Abstract
Purpose of Review
The purpose of this review was to summarize the clinical, diagnostic, and therapeutic features of blastic plasmacytoid dendritic cell neoplasm (BPDCN).
Recent Findings
Several case reports and series revealed new clinical, molecular, diagnostic, and therapeutic aspects of the disease. The clinical presentation diversity has been confirmed, with frequent leukemic non-cutaneous or rare atypical manifestations. The clonal evolution in the development of BPDCN has not been sufficiently elucidated. Although certain immunophenotypic markers (CD4, TCL1, CD123, CD56, CD303) are indicative of BPDCN, the diagnosis remains in certain cases challenging. Adult (ALL)-type chemotherapy followed by hematopoietic stem cell transplantation (HSCT) is related to a favorable outcome, while chemotherapy alone seems enough in children. Future studies should continue to investigate whether CD123-directed therapies could be utilized.
Summary
BPDCN is a rare aggressive malignancy that needs an aggressive induction therapy. Although a diagnostic consensus is still lacking, and large retrospective studies are also needed to obtain standardized treatment guidelines, the future perspectives are encouraging, because of novel therapeutic agents that are under investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is recognized in the WHO 2016 classification of hematopoietic neoplasms as a distinct acute leukemia entity [1]. Described for the first time in 1994 as CD4+ cutaneous lymphoma with high expression of CD56, BPDCN has been known previously with various names such as blastic natural killer (NK) leukemia/lymphoma, agranular CD4+/CD56+ hematodermic neoplasm, and agranular CD4+ NK cell leukemia [2]. It is a rare disease presenting across all ages with either skin or both skin and bone marrow involvement often conferring a poor prognosis [3]. BPDCN is often associated with a complex karyotype, frequent deletions of tumor suppressor genes, and mutations affecting either the DNA methylation or chromatin remodeling pathways [4].
Origin of the Neoplastic Cell
The potential of the transformed (leukemic) multipotential hematopoietic cell to differentiate and mature along any myeloid lineage forms the basis for the phenotypic classification of acute and chronic myelogenous leukemia [5]. BPDCN was once believed to be derived from natural killer cells and is now recognized as originating from precursors of plasmacytoid dendritic cells (DCs). DCs comprise two functionally distinct subsets: plasmacytoid DCs (pDCs) and myeloid DCs (mDCs). PDCs have been considered as Th2-type dendritic cell precursors characterized by its capacities to produce large amount of alpha interferon and to differentiate into dendritic cells [6]. PDCs, which are defined as lineage marker (Lin) (−)HLA-DR(+)CD56(−)CD123(+)CD11c(−) cells, are considered to be the normal counterpart of BPDCNs [7]. In BPDCN, which is characterized by a distinctive cutaneous and bone marrow tropism, proliferating cells have been proposed to derive from immediate CD4(+)CD56(+) precursors of pDCs, probably a minor subpopulation of Lin(−)DR(+)CD56(+)CD123(+)CD11c(−) cells, which express BDCA2, BDCA4, and myeloid antigens, which are frequently expressed by BPDCN [7]. Thus, BPDCN has been proposed to originate from the myeloid lineage and, in particular, from resting pDCs [8]. However, it seems to be more complicated, if we take into account another report, which characterized a CD56(+) DC population that express typical pDC markers including CD123 and BDCA2, but produce much less IFN-I comparing with pDCs [9•]. According to this report, BPDCN is closer to CD56(+) DCs, a novel mDC subset mixed with some pDC features, and not to pDCs, by global gene expression profiling [9•]. Thus, it was proposed that the CD4(+)CD56(+) neoplasm may be a tumor counterpart of CD56(+) mDCs but not pDCs [9•]. Additionally, it should be noted that the majority of published cases are de novo, although a rare case of BPDCN with deletion 7q.31, in the setting of heavy pre-treatment with alkylating chemotherapy, has been reported [10].
Clinical Presentation
BPDCN usually presents with cutaneous involvement as the first manifestation, with subsequent or simultaneous spread to bone marrow and peripheral blood. Patients with BPDCN usually present with solitary or multiple skin lesions. Cutaneous lesions can present as isolated nodules, macules, and disseminated macules and nodules [11]. A nodular pattern is a more common feature than the originally reported “bruise-like” pattern [12]. Localized or disseminated lymphadenopathy at presentation is common. Leukemia as the first presenting symptom without any cutaneous involvement is a rare finding and can masquerade as acute undifferentiated leukemia. The neoplasm presents with an aggressive behavior, and the clinical findings include cytopenia, particularly thrombocytopenia [13]. BPDCN with “leukemic” presentation otherwise presents no major distinguishing features and is at least as aggressive as its cutaneous-involved BPDCN counterpart [14].
The clinical presentation diversity of BPDCN has been highlighted through several case reports. Thus, BPDCN has previously appeared as a renal mass [15] and as complete monocular vision loss due to optic nerve involvement [16], while it has been identified in the nasal cavity [17], on the trunk, or even on the scalp [18]. Lung involvement at initial presentation lacking cutaneous lesion [19], colon involvement [20], leukemic presentation with massive splenomegaly [21], and atraumatic splenic ruptures that triggered both remission and death in a single case [22], have been previously reported.
Epidemiology
The precise incidence of BPDCN is difficult to estimate due to constantly changing nomenclature and lack of precise defining criteria prior to the 2008 WHO classification system [23]. A male predominance (male/female ratio = 3.3/1) and an incidence 0.000045% have been reported [24•] . In any case, the dismal course and prognosis of BPDCN have been underlined through the publication of a patient with BPDCN, who did not accept further therapy, and survived 3 months only [13]. Clinical characteristics at diagnosis that have been associated with poorer outcomes include age > 60 years, abnormal karyotype, and terminal deoxynucleotidyl transferase (TdT) negativity in the BPDCN cells [25••]. In the absence of reliable parameters for predicting prognosis in BPDCN other than age, tumor stage, and/or clinical presentation, simple methods, such as FISH for CDKN2A/CDKN2B, could help to identify the most aggressive cases (with biallelic loss of locus 9p21.3) [26].
Morphology
Common morphological features of BPDCN include a monotonous appearance of medium-sized tumor cells or large atypical monocytoid cells, resembling lymphoblasts or myeloblasts. BPDCN with immunoblastoid morphology and MYC rearrangement and overexpression has also been reported [27]. In BPDCN, the nuclei have a slightly irregular contour, finely dispersed chromatin, and a conspicuous nucleolus [28]. The nuclei can be irregular, folded, or flowerlike, and the cytoplasmic membrane might appear with dendritic-like protrusions and pseudopodia. Some tumor cells have intracytoplasmic microvacuoles [29], while necklace-like microvacuoles of tumor cells have also been described [30]. In the lymph nodes, hypercellularity with a monotonous population of intermediate-sized cells, dispersed singly or arranged in loose aggregates, can be observed. The cells have round to oval nuclei, with fine chromatin and prominent nucleoli; the cytoplasm is generally scant, without visible granules [31]. Histopathological examination of skin lesions reveals tumor infiltration, extended from the dermis to the cutaneous adipose tissue, but with no invasion of the epidermis [32]. The tumor cells may be plasmacytoid, ranging in size from small to intermediate, with a high nuclear-cytoplasmic ratio, probably without nucleoli [32]. In bone marrow smears, dysplastic changes can be observed [33], especially in megakaryocytes, [24•] while immunohistochemistry (IHC) might be the only method to detect minimal bone marrow infiltration [24•, 34, 35].
