Abstract
This review critically evaluates the literature on complementary and alternative medicine (CAM) as treatment options for rheumatoid arthritis and osteoarthritis. Design: Electronic databases were searched to identify all relevant systematic reviews of the effectiveness of CAM in rheumatoid arthritis and osteoarthritis published between January 2010 and January 2011. Reviews were defined as systematic if they included explicit and repeatable inclusion and exclusion criteria for studies. Their methodological quality was assessed using the Oxman criteria for systematic reviews. Results: Five systematic reviews met our inclusion criteria. They all arrived at cautious conclusions. Four reviews were of high quality and one was burdened with high risk of bias. The evidence to support the effectiveness of CAM as a treatment option for rheumatoid arthritis and osteoarthritis is ambiguous.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) and rheumatoid arthritis (RA) are common rheumatic diseases that are associated with morbidity, chronic disability, and poor quality of life [1, 2]. These diseases also have a significant impact on health care budgets, accounting for up to 1% to 2.5% of the gross national product of Western nations [2]. The costs related to the treatment of NSAID-induced adverse events are a significant component of the total costs of arthritis [3]. Additionally, small changes in systolic blood pressure associated with use of common arthritis medications can increase cardiovascular risk [4] and morbidity [5]. On this background, many patients seem to look for alternatives.
Complementary and alternative medicine (CAM) has become popular in patients with rheumatic diseases worldwide. The prevalence of CAM usage by RA patients in the United States was estimated to be anywhere from 28% to 90% [6••]. According to our own data, the lifetime prevalence of CAM use in patients with arthritis is 38% [7]. Whatever the reasons are for the popularity of CAM, it is important to know which form of CAM is a safe and effective option for patients with OA or RA.
This article provides an overview and critically evaluates the data from systematic reviews (SRs) of CAM as a treatment of OA and RA published within the past year.
Methods
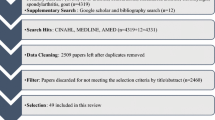
Electronic literature searches were conducted to identify systematic reviews of CAM for RA and OA published between January 2010 and January 2011. Searches were conducted in the following electronic databases: MEDLINE, Embase, AMED, and Cochrane database. The search terms were constructed over three concepts: “OA,” “RA," and “CAM.” Our own extensive department files were hand-searched.
No language barriers were imposed. Abstracts of reviews thus located were inspected, and those appearing to meet the inclusion criteria were retrieved for further evaluation by both authors. Systematic reviews were defined as articles that included an explicit and repeatable literature search method and that had explicit and repeatable inclusion and exclusion criteria for studies. To be included, SRs had to pertain to the effectiveness of one or multiple CAM modalities; to focus specifically on RA and/or OA; and to include evidence from at least two controlled clinical trials. SRs of nonrandomised clinical trials were excluded.
For the purpose of this review, CAM was defined as “diagnosis, treatment and/or prevention which complements mainstream medicine by contributing to a common whole, satisfying a demand not met by orthodoxy, or diversifying the conceptual framework of medicine” [8]. The following CAM modalities were considered eligible: acupuncture/acupressure, Alexander Technique, aromatherapy, (Bach) flower remedies, chiropractic, herbal medicine, homeopathy, hypnosis, massage of any form, naturopathy, osteopathy, spiritual healing, Tai Chi, traditional Chinese medicine, and yoga. Dietary supplements and vitamins or physical exercises were not considered as a part of CAM and therefore were excluded.
Two authors independently extracted the data from the identified articles according to predefined criteria (Table 1). The methodological quality of each SR was evaluated according to Oxman criteria (Table 2) [9]. This validated instrument consists of nine main criteria for assessing the scientific quality of review articles such as reporting of search methods and comprehensiveness of such search; repeatable inclusion and exclusion criteria; avoidance of selection bias; validity assessment; statistical or narrative data analysis; and supportiveness of conclusions. Disagreements were resolved through discussions between the authors.
Results
After removal of duplicates, the searches generated 616 articles, of which 611 were excluded. The reasons for exclusion were that the articles were CAM related or not reports of SRs. Five SRs met our eligibility criteria [10–14]. The included reviews fall into the following categories: acupuncture, mind–body medicine, and herbal medicine (Table 1).
Methodological Aspects of the Included Reviews
One SR was of low methodological quality as assessed by the Oxman criteria [9]. It lacked a validity assessment and a method for combining the included trials. The other SRs were of high methodological quality (ie, used extensive and explicit literature searches, repeatable eligibility criteria, validity assessment, and quantitative analysis). The conclusions of these SRs were supported by the primary data.
Acupuncture
Manheimer et al. [13] aimed to assess the effects of acupuncture for treating peripheral joint OA. The total number of patients with OA of the hip or knee joints (or both) included in their review was 3498. Although the authors concluded that “acupuncture may lead to small improvements in pain and physical function after 8 and 26 weeks post-intervention,” these improvements were not deemed to be clinically relevant.
Zhang et al. [10] aimed at updating the evidence for all available therapies in the treatment of hip and knee OA. This review considered acupuncture as one of two CAM modalities. Although acupuncture was superior to control treatment for pain relief and improved function, this effect was less pronounced in blinded trials with sham acupuncture controls. Further decreases were noted also with time (ie, 6 months after treatment).
