Abstract
Purpose of Review
Reversible cerebral vasoconstriction syndrome (RCVS) is a disorder with distinct features: recurrent thunderclap headaches with reversible vasoconstriction of intracranial arteries. Substantial studies regarding outcomes after RCVS were conducted, showing favorable functional outcomes in most patients despite the potentially life-threatening complications of RCVS, including ischemic stroke, intracranial hemorrhage, or convexity subarachnoid hemorrhage. However, patients may report headaches after the resolution of RCVS while relative studies were scarce.
Recent Findings
Two prospective studies from different cohorts consistently revealed that RCVS recurred in at least 5% of patients. Patients with prior migraine history and patients whose thunderclap headaches are elicited by sexual activity or exertion are at higher risk for RCVS recurrence. On the other hand, several retrospective studies and case reports reported that chronic headaches are common in RCVS patients after the resolution of acute bouts. The chronic headaches after RCVS are sometimes disabling in certain patients.
Summary
Headaches after RCVS are not uncommon but usually overseen. Medical attention and examinations are warranted in patient with RCVS who reported recurrence of thunderclap headaches or chronic headaches after RCVS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
RCVS is a syndrome characterized by recurrent thunderclap headaches that clustering within 2 to 3 weeks, accompanying with vasospasm of intracranial arteries revealed by neuroimaging techniques, including computed tomography (CT) or magnetic resonance (MR) angiography, or transcranial Doppler scan. Demonstrating the reversibility of cerebral vasoconstriction is essential for diagnosis, which usually occurs within 3 months after the onset of RCVS [1,2,3,4].
In most patients, certain triggers, including defecation, exertion, bathing, coughing, and sexual activity, may elicit their thunderclap headaches during the acute phase of RCVS. Also, some patients with RCVS had identifiable secondary etiologies for RCVS, including postpartum status, exposure to vasoactive substances, and intra-/extra-cranial arterial disorders or procedures like intracranial or cervical artery dissection or stenting [5, 6]. However, despite the heterogeneity of the etiologies, some phenomena are rather similar in patients with RCVS with different ethnicities: female predominant, middle aged (40 to 50 years old), and acute, severe headaches (even if not thunderclap at onset).
RCVS is a potentially life-threatening or even fatal disorder, with possible complications including convexity subarachnoid hemorrhage, ischemic stroke, intracranial hemorrhage, and posterior reversible encephalopathy syndrome. Therefore, several studies investigated the functional outcomes of patients with RCVS. In summary, despite its potentially fatal complications, RCVS leads to favorable functional outcome in most patients [3, 7, 8]. However, a topic is often neglected when investigating the outcomes of RCVS: the headaches after RCVS. In this article, we reviewed and summarized the currently available English literature regarding the headaches that developed or recurred after RCVS.
Recurrence of RCVS
RCVS was originally considered as a monophasic disease [3, 9]; however, some scattered case reports suggested otherwise. Ursell et al [10] reported a 39-year-old woman who presented with thunderclap headaches and diffuse beading of middle cerebral arteries 5 days after giving birth to her fourth child by cesarean section. She had a history of intracranial bleeding and diffuse intracranial arteries vasospasm 32 months earlier to her second bout of RCVS, which was 9 days after she delivered her third child. She was diagnosed with postpartum cerebral angiopathy, a disorder that is now recognized as a subtype of RCVS that usually occurs in postpartum period. Also, one of the sixteen patients with benign angiopathy of the central nervous system (CNS) that Hajj-Ali et al. [11] reported in 2002 had a recurrence of RCVS 14 months after the first bout. This 43-year-old woman was also complicated with intracranial bleeding during the first bout.
The concept that RCVS may be a recurrent disorder has been established and confirmed by two cohorts [12••, 13••] (Table 1). Chen et al. prospectively recruited 168 Taiwanese patients with RCVS that had been followed for 37.5 months on average [12••]. Among these patients, nine (5.4%) were confirmed to have recurrent RCVS during the follow-up period. Biotet et al. [13••] reported a cohort of 172 French patients with RCVS who were prospectively followed for 9.2 years on average. RCVS recurred in ten patients (5.8%). Of note, there are several distinct features between the two cohorts, including the different ethnicities (Asians vs. Caucasians) and the etiologies for the initial RCVS (mostly primary in the Taiwanese cohort vs. high proportion of vasoactive substances exposure in the French cohort). However, it is quite remarkable that RCVS recurred at a similar rate despite these differences. It is also consistent that patients with recurrent RCVS usually have favored outcomes without severe complications or sequelae.
Both studies identified several risk factors for recurrent RCVS. Thunderclap headaches triggered by sexual activity or exercise during the initial RCVS presentation were reported to be significant in predicting RCVS recurrence, with hazard ratio of 5.68 [12••] and 8.4 [13••], respectively. Having a history of migraine prior to the initial RCVS presentation was also predictive of RCVS recurrence (hazard ratio = 4.5). Of note, having any complications during the initial RCVS presentation did not predict RCVS recurrence in both studies.
