in the menopause transition (D-MT) are discussed. The available evidence suggests that HRT, specifically involving estrogen delivered through a skin patch, is a promising intervention in the treatment of D-MT. However, HRT of any form is an ineffective antidepressant in women who are well into the postmenopausal period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A 49-year-old woman presents to your office complaining of flattened mood, anhedonia, irritability, trouble sleeping, and decreased concentration. She “is just not herself” and feels disconnected from her friends and family. In the intake interview, she reveals that she has been coping with several psychosocial stressors, including her daughter’s departure for college and her elderly mother’s recent hip fracture. “On top of all this, these constant hot flashes are killing me!” she exclaims. When asked if she has noticed any other menopausal symptoms, she explains her menses have been irregular (longer cycles and a skipped menses or two) for the past year or so.
How do you treat this patient? Does the fact that she is in the menopause transition (MT) influence treatment? Hormone replacement therapy (HRT) is indicated for the treatment of vasomotor symptoms but does current evidence support its use as monotherapy in the treatment of mid-life depression? The current review aims to address the latter question by summarizing the most recent research examining the antidepressant effects of HRT. First, however, the phenomenology of depression with onset in the menopause transition (D-MT) will be discussed, including a review of its endocrinology, prevalence, and associated risk factors. Finally, we briefly discuss some recent clinical research providing insight into the putative pathophysiological mechanisms underlying D-MT development.
The Endocrinology of the Menopause Transition
As a woman approaches the end of her reproductive life, a depleted supply of ovarian follicles triggers a cascade of endocrine changes, disrupting the complex regulation of the hypothalamic-pituitary-ovarian axis (reviewed in [1, 2]). Among these changes are substantial fluctuations in follicle-stimulating hormone (FSH). As a result, although FSH levels have traditionally been used as an endocrine marker of postmenopausal status, they are less useful for reproductive staging in the MT. Instead, standard criteria for reproductive staging are based primarily on menstrual bleeding patterns, which can be corroborated with endocrine data. The most commonly used staging system is the Stages of Reproductive Aging Workshop (STRAW+10) [3], which divides a woman’s reproductive lifespan into stages based on bleeding patterns, using the final menstrual period as the anchor.
Consequent to fluctuating FSH concentrations, estradiol (E2) levels are also highly variable during the MT. On the one hand, there can be extended periods of low E2 in between menstrual cycles while on the other hand, some cycles may actually be characterized by E2 concentrations that are much higher than experienced premenopausally. E2 concentrations during anovulatory cycles, which become increasingly frequent as the MT progresses, are also very erratic. In contrast, an increasing number of anovulatory cycles translate to a stabilization of progesterone (P4) concentrations. As such, women are exposed to considerable E2 flux in the MT. Furthermore, this flux, which has recently been shown to continue into the early postmenopausal period [4], may extend over 5 years or more [5].
Depression With Onset in the Menopause Transition (D-MT)
Prevalence
Popular opinion suggests that this period of hormonal flux is often accompanied by increased moodiness, irritability, and risk for depression. Is there empirical evidence to support this belief? Yes, in fact, over the past decade, multiple studies have observed an increased risk of both elevated depressive symptoms and syndromal major depressive disorder (MDD) during the MT. For example, the Study of Women’s Health Across the Nation (SWAN) of 3302 women aged 42–52 who were followed over 5 years [6] observed an increased risk of clinically significant depressive symptoms in the early and late MT as well as the early postmenopause (STRAW stages −2 to +1), with odds ratios ranging from 1.30 to 1.71. Furthermore, the 15-year Seattle Midlife Women’s Health Study of 302 women aged 35 to 55 [7] found that the rate of elevated depressive symptoms doubled in the late MT. Studies excluding women with a history of MDD also find the risk of clinical elevations in depressive symptoms to be increased in the MT. For example, a sub-analysis of the Penn Ovarian Aging Study involving 231 women [8] found that over 8 years, the risk of elevated depressive symptoms (CES-D score ≥16) was four times greater during the MT compared to the premenopausal period. The 3-year Harvard Study of Moods and Cycles study of 460 women aged 35–45 [9] also found that the rate of clinically significant depressive symptoms in the pre- vs. perimenopause was 20 and 33 %, respectively.