Biofeedback, Relaxation, and Meditation
Dissanayake and Bertouch [11] aimed to identify the psychological interventions for which there is consistent, high-quality evidence of efficacy in the treatment of patients with RA. They reported that there was some evidence for improvement with biofeedback-based interventions. However, this statement was based on only two primary studies. Of those, one demonstrated no significant changes in pain, affective response to pain, improved communication, and range of motion at 18-months follow-up. The second study showed significant reductions in patients' pain behavior, disease activity, and trait anxiety at post-treatment and 6-month follow-up. In case of the latter study, the authors failed to mention the length of therapeutic intervention.
Regarding mindfulness and meditation, theses authors found conflicting evidence from the only two randomized controlled trials (RCTs) available. In these studies, mindfulness and meditation was combined with other modalities such as cognitive-behavioral therapy (CBP), yoga, or coping skills; therefore, the specific effects of this therapy alone are not clear.
The authors also reported that there was limited evidence regarding the effectiveness of relaxation therapy [11]. These findings are based on evidence from just two RCTs. One of these studies showed marked improvements in mobility, coordination, and self-care after intervention and at 6 months. The second RCT reported an increased ankle plantar flexion and lower extremity flexion, as well as increased enjoyment of exercise and rest.
Herbal Medicine
Rosenbaum et al. [14] aimed to review efficacy studies of antioxidant and anti-inflammatory dietary supplements used to manage OA and RA. They recommended the use of cat’s claw (Uncaria tomentosa and Uncaria guianen) for the treatment of OA. However, their conclusions are not supported by evidence from the primary studies. For instance, one of the placebo-controlled RCTs was too small to allow generalization and showed no significant effects on pain; two studies tested combinations of cat’s claw and glucosamine sulfate and Sierrasil (SierraSil Health, Inc., Beaverton, OR), a natural product containing several minerals from the Sierra Mountains; and the fourth trial showed no significant differences between cat’s claw and placebo on overall pain, swelling, and stiffness at 24 and 52 weeks.
De Silva et al. [12] aimed to critically evaluate the evidence regarding CAM taken orally or applied topically in the treatment of OA. They found evidence from four placebo-controlled trials that capsaicin gel was effective. One equivalence trial comparing the effectiveness of capsaicin gel and glyceryl trinitrate gel showed similar results in pain related to OA. De Silva et al. [12] also concluded that Indian frankincense may be effective for OA. However, one of the primary studies was underpowered, the second trial tested Indian frankincense enriched with 3-O-acetyl-11-keto-beta-boswellic acid, and the third study showed no differences between Indian frankincense and valdecoxib. De Silva et al. [12] and Zhang et al. [10] mentioned that rose hip may be effective for OA. Two of three relatively high-quality RCTs showed significant improvements in comparison to placebo, and one trial showed no differences in pain.
Conclusions
Our overview was aimed at summarizing and critically evaluating the evidence from SRs of CAM for OA and RA published in the past year. Five SRs were included [10–14]. They investigated the following CAM modalities: acupuncture, biofeedback, relaxation and meditation, and herbal medicine. There was some evidence to support acupuncture, capsaicin gel and cat’s claw, Indian Frankincense, and rose hip. There was not consistent evidence to support mind–body therapies.
We used Oxman criteria [9] for evaluating the methodological quality of the five SRs; four were of high quality [10–13] and one was of low quality [14]. This low-quality SR recommended the use of cat’s claw for OA. Therefore, in our view, this recommendation is of debatable value.
Four SRs mentioned adverse effects (AEs) [10, 12–14] and one failed to do so [11]. In most SRs that mentioned AEs, the incidence rates were low. However, this does not necessarily mean that all forms of CAM are risk-free. For instance, mild AEs from acupuncture occur in about 7% of patients and treatment of these effects can be expensive [15]. In addition, numerous serious complications of acupuncture, including numerous fatalities, are on record [16•, 17•].
Research into CAM faces a number of obstacles, including the use of placebo controls or double-blinding, which is not feasible in many CAM therapies such as healing or yoga [18, 19]. Often, poor quality of the primary studies such as small inadequate sample size, lack of power calculations, allocation concealment, intention to treat data analysis, and use of validated outcome measures increases the risk of bias in CAM research. These methodological problems make their interpretations difficult. Logistical problems include lack of research funds, expertise, and infrastructure.
The potential mechanisms of action of the treatments that show promise may involve the endogenous opioid system in regard to acupuncture [6••]; inhibition of tumor necrosis factor–α, nuclear factor kappa-Β, inducible nitric oxide synthase, or interleukin 1β–induced nitric oxide production in regard to cat’s claw, respectively [6••]. The mechanisms of action of rose hip remain not fully understood [20].
