Abstract
Purpose of Review
Complex regional pain syndrome (CRPS) is a painful debilitating neurological condition that accounts for approximately 1.2% of adult chronic pain population. Ketamine, an NMDA receptor antagonist, is an anesthetic agent that has been used by some pain specialists for CRPS. There is a growing body of clinical evidence to support the use of ketamine in the treatment of neuropathic pain, especially CRPS. This meta-analysis study was aimed to examine the efficacy of ketamine in the treatment of CRPS.
Recent Findings
A search of Embase, Pubmed, Web of Knowledge, Cochrane, Clinical Trial.gov, and FDA.gov between Jan 1, 1950, and August 1, 2017, was conducted to evaluate ketamine infusion therapy in the treatment of CRPS. We selected randomized clinical trials or cohort studies for meta-analyses. I2 index estimates were calculated to test for variability and heterogeneity across the included studies. The primary outcome is pain relief. The effect of ketamine treatment for complex regional pain syndrome was assessed by 0–10 scale numerical rating pain score. The secondary outcome is the pain relief event rate, which is defined as the percentage of participants who achieved 30% or higher pain relief in each of the qualified studies. Our meta-analysis results showed that the Ketamine treatment led to a decreased mean of pain score in comparison to the self-controlled baseline (p < 0.000001). However, there is a statistical significance of between-study heterogeneity. The immediate pain relief event rate was 69% (95% confidence interval (CI) 53%, 84%). The pain relief event rate at the 1–3 months follow-ups was 58% (95% CI 41%, 75%).
Summary
The current available studies regarding ketamine infusion for CRPS were reviewed, and meta-analyses were conducted to evaluate the efficacy of ketamine infusion in the treatment of CRPS. Our findings suggested that ketamine infusion can provide clinically effective pain relief in short term for less than 3 months. However, because of the high heterogeneity of the included studies and publication bias, additional random controlled trials and standardized multicenter studies are needed to confirm this conclusion. Furthermore, studies are needed to prove long-term efficacy of ketamine infusion in the treatment of CRPS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Complex regional pain syndrome (CRPS) is a painful debilitating neurological condition that accounts for approximately 1.2% of adult chronic pain population [1]. The prevalence is higher in female patients than male patients with a ratio of 3 to 1 [2]. This condition often develops after a noxious event such as trauma, minor injury, and surgeries. However, the probability of developing CRPS is not related to the extent of surgery or injuries [3]. This disease typically presents with allodynia, hyperalgesia, sudomotor and vasomotor abnormalities, and trophic changes. It has a varying clinical course from a mild and self-limiting to a severe and chronic disabling disease. While patients with new onset of CRPS may resolve with aggressive treatments, chronic CRPS patients with symptoms longer than a year rarely improve. And 80% of these chronic CRPS patients are severely disabled [4].
Despite the various available interventions and medications, many patients continue to suffer severe uncontrolled pain and have poor quality of life. While the pathophysiology of CRPS is unclear, prior studies have demonstrated that the activation of N-methyl-D-aspartate (NMDA) receptor increases excitatory transmission of afferent neurons, which can lead to central sensitization and development of chronic pain [5]. Ketamine, an NMDA receptor antagonist, is an anesthetic agent that acts on glutamate binding sites. There is a growing body of clinical evidence to support the use of ketamine in the treatment of neuropathic pain, especially CRPS. This meta-analysis study was aimed to examine the efficacy of ketamine in the treatment of CRPS.
Methods
Search Strategy and Selection Criteria
This systemic review and meta-analysis is in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement. This study was registered with International Prospective Register of Systematic Reviews (Registration number CRD42017067398).
We selected relevant studies published between Jan 1, 1950, and August 1, 2017, by searching Embase, Pubmed, Web of Knowledge, Cochrane, Clinical Trial.gov, and FDA.gov with no language restrictions. We utilized the following combined text and MeSH terms as search words: “Ketamine” and “complex regional pain syndromes”. The complete search used for Pubmed was: (“Complex regional pain syndromes” [MeSH] OR “causalgia”[MeSH] OR CRPS* OR reflex sympathetic dystrophy* OR RSD* OR algodystrophy*) AND ((2, 2 Chlorophenyl 2 methylamino cyclohexanone*) OR “ketamine”[MeSH]). We considered all potentially eligible studies for review and conducted a manual search on the reference lists of key articles.
