Abstract
Migraine pathophysiology is not completely understood and is still a matter of ongoing research. However, functional magnetic resonance imaging studies have provided, over the last few decades, notable insights into neuronal mechanisms underlying migraine. Recently, by using an innovative approach based on repetitive trigeminal painful stimulation, researchers have explored pain processing network functional changes associated with migraine and their correlations with specific migraineous clinical features. These functional changes have been demonstrated during different phases of migraine cycle. However, owing to the complexity of its neurobiology, migraine pathophysiology still has many secrets to be discovered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is one of the most common neurological diseases characterized by episodes of unilateral, throbbing and pulsating headache frequently associated with nausea, vomiting, photophobia, phonophobia, and disability [1, 2]. Although a growing body of discoveries in neurochemistry, genetics, and clinical pharmacology has significantly increased our current knowledge, the underlying mechanisms of migraine remain elusive [3]. The rapid evolution of advanced neuroimaging techniques to study human brain function, with greatly improved spatial and temporal resolution and a minimal invasiveness, has allowed us to further investigate migraine pathophysiology [4, 5]. Since the first report on blood oxygen level-dependent (BOLD) contrast [6], which is based on different magnetic characteristics of oxygenated/deoxygenated hemoglobin, many researchers have applied functional magnetic resonance imaging (fMRI) as an indirect surrogate marker of neuronal activity to study pain and migraine-related brain functional changes [7]. In BOLD-fMRI studies investigating migraine mechanisms, the headache attack might be considered such an obvious and “specific” stimulation paradigm, and BOLD changes during the headache attack could be contrasted to a baseline condition observed during interictal period [8]. Nevertheless, the main limitation of this experimental approach lies in the capture of spontaneous and unpredictable attacks of relatively short duration, such as migraine, while imaging techniques require considerable planning [9]. In the last few years, these factors have determined the selection of different study designs to better explore sensory, adaptive, and affective components of pain in healthy controls (HC) and in patients experiencing different pain conditions. Indeed, pain perception is a complex sensory experience that is processed in a network of distributed cortical areas and within this network (the so-called “pain matrix” or, more recently, “neurolimbic pain network” ) the encoding and evaluation of painful events depend crucially on the functional interplay of these regions [10, 11••]. Lately, pain functional imaging has been dominated by noxious stimulation paradigms that have been used to identify functional abnormalities in the abovementioned widespread network in patients with migraine. Since pioneer positron emission tomography studies using nitro-glycerine [12] or capsaicin [13] to elicit cranial pain in patients with migraine, various noxious stimuli have been used in different imaging studies, providing meaningful insights into the pain-processing network in migraine [14, 15]. More recently, by means of experimental tools characterized by a good-established and modifiable stimulus intensity and high-field magnetic resonance scanners, trigeminal stimulation fMRI studies have been characterized by excellent data, with high anatomical definition and good functional accuracy [16]. This review aims to address the additional insights that trigeminal stimulation fMRI studies have produced to increase the knowledge of migraine pathophysiology, and to integrate them into a more consistent and exhaustive neurobiological model of this complex disease.
