Abstract
Posttraumatic stress disorder (PTSD) is common in primary care but it is frequently not detected or treated adequately. There is insufficient evidence to recommend universal screening for PTSD in primary care, but clinicians should remain alert to PTSD among patients exposed to trauma, and among those with other psychiatric disorders, irritable bowel syndrome, multiple somatic symptoms and chronic pain. A two-stage process of screening (involving the PC-PTSD), and, for those with a positive screen, a diagnostic evaluation (using the PTSD-Checklist), can detect most patients with PTSD with few false positives. Evidence-based recommendations are provided for treatment in primary care or referral to mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
PTSD is common in primary care settings. The best estimates of prevalence of current PTSD are 6 % to 10 % in civilian primary care [1–3] and 11 % to 20 % in Department of Veterans Affairs (VA) primary care settings [4, 5]. Like persons who present with PTSD in psychiatric settings, persons with PTSD in primary care are likely to have other psychiatric disorders, including depression [6], substance abuse [7] and other anxiety disorders [8]. PTSD is also associated with long-term functional impairment even after remission [9•].
Despite its prevalence and seriousness, PTSD is frequently not detected or treated adequately by primary care clinicians [3, 10, 11]. The purpose of this article is to provide an evidence-based update on three key issues in the management of PTSD among adults in primary care: screening, diagnosis and treatment.
Screening
Screening Tests for PTSD
To make it easier for primary care clinicians to assess PTSD, given the time constraints in primary care, a significant amount of work has been devoted to development of screening tests that are brief and accurate for detection of PTSD in primary care settings. Six screening tests have been evaluated in primary care settings (Table 1).
Prior to 2010, the only screening test that had been evaluated in more than one primary care setting was the PC-PTSD [12–14]. Prins and colleagues reported a sensitivity of 78 % and a specificity of 87 % for the PC-PTSD (corresponding to a calculated positive likelihood ratio (LR+) of 6.0 and negative likelihood ratio (LR-) of 0.3 in a VA primary care sample, using a cutoff of 3 (out of 4) positive responses. Gore and colleagues reported a sensitivity of 70 % and specificity of 92 % (LR+8.8, LR- 0.3) in a military health setting serving active duty military and their family members, using the same cutoff. Oiumette and colleagues reported very different figures for sensitivity (45 %) and specificity (96 %) for the PC-PTSD in a VA sample [13]; however, the validity of their findings is questionable because the criterion standard was clinician identification of PTSD during routine care, a method that has been shown to result in detection of less than half the cases of PTSD in VA primary care settings [5].
It is unclear whether Prins’ and Ouimette’s findings apply to civilian primary care populations, where the prevalence, duration and spectrum of severity of PTSD may be different. Although it can be shown analytically that positive predictive value and negative predictive value are influenced by prevalence while sensitivity, specificity and likelihood ratios are not, there is growing literature demonstrating that, in the real world, the sensitivity, specificity and likelihood ratios for a test can vary dramatically across populations with different disease prevalences [15].
To assess the accuracy of the PC-PTSD (and other screening tests described below) in civilian primary care, Freedy and colleagues recruited a sample of 411 patients drawn from an academic Family Practice in Charleston, South Carolina [16•]. They reported a sensitivity of 85 %, specificity of 82 %, LR+ of 4.7 and LR- of 0.2 for the PC-PTSD. However, the diagnosis of PTSD was based on interviews by non-clinicians who had received only two one-hour training sessions, and who administered a diagnostic interview (the Clinician-Administered PTSD Scale, CAPS) that was designed for clinicians. The reported prevalence of PTSD (32 %) was much higher than other estimates of PTSD in primary care, suggesting that a substantial number of patients included in the PTSD group may have been false positives. This could have led to falsely high estimates of sensitivity, specificity, and the positive likelihood ratio and a falsely low estimate of the negative likelihood ratio.
Two scales, Breslau’s seven-item PTSD screen [17] and the SPAN [18], were evaluated in VA primary care settings [19, 20], and later, in Freedy’s civilian primary care sample. As shown in Table 1, the positive and negative likelihood ratios for Breslau’s scale were similar in Kimerling’s VA sample and Freedy’s civilian primary care sample. Likewise, the likelihood ratios for the SPAN were similar in Yeager’s VA sample and Freedy’s civilian primary care sample. The cautions about Freedy’s results for the PC-PTSD also apply to Freedy’s results for Breslau’s PTSD screen and the SPAN.