Inclusion Criteria and Data Collection
We regarded studies as eligible for inclusion if (A) they are randomized clinical trials or cohort studies. (B) Ketamine intravenous infusion was used in the treatment of complex regional pain syndrome with no restrictions of dosage and duration. (C) Pain outcomes were measured before and after ketamine treatment through validated tools such as VAS. Case reports, studies on animals, and reviews were excluded.
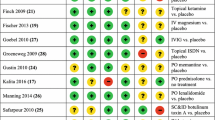
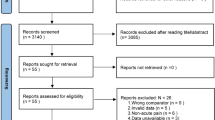
Two independent investigators (JZ, YW) reviewed study titles and abstracts. The studies that satisfied the inclusion criteria were retrieved for full text assessment. Two independent reviewers (JZ, YW) assessed risk for bias according to the PRISMA recommendations. Studies selected for detailed analysis and data extraction were analyzed by two investigators (JZ, YW) with an agreement value (κ) of 98%. Disagreements were resolved by a third investigator (DW).
We extracted the following data from the selected studies:
-
(A)
Demographic and clinical characteristics: (1) the total number of individuals, age, sex. (2) Ketamine dosage and treatment duration, side effects.
-
(B)
Pain scores at baseline, immediately after treatment, and 1–3 months after treatment.
-
(C)
The pain relief event rate (the percentage of participants who achieved 30% or higher pain relief) at immediately after treatment, and 1–3 months after treatment.
Outcome Measures and Statistical Analysis
The primary outcome is pain relief. The effect of ketamine treatment for complex regional pain syndrome was assessed by 0–10 scale numerical rating pain score (NRS) with one exception measured by 100-mm visual analogue scale [6••]. We analyzed pain score as continuous variables and reported absolute differences between arithmetic means before and after treatments.
The secondary outcome is the pain relief event rate, which is defined as the percentage of participants who achieved 30% or higher pain relief in each of the qualified studies. This analysis was used to estimate the incidence of clinically meaningful pain relief. The analysis was calculated for (1) immediate pain relief and (2) 1–3 months after treatment. Regarding the 1–3 months follow-up outcomes, we perform a meta-analysis at the time points between 1 to 3 months follow-ups after ketamine treatment. We calculated the estimates of the pain relief event rate using Stata 12.0 with a random-effect model. We chose this random-effect model because of the substantial statistical heterogeneity among the studies, and the clinical heterogeneity due to the differences in experimental designs.
We calculated estimates of the mean differences in pain scores between treatment and baseline groups by using random-effects model. We assessed the possibility of publication bias by constructing a funnel plot of each trial’s effect size against the standard error. We assessed funnel plot asymmetry using Begg’s and Egger’s tests, and defined significant publication bias as a P value < 0.05. We chose the Cochran Q test to assess heterogeneity between studies, with values greater than 50% regarded as being indicative of moderate-to-high heterogeneity. We used Stata 12.0 for statistical analysis. All meta-analyses were evaluated for heterogeneity using the chi-square-based I2 test and Q test. I2 index estimates were calculated to test for variability and heterogeneity across the included studies. If a moderate or high heterogeneity was observed, random-effects meta-analysis was conducted by the DerSimonian and Laird method. P < 0.05 was considered statistically significant.
Results
Included Studies Characteristics
We identified 82 studies, of which 15 studies were included in our analysis with data from 258 subjects [6••,7,8,9,10,11,12,13•,14,15,16,17,18,19,20] as shown in Fig. 1. All studies were published between 2002 and 2015 (Table 1). Mean treatment duration was 8.41 days (range 1 to 43.8 days). Patients had mean age of 37.34 ± 9.23 years, and mean duration of CRPS of 39.67 ± 31.61 months. Trials comprised CRSPI and CRSPII patients.
The Effect of Ketamine Treatment on Pain Score
In the pooled analysis of all 15 qualified studies, the ketamine treatment led to a decreased mean of pain score in comparison to the self-controlled baseline (p < 0.000001) as shown in Fig. 2. However, there is a statistical significance of between-study heterogeneity. In this analysis, there was evident publication bias presented by the funnel plot with Egger’s test (P < 0.05). The funnel plot was presented in Fig. 3 and publication bias was evident in all studies.