Discussion
To date, it is well-known that trigemino-vascular system activation plays a key role in migraine attack phenomenon [1, 3]. The trigemino-vascular system constitutes an anatomo-functional pain signal transmitting pathway from “dura mater” vessels to brain areas involved in pain sensation (i.e., caudal brainstem or rostral regions of the cervical spinal cord) by peripheral and central fibers of pseudo-unipolar neurons of the Gasser ganglion [17]. Painful trigeminal stimulation can be considered an easy approach to explore trigeminal system. Indeed, the regions innervated by the three branches of the trigeminal nerve can be easily distinct and stimuli to activate the trigeminal system are well-identified [18]. Moreover, the trigeminal system reflects a somatotopic representation in the brain regions, and functional changes in trigeminal system can be detected at multiple levels (from trigeminal ganglion to the trigeminal nucleus and even in higher brain centers, including thalamus and somatosensory cortex) [19••]. For these peculiar characteristics, experimental trigeminal pathway activation has been extensively used to explore neural mechanisms underlying migraine during both headache attack and interictal period. Although these fMRI studies have provided capital insights into migraine-related pain processing pathways, they did not produce any firm conclusion about migraine pathogenesis as experimental trigeminal pain cannot be assimilated to spontaneous migraineous headache. In fact, it is well known that migraine attack is not merely pain, but represents a multiphasic event [20] in which the initial phase is characterized by the presence of “prodromes” or “premonitory symptoms” (PS) [21]. PS of migraine include a wide and heterogeneous variety of cognitive, psychic, and physical changes, which precede by several hours the aura in migraine with aura and the onset of pain in migraine without aura (MwoA), with a frequency that varies from approximately 30 % to 80 % [22•] of patients experiencing migraine attacks. Despite the occurrence of these symptoms in a significant majority of patients, PS have received only little attention in the literature, whereas a better understanding of their underlying mechanisms would be critical for a more detailed interpretation of migraine attack-related brain changes taking place well before the events associated with aura and headache. Therefore, by means of fMRI even at the beginning of an headache, we may not observe a functional phenomenon strictly related to migraine onset or identify the so-called “migraine generator”, but a secondary epiphenomenon, possibly reflecting (i) an anti-nociceptive activation; (ii) a reverberating pro-nociceptive mechanism; or (iii) a neuronal activity related to anticipation, expectation, or other pain-related cognitive factors [4]. Moreover, it is noteworthy that migraineous pain is more similar to visceral pain than to somatic pain elicited by experimental painful stimulation [23]. Finally, knowing that a migraine attack may begin several hours or days before the headache phase would probably impose a revision of the concepts of “interictal”, “between attacks”, and “migraine free” periods, which are usually reported in migraine studies. Despite these potential limitations, fMRI studies during painful trigeminal stimulation (see Table 1) have certainly offered a more effective way of looking into the functional dynamic of the pain processing network and its correlation with migraine clinical features.
Among the non-irrelevant number of BOLD-fMRI studies, the elegant study of Moulton et al. [24] could be considered one of the landmarks of migraine fMRI research. The hypothesis of the experiment was that pain modulatory circuits may be dysfunctional in allodynic migraineurs and that the altered pain processing, probably characterized by low levels of descending inhibition or high levels of descending facilitation, may also be detectable in the interictal period. The authors, by means of a contact thermode, determined the heat pain threshold as the average of three different evaluations in patients with migraine and HC. During BOLD-fMRI sessions, a no-painful stimulation (41 °C) and a noxious heat stimulus (pain threshold +1 °C) were applied to the side of head (i.e., on the forehead, innervated by the ophthalmic branch of the trigeminal nerve) involved during migraine attacks. During no-painful stimulation there was a significantly greater BOLD response in the dorsolateral pons in HC than in patients with migraine. Conversely, during the painful stimulation a significant activation of dorsolateral pons was observed in both patient groups. The detected brainstem area was located in the nucleus cuneiformis (NCF), a structure involved in descending pain modulation through cholinergic and glutamatergic mechanisms. NCF could be activated by noxious stimulation, but also during pain expectation, indicating that awareness of impending pain could trigger a preparatory or modulatory process in NCF. Interestingly, perception of painful stimuli did not show differences between patients with migraine and HC. Taken together, clinical and fMRI findings suggested that a central sensitization during attacks (due to reduced inhibition and/or enhanced facilitation of ascending nociceptive pathways) may be related to NCF “hypo-function” in patients with migraine. The condition of putative disinhibition/facilitation did not affect the perception of experimental stimulation during the interictal phase, but it might facilitate central sensitization during migraine attacks. The same research group has lately conducted a functional and microstructural connectivity study made up of two experiments using an identical stimulation protocol [25]. In the first one, during the BOLD-fMRI session, patients with migraine during the interictal period and HC were tested with a painful trigeminal stimulation. In the second experiment, patients with migraine, during both the ictal and interictal periods, were tested by means of the same experimental stimulation. An increased BOLD-fMRI response to trigeminal painful stimulation was observed in temporal pole (TP) and parahippocampal gyrus, centered on the entorhinal cortex (EC) in patients with migraine, during the interictal period compared with HC and during migraine attack compared with the interictal period. The following microstructural connectivity analysis, by means of diffusion tensor imaging, revealed that TP and EC showed an enhanced connectivity with different brain structures involved in pain processing. These findings shed some light on migraine mechanisms, suggesting that hyper-excitability of associative multisensory areas, such as TP and EC (during both migraine attack and the interictal period), may be related to pain circuits. Furthermore, this study clarified some brain mechanisms related to perceptual changes in olfactory and auditory processes in patients with migraine. Moreover, the correlation of signal patterns between the TP, EC, and other brains areas involved in pain processing suggests the possibility that a brain functional reorganization may be implicated in central sensitization, possibly caused by repeated migraine attacks.