The recurrence rate in patients with secondary causes for RCVS who re-exposed to the same causes remained unknown. Biotet et al. [13••] reported five women with postpartum RCVS who had new pregnancies, and none of these patients had recurrent post-partum RCVS. Although the results may result from limited case numbers, it is somewhat reassuring to patients planning for subsequent pregnancies. The recurrence rate in patients who were re-exposed to the vasoactive agents, especially illicit drugs, that triggered their initial RCVS remained an unsolved but potentially significant issue.
For now, although several risk factors were identified, study that provides causalities and evidence at pathophysiological basis for recurrent RCVS is still lacking. Studies that investigate the association between recurrent RCVS and those identified risk factors are warranted.
Chronic Headache after RCVS
The acute bout of RCVS, consists of multiple and recurrent attacks of thunderclap headaches, usually lasts for 1 or 2 weeks [14]. Actually, according to the criteria of International Classification of Headache Disorders (ICHD), the clinical course of RCVS is limited within 3 months, as known as the time generally when the recovery of intracranial vasospasm requires. However, some studies (Table 2) suggest that RCVS not only causes excruciating headaches in its acute phase but also leads to chronic headaches afterward.
A retrospective study [11] of 16 patients with benign angiopathy of central nervous system (BACNS), a synonym of RCVS, investigated the clinical manifestations and outcomes of these patients. In this study, clinical status at the last visit was recorded and defined as “short-term outcome.” However, the interval from RCVS onset to when short-term outcomes were determined was not reported. Among the 16 patients, up to 44% (n = 7) of the patients reported residual headaches. Most patients with residual headaches reported that their headaches were mild in intensity, and none of them had major neurological sequelae. Another retrospective two-centered study [15••], conducted by the Cleveland Clinic Foundation and Massachusetts General Hospital in 2016, investigated the long-term outcomes of RCVS patients. Although the results may be limited by its low response rate (41.3%) and retrospective nature, this study provided valuable information regarding headaches after RCVS resolution. Fifty-three percent (24/45) of patients continued to have chronic headaches after RCVS resolution. Most of them reported that the headaches were improved in severity compared to those in the acute phase of RCVS, but they did not completely resolve. The intensity was mostly low. However, these residual headaches caused moderate to severe disability in 18% (8/45) of patients (determined by the Migraine Disability Assessment Test). Furthermore, Rozen and his colleagues [16•, 17•] reported four cases of RCVS that presented with new daily persistent headaches after RCVS onset and considered this presentation as a novel phenotype.
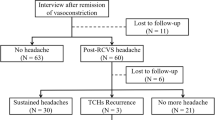
Although studies were still limited, chronic headache after RCVS has drawn more attention. It was formally included in the third edition of International Classification of Headache Disorders (ICHD-3, 2018) and was referred to as “persistent headache attributed to past RCVS” (code: 6.7.3.3) [18]. However, prospective studies that investigate the prevalence of chronic headaches after RCVS resolution are still lacking. The risk factors of chronic headaches after RCVS are urged to be identified. In our experience, patients with RCVS do develop chronic headaches after the recovery of intracranial vasospasm; part of them would need long-term medical attention due to chronic headaches that follow the acute bouts of RCVS. The occurrence of post-RCVS headache is associated with psychological distress (measured by Hospital Anxiety and Depression Scale) and prior history of migraine. Consistent with the unusual phenotype reported by Rozen and his colleagues [16•, 17•], we did recognize few patients who developed daily persistent headaches after RCVS onset.
The pathophysiology of chronic headaches after RCVS is unknown. However, several clinical studies that investigated the pathophysiology of RCVS may provide some hints. Studies showed dysfunction of autonomic system [19] and cerebral vasomotor reactivity [20] in patients with RCVS. The dysfunction persisted even after remission of cerebral vasoconstriction in some patients. These findings suggested that some patients may remain subclinically abnormal even after the resolution of RCVS, providing the physiological basis of persistent headaches after RCVS. Another possibility is that the trigeminovascular nociceptive pathway was sensitized upon the repeated attack of thunderclap headaches or by the extravasated intravascular components that leaked into the perivascular space after disruption of blood-brain barrier. Nevertheless, these hypotheses are purely speculative and await proven.
Conclusion
Headaches after RCVS, including RCVS recurrence and chronic persistent headache that developed after RCVS resolution, are not uncommon but usually overseen. Due to the potential clinical impacts on patients with RCVS, physicians should be aware of these conditions. Research regarding the pathophysiology of headaches after RCVS is lacking. Studies that elucidate the underlying mechanism of recurrent RCVS or chronic headaches after RCVS may help us demystify the pathophysiology of RCVS itself.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Chen SP, Fuh JL, Chang FC, Lirng JF, Shia BC, Wang SJ. Transcranial color Doppler study for reversible cerebral vasoconstriction syndromes. Ann Neurol. 2008;63:751–7.