The Effect of Ketamine on Pain Relief Event Rate in CRPS
Nine of the 15 studies (a total of 159 participants) included data of pain relief event rates for the immediate after treatment period [6••,7–11, 13•,14,15]. These nine studies were used for meta-analysis to estimate the pain relief event rate in the immediately after treatment period. Seven studies (a total of 115 participants) were found to have data of pain relief event rates for the 1–3-month period after treatment [6••,7,8, 10–12, 14]. These seven studies were used to estimate the 1–3 months after treatment pain relief event rates. It should be noted that the results from these studies showed a high level of variance, which may influence the pooled estimation of incidence. Therefore, we conducted data synthesis to exclude the studies with a low score of study quality. Based on this analysis, one study [9] was excluded for the analysis of immediate incidence. After adjustment, the pooled immediate pain relief event rate was 69% (95% confidence interval (CI) 53%, 84%). (Fig. 4a) The pain relief event rate at 1–3 months follow-ups was 58% (95%CI 41%, 75%) (Fig. 4b). The squares in Fig. 4b represent effect estimates of individual studies with the 95% confidence intervals of pain relief event rate with size of squares proportional to the weight assigned to the study in the meta-analysis.
Measurements of pain relief event rates. a The forest plot for the pain relief rate at immediately after treatment. b The forest plot for pain relief event rate at 1–3 months follow-ups. All studies assessed pain relief rates according to the outcomes presented in studies collected in Table 1. Squares represent the effect estimates of individual studies with their 95% confidence intervals of prevalence. The sizes of squares are proportional to the weight assigned to the study in the meta-analysis
Discussion
CRPS is a complex medical condition that remains a challenge in our daily clinical practice. Ketamine intravenous infusion has been a promising treatment that demonstrated beneficial effect in the management of CRPS. Same as other medical treatments when first introduced to clinical practice, the effectiveness of ketamine treatment in CRPS has been studied by different research teams in various locations with various approaches. Predictably, the results from these studies are diverse. Given the complexity of this disease and the lack of effective treatments, there is a clear need in reaching a conclusion regarding the efficacy of ketamine treatment. In the hierarchy of clinical evidences, when clinical studies are ranked according to their freedom of biases, the meta-analysis studies are in the top. Considering these facts, we conducted this meta-analysis study to examine the efficacy of ketamine treatment.
Our results clearly showed a significant difference in pain relief from ketamine treatment. These results were based on the 15 eligible studies. However, we were unable to conduct a meta-analysis to compare ketamine treatment to placebo, because only one of the studies was a randomized placebo-controlled prospective trial. Most of these studies were clinical studies that compared the baseline pain scores to after ketamine treatment pain scores. Therefore, the only approach to analyze these data was to compare the pain scores before and after ketamine treatments on the same patients. Additionally, while physicians and patients focus on pain reduction, functional improvement is another crucial factor to measure treatment success. But our review did not generate enough data to conduct appropriate analysis to assess the functional improvement associated with ketamine treatment. In addition, there are other limitations in this meta-analysis such as inclusion of retrospective studies, high heterogeneity of the included trials, and publication bias, which render this study susceptible to the influence of bias.
The reduction of the pain scores after ketamine treatment in comparison to baseline was statistically significant in this study. However, the clinical importance of reduction in pain scores remains difficult to interpret. Farrar JT conducted a study in which the clinical importance of changes in pain intensity was evaluated. This study was based on data collected from on 2724 subjects in 10 placebo-controlled clinical trials of pregabalin in diabetic neuropathy, postherpetic neuralgia, chronic low back pain, fibromyalgia, and osteoarthritis. The changes of pain intensity from baseline were compared to the standard 7-point patient global impression of change (PGIC) for each subject. The PGIC is a self-report measure that reports the patient’s perception of the efficacy of treatment. A consistent relationship between the change in pain intensity and the PGIC regardless of disease type, age, sex, study result, or treatment group was found in this study. And more importantly, this study demonstrated a reduction of approximately 30% in pain intensity is an indication of clinically significant difference [21]. Therefore, we used the 30% pain relief event rates to evaluate efficacy of ketamine treatments for clinically meaning pain relief. The rate meta-analysis results showed ketamine is effective with an incidence of 69% at immediately after treatment, and 58% at 1–3 months after treatment, which proved ketamine can provide CRPS patients with clinically meaningful pain relief.
While our meta-analysis results suggested ketamine treatment is effective in short term at immediate after and 1–3 months after treatments, there is no clear evidence regarding long-term effect of the ketamine treatment. Our review found two studies that conducted long-term follow-ups at 6 months after treatment. One of these studies was Correll’s retrospective study in which 33 patients were enrolled. This study showed 31% of the patients remained pain free at 6 months after inpatient ketamine infusion. The other study was an open-label trial by Kiefer et al. This trial enrolled 20 patients with CRPS who underwent subanesthetic low-dose ketamine infusion. It showed 16 patients had complete remission at 6 months. These studies clearly suggested that ketamine may offer long-term benefit up to 6 months. However, due to the low number of patients enrolled in these studies, it is not feasible to conduct a meta-analysis to prove its long-term effect.