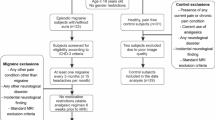
In our opinion, these studies, although of utmost importance, suffered from a methodological bias owing to the identification of an “a priori” region of interest. On the one hand, region of interest-based imaging migraine studies corroborate the functional role of a pre-identified brain structure in migraine mechanisms (e.g., the brainstem), but, on the other hand, they might be inappropriate to explore whole-brain functional changes involved in the complex migraine pathophysiology. To overcome these “caveats” we have recently explored the functional reorganization of pain-related pathways during trigeminal painful stimulation, using a whole-brain analysis approach, in drug-naïve patients with migraine during the interictal period [26]. We also concentrated on the importance of patient selection in our experiment. First, we selected only patients with MwoA. Second, in order to avoid any possible migraine related interference, all patients were migraine-free at least 3 days before MRI scan, and were interviewed 7 days after MRI scan to ascertain that they were also migraine-free in the week following the experimental day; those not fulfilling the latter criteria were excluded from the final analysis. By means of a contact thermode, a severely painful (53 °C), a moderately (51 °C) painful, and a control (41 °C) stimulus were applied randomly to the maxillary skin. Patients with MwoA and HC did not show any significant perception difference at any level of experimental stimulation. During the control trigeminal stimulus no differences in activation were observed between patients with MwoA and HC, whereas a significantly greater activation to the moderately painful heat stimulus was observed in the perigenual part of the anterior cingulate cortex (ACC), and a significantly decreased activation to the severe painful heat stimulus was observed bilaterally in the secondary somatosensory cortex. A group-by-stimulus whole-brain interaction analysis revealed a significant BOLD response in the anterior pons which was associated with higher headache-related disability, intensity of pain in the course of a migraine attack, and frequency of migraine. Although, in our experience, fMRI does not have sufficient anatomical resolution to localize individual brainstem nuclei, our findings corroborate the hypothesis that an altered pons response characterizes patients with MwoA. Moreover in our opinion, the functional reorganization of pain-related cortical areas in patients with MwoA could represent a compensatory mechanism to reduce painful input to the cortex by increasing cerebral anti-nociceptive activity. The application of a contact thermode is characterized by some limitations, such as the continuous tactile sensations due to the skin contact that could intermingle with nociceptive input, or the thermode dimensions which make placement between the subjects’ forehead and head coil of the MRI scanner to stimulate the first trigeminal nerve branch difficult. For these reasons, Stankewitz et al. [27] developed a new experimental stimulation approach based on the intranasal administration of low concentration of gaseous ammonia, which can be well-implemented within an event-related BOLD-fMRI study. Their method allows exploration of both the trigeminal pain pathway and the olfactory system; indeed, ammonia gas can produce a trigeminal nerve irritation to painful sensation, whereas rose odour can stimulate the olfactory nerve. The authors aimed to examine the hypothesis that an altered cortical information-processing, likely due to dysfunctional neuronal inhibitory circuits, may characterize migraineous brain and this may result in the so-called “lack of habituation”. This phenomenon has been extensively studied in patients with migraine with electrophysiological techniques [28, 29]. However, for the first time, processing, perception, and modulation of pain were explored by means of BOLD-fMRI in the course of repeated trigeminal painful stimulation over several days in patients with migraine [30]. Patients experiencing migraine and HC were stimulated for 8 consecutive days. BOLD-fMRI was assessed in the course of trigemino-nociceptive stimuli (ammonia) and no-noxious control stimuli (air puffs) on days 1, 8 and 90 in patients with migraine. fMRI findings demonstrated that several brain areas known to be involved in pain processing showed completely different behavior in patients with migraine compared with HC. Specifically, prefrontal cortex, ACC, red nucleus, and ventral medulla exhibited an increased activity in HC and a decreased response in patients with migraine, from the first to the eighth day. These divergent BOLD responses did not correlate with pain perception (i.e., patients with migraine and HC showed a gradual decrease of pain ratings from day 1 to day 8, which only marginally increased again on day 90). The authors suggested that altered pain processing networks may explain the dysfunctional neuronal filters of sensory input in patients with migraine, likely due to repetitive migraine attacks. The role of recurring headache attacks in patients with migraine has been further explored to evaluate whether alterations in patients with migraine are associated with the migraine cycle [31••]. During painful trigeminal stimulation using ammonia gas, the authors observed a robust activation pattern (in cortical and subcortical areas involved in pain processing) in patients with