Immunophenotype
Diagnosis of BPDCN is mainly based on immunophenotypical characterization of leukemic cells in skin lesions, blood, or bone marrow samples. Neoplastic cells express CD4, CD43 (also termed SPN), CD45RA, and CD56 (also termed NCAM1), as well as the plasmacytoid dendritic cell-associated antigens CD123 (also termed IL3RA), BDCA-2 (also termed CD303, CLEC4E), proto-oncogene T cell leukemia 1 (TCL1), and CTLA1 (also termed GZMB) [36]. On a series of 91 well-documented cases collected by the French Study Group on Cutaneous Lymphomas, the five most characteristic markers of this entity (CD4, CD56, CD123, CD303, and TCL1) were expressed simultaneously in only 46% of patients [37]. However, when 4 markers were expressed, the diagnosis could still be reliably made without resorting to any additional stains [37]. In a cohort of patients with bone marrow involvement, cells were positive for CD4, CD123, TCL1, and HLA-DR and negative for CD3, CD8, CD13, CD19, CD34, and myeloperoxidase (MPO) [33]. Other antigens expressed by subsets of BPDCN cases included the following: CD56 (81%), CD33 (70%), CD7 (69%), TdT (33%), CD2 (31%), CD117 (22%), and CD5 (15%) [33]. In our cohort of patients published 9 years ago, CD4, CD56, HLA-DR, and CD123 (bright) expression, in the absence of major B-, T- and myeloid-associated markers, represented the core of the immunophenotypic profile of our BPDCN cases. However, it should be noted that TCL1 expression had not been thoroughly investigated [28].
Intracellular expression of TCL1 is highly expressed in all pDCL samples, while at a statistically lower level in all B-ALL and 34% of AML [38]. The high intracellular intensity of TCL1 expression has been considered the best marker for pDC lineage assignment by flow cytometry (FC), being particularly useful to distinguish pDCL from CD4+/CD56 ± undifferentiated or monoblastic acute leukemia [38]. In a comparison of myeloid sarcoma (MS) cases with BPDCN cases, BPDCN was associated with positive staining for CD56, TdT or TCL1, or negative staining for lysozyme, while neither CD162 nor CD303 had good predictive value in distinguishing MS from BPDCN [39].
Special consideration should be given to the expression of CD56, CD13 and transcription factor 4 (TCF4). Myeloid antigen expression involving CD13 may not exclude a diagnosis of BPDCN [40]. Also, the absence of CD56 should not exclude BPDCN diagnosis, while loss of CD56 expression can also occur as a secondary event after chemotherapy and bone marrow transplantation (BMT), probably through the contribution of chemotherapy-induced mutations [41]. It is worth noting that a CD56 negative BPDCN case in young age has been published and presented as acute leukemia without skin lesion, with involvement of the central nervous system (CNS) [42]. Regarding TCF4, it is a highly sensitive marker for BPDCN and augments diagnostic specificity alongside CD4, CD56, CD123, and TCL1 [43].
Immunohistochemical analyses are highly recommended for CD123, CD56, and CD4 in BPDCN patients, particularly in cases where the initial BM study indicates normal morphology [34]. In a comparative study of biopsies between AML and BPDCN cases, all BPDCN cases lacked myeloid cell nuclear differentiation antigen (MNDA) expression, supporting the inclusion of MNDA IHC in the diagnostic evaluation of blastic hematopoietic infiltrates, particularly when the differential diagnosis is between myeloid leukemia and BPDCN [44]. Distinct findings of potential usefulness can also be met in the literature, such as the expression of thymic stromal lymphopoietin (TSLP) and its receptor in BPDCN cells [35], the immunohistochemical expression of CD31/PECAM-1 (platelet endothelial cell adhesion molecule 1) by BPDCN cells [45], and the presence of CXCL12-positive cells in the skin, which may be associated with leukemic change and a poor prognosis [46].
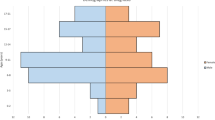
Taken into account all the above, but also the proposal of Garnache-Ottou et al. [47], our team recommends a three-stage immunophenotypical panel for BPDCN diagnosis, consisted of a panel of “indispensable criteria,” a panel of “major criteria,” and a panel of “minor criteria” (Fig. 1). The indispensable criteria panel includes a low CD45/side scatter (SS) blast pattern (homogeneous), MPO−, CD3−, cCD3dim/−, cCD79−, CD19−, CD20−, CD10−, CD11c−, CD14−, CD64−, lysozyme−, and HLA-DR+, which should all apply. The major criteria panel includes CD4+, CD56+, CD123++, TCL1+, CD43+, CD34−, and CD36+, where at least 6 out of 7 should apply, while the minor criteria panel includes BDCA-2+, BDCA-4+, NG2+, ILT3+, CD117−, CD13−, CD15−, and CD5−, where at least 5 out of 8 should apply (Fig. 1). Moreover, FC analysis permits the identification of cases with composite immunophenotype that could be considered as BPDCN. The ability of discrimination of coexistent or overlapping, normal, or abnormal cell populations confirms the determinant role of FC in the identification of “mixed-type” leukemias. The combined assessment of morphology and FC analysis can identify cases of leukemias of ambiguous lineage (LAL), always implicating a significant CD56- pDC population and a distinct leukemia component of different immunophenotype (myeloid, monocytic, myelomonocytic, even lymphoid). The qualitative assessment of blasts supports the existence of > 1 blast population, and the same is true in the FC assessment (Fig. 2). Also, the morphological blast count and the cytogenetic quantitative evaluation (in cases with abnormal findings) correspond to the quantitative sum of the two populations, as estimated with FC analysis, further supporting a clonal origin (data not shown). Similar clonal relations of DCs with myeloid malignancies have been previously described in AML and myelodysplastic syndromes [47,48,49].
Molecular and Cytogenetic Features
Clonal evolution in the development of BPDCN remains to be elucidated. Simple and complex recurrent cytogenetic abnormalities have been reported, which demonstrate predominantly genomic losses, of which deletions of 5q are the most frequent aberrations in BPDCN with or without cutaneous manifestation; however, the gene responsible for the disease remains unknown [50].
In a molecular cytogenetic analysis of 46 BPDCN cases, monoallelic deletion of NR3C1 (5q31), encoding the glucocorticoid receptor (GCR), was identified in 13 of 47 (28%) BPDCN cases [51]. A retrospective analysis of 46 BPDCN cases with abnormal karyotype has also showed that 12p- is one of the most common structural aberrations in BPDCN [52]. The ETV6 and CDKN1B on 12p were suggested to deserve further investigation as potential markers of BPDCN [52]. Monoallelic and biallelic 12p/ETV6 deletions have been also suggested to be highly prevalent in BPDCN, by a different study, and their detection is enhanced by the use of fluorescence in situ hybridization (FISH) and array-based comparative genomic hybridization (aCGH) [53]. In addition, 12p/ETV6 may be present in the bone marrow of BPDCN patients in the absence of detectable disease suggesting that such alterations might represent an early pathogenic event [53]. The analysis of 21 cases with array-based comparative genomic hybridization (aCGH) showed that complete or partial chromosomal losses largely outnumbered the gains, with common deleted regions involving 9p21.3 (CDKN2A/CDKN2B), 13q13.1-q14.3 (RB1), 12p13.2-p13.1 (CDKN1B), 13q11-q12 (LATS2), and 7p12.2 (IKZF1) regions [26]. CDKN2A/CDKN2B deletion was confirmed by FISH [26].