Adverse effects reported in these studies included anxiety, dysphoria, nightmares, hallucinations, insomnia, euphoria agitation, blurred vision, and sedation, which are all well-known common side effects of ketamine. It is worth noting that two studies reported elevation of liver enzymes. There is research to show that ketamine can induce hepatotoxicity by inducing mitochondrial impairment [22]. In Correll’s study, 4 of out of 33 patients were found to have elevated liver enzymes, all these patients’ enzyme levels returned to baseline within 20 days after discontinuation of ketamine [6••]. Goble’s study reported one case of elevated live enzymes in a group of five patients who underwent ketamine infusion for CRPS [7]. This patient’s liver enzyme level did not normalize for 2 months after ketamine infusion was stopped. In all our analyzed studies, 5 patients in a total of 258 patients developed hepatotoxicity. According to these data, the event rate of hepatotoxicity from ketamine infusion is 1.9%. However, it is possible some cases of liver dysfunction were not reported or missed in the studies, which can lead to underestimation of the event rate. Therefore, it is necessary to monitor liver enzymes prior to and during the ketamine treatment. If abnormal liver enzyme levels were detected, ketamine infusion should be promptly discontinued.
Conclusion
Patients with chronic pain secondary to CPRS who are refractory to conservative treatment modalities are left with few treatment options. Even with invasive interventions such as spinal cord stimulation and sympathetic blocks, there still remain a substantial number of patients who continue to suffer debilitating pain. Our study suggested that ketamine infusion can provide clinically effective pain relief in short term for less than 3 months. However, because of the high heterogeneity of the included trials and publication bias, additional prospective and standardized multicenter studies are needed to confirm this conclusion. In addition, more studies are needed to prove its long-term efficacy in the treatment of CRPS.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Murphy KR, Han JL, Yang S, Hussaini SM, Elsamadicy AA, Parente B, et al. Prevalence of specific types of pain diagnoses in a sample of United States adults. Pain Physician. 2017;20(2):E257–68.
de Mos M, de Bruijn AG, Huygen FJ, Dieleman JP, Stricker BH, Sturkenboom MC. The incidence of complex regional pain syndrome: a population-based study. Pain. 2007;129(1):12–20. https://doi.org/10.1016/j.pain.2006.09.008.
Veldman PH, Reynen HM, Arntz IE, Goris RJ. Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet. 1993;342(8878):1012–6. https://doi.org/10.1016/0140-6736(93)92877-V.
Schwartzman RJ, Erwin KL, Alexander GM. The natural history of complex regional pain syndrome. Clin J Pain. 2009;25(4):273–80. https://doi.org/10.1097/AJP.0b013e31818ecea5.
Bennett GJ. Update on the neurophysiology of pain transmission and modulation: focus on the NMDA-receptor. J Pain Symptom Manag. 2000;19:S2–6.
•• Correll GE, Maleki J, Gracely EJ, Muir JJ, Harbut RE. Subanesthetic ketamine infusion therapy: a retrospective analysis of a novel therapeutic approach to complex regional pain syndrome. Pain Med. 2004;5:263–75. This study reported several cases of ketamine-induced hepatotoxicity. This suggested liver functions should be monitored during ketamine infusion. If increased liver enzymes occur, ketamine infusion should be discontinued promptly.
Goebel A, Jayaseelan S, Sachane K, Gupta M, Frank B. Racemic ketamine 4.5-day infusion treatment of long-standing complex regional pain syndrome-a prospective service evaluation in five patients. Br J Anaesth. 2015;115(1):146–7. https://doi.org/10.1093/bja/aev183.
Goldberg ME, Torjman MC, Schwartzman RJ, Mager DE, Wainer IW. Pharmacodynamic profiles of ketamine (r)- and (s)- with 5-day inpatient infusion for the treatment of complex regional pain syndrome. Pain physician. 2010;13(4):379–87.
Kiefer RT, Rohr P, Ploppa A, Dieterich HJ, Grothusen J, Koffler S, et al. Efficacy of ketamine in anesthetic dosage for the treatment of refractory complex regional pain syndrome: an open-label phase II study. Pain Med. 2008;9(8):1173–201. https://doi.org/10.1111/j.1526-4637.2007.00402.x.