migraine exclusively within the interictal period and in HC. However, a lower activation in a brainstem area corresponding to the spinal trigeminal nucleus was detected in patients with migraine compared with HC. Interestingly, the BOLD response increased during the pain-free migraine cycle toward the migraine attack, and it was down-regulated just before or immediately at the beginning of a migraine attack. In our opinion, beyond the putative role of spinal trigeminal nucleus as “migraine modulator”, this event-related BOLD-fMRI study highlights two important concepts. The first is a phenomenological concept, which is necessary to better understand the neurobiological significance of periodic functional changes of migraineous brain. Migraine cycle spans over several days during different phases (prodromic, aura, headache, resolution, and recovery), and trigeminal activity in patients with migraine is not constant but strongly variable. The second is a methodological concept, which underlines the importance of taking the time to the next attack into account when investigating patients with migraine.
The correlation between intensity ratings of two different sensory modalities (smell and pain) and their neural correlates has been explored by administration of a chemical substance conveyed through a thin tube placed in the nostril of patients with migraine (in the interictal period) and HC [31••, 32]. By means of a whole-brain analysis, the authors observed that BOLD response increased in patients with migraine, but decreased in HC in bilateral anterior insula, in middle cingulate cortex, and in thalamus [33••]. This functional response was associated with an increased pain rating of the trigeminal painful stimulation in patients with migraine, which was not observed in HC. However, the perception of olfactory stimulus intensity (rose odor) gradually decreased, with no differences between patients with migraine and HC. These clinical and neuroimaging findings were considered related to different neuronal pathways involved in different sensorial systems. Habituation to specific stimuli, such as trigemino-nociceptive inputs, may depend on modulating effects by a specific brain network. Indeed, unlike the trigemino-nociception, the olfactory stimulus habituation may not occur because olfactory inputs are not processed through the thalamus. Interestingly, in contrast to previous studies aimed at detecting a single structure responsible for complex migraine mechanisms, this study suggests that there is no a single neuronal modulator involved in pain generation and processing, but rather a dysfunctional thalamo-cortical network, including several pain transmitting cortical and subcortical areas. It is noteworthy that the same research group, in a longitudinal voxel-based morphometry study, has shown that the repetitive application of painful stimuli may change gray matter density in pain-processing brain regions in HC characterized by “lack of habituation” [34]. Based on previous studies demonstrating similar decreases in gray matter density in patients experiencing chronic pain, it may be interesting to employ the same experimental paradigm in patients with migraine, in which the “lack of habituation phenomenon” is well established.
Conclusions
By using trigeminal painful stimulation in patients with migraine, researchers have developed an interesting imaging approach for a deeper knowledge of migraine pathophysiology. The fast-growing technical developments will increase the capacity to better image the migraineous brain and provide a more detailed picture of migraine neurobiology. Taken together, the results of the reviewed fMRI studies have consistently shown a functional reorganization in several pain processing-related cerebral areas in patients with migraine. These functional changes have been demonstrated during different phases of migraine cycle (i.e., interictal period, headache attack, or immediately before a headache attack). However, even using a specific model of trigeminal system stimulation, fMRI findings are not currently able to fully disentangle the complex scenario of migraine pathophysiology. Indeed, the “brain areas” puzzle, identified in different fMRI studies, is not oriented to a consistent pathophysiological model of the disease, and the conflicting data may reflect the clinical heterogeneity of patients involved in the reviewed studies (i.e., inclusion of patients suffering from migraine with aura and MwoA or other primary headaches; different frequency or intensity of attacks; different current or previous pharmacological treatments) [4]. We believe that, in order to better understand migraine pathophysiology, the choice of tasks, such as trigeminal painful stimulation, must be guided by specific neurobiological questions with a strong a priori hypothesis and with a methodological approach to image the whole-brain response without predefined regions of interest. Additionally, neuroimaging studies, including neuropsychological evaluations, are needed to examine whether personality traits or cognitive profiles may contribute to the different and divergent findings of brain functional changes reported in patients with migraine and HC. Finally, future detection of phenotypical markers and genetic/epigenetic variations will allow the identification of different patient subgroups in order to explore migraine-related brain functional mechanisms in strictly homogeneous groups of patients [35].