The gene expression profile (GEP) of 25 BPDCN samples was analyzed and compared with that of pDCs, their postulated normal counterpart [8]. It was the first speculation about the cellular derivation of BPDCN, suggested to be originated from the myeloid lineage and in particular, from resting pDCs. The GEP of BPDCN is characterized by aberrant NF-kappaB pathway activation, while its genomic landscape is dominated by structural chromosomal alterations involving ETV6, MYC, and NR3C1, as well as mutations in epigenetic regulators particularly TET2 [43]. TET2 and TP53 mutations are frequently observed in BPDCN [54]. Using targeted high-coverage massive parallel sequencing, 50 common cancer genes have also been investigated in 33 BPDCN samples [55]. Point mutations were revealed in NRAS (27.3% of cases), ATM (21.2%), MET, KRAS, IDH2, KIT (9.1% each), APC, and RB1 (6.1%), as well as in VHL, BRAF, MLH1, TP53, and RET1 (3% each) [55].
Whole-exome sequencing (WES) of three BPDCN cases revealed 37–99 deleterious gene mutations per exome (such as IKZF3, HOXB9, UBE2G2 and ZEB2) with no common affected genes between patients, but with clear overlap in terms of molecular and disease pathways (hematological and dermatological disease) [56]. Half of the tumors had mutations affecting either the DNA methylation or chromatin remodeling pathways [56]. In a different study, WES analysis of fourteen BPDCN patients and the patient-derived CAL-1 cell line revealed twenty-five epigenetic modifiers mutated (e.g., ASXL1, TET2, SUZ12, ARID1A, PHF2, CHD8), with ASXL1 being the most frequently affected (28.6% of cases) [57].
The E-box transcription factor TCF4 has been identified as a master regulator of the BPDCN oncogenic program using RNAi screening [58]. TCF4 served as a faithful diagnostic marker of BPDCN, and its downregulation caused the loss of the BPDCN-specific gene expression program and apoptosis [58]. Moreover, several additional genetic observations have been made lately, based mainly in case reports. These include cases with EWSR1 gene rearrangement [59], loss of genomic DNA copy numbers in the p18, p16, p27, and RB loci [60], AT-Rich Interaction Domain 1A (ARID1A) gene mutation [61], and absence of MYD88 L265P mutation [62].
Alterations of the cell-cycle checkpoint controlling proteins p27 (KIP1), encoded by CDKN1B, p16(INK4a), encoded by CDKN2A, and RB1 may exert a profound effect in malignant transformation in BPDCN [63]. The investigation of clonal evolution in a case of BPDCN, by analyzing the distribution of gene mutations in tumor cells and non-tumor blood cells, revealed that BPDCN originated from clonal hematopoiesis with the p.K1005fs TET2 and p.P95H SRSF2 mutations via acquisition of the additional p.D1129fs TET2 and p.L287fs NPM1 mutations [64].
The implication of 8q24/MYC in BPDCN cases is of special concern. 8q24/MYC rearrangements occur in 10–15% of BPDCN, often partnered with non-immunoglobulin chromosomal loci, and may play a role in BPDCN pathogenesis [65]. Boddu PC et al. revealed that 5 of 41 (12%) patients with BPDCN had 8q24/MYC rearrangements, including 2 with t(6;8)(p21;q24), 1 with t(8;14)(q24;q32), 1 with t(X;8)(q24;q24), and 1 with t(3;8)(p25;q24) [65]. Recently, in a study of 118 cases, forty-one (38%) MYC(+)BPDCN (positive for rearrangement and expression) and 59 (54%) MYC(−)BPDCN (both negative) cases were identified, while MYC(+)BPDCN cases showed older onset, poorer outcome, and localized skin tumors more commonly than MYC(−)BPDCN [66•]. In a different study of 16 cases, cytogenetic analysis revealed a single recurrent translocation partner of MYC at 6p21 in 11 cases (69%), whereas four cases showed different MYC translocation partners (2p12, Xq24, 3p25, and 14q32) [67]. It seems that translocations involving the 8q24/MYC locus more frequently manifest as t(6;8)(p21;q24), and, given its association with specific clinicopathological features suggesting even more aggressive behavior, t(6;8)(p21;q24) indicate a genetically defined subgroup within BPDCN [67]. It is remarkable that a case report has been published with immunoblastoid morphology and MYC rearrangement and overexpression [27], suggesting a distinct BPDCN profile. The identification of SUPT3H as a novel 8q24/MYC partner in BPDCN with t(6;8)(p21;q24) translocation has also been previously made [68].
Rare rearrangements that have been reported in BPDCN include a case with t(11;19)(q23;p13.3), KMT2A(MLL) rearranged [69], a pediatric case of BPDCN with a KMT2A (MLL)-MLLT1 rearrangement confirmed by molecular study [70], and a Philadelphia chromosome-positive BPDCN case [71].
Treatment
There is still no consensus for the treatment of BPDCN. Intensive therapy for acute leukemia can be useful, but allogeneic BMT has a greater chance of long-term survival. The majority of patients initially respond to multi-agent chemotherapy, though most relapse within a year, and the prognosis is very poor. Existing data on the clinical behavior of BPDCN are limited because reported outcomes are from small retrospective series, and standardized treatment guidelines are lacking [25••].
Intensive first-line therapy and “lymphoid-type” chemotherapy regimens have been associated with better outcomes [25••]. Despite the fact that BPDCN is often initially limited to the skin, only an aggressive initial therapy may improve the patients’ prognosis. Local treatments, such radiation therapy, seem useless [72].
Formerly, the therapeutic approach of BPDCN was based on regimens used for acute lymphoblastic or myeloid leukemia and non-Hodgkin’s lymphoma [e.g., hyperCVAD, (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high dose methotrexate and cytarabine)] and CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone-based regimens) followed by allogeneic stem cell transplantation (allo-HSCT) for eligible patients [73]. Front-line induction chemotherapy with HyperCVAD can yield high remission rates, but allo-HSCT is required for long-term durable remissions [74]. Auto-HSCT for BPDCN in CR1 (1st complete response) appeared to provide promising results and deserved further evaluation in the setting of prospective trials [75]. In the most recent study of 59 patients with BPDCN, the median overall survival from diagnosis was 24 months, and outcomes were similar in patients with “skin only” or with systemic disease at presentation [25••]. Only 55% of patients received intensive chemotherapy, and 42% of patients underwent stem cell transplantation.
Alternative treatment options that have been previously used for BPDCN treatment are CD123-related therapies, venetoclax, nuclear factor-kappa B (NF-kB) inhibitors, BET inhibitors, demethylating agents, and other chemotherapy agents, such as pralatrexate, enasidenib, l-asparaginase with methotrexate and dexamethasone, gemcitabine, docetaxel, and bendamustine.
While the current standard treatment for BPDCN is acute leukemia-based regimen followed by HSCT for transplant-eligible patients, there are very promising results for CD123-directed therapies [73]. The future of BPDCN treatment may include targeted therapies without the need for cytotoxic chemotherapy [73]. In December 2018, tagraxofusp [Elzonris], an intravenously administered CD123-directed cytotoxin that was developed by Stemline Therapeutics, Inc., received its first global approval in the USA for the treatment of BPDCN in adults and in pediatric patients aged 2 years and older [76•]. A centralized registration application for the use of tagraxofusp in patients with BPDCN is under review in the EU.