The incidence of syndromal MDD is also increased in the MT in mixed samples of women with and without a history of MDD. In a sub-analysis of 221 initially premenopausal SWAN participants involving a 10-year follow-up and including women both with and without a history of depression, the rate of syndromal MDD, assessed using the Structured Clinical Interview for DSM Disorders IV (SCID-IV), was found to be doubled during the MT [10]. In contrast, it is unclear whether the risk of first-onset MDD is increased during the MT: in 260 SWAN participants free of a history of MDD, the risk of first-onset MDD, assessed using the SCID-IV, was not increased in the MT over 7 years [11].
The above research provides strong evidence that the risk of clinically significant elevations in depressive symptoms is increased in the MT and early postmenopausal period. However, the available evidence suggests that the risk of syndromal MDD may only be increased in the MT among those women with a positive depression history.
Clinical Phenomenology
D-MT and MDD unrelated to reproductive events share the same basic diagnostic criteria (e.g., depressed mood, anhedonia), and a diagnosis of MDD should be made if these criteria are met regardless of whether one or more of the symptoms might overlap with classic menopausal symptoms. However, the presence of additional bothersome menopausal symptoms may present additional challenges and exacerbate depressive symptoms in perimenopausal women. For example, over half of women in the MT and early postmenopausal period experience vasomotor symptoms [12]. In addition, women reporting clinical elevations in depressive symptoms are more likely to experience subjective hot flashes lacking physical corroboration [13]; the impairment attributed to vasomotor symptoms may therefore be particularly great in women with D-MT. Sleep disturbances, both related and unrelated to night sweats, are also reported in approximately half of women in the MT [12], and, not surprisingly, this frequency is even greater in women with D-MT [14]. Finally, vaginal dryness, reported by 7–39 % of perimenopausal women [12], can contribute to sexual dysfunction, creating an additional barrier to intimacy with loved ones.
If D-MT and MDD share the same diagnostic criteria, what then determines the diagnosis of D-MT and why might it be important to differentiate it from MDD unrelated to reproductive events? To diagnose D-MT, it is necessary to establish the presence of perimenopausal events as the context—such as irregular or skipped cycles, hot flashes, vaginal dryness, elevated FSH—and exclude the possibility of pregnancy or other endocrine issues that could cause amenorrhea. The diagnosis of D-MT as opposed to MDD occurring at other life phases may well influence the therapeutic approach.
The Role of Hormonal Fluctuation in D-MT
Several theories explaining the increased risk of depression in the MT have been proposed. Among them are the empty nest syndrome and the domino theory, the latter hypothesizing that vasomotor symptoms trigger depressed mood through sleep disruption and functional impairment. While familial stress and vasomotor symptoms may contribute to depressive symptoms in some perimenopausal women, neither are any longer believed to be solely responsible for the increased risk of depressed mood in the MT. Rather, the potential involvement of hormonal fluctuation in the etiology of D-MT has been of increasing scientific interest.
In 2005, the NIH State-of-the-Science Conference Statement on Management of Menopause-Related Symptoms [12] concluded that there was “limited evidence that ovarian changes associated with menopause might be a cause of depression.” Indeed, not all studies directly examining the relationship between E2 fluctuations and mood have found a significant effect [7, 10, 15]. However, design limitations, most notable of which is infrequent hormone measurement, may account for these negative findings. Consistent with this, the two studies using a more frequent hormone sampling interval have observed a significant relationship between hormonal variability (E2 and FSH, respectively) and D-MT [8, 16]. Supporting this theory is the finding that both a history of premenstrual syndrome and a history of postpartum depression—two disorders for which reproductive hormonal flux has been shown to play a role [17, 18]—are each strong predictors of D-MT [7, 8, 14].
