Abstract
Purpose of Review
3D cone beam imaging (CBCT) has allowed clinicians to better understand the anatomical variations of cranial anatomy. One crucial aspect of this technology plays is the understanding of alveolar bone morphology and remodeling. Variations in cortical bone thickness between individuals have been reported. No published study has analyzed the relationship between cortical bone thickness and rate of tooth movement. The aim of this study is to begin answering the question: is there an association between rate of tooth movement and cortical bone thickness?
Recent Findings
Twenty-three patients underwent extraction of a single premolar in each of the four quadrants prior to orthodontic therapy. Routine clinical records including 3D CBCT images were acquired of all patients prior to first premolar extractions. Rate of tooth movement in each quadrant for each patient was determined via mesiodistal millimetric measurements obtained by a single calibrated operator. With CBCT images, cortical bone thickness was measured at various levels from the alveolar crest along the long axis of the to-be-extracted first premolars. The association between cortical bone thickness and rate of tooth movement was analyzed. Statistically significant associations were found between rate of tooth movement and cortical bone thickness at levels 2 mm, 5 mm, and 8 mm, apical to the alveolar crest in both the right and left maxillary quadrants (p < 0.05). Statistically significant associations were found between rate of tooth movement and cortical bone thickness at levels 5 mm and 8 mm apical to the alveolar crest in both mandibular quadrants (p < 0.05). Increased cortical bone thickness was associated with decreased rate of tooth movement. There was no statistically significant association between rate of tooth movement and cortical bone thickness 2 mm apical to the alveolar crest of the to-be-extracted first premolars in the mandibular left nor right quadrants (p > 0.05).
Summary
Results suggest an inverse relationship may exist between cortical bone thickness and rate of tooth movement in both the maxilla and mandible. Cortical bone thickness may have the potential to serve as a predictive tool for rate of orthodontic tooth movement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Traditional orthodontic records for patients include clinical photographs, study models, and radiographs. In the past, lateral cephalograms and panorex radiographs provided the mainstay of understanding orthodontic diagnosis, treatment planning, treatment progress, and clinical success. Routine clinical records are now replaced by 3D surface imaging [1,2,3] and study models [4, 5•,6]. In the modern age, orthodontic radiographs are replaced by 3D radiographs [7,8,9,10]. One such technology is the advancements in fast acquisition time and low radiation cone beam computed tomography devices. Improvements in CBCT techniques allow dental professionals to more accurately assess anatomical variations between patients, create better diagnosis and treatment outcomes [11,12••]. One such area of evaluation is the dental alveolus in which the teeth are housed [13]. Craniometric and 3D imaging studies have proven differences in cortical bone widths exist between individuals [14,15,16,17] and also evaluated treatment effects of structures surrounding the teeth [18,19•].
Much research has focused on the metabolic coordination of the alveolar bone as the teeth move in the arch. Yet, no studies have attempted to link the varying morphology of cortical bone to rate of orthodontic tooth movement. Upon mechanical stimulus, blood flow alterations to the supporting tooth structures initiate electrical and chemical cascades involving pro-inflammatory cytokines such as interleukin-1 (IL-1), IL-6, IL-8, tumor necrosis factor-α (TNF-α), interferon-γ which in turn RANKL and OPG levels to control the bone remodeling process [20]. Previous studies have analyzed the levels of OPG and RANKL in the gingival crevicular fluid in orthodontic patients undergoing canine distalization [4]. Numerous additional studies have analyzed the roles of cytokines, prostaglandins, vitamin D3, PTH, and relaxin during orthodontic tooth movement [21,22]. All these mediators affect the bone density and structures around the teeth.
In the series of patients described in this paper, the same clinician provided each patient with the same orthodontic treatment. Yet, a large variability in rate of extraction site space closure was noted. A literature search was performed to determine if previous studies have analyzed the relationship between thickness of bone and rate of orthodontic tooth movement. After failing to find literature examining this relationship, the null hypothesis that cortical bone thickness plays no role in determining rate of orthodontic tooth movement was made.