Tagraxofusp (SL-401) is a CD123-directed cytotoxin consisting of human interleukin-3 fused to truncated diphtheria toxin that has shown robust activity in BPDCN [77] and considerable promise in ongoing clinical trials [78]. SL-401 was also well tolerated in pediatric patients with BPDCN, and further testing of this agent in children is warranted [79]. While SL-401 has shown potential to provide durable responses even without transplant, we do not yet know whether it will be effective as a means to avoid transplant in patients who are otherwise eligible [80]. The cytotoxicity of SL-401 was assessed in patient-derived BPDCN cell lines (CAL-1 and GEN2.2) and in primary BPDCN cells isolated from 12 patients using FC and an in vitro cytotoxicity assay [81]. SL-401 exhibited a robust cytotoxicity against BPDCN cells in a dose-dependent manner [81]. In a separate study, seven of 9 evaluable (78%) BPDCN patients had major responses including 5 complete responses and 2 partial responses after a single course of SL-401 [82]. The median duration of responses was 5 months (range, 1–20+ months) [82]. In a very recent open-label, multicohort study, 47 patients were assigned with untreated or relapsed BPDCN to receive an intravenous infusion of tagraxofusp at a dose of 7 mug or 12 mug per kilogram of body weight on days 1 to 5 of each 21-day cycle [83•]. Treatment continued until disease progression or unacceptable toxic effects. Of the 47 patients, 32 were receiving tagraxofusp as first-line treatment, and 15 had received previous treatment [83•]. Among the 29 previously untreated patients who received tagraxofusp at a dose of 12 mug per kilogram, the primary outcome occurred in 21 (72%), and the overall response rate was 90%; of these patients, 45% went on to undergo stem-cell transplantation [83•]. Survival rates at 18 and 24 months were 59% and 52%, respectively. Among the 15 previously treated patients, the response rate was 67%, and the median overall survival was 8.5 months [83•]. Serious adverse events included capillary leak syndrome, while hepatic dysfunction and thrombocytopenia were common [83•].
According to Kerr D et al., all transplant-eligible patients should undergo allo-HSCT consolidation given the current available data indicating this is the optimal approach to achieve a long-term remission [80]. Once the CD123-directed therapies are established as standard regimens, future studies may be designed to investigate whether these therapies can be utilized without the use of transplant [80]. Furthermore, combination therapy using anti-CD123 agents with high-dose induction chemotherapy or other low-dose regimens for elderly/frail patients should be investigated [80]. Given its promising results in early clinical trials, it appears that CD123 is the most viable target for BPDCN, and future studies should continue to exploit its expression on BPDCN cells [80]. Additional CD123-directed therapies, especially chimeric antigen receptor-therapy (CAR-T), may also give promising results in trials that are currently underway [80].
It has been also disclosed that venetoclax or other BCL2 inhibitors undergo expedited clinical evaluation in BPDCN, alone, or in combination with other therapies [84]. In vivo clinical activity of venetoclax in patient-derived xenografts and in 2 patients with relapsed chemotherapy-refractory disease has been demonstrated, through primary tumor cell functional profiling to predict BCL2 antagonist sensitivity [84]. A different case report has supported the use of venetoclax in the off-label treatment of BPDCN with Bcl-2 overexpression [85].
An aberrant activation of the NF-kB pathway and a molecular shutoff of the NF-kB pathway with anti-NF-kB-treatment have been successfully demonstrated by GEP and IHC on the BPDCN cell line CAL-1 [8]. NF-kB inhibition in BPDCN cell lines, achieved using either an experimental specific inhibitor JSH23 or the clinical drug bortezomib, interferes in vitro with leukemic cell proliferation and survival [86]. Bortezomib efficiently inhibited the phosphorylation of the RelA NF-kB subunit in BPDCN cell lines and primary cells from patients in vitro and in vivo in a mouse model [86]. Bortezomib can be associated with other drugs used in different chemotherapy regimens to improve its impact on leukemic cell death [86].
Moreover, high-throughput drug screening revealed that bromodomain and extra-terminal domain inhibitors (BETis) induced BPDCN apoptosis, attributable to disruption of a BPDCN-specific transcriptional network controlled by TCF4-dependent super enhancers [58]. BETis retarded the growth of BPDCN xenografts, supporting their clinical evaluation in this malignancy [58]. Also, inhibitors for bromodomain and BETis and aurora kinases (AKis), inhibited CAL-1 (MYC(+)BPDCN) growth more effectively than PMDC05 (MYC(−)BPDCN) cell lines [66•], while a BCL2 inhibitor was effective in both CAL-1 and PMDC05, indicating that this inhibitor can be used to treat MYC(−)BPDCN [66•]. Another study pointed to NR3C1 as a haploinsufficient tumor suppressor in a subset of BPDCN and identified BET inhibition, acting at least partially via a long noncoding RNA (lncRNA) gene blockade, as a novel treatment option in BPDCN [51].
Additional reports have proposed several different potential therapeutic alternatives. Thus, case reports of three older patients with BPDCN demonstrated that azacitidine was insufficient as monotherapy to provide durable disease control but was a well-tolerated therapy [87]. The median survival in this small series was 17 months, consistent with previous reports in the literature, justifying the use of this therapy in patients who are unfit for intensive chemotherapy and HSCT [87]. l-asparaginase with methotrexate and dexamethasone had also been proposed as an effective treatment combination in BPDCN [88], while a case report suggested ABVD therapy as useful for patients with BPDCN who cannot receive HSCT [89]. Bendamustine hydrochloride, a well-tolerated bifunctional drug acting as an alkylating and antimetabolite agent, was tested in five cases of relapsed BPDCN with moderate results [90], and disease responses to pralatrexate [25••, 91, 92] and enasidenib [25••] have been identified. Gemcitabine and docetaxel have also been proposed as a novel treatment combination regimen for BPDCN [93]. Through the adoption of a preclinical BPDCN mouse model, established by the CAL-1 cell line xenografting, the efficacy of the combination of the epigenetic drugs 5′-azacytidine and decitabine in controlling the disease progression in vivo has also been demonstrated [57].
Liver X receptor (LXR) agonists have also been proposed as a novel therapeutic option, as it was demonstrated that the modified cholesterol homeostasis observed in BPDCN can be normalized by treatment with LXR agonists and apoptosis is triggered [94]. Finally, the efficacy of a novel chimeric monoclonal antibody (ch122A2 mAb) that mediates a strong cellular cytotoxicity directed against a specific human pDC marker, CD303, has been demonstrated in humanized mice, resulting in significant pDC depletion in bloodstream and secondary lymphoid organs such as spleen [95]. Thus, it could represent a promising cytotoxic mAb candidate for pathologies in which decreasing type I IFNs or pDCs depleting may improve patient prognosis [95].
A special comment should be made for CNS involvement. BPDCN patients studied at diagnosis frequently display occult CNS involvement and treatment of occult CNS disease might lead to a dramatically improved outcome of BPDCN [96]. Also, implementation of lumbar punctures and preventive intrathecal chemotherapy are proposed in BPDCN patients with leukemic manifestation during the remission stage [97].
Radiation
BPDCN is highly aggressive even without systemic dissemination, and radiotherapy appears to be ineffective in treating this tumor [98]. According to a case report, the simultaneous combination of low-dose DeVIC (dexamethasone, VP16, ifosfamide, and carboplatin) therapy with local radiation therapy (LRT) could be useful in the treatment of limited-stage BPDCN even in the elderly [32].
Transplantation
Regardless of the initial extension of the disease, it has been suggested that only BMT significantly improved the outcome [72]. BPDCN with marrow involvement behaves like acute myeloid leukemia (AML), and aggressive treatment followed by stem cell transplantation may lead to long-term remission in selected cases. A study of 45 consecutive patients who received an allo-HSCT (n = 37) or an auto-HSCT (n = 8) regardless of age, pre-transplant therapies, or remission status at transplantation, revealed efficacy of allo-HSCT, especially in patients in first complete remission (CR1), and lack of efficacy of auto-HSCT [99]. Moreover, allo-HSCT in CR1 yielded superior 3-year OS (versus not in CR1) [99]. In a large meta-analysis of four studies (128 patients), the pooled OS rate was 50% for all patients [100•]. Among patients who underwent allografting whose disease was in CR1, pooled OS, and PFS/DFS rates were 67% and 53%, respectively [100•]. For patients who underwent allografting in > CR1, pooled OS, and PFS/DFS rates were 7% for both outcomes. Relapse rates were higher when reduced-intensity regimens were used (40% vs. 18%) [100•]. In an older study, reduced-intensity conditioning (RIC) allo-HSCT from unrelated donors proved feasible and seemed to be effective in elderly patients with BPDCN, suggesting that allo-HSCT should be pursued aggressively in patients with this otherwise fatal disease up to 70 years of age [101]. RIC/nonmyeloablative (RIC/NMA) conditioning regimens were found equivalent to myeloablative conditioning (MAC) in terms of outcome, confirming that long-lasting remissions can be achieved in this disease, even in patients aged 60 or older [102]. RIC/NMA should thus be proposed to patients not eligible for MAC, because of their age or co-morbidities, while representing the majority of patients suffering from BPDCN [102]. Moreover, a case report has been presented, where the addition of IL-2 and IFN-a to the donor leukocyte infusions resulted in a strong graft-versus-leukemia (GVL) effect, probably by enhancing T- and NK-alloreactivity, activating pDC-blasts and augmenting their Ag-presenting properties [103]. The usefulness of allo-HSCT in CR1 for pediatric BPDCN with skin involvement has also been suggested in a case report [104].