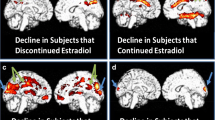
Our preliminary data further support a role of E2 fluctuation in the etiology of D-MT. In our ongoing research, E2 concentrations and CES-D scores are obtained four times (baseline, months 1, 8, and 14) in initially euthymic healthy women (ages 45–55) meeting STRAW+10 criteria for the early or late menopause transition (stages −2 and −1) over a period of 14 months. The Life Experiences Scale (LES), providing a measure of overall life stress in the previous 6 months (a composite of number and severity of stressors), was also administered at the baseline assessment. Interestingly, the standard deviation calculated across the four E2 concentrations, providing a proxy of E2 fluctuation, was found to be associated with elevated depressive symptoms at the end of the 14-month interval but only in women falling above the median LES score. E2 fluctuation was also associated with exaggerated emotional responses to a psychosocial laboratory stressor; furthermore, this association was significant at both months 8 and 14 (thus preceding the effect of E2 fluctuation on depressive symptoms). These data therefore suggest that fluctuating E2 may increase a woman’s sensitivity to stress, which, when combined with significant life stress proximal to the MT (e.g., divorce, child leaving for college, caring for elderly parents, etc.), may contribute to D-MT. However, in the absence of significant life stress, the risk of D-MT is not increased. These findings must be considered preliminary, but they are consistent with the observation that although hormonal fluctuation is believed to play a role in triggering D-MT, psychosocial stress including unemployment [14], financial strain [6], lack of social support [6] and stressful life events proximate to the MT [6, 10] have also been shown to predict an increased risk for both clinical elevations in depressive symptoms and syndromal MDD in the MT.
To the extent that fluctuations in E2 contribute to increased emotional lability in the face of life stress, stabilizing the hormonal environment may benefit mood in the MT. E2 therapy, by impairing ovulation [19] and preventing E2 concentrations from dipping below premenopausal follicular phase levels [20], does just that. As such, the potential antidepressant effects of E2 therapy are of interest. In the following section, we review the existing literature examining the efficacy of E2 therapy in the treatment of D-MT and contrast this literature with studies conducted in postmenopausal women, placing particular emphasis on the most recent research.
HRT in the Treatment of D-MT
The Perimenopause and Early Postmenopause
Studies evaluating the efficacy of oral preparations of E2 in treating D-MT have obtained mixed results [21–23]. In contrast, transdermal E2 may be a more promising treatment for D-MT. To date, one open-label study and three small RCTs have examined the efficacy of transdermal E2 as a treatment for D-MT. The open-label study observed a remission rate of 60 % among its perimenopausal participants [24] while in the two older RCTs, remission rates of 68 and 80 % were observed compared to rates of approximately 20 and 22 % in the placebo groups [25, 26•].
The third study, a recent double-blind RCT [27] aimed at examining the role of sleep disturbance in the etiology of menopausal depression, compared the efficacy of 8 weeks of transdermal 17-β estradiol (0.05 mg/day), the hypnotic zolpidem (10 mg/day), and placebo. It included 72 peri- and postmenopausal women aged 40–60 meeting DSM-IV criteria for a unipolar depressive disorder of mild to moderate severity as well as meeting threshold criteria for an insomnia syndrome. The results revealed no significant differences in depressive symptom improvement between the three treatment arms. However, subgroup analyses suggested that among the peri- but not postmenopausal women, the within-woman increase in serum E2 concentrations across all treatment arms were predictive of improved depressive symptoms, suggesting specificity of mood effects of increasing E2 levels for perimenopausal women.
Follow-up analyses from the above study, combined with data from a similar RCT examining the cognitive effects of transdermal E2 in euthymic women [28•], aimed to assess the mood effects of P4 supplementation. More specifically, depressive symptoms were assessed before and after the administration of 14 days of medroxyprogesterone (10 mg/day) to women who had been assigned to the transdermal E2 treatment arm. Participants included 24 euthymic and 14 depressed peri- and early postmenopausal women. Results revealed that mood did not significantly change with the administration of medroxyprogesterone in either the euthymic or depressed women [29•].
The Late Postmenopausal Period
Consistent with the notion that hormonal flux, rather than low ovarian hormone levels per se, triggers depressive symptoms, recent studies find HRT to be an ineffective treatment for depression in the older postmenopausal woman. In one RCT [30] examining the effect of hormone replacement and vitamin D for age-related bone loss, 489 older postmenopausal women (aged 65–77) were randomized to 36 months of conjugated equine estrogen (0.625 mg/day) alone or combined with calcitriol, calcitriol alone, or placebo. Women with an intact uterus (59 % of the total sample) receiving estrogen also received daily medroxyprogesterone acetate (2.5 mg/day) for uterine protection. HRT was not found to significantly impact the percentage of women endorsing clinically significant elevations in depressive symptoms. Similarly, an RCT of 76 hysterectomized euthymic postmenopausal women did not find an effect of treatment on mood or anxiety after randomization to six 28-day cycles of either conjugated equine estrogen (0.625 mg/day) or placebo [31].