The aim of this study was to determine if a relationship between CBCT-measured alveolar cortical bone thickness and rate of orthodontic extraction site space closure exists. Such an understanding may allow more precise treatment plans and durations to be developed for patients and may prove to be especially useful for patients whose treatment necessitates premolar extractions. To date, no study has attempted to quantify this information.
Materials and Methods
This study took place at a dental university and the protocol received approval from the Institutional Review Board (IRB) #WRIB 1142185 at the university prior to study commencement.
All patients provided consent to participate in the study as part of a larger study of orthodontic treatment. Twenty-three patients involved in this study met the following requirements: permanent dentition, initial class I malocclusion with irregularity score of > 2 mm in either arch [23], and CBCT image acquisition was part of the clinical records for diagnosis and treatment planning of the type of orthodontic treatment. In this cohort of patients, all patients that had first premolar extractions to alleviate crowding were included. Exclusion criteria for this study included the following: any medical or dental condition that, in the opinion of the investigator, could negatively affect study results, currently utilizing an investigational drug or device, planning to relocate or move during the trial period, utilizing bisphosphonates, and pregnancy.
Clinical Procedures
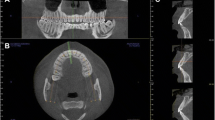
Prior to and within 1 week of first premolar extraction, each patient received a CBCT image utilizing the Kodak 9500 CBCT (Carestream Dental LLC, Atlanta, GA, USA) machine. CBCT scans of each patient were obtained with a voxel resolution of 0.3 mm and a field of view of 18 × 25 cm. Sophisticated algorithms were utilized to reconstruct data from the series of two-dimensional projections into coronal, axial, and sagittal plane x-ray projections. The resulting 599 slices were saved to a Dicom file with “.dcm” file extension.
All twenty-three patients received first premolar extractions to alleviate crowding. Traditional orthodontic wires and brackets were utilized on all patients. Following first premolar extractions, the leveling and aligning stage of treatment culminated with Little’s Index of Irregularity (LII) < 1 mm. Measurements to determine the LII were taken at the five contact points for the mandibular and maxillary anterior teeth between the canines on each half of the arches every 4 weeks. The date of LII < 1 mm was recorded.
The second stage of treatment involved the closure of the first premolar extraction sites. Space closure was done with active “tie-backs” (a rubber elastomeric module attached to a metal ligature) over large extraction spaces. When the space remaining was 1 mm or less, space closure was done with an elastic power chain attached to each tooth. The date of initiation of the extraction site closure phase of treatment was recorded and the mesiodistal distance from the mesial-most contour of the mesial contact of the second premolar and the distal-most contour of the distal contact of the canine was measured and recorded in millimeters as initial extraction site size via use of a digital electronic caliper (Orthopli Corp, Philadelphia, PA) with an accuracy of 0.01 mm. This initiation of the extraction site closure phase of treatment was designated “appointment zero.” Outcome assessments were scheduled on a regular basis every 2 weeks until orthodontic therapy was complete.
At each appointment throughout the extraction site closure phase of treatment, the mesiodistal size of the first premolar extraction site in each of the four quadrants was measured and recorded in millimeters by one designated calibrated operator utilizing the same digital electronic caliper and techniques previously mentioned. The same designated calibrated operator took all clinical measurements for this study. Occlusal-view clinical photographs were obtained during each appointment. Figure 1 portrays maxillary occlusal photographs of a patient at appointment zero (Fig. 1a) and at the end of the premolar extraction site closure phase of treatment (Fig. 1b). Utilizing the time and space measurements recorded at each appointment, the average rate of extraction site closure in each quadrant was determined in millimeters per week.