References
Papers of particular interest, published recently, have been highlighted as: •Of importance •• Of major importance
Pietrobon D. Moskowitz MA Pathophysiology of migraine. Annu Rev Physiol. 2013;75:365–91.
Launer LJ, Terwindt GM, Ferrari MD. The prevalence and characteristics of migraine in a population-based cohort: the GEM study. Neurology. 1999;53:537–42.
Goadsby PJ, Charbit AR, Andreou AP, Akerman S, Holland PR. Neurobiology of migraine. Neuroscience. 2009;161:327–41.
Tedeschi G, Russo A, Tessitore A. Relevance of functional neuroimaging studies for understanding migraine mechanisms. Expert Rev Neurother. 2013;13:275–85.
Cohen AS, Goadsby PJ. Functional neuroimaging of primary headache disorders. Expert Rev Neurother. 2006;6:1159–71.
Ogawa S, Lee TM, Kay AR, Tank DW. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci U S A. 1990;87:9868–72.
Lakhan SE, Avramut M, Tepper SJ. Structural and functional neuroimaging in migraine: insights from 3 decades of research. Headache. 2013;53:46–66.
Clark VP. A history of randomized task designs in fMRI. Neuroimage. 2012;62:1190–4.
Tedeschi G, Russo A, Tessitore A. Functional neuroimaging in migraine: usefulness for the clinical neurologist. Neurol Sci. 2012;33 Suppl 1:S91–4.
Duerden EG, Albanese MC. Localization of pain-related brain activation: a meta-analysis of neuroimaging data. Hum Brain Mapp. 2013;34:109–49.
•• Maizels M, Aurora S, Heinricher M. Beyond neurovascular: migraine as a dysfunctional neurolimbic pain network. Headache. 2012, Jul 3 [Epub ahead of print]. This work improved our knowledge of migraine underlying mechanisms. The authors propose a model of migraine as a dysfunction of a “neurolimbic” pain network, characterized by a bidirectional influence between brainstem and cortical areas, reflecting the bidirectional interaction of pain and mood in patients with migraine.
Afridi SK, Matharu MS, Lee L, et al. A PET study exploring the laterality of brainstem activation in migraine using glyceryl trinitrate. Brain. 2005;128:932–9.
May A, Kaube H, Büchel C, et al. Experimental cranial pain elicited by capsaicin: a PET study. Pain. 1998;74:61–6.
Ferraro S, Grazzi L, Mandelli ML, et al. Pain processing in medication overuse headache: a functional magnetic resonance imaging (fMRI) study. Pain Med. 2012;13:255–62.
Gierse-Plogmeier B, Colak-Ekici R, Wolowski, et al. Differences in trigeminal and peripheral electrical pain perception in women with and without migraine. J Headache Pain. 2009;10:249–54.
Roberts K, Papadaki A, Goncalves C, et al. Contact heat evoked potentials using simultaneous EEG and fMRI and their correlation with evoked pain. BMC Anesthesiol. 2008;8:8.
Akerman S, Holland PR, Hoffmann J. Pearls and pitfalls in experimental in vivo models of migraine: dural trigeminovascular nociception. Cephalalgia. 2013;33:577–92.
DaSilva AF, Becerra L, Makris N, Strassman AM, Gonzalez RG, Geatrakis N, et al. Somatotopic activation in the human trigeminal pain pathway. J Neurosci. 2002;22:8183–92.