The Experience from Children
In a systematic literature review published in 2017, 74 children and 283 adults aged 19 or over were reviewed and compared [105••]. Age was shown to be an independent prognostic factor predictive of more favorable outcomes across measures including initial response to therapy, likelihood of relapse, and overall survival at follow-up [105••]. The distribution of affected organs at diagnosis was similar, and the type of clinical presentation did not affect prognosis [105••]. Acute lymphoblastic leukemia (ALL)-type chemotherapy regimens were shown to be superior to other chemotherapy regimens (AML, lymphoma, ALL/lymphoma, other, or none) in inducing complete remission, and allo-HSCT was shown to increase mean survival time [105••]. HSCT may be reserved for children who relapse and achieve a second remission [106]. Besides, not all pediatric BPDCN patients may be able to achieve complete remission following chemotherapy with the high-risk ALL regimen, and other treatment options must be investigated in the future [107]. However, efficacy of AML therapy without stem-cell transplantation in a child with BPDCN has also been reported [108].
Remarkable are some unusual clinical presentations that have been previously published, such as an asymptomatic 8-year-old boy who noticed a painless mass within the subcutaneous tissues below the left calf [109], a solitary skin lesion mimicking traumatic purpura [110], and a case resembling acute rheumatic fever at presentation [111]. Skin lesions have been proposed as possible clues to relapse of pediatric BPDCN [112].
Differential Diagnosis
BPDCN was earlier called as blastic NK-cell lymphoma, agranular CD4 NK-cell leukemia, agranular CD4, and 56 positive hematodermic neoplasm [106]. The differential diagnosis includes myeloid sarcoma/AML, T cell lymphoblastic leukemia/lymphoma, NK-cell lymphoma/leukemia, myeloid/NK cell precursor acute leukemia, and some mature T cell lymphomas/leukemias [113, 114]. AML with MLL rearrangement and CD4+/CD56+ expression can be misdiagnosed as BPDCN [115]. BPDCN should be considered in differential diagnosis of blastic leukemia with an undifferentiated and ambiguous immunophenotype despite the absence of skin lesions [17], while an exhaustive immunohistochemical workup is required to differentiate it from myeloid sarcoma and extranodal NK/T cell lymphoma [116]. A case of myeloid leukemia cutis with MPO, CD4, CD56, CD123, and TCL1, has been previously published [117], and a case initially diagnosed and treated as non-Hodgkin CD4+ T cell lymphoma, which evolved with early CNS relapse after an initial remission, and died 2 months later, after a second failed attempt of chemotherapy [118]. Moreover, a rare case of BPDCN that was initially misinterpreted as cutaneous lupus erythematosus [119], and a histopathologically proven BPDCN initially misdiagnosed as breast infiltrating ductal carcinoma in a 39-year-old woman [120], have also been previously reported. It is worth noting that a case report was referred to the existence of BPDCN with a concomitant CD5-/CD10- B cell lymphoproliferative disorder [121].
A high degree of suspicion and bone marrow examination in patients with a new diagnosis of BPDCN is required to avoid diagnostic pitfalls [121]. FC seems to represent the most valuable approach to avoid misinterpretation and obtain a useful pattern for measurable residual disease evaluation. The evaluation of CD4 and CD56 expression for BPDCN diagnosis should always be considered in a low CD45/SS blast pattern and different from the typical pattern of monocytic leukemia, which has increased CD45 intensity and high SS. The absence of CD19, cytoplasmic CD3 and MPO positivity, and the identification of TCL1/CD56 co-expression, should always be confirmed for a definitive typical BPDCN diagnosis.
The Relation of BPDCN with the Myeloid Component
BPDCN is a rare, aggressive entity that frequently presents in extramedullary sites and can show morphologic and immunophenotypic overlap with myeloid neoplasms. Until recently, neoplasms derived from plasmacytoid dendritic cells (pDCs) were currently divided into two broad categories: mature pDC proliferations associated with myeloid neoplasms (MPDMN) and BPDCN, while only BPDCN has been recognized in the WHO 2016 classification of hematopoietic neoplasms. Recently, it was suggested that AML can exhibit pDC differentiation, with or without monocytic differentiation, in a manner distinct from MPDMN or BPDCN [122]. This was based on the identification of cases, having increased myeloblasts and prominent CD56-negative pDC proliferations comprising 5–26% of bone marrow or blood cellularity as measured by FC. Thus, the existence of myeloid neoplasms with immature pDC proliferations suggested the existence of a broader spectrum of pDC-associated neoplasms than currently recognized [122]. This was firstly described by Tsagarakis et al. through the presentation of four cases diagnosed as LAL [28]. These LAL cases revealed two significant distinct populations in the CD45/RT-SC defined “blast pattern” of FC, one of pDC origin, with a BPDCN phenotype although CD56-, and another of monoblastic or precursor myeloid origin [28]. Extended bone marrow infiltration and blastoid cell detection in peripheral blood, and no skin involvement, were documented in all four patients, supporting the absence of cells with mature morphology and the close association of pDCs with leukemic cells [28]. Similar observations were later made by Martin-Martin L et al., who suggested that the maturational profile of pDC blasts in BPDCN is highly heterogeneous, where blasts from cases with an immature pDC phenotype exhibit an uncommon CD56-phenotype, coexisting with CD34+ non-pDC tumor cells, typically in the absence of extramedullary (e.g., skin) disease at presentation [123]. Besides, in an older study, it was noticed that both mDC and pDC subsets in circulation exhibited the original leukemic chromosomal abnormality in AML cases, providing evidence that DC subsets in vivo may be affected by leukemogenesis and may contribute to leukemia escape from immune control [49].
The complicated correlation of BPDCN with myeloid neoplasms can be easily concluded by the proposal of a shared clonal origin of BPDCN and chronic myelomonocytic leukemia (CMML) [124], the reports of BPDCN cases associated with CMML [125, 126], the report of BPDCN with AML [127], and the report of cutaneous BPDCN occurring after spontaneous remission of AML [128] and of spontaneous regression of cutaneous BPDCN followed by acute monocytic leukemia evolving from MDS [129]. Maybe it is not accidental that a BPDCN-like phenotype has been proposed as a subgroup of npm1-mutated AML with worse prognosis [130], and nucleophosmin is nucleus-restricted (predictive of a germline NPM1 gene) in BPDCN, contrary to the cytoplasmic-mutated nucleophosmin (NPMc(+) AML) in AML [131], probably indicating a common progenitor of similar phenotype. Nevertheless, it seems that the status of CD56 is closely related to the maturational level of the initial leukemic clone.