The findings of these two studies are in line with older studies using transdermal E2, which also did not find an antidepressant effect of E2 therapy in older postmenopausal women [24, 32]. Thus, the negative findings of the above studies are more likely to be related to the late postmenopausal status of the participants rather than the hormonal preparation used.
Research investigating the efficacy of E2 therapy as an adjunct to standard antidepressant treatment also does not support the use of E2 therapy in late postmenopausal women for the treatment of mood symptoms. Recently, the STAR*D trial [33] of 896 premenopausal and 544 postmenopausal women meeting DSM-IV criteria for MDD administered 12–14 weeks of citalopram. One quarter of the women were taking exogenous hormones (oral contraceptives in the premenopausal women and HRT in the postmenopausal women). When the authors compared the efficacy of citalopram in women taking versus not taking exogenous hormones, differential effects were obtained for pre- versus postmenopausal women. While citalopram’s antidepressant effect was greater in premenopausal women taking (versus not taking) oral contraceptives, it did not differ according to hormonal status in the postmenopausal women. While it remains to be seen whether E2 therapy is useful as an adjunct treatment to SSRIs in depressed peri- and early postmenopausal women, the above study suggests that it is not an effective adjunct treatment in postmenopausal women.
Issues to Consider When Prescribing HRT
The prescription of E2 therapy for menopausal symptoms remains strongly influenced by the surprising results of the Women’s Health Initiative (WHI), suggesting that E2 therapy increased the risk of both non-fatal cardiovascular events [34] and breast cancer [35]. However, as summarized in the 2012 Position Statement of the North American Menopause Society [36] and 2010 Endocrine Society Scientific Statement [37], secondary analyses of the WHI, as well as more recent research, have revealed that earlier findings were likely partially a function of the participant’s older age (mean age = 63, range 50–79) and the fact that they were on average 12 years postmenopausal and likely to be in advanced stages of atherosclerotic progression. Subgroup analyses [38] and one surrogate endpoint study [39] from the WHI demonstrate that the effects of HRT on cardiovascular disease are modified by the timing of its initiation relative to the cessation of menses, indicating that the risk of cardiovascular disease in the WHI was observed in older but not younger women. In line with this, HRT should be initiated only in women within 10 years of menopause [36].
The preparation of E2 and P4 used in WHI (conjugated equine estrogen and medroxyprogesterone) likely also helps to explain its findings. Recent evidence suggests that transdermal E2, because it is not subject to first-pass hepatic metabolism as are oral preparations, does not exhibit the prothrombotic and proinflammatory effects that are observed with oral E2 [40]. Second best in terms of cardiovascular profile is oral 17-β E2, exhibiting a more favorable cardiovascular profile when compared to conjugated equine estrogen [41]. Furthermore, the progestogen used in the WHI, medroxyprogesterone, has been shown to be particularly antagonistic to E2’s cardiovascular benefits [42, 43]. Micronized P4 has therefore been proposed as a safer alternative [42]. As such, transdermal E2, combined with micronized P4 in women requiring uterine protection, may be the safest HRT [42] in terms of cardiovascular and prothrombotic effects.
To minimize HRT-associated risks, treatment guidelines also recommend using the lowest possible E2 dose necessary to obtain the desired effect. The duration of use is also important to consider: while unopposed E2 has a more favorable benefit-risk profile even with longer use (11 years), the use of combined E2 and P4 should be limited to 3 to 5 years of use to avoid an increased risk of breast cancer [36]. Finally, it is recommended that the use of HRT to manage D-MT should involve a general practitioner or gynecologist to monitor the effects of HRT on other systems.