Image Analysis
The CBCT images were retrospectively analyzed. Images were analyzed by a separate investigator than the investigator making clinical measurements. Upon conclusion of the patient’s treatment, mid-mesiodistal slices of the to-be-extracted teeth were extrapolated as follows. The sagittal slice was utilized to identify the mid-mesiodistal locus of interest on the to-be-extracted first premolar. This slice was oriented in a manner such that the vertical reference line was oriented parallel to the long axis of the to-be-extracted premolar. The transverse slice was utilized to ensure the reference line bisected the to-be-extracted first premolar. The transverse slice was oriented in a manner such that the vertical reference line was oriented parallel to the buccal and lingual cortical plates lying immediately adjacent to the to-be-extracted premolars. Via the coronal slice, final measurements were made. The alveolar crest and levels 2 mm, 5 mm, and 8 mm apical to the alveolar crest were identified and marked (Fig. 2). At each marked level, buccolingual dimensions of the facial and lingual cortical plates were measured perpendicular to the outer cortical surface to the junction of the cortical and cancellous bones [13]. Radiographic measurements were made by the single operator after 3 weeks of training alongside trial measurements on thirty images. Measurements were recorded in an Excel file (Microsoft, Redmond, Wash). Figure 3 portrays a sample measurement of facial and lingual cortical bone at a level 5 mm apical to the alveolar crest of the mandibular to-be-extracted first premolar. The total cortical bone thickness at each level along the long axis of the to-be-extracted premolars was calculated.
Statistical Analysis
Demographics, total cortical bone widths, initial first premolar extraction site sizes, and rates of extraction site closure were summarized using descriptive statistics with mean ± standard deviation (SD) for continuous variables, frequency, and percentage for categorical variables. The normality assumption for the outcome (rate of premolar extraction site closure) was verified by the Shapiro-Wilk test. Linear regression was used to assess associations between total cortical bone at each of the aforementioned levels and rate of premolar extraction site closure with a covariate adjustment in the linear regression analysis for age. Post hoc power analysis was performed to determine the observed power of our results (Fig. 4).
Intra-examiner reliability for the measurement of the palatal cortical bone thickness and facial cortical bone thickness for maxilla and lingual cortical bone thickness and facial cortical bone thickness for the mandible were assessed using an intra-class correlation coefficient (ICC) in a random sample of five sites in six randomly selected patients. A total of thirty measurements in twenty different images were re-measured. The ICC for intra-rater agreement was estimated for the two sets of measurement taken at least 1 week apart. An ICC score of 0.75 or higher was considered as an acceptable reliability for our quality control criterion. The intra-class correlation coefficients were between 0.85 and 0.96 for each of the measured values. To assess intra-examiner reliability of the calibrated examiner, duplicate sets of six pairs of plaster models were randomly selected. Over a period of 6 weeks, the examiner measured the size of the premolar extraction sites in each of the four quadrants on each of the six duplicate casts using the aforementioned digital electronic caliper. Reliability of measurements was assessed via calculation of intra-class correlation. Results yielded a strong reliability of measurements with ICC greater than 0.95. A p value of < 0.05 was considered statistically significant in two-tailed statistical tests. All analyses were conducted using SAS 9.4 software (SAS Institute, Cary, NC).
Results
This study was composed of eighteen females and five males. The ages of our cohort at the initiation of treatment ranged from 12 to 37 years with a mean age of 19.46 years. Of the twenty-three patients, thirteen were between the ages of twelve and seventeen, six were between the ages of eighteen and twenty-seven, and four were between the ages of twenty-eight and thirty-seven. Table 1 highlights the demographic characteristics of our cohort.
Descriptive statistics pertaining to the average rates of premolar extractions site closure (AR), duration of the first premolar extraction site closure phase of treatment (SC), as well as mesiodistal size of the first premolar extraction site (ES) at appointment zero in each of the four quadrants are presented in Table 2.
Descriptive statistics for total cortical bone width (TC) at levels 2 mm, 5 mm, and 8 mm apical to the alveolar crest for each quadrant are reported in Table 3. Statistically significant associations were found between average rate of premolar extraction site closure and total cortical bone width at levels 2 mm, 5 mm, and 8 mm, apical to the alveolar crest in both the right and left maxillary quadrants (p < 0.05). Statistically significant associations were found between average rate of premolar extraction site closure and total cortical bone width at levels 5 mm and 8 mm apical to the alveolar crest in both mandibular quadrants (p < 0.05). At these aforementioned sites, an increase in bone width was associated with a slower rate of tooth movement.