The present analysis has several limitations that should be kept in mind when interpreting its conclusions. Even though thorough search strategy was employed, there is no guarantee that all relevant articles published were located. The validity of any overview of SRs has its limitations. In particular, all SRs are prone to publication bias within the primary research data that they include, and therefore, any such bias may have been inherited in our study. The timeframe we were given for this overview was tight. Thus, it is possible that SRs published before 2010 significantly contribute to the evidence. In fact, our own team has published several SRs that fall outside this timeframe but are nevertheless relevant (Table 3).
In conclusion, recently published SRs generated limited evidence for the effectiveness of CAM in patients with OA or RA.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pirotta M. Arthritis disease the use of complementary therapies. Aust Fam Physician. 2010;39:638–40.
Reginster JY. The prevalence and burden of arthritis. Rheumatology. 2002;41:3–6.
Hunsche E, Chancellor JVM, Bruce N. The burden of arthritis and nonsteroidal anti-inflammatory treatment - A European literature review. PharmacoEconomics. 2001;19:1–15.
Singh G, Miller JD, Huse DM, Pettitt D, D'Agostino RB, Russell MW. Consequences of increased systolic blood pressure in patients with osteoarthritis and rheumatoid arthritis. J Rheumatol. 2003;30:714–9.
Wolfe F, Freundlich B, Straus WL. Increase in cardiovascular and cerebrovascular disease prevalence in rheumatoid arthritis. J Rheumatol. 2003;30:36–40.
•• Efthimiou P, Kukar M. Complementary and alternative medicine use in rheumatoid arthritis: proposed mechanism of action and efficacy of commonly used modalities. Rheumatol Int Berlin. 2010;30:571–86. This article is a good review of mechanisms of action of various CAM modalities.
Hunt K, Ernst E. Patients' use of CAM: results from the Health Survey for England 2005. Focus Altern Complement Ther. 2010;15:101–3.
Ernst E, Pittler MH, Wider B, Boddy K. The Desktop Guide to Complementary and Alternative Medicine. 2nd ed. Edinburgh: Elsevier Mosby; 2006.
Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44:1271–8.
Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis Part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr Cartil. 2010;18:476–99.
Dissanayake RK, Bertouch JV. Psychosocial interventions as adjunct therapy for patients with rheumatoid arthritis: a systematic review. Int J Rheum Dis. 2010;13:324–34.
De Silva V, El-Metwally A, Ernst E, Lewith G, Macfarlane G. Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: a systematic review. Rheumatology (Oxford) 2010; Dec.
Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev. 2010;1:CD001977.
Rosenbaum CC, O'Mathuna DP, Chavez M, Shields K. Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis. Alternative Ther Health Med. 2010;16:32–40.
Witt C, Pach D, Reinhold T, et al. Treatment of the adverse effects from acupuncture and their economic impact: a prospective study in 73,406 patients with low back or neck pain. Eur J Pain. 2011;15:193–7.
• Ernst E. Deaths after acupuncture: a systematic review. Int J Risk Saf Med. 2010;22:131–6. This article emphasizes the potential risks associated with acupuncture.
• Ernst E. Serious adverse effects after acupuncture- a systematic review (2000–2009). Perfusion. 2010;23:214–25. This article reviews risks associated with acupuncture.
Vickers A. Methodological issues in complementary and alternative medicine research: a personal reflection on 10 years of debate in the United Kingdom. J Alter Complement Med. 1996;2:515–24.
Lewith G, Barlow F, Eyles C, et al. The context and meaning of placebos for complementary medicine. Forschende Komplementarmedizin. 2009;16:404–12.
Willich SN, Rossnagel K, Roll S, et al. Patients with rheumatoid arthritis may benefit from a standardised powder of Rosa canina (rose hip). Focus Altern Complement Ther. 2010;15:114–5.
Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American pain Society/American college of physicians clinical practice guideline. Ann Intern Med. 2007;147:492–504.
Harlow T, Greaves C, White A, Brown L, Hart A, Ernst E. Randomised controlled trial of magnetic bracelets for relieving pain in osteoarthritis of the hip and knee. BMJ. 2004;329:1450–4.
Long L, Ernst E. Homeopathic remedies for the treatment of osteoarthritis a systematic review. Br Homeopathic J. 2001;90:37–43.
Ernst E. Avocado-soybean unsaponifiables (ASU) for osteoarthritis - a systematic review. Clin Rheumatol. 2003;22:285–8.
Lee MS, Pittler MH, Ernst E. Tai chi for osteoarthritis: a systematic review. Clin Rheumatol. 2007;27:211–8.
Park J, Ernst E. Ayurvedic medicine for rheumatoid arthritis: a systematic review. Semin Arthritis Rheum. 2005;34:705–13.
Lee MS, Pittler MH, Ernst E. Tai chi for rheumatoid arthritis: systematic review. Rheumatology. 2007;46:1648–51.
Canter PH, Lee HS, Ernst E. A systematic review of randomised clinical trials of Tripterygium wilfordii for rheumatoid arthritis. Phytomedicine. 2006;13:371–7.
Disclosures
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ernst, E., Posadzki, P. Complementary and Alternative Medicine for Rheumatoid Arthritis and Osteoarthritis: an Overview of Systematic Reviews. Curr Pain Headache Rep 15, 431–437 (2011). https://doi.org/10.1007/s11916-011-0227-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-011-0227-x