Summary and Conclusions
Taken together, the available evidence supports the use of E2 therapy in the treatment of depression among peri- and early postmenopausal women but not women who are well into the postmenopausal period. Among peri- and early postmenopausal women, there is growing evidence that transdermal E2 may be superior to oral preparations in terms of its antidepressant effects. There are several possible reasons for this (discussed in [44, 45•]), including the greater bioavailability of E2 when delivered transdermally and an E2-to-estriol ratio that is more comparable to that observed in premenopausal women when compared to conjugated equine estrogen. In theory, transdermal E2 should also result in more constant E2 concentrations in blood when compared to oral preparations, although if this is true in practice is uncertain given that issues related to patch adherence are not uncommon. For these reasons, we hypothesize that transdermal E2’s antidepressant effects may be more pronounced than oral HRT’s in treating D-MT. However, upcoming research, such as the recently completed Kronos Early Estrogen Prevention Study (KEEPS) Cognitive and Affective ancillary study (KEEPS-cog) [45•], a placebo-controlled RCT comparing the cognitive and mood effects of low-dose conjugated equine estrogen and low-dose transdermal E2 in the late perimenopause and early postmenopause, will more definitively clarify this issue.
Though the coming years will undoubtedly spawn more definitive conclusions about the treatment of D-MT, we believe the available preliminary evidence supports the use of E2 therapy, particularly transdermal E2, in the treatment of D-MT. While the exact mechanisms by which depressive symptoms are triggered in the MT are unknown, it may be safe to assume that changes in E2, be it E2 withdrawal or fluctuation, play an important role. Based on this assumption, we suggest that the following factors be considered before prescribing HRT as a possible treatment for mid-life depression:
-
Menopausal status: The existing literature, while limited by small sample sizes, suggests that HRT may not be an effective treatment for depression in an older postmenopausal woman.
-
Timing of depressive symptom onset: Depressive symptoms whose onset coincides with the onset of menstrual irregularity may be more likely to be hormonally related and thus more responsive to E2 therapy.
-
History of reproductive mood disorders: A positive history of reproductive mood disorders such as premenstrual dysphoric disorder or postpartum depression may indicate an increased sensitivity to fluctuations in ovarian hormones.
-
Medical history: E2 therapy has been shown to increase the reoccurrence of venous thromboembolism, endometrial cancer, and breast cancer in women with a positive history of these diseases [36].
-
Patient preference: Perhaps more so than any physical disorder, patient buy-in is critical in the treatment of depression. Thus, the treatment modality—HRT, an SSRI, or psychotherapy—should always be chosen with the patient’s preference in mind.
-
Other menopausal symptoms: A trial of HRT as monotherapy may be particularly worthwhile in the case of a woman suffering from severe hot flashes and sleep-disturbing night sweats in addition to D-MT. If depressive symptoms do not remit with HRT, a conventional antidepressant may be prescribed.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Hale GE, Robertson DM, Burger HG. The perimenopausal woman: endocrinology and management. J Steroid Biochem Mol Biol. 2014;142(7):121–31.
Santoro N, Randolph Jr JF. Reproductive hormones and the menopause transition. Obstet Gynecol Clin N Am. 2011;38(3):455.
Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop+10: addressing the unfinished agenda of staging reproductive aging. Climacteric. 2012;15(2):105–14.
Tepper PG, Randolph Jr JF, McConnell DS, Crawford SL, El Khoudary SR, Joffe H, et al. Trajectory clustering of estradiol and follicle-stimulating hormone during the menopausal transition among women in the Study of Women’s Health Across the Nation (SWAN). J Clin Endocrinol Metab. 2012;97(8):2872–80.
McKinlay SM, Brambilla DJ, Posner JG. The normal menopause transition. Maturitas. 1992;14(2):103–15.
Bromberger JT, Matthews KA, Schott LL, Brockwell S, Avis NE, Kravitz HM, et al. Depressive symptoms during the menopausal transition: the Study of Women’s Health Across the Nation (SWAN). J Affect Disord. 2007;103(1):267–72.
Woods NF, Smith-DiJulio K, Percival DB, Tao EY, Mariella A, Mitchell ES. Depressed mood during the menopausal transition and early postmenopause: observations from the Seattle midlife women’s health study. Menopause. 2008;15(2):223–32.
Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63(4):375.
Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385.
Bromberger JT, Kravitz HM, Chang Y-F, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Psychol Med. 2011;41(9):1879–88.
Bromberger J, Kravitz H, Matthews K, Youk A, Brown C, Feng W. Predictors of first lifetime episodes of major depression in midlife women. Psychol Med. 2009;39(1):55.
National Institutes of Health. National Institutes of Health State-of-the-Science Conference statement: management of menopause-related symptoms. Ann Intern Med. 2005;142(12 Pt 1):1003.