Conclusions
BPDCN (BPDCN) is a rare, highly aggressive hematopoietic malignancy, characterized by cutaneous and bone marrow involvement and leukemic spread. Molecular data support the current WHO classification of the disease as a myeloid disorder and provide a biological rationale for the incorporation of epigenetic therapies for its treatment [56]. Chromosomal aberrations are frequent, and the mutational landscape of BPDCN is being rapidly characterized, although no obvious molecular target for chemoimmunotherapy has been identified [78]. At present, the diagnosis and management of BPDCN are still challenging. (ALL)-type chemotherapy followed by HSCT is commonly thought to be related to a favorable outcome in adults with BPDCN [132]. (ALL)-type chemotherapy alone seems enough in children with BPDCN with or without cutaneous lesions [132]. HSCT increases the mean survival time and should be performed for children who relapse and achieve a second remission [132]. A disease-specific Twitter community: #BPDCN = “BPDCN on social media” has been created, which has led to higher levels of engagement and discussion in the field [133].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Awasthi NP, Qayoom S, Dabadghao S. Blastic plasmacytoid dendritic cell neoplasm presenting as leukemia without cutaneous lesion. J Cancer Res Ther. 2017;13(6):1056–8.
Fernandes F, Barreira R, Cortez J, Silveira M, Bain BJ. The distinctive cytology and disease evolution of blastic plasmacytoid dendritic cell neoplasm. Am J Hematol. 2018;93(11):1431–2.
Laribi K, Denizon N, Besancon A, Farhi J, Lemaire P, Sandrini J, et al. Blastic plasmacytoid dendritic cell neoplasm: from origin of the cell to targeted therapies. Biol Blood Marrow Transplant. 2016;22(8):1357–67.
Lichtman MA, Segel GB. Uncommon phenotypes of acute myelogenous leukemia: basophilic, mast cell, eosinophilic, and myeloid dendritic cell subtypes: a review. Blood Cells Mol Dis. 2005;35(3):370–83.
Petrella T, Facchetti F. Tumoral aspects of plasmacytoid dendritic cells: what do we know in 2009? Autoimmunity. 2010;43(3):210–4.
Osaki Y, Yokohama A, Saito A, Tahara K, Yanagisawa K, Ogawa Y, et al. Characterization of CD56+ dendritic-like cells: a normal counterpart of blastic plasmacytoid dendritic cell neoplasm? PLoS One. 2013;8(11):e81722.
Sapienza MR, Fuligni F, Agostinelli C, Tripodo C, Righi S, Laginestra MA, et al. Molecular profiling of blastic plasmacytoid dendritic cell neoplasm reveals a unique pattern and suggests selective sensitivity to NF-kB pathway inhibition. Leukemia. 2014;28(8):1606–16.
• Yu H, Zhang P, Yin X, Yin Z, Shi Q, Cui Y, et al. Human BDCA2+CD123+CD56+ dendritic cells (DCs) related to blastic plasmacytoid dendritic cell neoplasm represent a unique myeloid DC subset. Protein Cell. 2015;6(4):297–306 This study presents for the first time a different option about the ontogeny of BPDCN.
Kaur V, Swami A, Shebli A, Shalin S, Veeraputhiran M, Emanuel P, et al. A rare case of blastic plasmacytoid dendritic cell neoplasm with deletion 7q.31, in the setting of heavy pre-treatment with alkylating chemotherapy. J Oncol Pharm Pract. 2017;23(7):552–6.
Atalay F, Demirci GT, Bayramgurler D, Atesoglu EB, Yildiz S. Blastic plasmacytoid dendritic cell neoplasm: skin and bone marrow infiltration of three cases and the review of the literature. Indian J Hematol Blood Transfus. 2015;31(2):302–6.
Julia F, Petrella T, Beylot-Barry M, Bagot M, Lipsker D, Machet L, et al. Blastic plasmacytoid dendritic cell neoplasm: clinical features in 90 patients. Br J Dermatol. 2013;169(3):579–86.
Cui XB, Jin J, Pang XL, Li S, Liu CX, Li TT, et al. A case of blastic plasmacytoid dendritic cell neoplasm with ecchymotic lesions on the whole body. Int J Clin Exp Pathol. 2014;7(7):4391–9.
Rauh MJ, Rahman F, Good D, Silverman J, Brennan MK, Dimov N, et al. Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation, lacking cutaneous involvement: case series and literature review. Leuk Res. 2012;36(1):81–6.
Prematilleke I, Mohan V, Roberts I, Protheroe A, Gatter K. Blastic plasmacytoid dendritic cell neoplasm presenting as a renal mass. Histopathology. 2011;59(4):799–801.
Chou PY, Lai CL, Huang P. Complete monocular vision loss due to optic nerve involvement of blastic plasmacytoid dendritic cell neoplasm. Acta Oncol. 2018;57(7):989–91.
Lee SE, Park HY, Kwon D, Jeon YK, Kim WY. Blastic plasmacytoid dendritic cell neoplasm with unusual extracutaneous manifestation: two case reports and literature review. Medicine (Baltimore). 2019;98(6):e14344.
Andrese E, Solovastru LG, Dimofte G, Ferariu D, Porumb V, Vata D, et al. Blastic plasmacytoid dendritic cell neoplasm --a rapidly evolving entity. Case report. Rev Med Chir Soc Med Nat Iasi. 2015;119(2):379–83.
Endo K, Mihara K, Oiwa H, Yoshida T, Mino T, Sasaki N, et al. Lung involvement at initial presentation in blastic plasmacytoid dendritic cell neoplasm lacking cutaneous lesion. Ann Hematol. 2013;92(2):269–70.
Saito M, Irie T, Miyashita K, Tanino M. Colon involvement in blastic plasmacytoid dendritic cell neoplasm. Intern Med. 2015;54(13):1677.
Blennerhassett R, McCaughan G, Tegg E. An unexpected diagnosis: leukaemic presentation of blastic plasmacytoid dendritic cell neoplasm with massive splenomegaly. Pathology. 2018;50(7):773–5.
Daitoku S, Onimaru M, Tanimoto K, Kuroiwa M. Atraumatic splenic ruptures triggered both remission and death in a single case of blastic plasmacytoid dendritic cell neoplasm. J Clin Exp Hematop. 2019;59(1):40–5.
Owczarczyk-Saczonek A, Sokolowska-Wojdylo M, Olszewska B, Malek M, Znajewska-Pander A, Kowalczyk A, et al. Clinicopathologic retrospective analysis of blastic plasmacytoid dendritic cell neoplasms. Postepy Dermatol Alergol. 2018;35(2):128–38.
• Sapienza MR, Pileri A, Derenzini E, Melle F, Motta G, Fiori S, et al. Blastic plasmacytoid dendritic cell neoplasm: state of the art and prospects. Cancers (Basel). 2019;28;11(5). This is a very informative review about all the aspects of the disease. https://doi.org/10.3390/cancers11050595.
•• Taylor J, Haddadin M, Upadhyay VA, Grussie E, Mehta-Shah N, Brunner AM, et al. Multicenter analysis of outcomes in blastic plasmacytoid dendritic cell neoplasm offers a pretargeted therapy benchmark. Blood. 2019;134(8):678–87 This is the most contemporary cohort, which can be used for the evaluation of ongoing clinical trials.
Lucioni M, Novara F, Fiandrino G, Riboni R, Fanoni D, Arra M, et al. Twenty-one cases of blastic plasmacytoid dendritic cell neoplasm: focus on biallelic locus 9p21.3 deletion. Blood. 2011;118(17):4591–4.
Chang KC, Yu-Yun LJ, Sakamoto K, Baba S, Takeuchi K. Blastic plasmacytoid dendritic cell neoplasm with immunoblastoid morphology and MYC rearrangement and overexpression. Pathology. 2019;51(1):100–2.