Three other screening tests (Gerrity’s 4-item PTSD Screen [21], the Abbreviated PTSD Checklist [22] and the Single Item PTSD Screen [14]) have all been tested in only one VA or military primary care setting; their operating characteristics are shown in Table 1.
In summary, there is moderate evidence that the PC-PTSD has good accuracy as a screening test in VA and military primary care settings, using a cutoff of three positive responses, based on similar findings across two studies. Further research is needed to confirm its accuracy in civilian primary care settings. There is insufficient evidence, based on the research to date, to recommend any of the other screening tests shown in Table 1; none of them have higher positive likelihood ratios or lower negative likelihood ratios than the PC-PTSD and each of them has been evaluated in only one study, not counting the Freedy study.
Screening Tests for Multiple Psychiatric Disorders Including PTSD
Because multiple psychiatric disorders other than PTSD are common in primary care, several authors have developed instruments to screen for multiple psychiatric disorders in primary care, including PTSD. The advantages of multi-disorder screeners are that patients frequently have more than one disorder and the use of a multi-disorder screener is more efficient and practical than multiple single-disorder instruments.
Houston and colleagues developed the Provisional Diagnostic Instrument-4 Anxiety (PDI-4A) to screen for multiple psychiatric disorders, including PTSD [23•]. The PDI-4A has 22 items, and includes only one item (disturbing memories or dreams related to previous trauma) for PTSD. The PDI-4A was reported to have a sensitivity of 71 % and specificity of 72 %. These results are weaker than most of the dedicated PTSD screening instruments, not surprisingly because it has only one item for PTSD. Only 38.2 % of persons who were screened were assessed with a diagnostic interview, raising concerns that the estimated indicators of accuracy are biased. Accordingly, the PDI-4A cannot be recommended at this time.
Gaynes and colleagues developed the My Mood Monitor (M-3), a 27-item instrument, including four items for PTSD, to screen for major depressive disorder, generalized anxiety disorder, panic disorder, social anxiety disorder, obsessive compulsive disorder, bipolar spectrum disorder and PTSD [24••]. In a study of 723 patients recruited from a single academic family practice (89 % of whom completed the diagnostic interview with the MINI by evaluators blinded to the results of the M-3), the reported operating characteristics were: sensitivity 88 %; specificity 76 %; LR+3.7; LR- 0.2. The estimated accuracy of the M-3 is comparable in magnitude to dedicated PTSD screening instruments and is estimated with a high degree of precision. The M-3 is a promising new instrument for screening multiple disorders, including PTSD, in primary care; however, because the findings are based on one study conducted in a single primary care site, the findings should be confirmed in multiple primary care settings before the instrument can be recommended for widespread use in clinical settings.
Should Universal Screening for PTSD be Implemented in Primary Care?
There are standard criteria for assessing whether screening should be implemented in clinical care [25, 26•]. Development of an accurate screening test that is acceptable to patients and clinicians is a necessary but not sufficient condition for implementing screening. Perhaps the most important criterion is that early detection, through screening, must lead to improved outcomes, compared to detection through routine clinical care [27].
It is sometimes asserted that the existence of effective treatments for PTSD means that early detection of PTSD through screening would lead to improved outcomes. However, persons with PTSD that is detected in primary care through screening may have less severe disorder than persons whose PTSD is detected through routine clinical care and may respond differently to treatments.
Determining whether early detection through screening leads to improved outcomes requires a randomized trial comparing outcomes among persons screened for PTSD to outcomes among persons who are not screened. The issue is not whether treatment improves outcome among persons who screen positive and are then diagnosed with PTSD. Rather, the key is whether outcomes are improved in an entire group of persons systematically screened for PTSD (including those with negative screening results [true negatives and false negatives] and those with positive screening result [true positives and false positives]) compared to a group a people who are not systematically screened (some of whom may be treated for PTSD in routine clinical care). No such study has been done.
In summary, despite the development of screening tests for PTSD in primary care, there is insufficient evidence to recommend universal screening for PTSD in civilian or military primary care at this time.
Screening for Psychological Trauma
Despite the devastating impact that violence can play in the lives of patients in primary care, there is no evidence that screening for trauma, such as domestic violence, reduces recurrent violence or improves health outcomes [28].