•• Borsook D, DaSilva AF, Ploghaus A, Becerra L. Specific and somatotopic functional magnetic resonance imaging activation in the trigeminal ganglion by brush and noxious heat. J Neurosci. 2003;23:7897–903. Excellent fMRI study showing a divergent response of trigeminal system to different experimental paradigms.
Russo A, Tessitore A, Giordano A, Salemi F, Tedeschi G. The pain in migraine beyond the pain of migraine. Neurol Sci. 2012;33:S103–6.
Quintela E, Castillo J, Munoz P, et al. Premonitory and resolution symptoms in migraine: a prospective study in 100 unselected patients. Cephalalgia. 2006;26:1051–60.
• Becker WJ. The premonitory phase of migraine and migraine management. Cephalalgia 2012, Feb 15 [Epub ahead of print]. The article highlights the key role of premonitory symptoms to better understand migraine attack pathophysiology. Furthermore, premonitory symptoms may be useful in migraine management strategy.
Cortelli P, Montagna P. Migraine as a visceral pain. Neurol Sci. 2009;30 Suppl 1:S19–22.
Moulton EA, Burstein R, Tully S, et al. Interictal dysfunction of a brainstem descending modulatory center in migraine patients. PLoS ONE. 2008;3:e3799.
Moulton EA, Becerra L, Maleki N, et al. Painful heat reveals hyperexcitability of the temporal pole in interictal and ictal migraine States. Cereb Cortex. 2011;21:435–48.
Russo A, Tessitore A, Esposito F, et al. Pain processing in patients with migraine: an event-related fMRI study during trigeminal nociceptive stimulation. J Neurol. 2012;259:1903–12.
Stankewitz A, Voit HL, Bingel U, Peschke C, May A. A new trigemino-nociceptive stimulation model for event-related fMRI. Cephalalgia. 2010;30:475–85.
Magis D, Vigano A, Sava S, et al. Pearls and pitfalls: electrophysiology for primary headaches. Cephalalgia. 2013;33:526–39.
Ambrosini A, de Noordhout AM, Sándor PS, Schoenen J. Electrophysiological studies in migraine: a comprehensive review of their interest and limitations. Cephalalgia. 2003;23 Suppl 1:13–31.
Aderjan D, Stankewitz A, May A. Neuronal mechanisms during repetitive trigemino-nociceptive stimulation in migraine patients. Pain. 2010;151:97–103.
•• Stankewitz A, Aderjan D, Eippert F, May A. Trigeminal nociceptive transmission in migraineurs predicts migraine attacks. J Neurosci. 2011;31:1937–43. This fMRI-study during trigeminal nociceptive stimulation showed periodic functional changes of migraineous brain in different phases of migraine. These findings are necessary to understand the complex neurobiology of migraine phenomenon.
Albrecht J, Kopietz R, Linn J, et al. Activation of olfactory and trigeminal cortical areas following stimulation of the nasal mucosa with low concentrations of S(-)-nicotine vapour - an fMRI study on chemosensory perception. Hum Brain Mapp. 2009;30:699–710.
•• Stankewitz A, Schulz E, May A. Neuronal correlates of impaired habituation in response to repeated trigemino-nociceptive but not to olfactory input in migraineurs: an fMRI study. Cephalalgia. 2013;33:256–65. This work is the first BOLD-fMRI study demonstrating a correlation between habituation to specific stimuli and modulating effects by a specific brain network, such as dysfunctional thalamo-cortical network other than several pain transmitting cortical and subcortical areas.
Stankewitz A, Valet M, Schulz E, et al. Pain sensitisers exhibit grey matter changes after repetitive pain exposure: a longitudinal voxel-based morphometry study. Pain. 2013.
Cutrer FM, Smith JH. Human studies in the pathophysiology of migraine: genetics and functional neuroimaging. Headache. 2013;53:401–12.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. Antonio Russo, Dr. Alessandro Tessitore, and Dr. Gioacchino Tedeschi reported no potential conflicts of interest relevant to this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Russo, A., Tessitore, A. & Tedeschi, G. Migraine and Trigeminal System—I can Feel it Coming…. Curr Pain Headache Rep 17, 367 (2013). https://doi.org/10.1007/s11916-013-0367-2
Published:
DOI: https://doi.org/10.1007/s11916-013-0367-2