Tsagarakis NJ, Kentrou NA, Papadimitriou KA, Pagoni M, Kokkini G, Papadaki H, et al. Acute lymphoplasmacytoid dendritic cell (DC2) leukemia: results from the hellenic dendritic cell leukemia study group. Leuk Res. 2010;34(4):438–46.
Nakatsuka S, Nagano T, Kimura H, Nagatomo T, Urase Y, Hashimoto K. A case of blastic plasmacytoid dendritic cell neoplasm: cytomorphological findings of the touch imprint specimen of lymph node. Diagn Cytopathol. 2013;41(1):67–70.
Hwang SM, Kim HK. Necklace-like microvacuoles of tumor cells in blastic plasmacytoid dendritic cell neoplasm. Korean J Hematol. 2010;45(1):7.
Ferreira J, Gasparinho MG, Fonseca R. Cytomorphological features of blastic plasmacytoid dendritic cell neoplasm on FNA and cerebrospinal fluid cytology: a review of 6 cases. Cancer Cytopathol. 2016;124(3):196–202.
Sugimoto KJ, Shimada A, Yamaguchi N, Imai H, Wakabayashi M, Sekiguchi Y, et al. Sustained complete remission of a limited-stage blastic plasmacytoid dendritic cell neoplasm followed by a simultaneous combination of low-dose DeVIC therapy and radiation therapy: a case report and review of the literature. Int J Clin Exp Pathol. 2013;6(11):2603–8.
Alayed K, Patel KP, Konoplev S, Singh RR, Routbort MJ, Reddy N, et al. TET2 mutations, myelodysplastic features, and a distinct immunoprofile characterize blastic plasmacytoid dendritic cell neoplasm in the bone marrow. Am J Hematol. 2013;88(12):1055–61.
Hwang K, Park CJ, Jang S, Chi HS, Huh JR, Lee JH, et al. Immunohistochemical analysis of CD123, CD56 and CD4 for the diagnosis of minimal bone marrow involvement by blastic plasmacytoid dendritic cell neoplasm. Histopathology. 2013;62(5):764–70.
Ohe R, Aung NY, Shiono Y, Utsunomiya A, Kabasawa T, Tamazawa N, et al. Detection of minimal bone marrow involvement of blastic plasmacytoid dendritic cell neoplastic cells - CD303 immunostaining as a diagnostic tool. J Clin Exp Hematop. 2018;58(1):1–9.
Pagano L, Valentini CG, Grammatico S, Pulsoni A. Blastic plasmacytoid dendritic cell neoplasm: diagnostic criteria and therapeutical approaches. Br J Haematol. 2016;174(2):188–202.
Julia F, Dalle S, Duru G, Balme B, Vergier B, Ortonne N, et al. Blastic plasmacytoid dendritic cell neoplasms: clinico-immunohistochemical correlations in a series of 91 patients. Am J Surg Pathol. 2014;38(5):673–80.
Angelot-Delettre F, Biichle S, Ferrand C, Seilles E, Gaugler B, Harrivel V, et al. Intracytoplasmic detection of TCL1--but not ILT7-by flow cytometry is useful for blastic plasmacytoid dendritic cell leukemia diagnosis. Cytometry A. 2012;81(8):718–24.
Sangle NA, Schmidt RL, Patel JL, Medeiros LJ, Agarwal AM, Perkins SL, et al. Optimized immunohistochemical panel to differentiate myeloid sarcoma from blastic plasmacytoid dendritic cell neoplasm. Mod Pathol. 2014;27(8):1137–43.
Inoue D, Maruyama K, Aoki K, Nagano S, Maruoka H, Imai Y, et al. Blastic plasmacytoid dendritic cell neoplasm expressing the CD13 myeloid antigen. Acta Haematol. 2011;126(2):122–8.
Mitteldorf C, Bertsch HP, Baumgart M, Haase D, Wulf G, Schon MP, et al. Lacking CD56 expression in a relapsing cutaneous blastic plasmacytoid dendritic cell neoplasm after allogeneic bone marrow transplantation: FISH analysis revealed loss of 11q. J Eur Acad Dermatol Venereol. 2011;25(10):1225–9.
Liu H, Li S. Pediatric blastic plasmacytoid dendritic cell neoplasm, acute leukemic variant. Blood. 2015;126(25):2764.
Khoury JD. Blastic plasmacytoid dendritic cell neoplasm. Curr Hematol Malig Rep. 2018;13(6):477–83.
Johnson RC, Kim J, Natkunam Y, Sundram U, Freud AG, Gammon B, et al. Myeloid cell nuclear differentiation antigen (MNDA) expression distinguishes extramedullary presentations of myeloid leukemia from blastic plasmacytoid dendritic cell neoplasm. Am J Surg Pathol. 2016;40(4):502–9.
Salva KA, Haemel AK, Pincus LB, Liu J, Sundram U, Guitart J, et al. Expression of CD31/PECAM-1 (platelet endothelial cell adhesion molecule 1) by blastic plasmacytoid dendritic cell neoplasms. JAMA Dermatol. 2014;150(1):73–6.
Hashikawa K, Niino D, Yasumoto S, Nakama T, Kiyasu J, Sato K, et al. Clinicopathological features and prognostic significance of CXCL12 in blastic plasmacytoid dendritic cell neoplasm. J Am Acad Dermatol. 2012;66(2):278–91.
Garnache-Ottou F, Feuillard J, Ferrand C, Biichle S, Trimoreau F, Seilles E, et al. Extended diagnostic criteria for plasmacytoid dendritic cell leukaemia. Br J Haematol. 2009;145(5):624–36.
Ma L, Delforge M, van Duppen V, Verhoef G, Emanuel B, Boogaerts M, et al. Circulating myeloid and lymphoid precursor dendritic cells are clonally involved in myelodysplastic syndromes. Leukemia. 2004;18(9):1451–6.
Mohty M, Jarrossay D, Lafage-Pochitaloff M, Zandotti C, Briere F, de Lamballeri XN, et al. Circulating blood dendritic cells from myeloid leukemia patients display quantitative and cytogenetic abnormalities as well as functional impairment. Blood. 2001;98(13):3750–6.
Fu Y, Fesler M, Mahmud G, Bernreuter K, Jia D, Batanian JR. Narrowing down the common deleted region of 5q to 6.0 Mb in blastic plasmacytoid dendritic cell neoplasms. Cancer Gene Ther. 2013;206(7–8):293–8.
Emadali A, Hoghoughi N, Duley S, Hajmirza A, Verhoeyen E, Cosset FL, et al. Haploinsufficiency for NR3C1, the gene encoding the glucocorticoid receptor, in blastic plasmacytoid dendritic cell neoplasms. Blood. 2016;127(24):3040–53.
Tang Z, Tang G, Wang SA, Lu X, Young KH, Bueso-Ramos CE, et al. Simultaneous deletion of 3'ETV6 and 5'EWSR1 genes in blastic plasmacytoid dendritic cell neoplasm: case report and literature review. Mol Cytogenet. 2016;9:23.
Tang Z, Li Y, Wang W, Yin CC, Tang G, Aung PP, et al. Genomic aberrations involving 12p/ETV6 are highly prevalent in blastic plasmacytoid dendritic cell neoplasms and might represent early clonal events. Leuk Res. 2018;73:86–94.
Jardin F, Ruminy P, Parmentier F, Troussard X, Vaida I, Stamatoullas A, et al. TET2 and TP53 mutations are frequently observed in blastic plasmacytoid dendritic cell neoplasm. Br J Haematol. 2011;153(3):413–6.
Stenzinger A, Endris V, Pfarr N, Andrulis M, Johrens K, Klauschen F, et al. Targeted ultra-deep sequencing reveals recurrent and mutually exclusive mutations of cancer genes in blastic plasmacytoid dendritic cell neoplasm. Oncotarget. 2014;5(15):6404–13.