Thurston RC, Blumenthal JA, Babyak MA, Sherwood A. Emotional antecedents of hot flashes during daily life. Psychosom Med. 2005;67(1):137–46.
Freeman EW, Sammel MD, Liu L, Gracia CR, Nelson DB, Hollander L. Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry. 2004;61(1):62.
Avis NE, Crawford S, Stellato R, Longcope C. Longitudinal study of hormone levels and depression among women transitioning through menopause. Climacteric. 2001;4(3):243–9.
Daly RC, Danaceau MA, Rubinow DR, Schmidt PJ. Concordant restoration of ovarian function and mood in perimenopausal depression. Am J Psychiatr. 2003;160(10):1842–6.
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatr. 2000;157(6):924–30.
Schmidt PJ, Nieman LK, Danaceau MA, Adams LF, Rubinow DR. Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med. 1998;338(4):209–16.
De Leo V, Lanzetta D, Morgante G, De Palma P, D’Antona D. Inhibition of ovulation with transdermal estradiol and oral progestogens in perimenopausal women. Contraception. 1997;55(4):239–43.
Girdler SS, Hinderliter AL, Wells EC, Sherwood A, Grewen KM, Light KC. Transdermal versus oral estrogen therapy in postmenopausal smokers: hemodynamic and endothelial effects. Obstet Gynecol. 2004;103(1):169–80.
Bukulmez O, Al A, Gurdal H, Yarali H, Ulug B, Gurgan T. Short-term effects of three continuous hormone replacement therapy regimens on platelet tritiated imipramine binding and mood scores: a prospective randomized trial. Fertil Steril. 2001;75(4):737–43.
Ross L, Alder E, Cawood RH, Brown J, Gebbie AE. Psychological effects of hormone replacement therapy: a comparison of tibolone and a sequential estrogen therapy. J Psychosom Obstet Gynecol. 1999;20(2):88–96.
Soares CN, Arsenio H, Joffe H, Bankier B, Cassano P, Petrillo LF, et al. Escitalopram versus ethinyl estradiol and norethindrone acetate for symptomatic peri-and postmenopausal women: impact on depression, vasomotor symptoms, sleep, and quality of life. Menopause. 2006;13(5):780–6.
Cohen LS, Soares CN, Poitras JR, Prouty J, Alexander AB, Shifren JL. Short-term use of estradiol for depression in perimenopausal and postmenopausal women: a preliminary report. Am J Psychiatr. 2003;160(8):1519–22.
de Novaes SC, Almeida OP, Joffe H, Cohen LS. Efficacy of estradiol for the treatment of depressive disorders in perimenopausal women: a double-blind, randomized, placebo-controlled trial. Arch Gen Psychiatry. 2001;58(6):529.
Schmidt PJ, Nieman L, Danaceau MA, Tobin MB, Roca CA, Murphy JH, et al. Estrogen replacement in perimenopause-related depression: a preliminary report. Am J Obstet Gynecol. 2000;183(2):414–20. This position statement provides an excellent summary of our current understanding of the risks and benefits of HRT in relation to health and disease.
Joffe H, Petrillo LF, Koukopoulos A, Viguera AC, Hirschberg A, Nonacs R, et al. Increased estradiol and improved sleep, but not hot flashes, predict enhanced mood during the menopausal transition. J Clin Endocrinol Metab. 2011;96(7):E1044–54.
Joffe H, Hall JE, Gruber S, Sarmiento IA, Cohen LS, Yurgelun-Todd D, et al. Estrogen therapy selectively enhances prefrontal cognitive processes: a randomized, double-blind, placebo-controlled study with functional magnetic resonance imaging in perimenopausal and recently postmenopausal women. Menopause. 2006;13(3):411–22. This manuscript describes the most recent RCT of transdermal estradiol in the treatment of depression in peri- and early postmenopausal women.
Rogines-Velo MP, Heberle AE, Joffe H. Effect of medroxyprogesterone on depressive symptoms in depressed and non-depressed perimenopausal and postmenopausal women following discontinuation of transdermal estradiol therapy. Menopause. 2012;19(4):471. This is the most recent study examining the mood effects of P4 supplementation and one of the few that includes depressed women.
Yalamanchili V, Gallagher JC. Treatment with hormone therapy and calcitriol did not affect depression in elderly postmenopausal women: no interaction with estrogen and vitamin D receptor genotype polymorphisms. Menopause. 2012;19(6):697.