Targeted Assessment for PTSD
If universal screening is not recommended and more than half of patients with PTSD in primary care settings are not identified by their primary care clinicians, what should be done to improve overall care of PTSD in primary care?
The UK National Institute for Health and Clinical Excellence does not recommend screening for depression but they do suggest a middle path. They recommend that clinicians “Be alert to possible depression (particularly in people with a past history of depression or a chronic physical health problem with associated functional impairment) and consider asking people who may have depression” questions to screen for depression [29]. Similarly, in the absence of evidence to recommend universal screening for PTSD in all primary care patients, it is prudent to recommend that a primary care clinician consider initiating evaluation for PTSD among persons who are at higher risk of PTSD if the clinician is capable of treating persons with PTSD appropriately or referring for specialist management. Persons at higher risk of PTSD in primary care include persons recently exposed to psychological trauma, including acute medical conditions that developed unexpectedly and are associated with high risk of death, such as myocardial infarction and persons with: 1) other psychiatric disorders, particularly depression, other anxiety disorders and substance abuse [21, 30]; 2) irritable bowel syndrome [31]; 3) chronic pain [32]; 4) multiple somatic symptoms [33, 34].
Diagnosis of PTSD in Primary Care
A diagnostic interview is considered the gold standard for diagnosis of psychiatric disorders but is not feasible during an office visit in primary care. Based on the belief that primary care clinicians may not be able to diagnose or optimally treat PTSD, some have recommended that primary care clinicians administer a screening test if PTSD is suspected and then refer patients who screen positive to mental health for further evaluation [35•].
Others have recommended that primary care clinicians use a two-stage screening and diagnosis process, in which clinicians first administer a screening test and then administer a self-report diagnostic instrument to patients who screen positive. For example, the Re-Engineering Systems of Primary Care Treatment in the Military (RESPECT-MIL) program, designed to improve detection and treatment of PTSD in the military, recommends that primary care clinicians screen patients with the PC-PTSD and then administer the PTSD-Checklist (PCL) to patients who have positive screening tests [36].
Although there are many self-report instruments for assessing PTSD, the PCL is the most widely used self-report instrument used in research and clinical settings for assessment of PTSD [37]. There are three versions of the PCL, the PCL-C (Civilian version, referring to “stressful experiences”), the PCL-M (Military version, referring to “stressful military experiences”), and the PCL-S (Specific version, referring to a specific identified “stressful experience”). Because it is framed most generally, the PCL-C has been the most widely used form of the PCL, even in military or VA settings. The use of “PCL” here refers to the PCL-C unless specified otherwise.
Its accuracy in primary care has been assessed in four studies, all of which were conducted in VA primary care settings [12, 19, 38, 39]. Although each of the studies recommended a different cutoff point, McDonald and colleagues calculated the accuracy of the PCL from data in those studies using a common cutoff of 50 to define a positive test [40•]. The range for positive likelihood ratios was 6.5 to 10.6 and the range for negative likelihood ratios was 0.46 to 0.65, indicating that the PCL, using the cutoff of 50, is much better at ruling in than ruling out PTSD.
Although the RESPECT-MIL program recommends using a cutoff of 30 for diagnosis of PTSD (with a score of 30–49 defining mild PTSD) in the military, the cutoff score of 50 is perhaps more reasonable when used as part of a two-stage process. Assuming a prevalence of current PTSD of 15 % in VA primary care settings, the probability of PTSD, given a positive PC-PTSD screen is 51 %. Assuming an LR+ of 8.5 and an LR- of 0.55 (mid-points for the range of LR+and LR- for the four studies conducted in VA primary care), the probability of PTSD for someone in VA primary care who has a positive PC-PTSD screen and a positive (i.e., 50 or greater) PCL, is 90 % and the probability of PTSD for someone who has a positive PC-PTSD and a negative PCL, is 36 %. While the percentage of persons with PTSD who would be missed using this approach (36 %) is relatively high, the percentage of persons who would be treated for PTSD unnecessarily (10 %) is low. One option to mitigate the possibility of missing PTSD would be to refer patients who are believed to be at high risk of PTSD and screen positive on the PC-PTSD but negative on the PCL to mental health clinicians for a diagnostic interview.
There are no data available from studies with low risk of bias on the accuracy of the PCL in civilian primary care.