Calabrese LH, Dodick DW, Schwedt TJ, Singhal AB. Narrative review: reversible cerebral vasoconstriction syndromes. Ann Intern Med. 2007;146:34–44.
Ducros A. Reversible cerebral vasoconstriction syndrome. Lancet Neurol. 2012;11:906–17.
Choi HA, Lee MJ, Choi H, Chung C-S. Characteristics and demographics of reversible cerebral vasoconstriction syndrome: a large prospective series of Korean patients. Cephalalgia. 2018;38:765–75.
Aghaebrahim A, Jadhav AP, Saeed Y, Totoraitis R, Jankowitz BT, Jovin TG, et al. Reversible cerebral vasoconstriction syndrome following carotid stenting. Neurology. 2014;83:570–1.
Rosenbloom M, Singhal A. CT angiography and diffusion-perfusion MR imaging in a patient with ipsilateral reversible cerebral vasoconstriction after carotid endarterectomy. Am J Neuroradiol. 2007;28:920–2.
Katz BS, Fugate JE, Ameriso SF, Pujol-Lereis VA, Mandrekar J, Flemming KD, et al. Clinical worsening in reversible cerebral vasoconstriction syndrome. JAMA Neurol. 2014;71:68–73.
Singhal AB, Hajj-Ali RA, Topcuoglu MA, Fok J, Bena J, Yang D, et al. Reversible cerebral vasoconstriction syndromes: analysis of 139 cases. Arch Neurol. 2011;68:1005–12.
Ducros A, Bousser M-G. Reversible cerebral vasoconstriction syndrome. Pract Neurol. 2009;9:256–67.
Ursell MR, Marras CL, Farb R, Rowed DW, Black SE, Perry JR. Recurrent intracranial hemorrhage due to postpartum cerebral angiopathy: implications for management. Stroke. 1998;29:1995–8.
Hajj-Ali RA, Furlan A, Abou-Chebel A, Calabrese LH. Benign angiopathy of the central nervous system: cohort of 16 patients with clinical course and long-term followup. Arthritis Care Res. 2002;47:662–9.
•• Chen S-P, Fuh J-L, Lirng J-F, Wang Y-F, Wang S-J. Recurrence of reversible cerebral vasoconstriction syndrome: a long-term follow-up study. Neurology. 2015;84:1552–8 This is the first prospective study which reported the recurrence rate of RCVS and risk factors for RCVS recurrence.
•• Boitet R, de Gaalon S, Duflos C, et al. Long-term outcomes after reversible cerebral vasoconstriction syndrome. Stroke. 2020;51:670–3 This prospective follow-up study of RCVS patients is consistent with Chen et al. (2015), revealing the incidence and risk factors for the recurrence of RCVS.
Chen S-P, Fuh J-L, Wang S-J, et al. Reversible cerebral vasoconstriction syndrome: current and future perspectives. Expert Rev Neurother. 2011;11:1265–76.
•• John S, Singhal AB, Calabrese L, et al. Long-term outcomes after reversible cerebral vasoconstriction syndrome. Cephalalgia. 2016;36:387–94 This retrospective study investigated the long-term outcomes of RCVS, showing that half of RCVS patients suffered from chronic headaches after resolution of acute bouts.
• Jamali SA, Rozen TD. An RCVS Spectrum disorder? New daily persistent headache starting as a single thunderclap headache (3 new cases). Headache: J Head Face Pain. 2019;59:789–94 Reference 15 and 16 are studies that reported an unusual phenotype of RCVS. There were four patients in total who presented with new daily persistent headaches after RCVS onset.
• Rozen TD, Beams JL. New daily persistent headache with a thunderclap headache onset and complete response to nimodipine (a new distinct subtype of NDPH). J Headache Pain. 2013;14:100 Reference 15 and 16 are studies that reported a unusual phenotype of RCVS. There were four patients in total who presented with new daily persistent headaches after RCVS onset.
Headache Classification Committee of the International Headache Society. The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38:1–211.
Chen S-P, Yang AC, Fuh J-L, Wang S-J. Autonomic dysfunction in reversible cerebral vasoconstriction syndromes. J Headache Pain. 2013;14:94.
Choi HA, Lee MJ, Chung C-S. Cerebral endothelial dysfunction in reversible cerebral vasoconstriction syndrome: a case-control study. J Headache Pain. 2017;18:29.
Funding
This work was supported by the Brain Research Center, National Yang-Ming University from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan (to SPC); Ministry of Science and Technology of Taiwan [MOST-108-2314-B-010-022-MY3] (to SPC); and Taipei Veterans General Hospital [V109C-139] (to SPC). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Shih-Pin Chen and Yu-Hsiang Ling declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Chronic Daily Headache
Rights and permissions
About this article
Cite this article
Ling, YH., Chen, SP. Narrative Review: Headaches After Reversible Cerebral Vasoconstriction Syndrome. Curr Pain Headache Rep 24, 74 (2020). https://doi.org/10.1007/s11916-020-00908-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s11916-020-00908-1