Demetrio FN, Rennó Jr J, Gianfaldoni A, Gonçalves M, Halbe HW, Filho AH, et al. Effect of estrogen replacement therapy on symptoms of depression and anxiety in non-depressive menopausal women. Arch Women’s Ment Health. 2011;14(6):479–86.
Morrison MF, Kallan MJ, Ten Have T, Katz I, Tweedy K, Battistini M. Lack of efficacy of estradiol for depression in postmenopausal women: a randomized, controlled trial. Biol Psychiatry. 2004;55(4):406–12.
Kornstein SG, Toups M, Rush AJ, Wisniewski SR, Thase ME, Luther J, et al. Do menopausal status and use of hormone therapy affect antidepressant treatment response? Findings from the sequenced treatment alternatives to relieve depression (STAR*D) study. J Women’s Health. 2013;22(2):121–31.
Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. J Am Med Assoc. 2002;288(3):321–33.
Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the women’s health initiative randomized trial. J Am Med Assoc. 2003;289(24):3243–53.
Schmidt P. The 2012 hormone therapy position statement of the North American Menopause Society. Menopause. 2012;19(3):257.
Santen RJ, Allred DC, Ardoin SP, Archer DF, Boyd N, Braunstein GD, et al. Postmenopausal hormone therapy: an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2010;95(7 supplement 1):s1–66.
Rossouw JE, Prentice RL, Manson JE, Wu L, Barad D, Barnabei VM, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. J Am Med Assoc. 2007;297(13):1465–77.
Manson JE, Allison MA, Rossouw JE, Carr JJ, Langer RD, Hsia J, et al. Estrogen therapy and coronary-artery calcification. N Engl J Med. 2007;356(25):2591–602.
Canonico M, Oger E, Plu-Bureau G, Conard J, Meyer G, Lévesque H, et al. Hormone therapy and venous thromboembolism among postmenopausal women impact of the route of estrogen administration and progestogens: the ESTHER study. Circulation. 2007;115(7):840–5.
Smith NL, Blondon M, Wiggins KL, Harrington LB, van Hylckama VA, Floyd JS, et al. Lower risk of cardiovascular events in postmenopausal women taking oral estradiol compared with oral conjugated equine estrogens. JAMA Intern Med. 2014;174(1):25–31.
L’hermite M. HRT optimization, using transdermal estradiol plus micronized progesterone, a safer HRT. Climacteric. 2013;16(S1):44–53.
Adams MR, Register TC, Golden DL, Wagner JD, Williams JK. Medroxyprogesterone acetate antagonizes inhibitory effects of conjugated equine estrogens on coronary artery atherosclerosis. Arterioscler Thromb Vasc Biol. 1997;17(1):217–21.
Goodman MP. Are all estrogens created equal? A review of oral vs. transdermal therapy. J Women’s Health. 2012;21(2):161–9.
Wharton W, Gleason CE, Miller VM, Asthana S. Rationale and design of the Kronos Early Estrogen Prevention Study (KEEPS) and the KEEPS Cognitive and Affective sub study (KEEPS Cog). Brain Res. 2013;1514:12–7. This manuscript summarizes the rationale and design of the cognitive and affective substudy of the Kronos Early Estrogen Prevention Study (KEEPS Cog), an RCT evaluating the mood benefits of conjugated equine estrogen and transdermal estradiol. In doing so, it summarizes many of the key issues that are currently of interest in the field of perimenopausal depression treatment.
Acknowledgments
This work was supported by NIH grant RO1-MH087619. Dr. Gordon is also the recipient of a Postdoctoral Fellowship of the Fonds de la Recherche du Québec–Santé (FRQS).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Jennifer L. Gordon has received a grant from the Fonds de la Recherche du Québec – Santé (FRQS).
Susan S. Girdler has received a grant from the National Institute of Health, R01-MH087619.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Women’s Mental Health
Rights and permissions
About this article
Cite this article
Gordon, J.L., Girdler, S.S. Hormone Replacement Therapy in the Treatment of Perimenopausal Depression. Curr Psychiatry Rep 16, 517 (2014). https://doi.org/10.1007/s11920-014-0517-1
Published:
DOI: https://doi.org/10.1007/s11920-014-0517-1