Treatment of PTSD in Primary Care
Randomized trials and meta-analyses of those trials have identified medications and psychological treatments that reduce symptoms and increase remission among persons diagnosed with PTSD [41, 42]. However, because none of the trials recruited patients from primary care settings, it is unclear whether the findings are applicable to patients in primary care. It is possible that the severity, presenting symptoms, preference for treatment, and therefore, response to treatment might be different in patients with PTSD who present in primary care than in those who present in mental health settings.
Gaynes and colleagues addressed this issue for patients with major depressive disorder in the STAR*D trial [43]. In a randomized trial with a large sample drawn from 14 US regional centers including 18 primary care (N = 1091) and 23 specialty mental health sites (N = 1,785), depressed patients in primary care had the same response rate and remission rate as depressed patients from specialty mental health settings. They concluded, “identical remission and response rates can be achieved in primary and specialty settings when identical care is provided.” Those findings are likely to be applicable to PTSD in primary care versus specialty mental health settings.
The key issue, though, is guaranteeing “identical care” in the real world, outside of a randomized trial, given that PTSD is frequently not detected or treated optimally in primary care. For that reason, some have recommended that primary care clinicians refer all patients who have positive screening tests to specialty mental health providers for further evaluation and treatment [35•]. However, many patients seek care for mental health problems in primary care because of the stigma of mental health problems and/or difficulty accessing mental health services due to financial, geographical or logistical barriers [44, 45]. Referring all patients with possible PTSD to mental health care may decrease the chance that they will receive adequate care, if they prefer treatment in primary care or cannot access specialty mental health care.
Collaborative Care for PTSD
Collaborative care is an intervention that uses case managers to coordinate care by primary care clinicians and mental health specialists. Based on strong evidence that collaborative care is more effective than usual care in the management of depression in primary care [46], collaborative care interventions for management of PTSD in primary care have been developed and evaluated in several studies.
Schnurr and colleagues randomized 195 persons with PTSD recruited from primary care clinics at four VA health care facilities to usual care or the Three Component Model (3CM), a collaborative care intervention, plus usual care [47••]. Participants randomized to the collaborative care intervention were more likely to have filled an antidepressant prescription but there were no differences in PTSD symptoms or depression symptoms between the two groups at 6 months. The authors suggested that the lack of benefit may have been due to low levels of primary care physician involvement in the intervention or the chronicity of PTSD in VA patients. There was low fidelity to the intervention, but fidelity was not associated with outcome.
Roy-Byrne and colleagues compared the effectiveness of an intervention (Coordinated Anxiety Learning and Management, CALM) to usual care for the treatment of any one of the four most common anxiety disorders (panic disorder (PD), generalized anxiety disorder (GAD), social anxiety disorder (SAD) and PTSD) among 1004 patients recruited from 17 civilian primary care settings in three states [48••]. CALM included choice of medication or cognitive behavior therapy (CBT), a computer program to facilitate delivery of CBT in primary care by non-clinicians care managers, and a collaborative care component. There were small to moderate effect sizes, based on differences between CALM and usual care in disorder-specific outcome measures, favoring the intervention, for GAD, PD and SAD at one or more of the three time points (6, 12 and 18 months). The effect sizes for PTSD for the three time points were comparable in magnitude and direction to the effect sizes for the other disorders; however, the 95 % confidence intervals were wide (because of the small number of participants with PTSD) and included the null value of 0. I believe that the best interpretation of the data is that the intervention was as effective for PTSD as it was for the other disorders, though we have less confidence in magnitude of the effect.
Engel and colleagues [36] and Corso and colleagues [49] reported large improvements in PTSD symptoms from baseline to post-intervention for collaborative care interventions in military settings, but did not include control groups. A substantial number of articles have described efforts at increasing integration between primary care and mental health, but none were randomized and none reported patient outcomes [50–54]. Zatzick and colleagues reported significantly higher PTSD response and remission rates for acutely injured trauma survivors randomized recruited from inpatient trauma surgery services to a collaborative care intervention, compared to usual care [55••]. It is unclear whether Zatzick’s findings are generalizable to primary care. Possemato recently conducted a thoughtful review of interventions, such as internet based psychotherapy, that have the potential to be useful for treatment of PTSD in primary care but not have yet been tested [56••].