Kiefer RT, Rohr P, Ploppa A, Nohe B, Dieterich HJ, Grothusen J, et al. A pilot open-label study of the efficacy of subanesthetic isomeric s(+)-ketamine in refractory CRPS patients. Pain Med (Malden, Mass.). 2008;9:44–54.
Patil S, Anitescu M. Efficacy of outpatient ketamine infusions in refractory chronic pain syndromes: a 5-year retrospective analysis. Pain Medicine (Malden, Mass). 2012;13:263–9.
Kiefer R, Rohr P, Unertl K, Altemeyer KH, Grothusen J, Schwartzman RJ. Recovery from intractable complex regional pain syndrome type I (RSD) under high-dose intravenous ketamine-midazolam sedation International Research Foundation For RSD/CRPS. 2002;NEUROLOGY A474.
• Schwartzman RJ, Alexander GM, Grothusen JR, Paylor T, Reichenberger E, Perreault M. Outpatient intravenous ketamine for the treatment of complex regional pain syndrome: a double-blind placebo controlled study. Pain. 2009;147:107–15. This is the only double-blind placebo-controlled study on the topic of intravenous ketamine for CRPS. This study showed outpatient intravenous ketamine can provide pain relief.
Webster LR, Walker MJ. Safety and efficacy of prolonged outpatient ketamine infusions for neuropathic pain. Am J Ther. 2006;13(4):300–5. https://doi.org/10.1097/00045391-200607000-00004.
Dahan A, Olofsen E, Sigtermans M, Noppers I, Niesters M, Aarts L, Bauer M, Sarton E. Population pharmacokinetic-pharmacodynamic modeling of ketamine-induced pain relief of chronic pain. Eur J Pain (London). 2011;15:258–267.
Koffler SP, Hampstead BM, Irani F, Tinker J, Kiefer RT, Rohr P, et al. The neurocognitive effects of 5 day anesthetic ketamine for the treatment of refractory complex regional pain syndrome. Arch Clin Neuropsychol: Off J Natl Acad Neuropsychol. 2007;22(6):719–29. https://doi.org/10.1016/j.acn.2007.05.005.
Schilder JC, Sigtermans MJ, Schouten AC, Putter H, Dahan A, Noldus LP, et al. Pain relief is associated with improvement in motor function in complex regional pain syndrome type 1: secondary analysis of a placebo-controlled study on the effects of ketamine. J Pain: Off J Am Pain Soc. 2013;14(11):1514–21. https://doi.org/10.1016/j.jpain.2013.07.013.
Sheehy KA, Muller EA, Lippold C, Nouraie M, Finkel JC, Quezado ZM. Subanesthetic ketamine infusions for the treatment of children and adolescents with chronic pain: a longitudinal study. BMC Pediatr. 2015;15(198) https://doi.org/10.1186/s12887-015-0515-4.
Sigtermans M, Noppers I, Sarton E, Bauer M, Mooren R, Olofsen E, et al. An observational study on the effect of s+−ketamine on chronic pain versus experimental acute pain in complex regional pain syndrome type 1 patients. Eur J Pain (London). 2010;14:302–7.
Sigtermans MJ, van Hilten JJ, Bauer MC, Arbous MS, Marinus J, Sarton EY, et al. Ketamine produces effective and long-term pain relief in patients with complex regional pain syndrome type 1. Pain. 2009;145(3):304–11. https://doi.org/10.1016/j.pain.2009.06.023.
Farrar JT, Young JP Jr, La Moreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58. https://doi.org/10.1016/S0304-3959(01)00349-9.
Venancio C, Antunes L, Felix L, Rodrigues P, Summavielle T, Peixoto F. Chronic ketamine administration impairs mitochondrial complex I in the rat liver. Life Sci. 2013;93(12-14):464–70. https://doi.org/10.1016/j.lfs.2013.08.001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jianli Zhao, Yajing Wang, and Dajie Wang declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Hot Topics in Pain and Headache
Rights and permissions
About this article
Cite this article
Zhao, J., Wang, Y. & Wang, D. The Effect of Ketamine Infusion in the Treatment of Complex Regional Pain Syndrome: a Systemic Review and Meta-analysis. Curr Pain Headache Rep 22, 12 (2018). https://doi.org/10.1007/s11916-018-0664-x
Published:
DOI: https://doi.org/10.1007/s11916-018-0664-x