There was no statistically significant association between average rate of premolar extraction site closure and total cortical bone width at a level 2 mm apical to the alveolar crest of the to-be-extracted premolars in neither the mandibular left nor right quadrants (p > 0.05). Post hoc power analysis portrayed the two-tailed t tests were all powered at least 80% to detect the significant slopes of total cortical bone width (TC), based on the type I error α = 0.05 and standard deviations. The effect size and corresponding power are presented in Table 4 alongside linear regression results.
Discussion
Few studies to date have tried to quantify the relationship of bone morphology and rates of the tooth [21,24]. Most studies quantified bone thickness around anterior teeth and the movement of teeth rather than rates of tooth movment [25,26]. Some suggests the importance of the amounts of bone and tooth movement [27]. In this study, we found the average rates of premolar extraction site closure were not statistically significantly different in the right versus left quadrants (p > 0.05) nor were mean total cortical bone widths significantly different in the right versus left quadrants (p > 0.05) for corresponding structures. In comparison, average rates of premolar extraction site closure were greater in the maxillary quadrants versus mandibular quadrants (Table 2). Such results are consistent with the findings of mean cortical bone thickness in the maxilla being less than that of the mandible (Table 3). Previous studies have confirmed this variation in cortical bone width in the mandible versus the maxilla [28].
Statistically significant associations were found between total cortical bone width and rate of extraction site closure at levels 2 mm, 5 mm, and 8 mm apical to the alveolar crest of the to-be-extracted premolars in both the right and left maxillary quadrants as well as levels 5 mm and 8 mm apical to the alveolar crest of the to-be-extracted premolars in both mandibular quadrants (Table 4). Such results, as shown in this study, suggest the potential for an association between a patient’s cortical bone thickness and the rate of bodily tooth movement during orthodontic therapy.
As forces are applied to brackets attached to the crowns of the teeth adjacent to the extraction site, moments are generated as the applied force vector is occlusal and buccal to the center of rotation of the tooth. Such a moment results in alternating tipping and rotation of the tooth being mobilized. The extent of tipping and rotation will depend on the size of the space needing to be closed as well as the ability of the clinician to successfully apply a counteracting moment to the moment generated by the force vector. Previous studies have shown the highest level of resistance to bodily tooth movement during orthodontic alignment occurs near one-third to one-half the distance from the alveolar crest to the apex of the tooth. This region of resistance correlates with the center of resistance of the majority of teeth. Such outcomes correlate with our study’s findings of cortical bone thickness 5 mm and 8 mm apical to the alveolar crest of the tooth correlating with rate of gap closure in all four quadrants.
There were limitations to this study. The sample size did not allow a meaningful statistical analysis of the bone turnover rate versus cortical bone thickness for between the ages. This was attributed the range of ages presented. The study measured only the cortical bone thickness as this was the most accurately reproducible measurement and the study was not able to determine if the extraction sites were damaged. Trabecular bone was less identifiable as it was dark and may include artifacts. Finally, the measurement site was the premolar region which has bone morphology that differs from other parts of the jaw. An example of which is the anterior zone of the alveolar bone.
A future direction for this line of research lies in analyzing the correlation between cortical and trabecular bone density and rate of tooth movement. Modern cone beam computed tomography devices allow the estimation of bone mineral density via the use of Hounsfield units (HU) [29]. In such an analysis, bone mineral density in HUs is represented as the relative density of the specimen in question to a calibrated gray-scale designed from HU values of air (− 1000 HU), water (0 HU) and dense bone (+ 1000 HU) [29]. The most debated topic regarding the use of HUs is the non-uniformity of values amongst different machines [29]. The purpose of this study is to assess the association between cortical bone thickness and rate of gap closure in a reproducible manner such that future studies can further such a correlation. For that reason, Hounsfield units were not utilized to assess bone mineral density. As technology advances and more accurate means of measuring such a parameter become available, the analysis between bone mineral density and rate of tooth movement can begin.