In summary, one randomized trial, in VA primary care, showed no difference in PTSD symptoms between a collaborative care intervention and usual care and the other trial, in civilian primary care, showed a moderate reduction in PTSD symptoms in persons randomized to a multi-component intervention including collaborative care, though that effect was estimated imprecisely and is compatible with no reduction or even a small increase in PTSD symptoms. There is, therefore, insufficient evidence to recommend that collaborative care be implemented to improve management of PTSD in civilian or VA primary care settings at this time. Because collaborative care is effective in the treatment of depression in primary care and PTSD among injured patients from trauma surgery settings, there is reason to believe that collaborative care may be effective for PTSD in primary care if the intervention can be tweaked to incorporate the unique issues in primary care. Further research in this area is strongly needed.
Management of PTSD in Primary Care: Putting it All Together
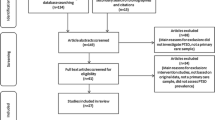
Evaluation: Patients Who Do Not Volunteer Symptoms of PTSD
An algorithm for evaluation of PTSD in primary care is shown in Fig. 1. The algorithm is based on evidence, if available (e.g., routine screening for PTSD is not recommended) and clinical judgment for those areas for which there is insufficient evidence (e.g., referring to Psychiatry for further evaluation those patients for whom clinical suspicion is high but the PCL is negative).
Among patients who do not report PTSD symptoms, primary care clinicians should remain alert to the possibility of PTSD for those with recent or remote trauma, and to those with other psychiatric disorders, multiple somatic symptoms, irritable bowel syndrome or chronic pain. If clinically appropriate, the clinician should raise concern with the patient that his/her symptoms may be related to previous upsetting events and discuss the option of having the patient take the brief 4-item PC-PTSD. Clinicians should reassure patients who decline that those issues can always be revisited at another time.
Patients who agree to take the PC-PTSD and endorse three or more items on the PC-PTSD should be informed that their results indicate that their responses may indicate a problem, but that further evaluation is needed. At that point, it can be useful to empathize with the patient about one or more of the positive responses on the PC-PTSD (“I’m sorry that you have felt numb or detached from others.”) [35•]. In most cases, patients who endorse two or fewer items on the PC-PTSD should be informed that their results do not indicate a problem related to previous upsetting events. However, if a patient spontaneously reports an event, such as rape, that is highly traumatic to most people, but has a negative PC-PTSD, it may be useful to consider a referral to a mental health provider. Primary care clinicians should not attempt to explore the trauma(s) that have produced symptoms and should reassure patients of that.
Patients who have positive PC-PTSD screens should be administered the PCL-C (Civilian version). Based on a higher specificity of a higher cutoff point, a score of 50 or greater should be considered a positive PCL. Although use of the PCL with a cutoff threshold does not require that patients separately endorse functional impairment, a one-item functional assessment, such as the one from the PHQ-9, may reduce the possibility of treating false positives for patients whose scores are near 50: “How difficult have these symptoms made it for you to do your work, take care of things at home or get along with other people?”[57]. Patients should also be asked about suicide and about ongoing threats. If a patient is in danger, the most important priority is safety.
Patients who have a PCL less than 50, should be informed that they probably do not have PTSD at that time. If there is a high risk for PTSD or strong clinical suspicion that the patient has PTSD, mental health referral for a diagnostic interview is indicated.
Evaluation: Patients Who Volunteer Symptoms of PTSD
Patients who voluntarily report some symptoms of PTSD should be evaluated initially with the PC-PTSD, and, if positive, with the PCL.
Treatment
If the patient has a positive PCL, the clinician should discuss the diagnosis of PTSD and emphasize that there are good treatments available. Clinicians who feel comfortable managing medication treatment of patients with PTSD should explore the patient’s preference for psychological treatment or medication treatment. Patients who prefer psychological treatments should be referred for one of the evidence-based psychotherapies. Patients who prefer medication treatment and do not otherwise meet criteria for referral to psychiatry should be treated with one of the medications effective for treatment of PTSD. A recent meta-analysis showed that fluoxetine, paroxetine, sertraline, topiramate, and venlafaxine were effective for improving PTSD symptoms and paroxetine and venlafaxine for inducing remission [58••].
Patients should be seen within the first week or two of starting treatment, even though they are unlikely to have responded to medication treatment by that time. They almost always have questions about the medication (e.g., adverse effects); giving them an opportunity to have their questions answered may promote long-term adherence. A clinical response, defined as a decrease of 5–10 points on the PCL, should be evident within 6–8 weeks and the dose of medication should be increased if there is no response by that time [59•]. Patients should be treated for 12 months once a response has been obtained.
Referral to psychiatry should be considered when the diagnosis is in doubt, if the patient has psychosis or is acutely suicidal, or if the patient does not respond to one of the medications for which there is evidence of effectiveness.
Conclusion
PTSD is a common and disabling mental illness in primary care. Although there is insufficient evidence to recommend universal screening in primary care, clinicians should remain alert to clinical situations that increase the risk of PTSD. Most of the medications that are effective for the treatment of PTSD are used frequently by primary care clinicians to treat depression in primary care. There is insufficient evidence to recommend implementation of collaborative care for treatment of PTSD at this time, but the existing evidence suggests that further research should be done.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Thulesius H, Alveblom AK, Hakansson A. Post-traumatic stress associated with low self-rated well-being in primary care attenders. Nord J Psychiatr. 2004;58(4):261–6.
Stein MB, McQuaid JR, Pedrelli P, et al. Posttraumatic stress disorder in the primary care medical setting. Gen Hosp Psychiatr. 2000;22(4):261–9.
Taubman-Ben-Ari O, Rabinowitz J, Feldman D, et al. Post-traumatic stress disorder in primary-care settings: prevalence and physicians' detection. Psychol Med. 2001;31(3):555–60.
Frueh BC, Grubaugh AL, Yeager DE, et al. Delayed-onset post-traumatic stress disorder among war veterans in primary care clinics. Br J Psychiatry. 2009;194(6):515–20.
Magruder KM, Yeager DE. Patient factors relating to detection of posttraumatic stress disorder in Department of Veterans Affairs primary care settings. J Rehabil Res Dev. 2008;45(3):371–81.
Campbell DG, Felker BL, Liu CF, et al. Prevalence of depression-PTSD comorbidity: implications for clinical practice guidelines and primary care-based interventions. J Gen Intern Med. 2007;22(6):711–8.
Zlotnick C, Bruce SE, Weisberg RB, et al. Social and health functioning in female primary care patients with post-traumatic stress disorder with and without comorbid substance abuse. Compr Psychiatr. 2003;44(3):177–83.
Gros DF, Frueh BC, Magruder KM. Prevalence and features of panic disorder and comparison to posttraumatic stress disorder in VA primary care. Gen Hosp Psychiatr. 2011;33(5):482–8.
• Westphal M, Olfson M, Gameroff MJ, et al. Functional impairment in adults with past posttraumatic stress disorder: findings from primary care. Depress Anxiety. 2011;28(8):686–95. Patients in primary care with PTSD that has resolved clinically continue to have functional impairment after resolution of PTSD symptoms.
Kroenke K, Spitzer RL, Williams JB, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–25.
Liebschutz J, Saitz R, Brower V, et al. PTSD in urban primary care: high prevalence and low physician recognition. J Gen Intern Med. 2007;22(6):719–26.
Prins A, Ouimette P, Kimerling R, et al. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatr. 2003;9(1):9–14.
Ouimette P, Wade M, Prins A, et al. Identifying PTSD in primary care: comparison of the Primary Care-PTSD screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ). J Anxiety Disord. 2008;22(2):337–43.
Gore KL, Engel CC, Freed MC, et al. Test of a single-item posttraumatic stress disorder screener in a military primary care setting. Gen Hosp Psychiatr. 2008;30(5):391–7.
Leeflang MM, Bossuyt PM, Irwig L. Diagnostic test accuracy may vary with prevalence: implications for evidence-based diagnosis. J Clin Epidemiol. 2009;62(1):5–12.
• Freedy JR, Steenkamp MM, Magruder KM, et al. Post-traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010;27(6):615–24. This study evaluated screening tests for PTSD in civilian primary care but the criterion standard that was used was problematic, raising concerns about the validity of the findings.
Breslau N, Peterson EL, Kessler RC, et al. Short screening scale for DSM-IV posttraumatic stress disorder. Am J Psychiatry. 1999;156(6):908–11.