Conclusion
The following conclusions may be inferred from this study;
-
Thicker cortical bone at levels 5 mm and 8 mm apical to the alveolar crest of the mandibular premolar region was associated with a decreased rate of premolar extraction site closure in the right and left mandibular quadrants.
-
Thicker cortical bone at levels 2 mm, 5 mm, and 8 mm apical to the alveolar crest of the maxillary premolar region was associated with a decreased rate of premolar extraction site closure in the right and left maxillary quadrants.
Such results suggest an inverse relationship exists between thickness of cortical bone and the rate of extraction site closure in both the maxilla and the mandible. Cortical bone thickness has the potential to serve as a predictive tool for rate of orthodontic space closure and may be especially useful in orthodontic patients receiving dental extractions.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CBCT:
-
cone-beam computed tomography
- TNF-α:
-
tumor necrosis factor-α
- IL:
-
interleukin
- RANKL:
-
receptor activator of nuclear factor kappa-beta ligand
- OPG:
-
osteoprotegerin
- PTH:
-
parathyroid hormone
- IRB:
-
institutional review board
- LII:
-
Little’s Index of irregularity
- SD:
-
standard deviation
- ICC:
-
intra-class correlation coefficient
- AR:
-
average rates of premolar extractions site closure
- SC:
-
extraction site closure duration
- ES:
-
extraction site mesiodistal dimension
- TC:
-
total cortical bone width
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bo Ic M, Kau CH, Richmond S, Hren NI, Zhurov A, Udovic M, et al. Facial morphology of Slovenian and Welsh white populations using 3-dimensional imaging. Angle Orthod. 2009;79(4):640–5.
Seager DC, Kau CH, English JD, Tawfik W, Bussa HI, Ahmed AY. Facial morphologies of an adult Egyptian population and an adult Houstonian white population compared using 3D imaging. Angle Orthod. 2009;79(5):991–9.
Kesterke MJ, Raffensperger ZD, Heike CL, Cunningham ML, Hecht JT, Kau CH, et al. Using the 3D facial norms database to investigate craniofacial sexual dimorphism in healthy children, adolescents, and adults. Biol Sex Differ. 2016;7:23.
Kau CH, Wang J, Davis M. A cross-sectional study to understand 3D facial differences in a population of African Americans and Caucasians. Eur J Dent. 2019;13(4):485–96.
• Kau CH, Li JL, Li Q, Abou Kheir N. Update on cone beam technology and orthodontic analysis. Dent Clin N Am. 2014;58(3):653–69.
Torassian G, Kau CH, English JD, Powers J, Bussa HI, Marie Salas-Lopez A, et al. Digital models vs plaster models using alginate and alginate substitute materials. Angle Orthod. 2010;80(4):474–81.
Kau C, Richmond S, eds. Three-dimensional imaging for orthodontics and maxillofacial imaging. 1st ed: Blackwell Wiley; 2010.
Kau CH. Creation of the virtual patient for the study of facial morphology. Facial Plast Surg Clin North Am. 2011;19(4):615–22 viii.
Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32(4):282–93.
Lightheart KG, English JD, Kau CH, Akyalcin S, Bussa HI Jr, McGrory KR, et al. Surface analysis of study models generated from OrthoCAD and cone-beam computed tomography imaging. Am J Orthod Dentofac Orthop. 2012;141(6):686–93.
Palomo JM, Kau CH, Palomo LB, Hans MG. Three-dimensional cone beam computerized tomography in dentistry. Dent Today. 2006;25(11):130 132-135.
•• Kau CH, Bozic M, English J, Lee R, Bussa H, Ellis RK. Cone-beam computed tomography of the maxillofacial region--an update. Int J Med Robot. 2009;5(4):366–80.
Pan F, Kau CH, Zhou H, Souccar N. The anatomical evaluation of the dental arches using cone beam computed tomography--an investigation of the availability of bone for placement of mini-screws. Head Face Med. 2013;9:13.
Ozdemir F, Tozlu M, Germec-Cakan D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am J Orthod Dentofac Orthop. 2013;143(2):190–6.