Meltzer-Brody S, Churchill E, Davidson JR. Derivation of the SPAN, a brief diagnostic screening test for post-traumatic stress disorder. Psychiatr Res. 1999;88(1):63–70.
Yeager DE, Magruder KM, Knapp RG, et al. Performance characteristics of the posttraumatic stress disorder checklist and SPAN in Veterans Affairs primary care settings. Gen Hosp Psychiatr. 2007;29(4):294–301.
Kimerling R, Trafton JA, Nguyen B. Validation of a brief screen for Post-Traumatic Stress Disorder with substance use disorder patients. Addict Behav. 2006;31(11):2074–9.
Gerrity MS, Corson K, Dobscha SK. Screening for posttraumatic stress disorder in VA primary care patients with depression symptoms. J Gen Intern Med. 2007;22(9):1321–4.
Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther. 2005;43(5):585–94.
• Houston JP, Kroenke K, Davidson JR, et al. PDI-4A: an augmented provisional screening instrument assessing 5 additional common anxiety-related diagnoses in adult primary care patients. Postgrad Med. 2011;123(5):89–95. This study reports the psychometric properties of a multi-disorder screening instrument for PTSD, but it only included one item for PTSD.
•• Gaynes BN, DeVeaugh-Geiss J, Weir S, et al. Feasibility and diagnostic validity of the M-3 checklist: a brief, self-rated screen for depressive, bipolar, anxiety, and post-traumatic stress disorders in primary care. Ann Fam Med. 2010;8(2):160–9. The M-3 is a very promising multi-disorder screening instrument that has strong psychometric properties but needs additional validation in multiple primary care sites.
Andermann A, Blancquaert I, Beauchamp S, et al. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull World Health Organ. 2008;86(4):317–9.
• Harris R, Sawaya GF, Moyer VA, et al. Reconsidering the criteria for evaluating proposed screening programs: reflections from 4 current and former members of the U.S. Preventive services task force. Epidemiol Rev. 2011;33(1):20–35. This article critically reviews guidelines for adopting screening programs and proposes new guidelines.
O'Connor EA, Whitlock EP, Beil TL, et al. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med. 2009;151(11):793–803.
MacMillan HL, Wathen CN, Jamieson E, et al. Screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2009;302(5):493–501.
UK National Institute for Health and Clinical Excellence. Depression in adults: The treatment and management of depression in adults. 2009. Available at http://publications.nice.org.uk/depression-in-adults-cg90. Accessed December 2012.
Staiger PK, Thomas AC, Ricciardelli LA, et al. Identifying depression and anxiety disorders in people presenting for substance use treatment. Med J Australia. 2011;195(3):S60–3.
Schur EA, Afari N, Furberg H, et al. Feeling bad in more ways than one: Comorbidity patterns of medically unexplained and psychiatric conditions. J Gen Intern Med. 2007;22(6):818–21.
Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and post-traumatic stress disorder. J Rehabil Res Dev. 2003;40(5):397–405.
Aragona M, Catino E, Pucci D, et al. The relationship between somatization and posttraumatic symptoms among immigrants receiving primary care services. J Trauma Stress. 2010;23(5):615–22.
Escalona R, Achilles G, Waitzkin H, et al. PTSD and somatization in women treated at a VA primary care clinic. Psychosomatics. 2004;45(4):291–6.
• US Department of Veteran Affairs National Center for PTSD. PTSD Screening and Referral: For Health Care Providers. Available at http://www.ptsd.va.gov/professional/pages/screening-and-referral.asp. Accessed December 2012. This web site provides useful and practical advice for primary care clinicians on how to discuss PTSD screening test results with patients.
Engel CC, Oxman T, Yamamoto C, et al. RESPECT-Mil: feasibility of a systems-level collaborative care approach to depression and post-traumatic stress disorder in military primary care. Mil Med. 2008;173(10):935–40.
Elhai JD, Gray MJ, Kashdan TB, et al. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects?: A survey of traumatic stress professionals. J Trauma Stress. 2005;18(5):541–5.
Lang AJ, Laffaye C, Satz LE, et al. Sensitivity and specificity of the PTSD checklist in detecting PTSD in female veterans in primary care. J Trauma Stress. 2003;16(3):257–64.
Dobie DJ, Kivlahan DR, Maynard C, et al. Screening for post-traumatic stress disorder in female Veteran's Affairs patients: validation of the PTSD checklist. Gen Hosp Psychiatr. 2002;24(6):367–74.
• McDonald SD, Calhoun PS. The diagnostic accuracy of the PTSD Checklist: A critical review. Clin Psychol Rev. 2010;30(8):976–87. This is an excellent review of the psychometric properties of the PTSD Checklist, informed by the principles of clinical epidemiology.
Bisson JI, Ehlers A, Matthews R, et al. Psychological treatments for chronic post-traumatic stress disorder. Systematic review and meta-analysis. Br J Psychiatry. 2007;190:97–104.
Stein DJ, Ipser JC, Seedat S. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews: Wiley. 2006.
Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23(5):551–60.
Davis RG, Ressler KJ, Schwartz AC, et al. Treatment barriers for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. J Trauma Stress. 2008;21(2):218–22.
Pietrzak RH, Johnson DC, Goldstein MB, et al. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatr Serv. 2009;60(8):1118–22.
Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10, CD006525.
•• Schnurr PP, Friedman MJ, Oxman TE, et al. RESPECT-PTSD: re-engineering systems for the primary care treatment of PTSD, a randomized controlled trial. J Gen Intern Med. 2013;28(1):32–40. This collaborative care intervention for PTSD increased utilization but it did not change remission or response rates for PTSD.
•• Roy-Byrne PP, Craske MG, Sullivan G, et al. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303(19):1921–8. A multi-component intervention, including collaborative care, for panic disorder, generalized anxiety disorder, social anxiety disorder and PTSD, improved response and remission rates for all four disorders, though the strength of the effect is less certain for PTSD than for other disorders.
Corso KA, Bryan CJ, Morrow C, et al. Managing posttraumatic stress disorder symptoms in active-duty military personnel in primary care settings. J Men Health Counseling. 2009;31:119–36.
Kaltman SI, Pauk J, Alter CL. Meeting the mental health needs of low-income immigrants in primary care: a community adaptation of an evidence-based model. Am J Orthopsychiatr. 2011;81(4):543–51.
Zivin K, Pfeiffer PN, Szymanski BR, et al. Initiation of Primary Care-Mental Health Integration programs in the VA Health System: associations with psychiatric diagnoses in primary care. Med Care. 2010;48(9):843–51.
Possemato K, Ouimette P, Lantinga LJ, et al. Treatment of Department of Veterans Affairs primary care patients with posttraumatic stress disorder. Psychol Serv. 2011;8(2):82–93.
Seal KH, Cohen G, Bertenthal D, et al. Reducing barriers to mental health and social services for Iraq and Afghanistan veterans: outcomes of an integrated primary care clinic. J Gen Intern Med. 2011;26(10):1160–7.
Wray LO, Szymanski BR, Kearney LK, et al. Implementation of primary care-mental health integration services in the Veterans Health Administration: program activity and associations with engagement in specialty mental health services. J Clin Psychol Med Settings. 2012;19(1):105–16.
•• Zatzick D, Jurkovich G, Rivara FP, et al. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg. 2013;257(3):390–9. A collaborative care intervention among acutely injured patients recruited from trauma surgery increased response and remission rates for PTSD.
•• Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18(3):268–80. An excellent review of interventions that may be able to be adapted for use in treatment of PTSD in primary care.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
•• Jonas DE, Cusack K, Forneris CA et al. Psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD). Comparative Effectiveness Review No. 92. (Prepared by the RTI International-University of North Carolina Evidence-based Practice Center under Contract No. 290-2007-10056-I.) Publication No. 13-EHC011-EF. Rockville, MD:Agency for Healthcare Research and Quality; April 2013.
• Lang AJ, Wilkins K, Roy-Byrne PP, et al. Abbreviated PTSD Checklist (PCL) as a guide to clinical response. Gen Hosp Psychiatr. 2012;34(4):332–8. This article provides identifies numeric targets for clinical treatment response among patients with PTSD in primary care.
Conflict of Interest
Jeffrey Sonis declares that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Psychiatry in Primary Care
Rights and permissions
About this article
Cite this article
Sonis, J. PTSD in Primary Care—An Update on Evidence-based Management. Curr Psychiatry Rep 15, 373 (2013). https://doi.org/10.1007/s11920-013-0373-4
Published:
DOI: https://doi.org/10.1007/s11920-013-0373-4