Farahamnd A, Sarlati F, Eslami S, Ghassemian M, Youssefi N, Jafarzadeh EB. Evaluation of impacting factors on facial bone thickness in the anterior maxillary region. J Craniofac Surg. 2017;28(3):700–5.
Cassetta M, Sofan AA, Altieri F, Barbato E. Evaluation of alveolar cortical bone thickness and density for orthodontic mini-implant placement. J Clin Exp Dent. 2013;5(5):e245–52.
Cassetta M, Stefanelli LV, Pacifici A, Pacifici L, Barbato E. How accurate is CBCT in measuring bone density? A comparative CBCT-CT in vitro study. Clin Implant Dent Relat Res. 2014;16(4):471–8.
Kau CH. A radiographic analysis of tooth morphology following the use of a novel cyclical force device in orthodontics. Head Face Med. 2011;7:14.
• Kau CH, English JD, Muller-Delgardo MG, Hamid H, Ellis RK, Winklemann S. Retrospective cone-beam computed tomography evaluation of temporary anchorage devices. Am J Orthod Dentofac Orthop. 2010;137(2):166 e161–5 discussion 166–167.
Arabshahi B, Dewitt EM, Cahill AM, Kaye RD, Baskin KM, Towbin RB, et al. Utility of corticosteroid injection for temporomandibular arthritis in children with juvenile idiopathic arthritis. Arthritis Rheum. 2005;52(11):3563–9.
Nimeri G, Kau CH, Abou-Kheir NS, Corona R. Acceleration of tooth movement during orthodontic treatment--a frontier in orthodontics. Prog Orthod. 2013;14:42.
Kanzaki H, Chiba M, Arai K, Takahashi I, Haruyama N, Nishimura M, et al. Local RANKL gene transfer to the periodontal tissue accelerates orthodontic tooth movement. Gene Ther. 2006;13(8):678–85.
Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008;23(1):27–33.
Sendyk M, Linhares DS, Pannuti CM, Paiva JB, Rino NJ. Effect of orthodontic treatment on alveolar bone thickness in adults: a systematic review. Dental Press J Orthod. 2019;24(4):34–45.
Uribe F, Padala S, Allareddy V, Nanda R. Cone-beam computed tomography evaluation of alveolar ridge width and height changes after orthodontic space opening in patients with congenitally missing maxillary lateral incisors. Am J Orthod Dentofac Orthop. 2013;144(6):848–59.
Ahn HW, Moon SC, Baek SH. Morphometric evaluation of changes in the alveolar bone and roots of the maxillary anterior teeth before and after en masse retraction using cone-beam computed tomography. Angle Orthod. 2013;83(2):212–21.
Enhos S, Uysal T, Yagci A, Veli I, Ucar FI, Ozer T. Dehiscence and fenestration in patients with different vertical growth patterns assessed with cone-beam computed tomography. Angle Orthod. 2012;82(5):868–74.
Khumsarn N, Patanaporn V, Janhom A, Jotikasthira D. Comparison of interradicular distances and cortical bone thickness in Thai patients with class I and class II skeletal patterns using cone-beam computed tomography. Imaging Sci Dent. 2016;46(2):117–25.
Campos MJ, de Souza TS, Mota Junior SL, Fraga MR, Vitral RW. Bone mineral density in cone beam computed tomography: only a few shades of gray. World J Radiol. 2014;6(8):607–12.
Funding
Statistical analysis was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR001417.
Author information
Authors and Affiliations
Contributions
CHK obtained consent from all patients, obtained CBCT images of all patients, treated all patients, obtained all clinical measurements, and provided guidance in writing the manuscript. DCW obtained radiographic measurements and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
All participants consented to publication of de-identified data reported in this study. 1142185 is the reference number for consent to participate documentation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Craniofacial Skeleton
Rights and permissions
About this article
Cite this article
Kau, C.H., Cruz Wilma, D.A. 3D Analysis of Tooth Movement Using 3D Technology. Curr Osteoporos Rep (2020). https://doi.org/10.1007/s11914-020-00625-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s11914-020-00625-z