Menezes J, Acquadro F, Wiseman M, Gomez-Lopez G, Salgado RN, Talavera-Casanas JG, et al. Exome sequencing reveals novel and recurrent mutations with clinical impact in blastic plasmacytoid dendritic cell neoplasm. Leukemia. 2014;28(4):823–9.
Sapienza MR, Abate F, Melle F, Orecchioni S, Fuligni F, Etebari M, et al. Blastic plasmacytoid dendritic cell neoplasm: genomics mark epigenetic dysregulation as a primary therapeutic target. Haematologica. 2019;104(4):729–737. https://doi.org/10.3324/haematol.2018.202093. Accessed 31 Oct 2018.
Ceribelli M, Hou ZE, Kelly PN, Huang DW, Wright G, Ganapathi K, et al. A Druggable. Cancer Cell. 2016;30(5):764–78.
Cao Q, Liu F, Niu G, Xue L, Han A. Blastic plasmacytoid dendritic cell neoplasm with EWSR1 gene rearrangement. J Clin Pathol. 2014;67(1):90–2.
Oiso N, Tatsumi Y, Arao T, Rai S, Kimura M, Nakamura S, et al. Loss of genomic DNA copy numbers in the p18, p16, p27 and RB loci in blastic plasmacytoid dendritic cell neoplasm. Eur J Dermatol. 2012;22(3):393–4.
Wang L, Yang M, Zhang X, Yang C, Huang X, Wang Z, et al. ARID1A mutation in blastic plasmacytoid dendritic cell neoplasm. Haematologica. 2017;102(11):e470–2.
Fiandrino G, Arra M, Riboni R, Lucioni M, Dallera E, Arcaini L, et al. Absence of MYD88 L265P mutation in blastic plasmacytoid dendritic cell neoplasm. Br J Dermatol. 2013;168(4):883–4.
Wiesner T, Obenauf AC, Cota C, Fried I, Speicher MR, Cerroni L. Alterations of the cell-cycle inhibitors p27(KIP1) and p16(INK4a) are frequent in blastic plasmacytoid dendritic cell neoplasms. J Invest Dermatol. 2010;130(4):1152–7.
Suma S, Sakata-Yanagimoto M, Nguyen TB, Hattori K, Sato T, Noguchi M, et al. Blastic plasmacytoid dendritic cell neoplasm arising from clonal hematopoiesis. Int J Hematol. 2018;108(4):447–51.
Boddu PC, Wang SA, Pemmaraju N, Tang Z, Hu S, Li S, et al. 8q24/MYC rearrangement is a recurrent cytogenetic abnormality in blastic plasmacytoid dendritic cell neoplasms. Leuk Res. 2018;66:73–8.
• Sakamoto K, Katayama R, Asaka R, Sakata S, Baba S, Nakasone H, et al. Recurrent 8q24 rearrangement in blastic plasmacytoid dendritic cell neoplasm: association with immunoblastoid cytomorphology, MYC expression, and drug response. Leukemia. 2018;32(12):2590–603 This study reveals the multipotential role of MYC in BPDCN.
Sumarriva LL, Chisholm KM, Carneal E, Nagy A, Cascio MJ, Yan J, et al. An analysis of blastic plasmacytoid dendritic cell neoplasm with translocations involving the MYC locus identifies t(6;8)(p21;q24) as a recurrent cytogenetic abnormality. Histopathology. 2018;73(5):767–76.
Nakamura Y, Kayano H, Kakegawa E, Miyazaki H, Nagai T, Uchida Y, et al. Identification of SUPT3H as a novel 8q24/MYC partner in blastic plasmacytoid dendritic cell neoplasm with t(6;8)(p21;q24) translocation. Blood Cancer J. 2015;5:e301.
Gehlbach D, Koduru P, John G, Fuda F, Frankel AE, Chen W. Blastic plasmacytoid dendritic cell neoplasm with t(11;19)(q23;p13.3);KMT2A(MLL) rearranged: a diagnostic challenge. Br J Haematol, 2017. 176(1):8.
Yang N, Huh J, Chung WS, Cho MS, Ryu KH, Chung HS. KMT2A (MLL)-MLLT1 rearrangement in blastic plasmacytoid dendritic cell neoplasm. Cancer Gene Ther. 2015;208(9):464–7.
Adams RL, McCarthy C, Bird RJ. Philadelphia chromosome-positive blastic plasmacytoid dendritic cell leukemia. Cancer Genet Cytogenet. 2009;195(2):186–8.
Dalle S, Beylot-Barry M, Bagot M, Lipsker D, Machet L, Joly P, et al. Blastic plasmacytoid dendritic cell neoplasm: is transplantation the treatment of choice? Br J Dermatol. 2010;162(1):74–9.
Kerr D, Sokol L. The advances in therapy of blastic plasmacytoid dendritic cell neoplasm. Expert Opin Investig Drugs. 2018;27(9):733–9.
Deotare U, Yee KW, Le LW, Porwit A, Tierens A, Musani R, et al. Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: 10-color flow cytometry diagnosis and HyperCVAD therapy. Am J Hematol. 2016;91(3):283–6.
Aoki T, Suzuki R, Kuwatsuka Y, Kako S, Fujimoto K, Taguchi J, et al. Long-term survival following autologous and allogeneic stem cell transplantation for blastic plasmacytoid dendritic cell neoplasm. Blood. 2015;125(23):3559–62.
• Syed YY. Tagraxofusp: first global approval. Drugs. 2019;79(5):579–83 The first global approval of tagraxofusp [Elzonris] in the USA, for the treatment of BPDCN in adults and in pediatric patients aged 2 years and older.
Alkharabsheh O, Frankel AE. Clinical activity and tolerability of SL-401 (Tagraxofusp): recombinant diphtheria toxin and Interleukin-3 in hematologic malignancies. Biomedicines. 2019;5:7(1). https://doi.org/10.3390/biomedicines7010006.
Sullivan JM, Rizzieri DA. Treatment of blastic plasmacytoid dendritic cell neoplasm. Hematology Am Soc Hematol Educ Program. 2016;2016(1):16–23.
Sun W, Liu H, Kim Y, Karras N, Pawlowska A, Toomey D, et al. First pediatric experience of SL-401, a CD123-targeted therapy, in patients with blastic plasmacytoid dendritic cell neoplasm: report of three cases. J Hematol Oncol. 2018;11(1):61.
Kerr D, Zhang L, Sokol L. Blastic plasmacytoid dendritic cell neoplasm. Curr Treat Options in Oncol. 2019;20(1):9.
Angelot-Delettre F, Roggy A, Frankel AE, Lamarthee B, Seilles E, Biichle S, et al. In vivo and in vitro sensitivity of blastic plasmacytoid dendritic cell neoplasm to SL-401, an interleukin-3 receptor targeted biologic agent. Haematologica. 2015;100(2):223–30.
Frankel AE, Woo JH, Ahn C, Pemmaraju N, Medeiros BC, Carraway HE, et al. Activity of SL-401, a targeted therapy directed to interleukin-3 receptor, in blastic plasmacytoid dendritic cell neoplasm patients. Blood. 2014;124(3):385–92.
• Pemmaraju N, Lane AA, Sweet KL, Stein AS, Vasu S, Blum W, et al. Tagraxofusp in blastic plasmacytoid dendritic-cell neoplasm. N Engl J Med. 2019;380(17):1628–37 A recent significant clinical study evaluating tagraxofusp.
Montero J, Stephansky J, Cai T, Griffin GK, Cabal-Hierro L, Togami K, et al. Blastic plasmacytoid dendritic cell neoplasm is dependent on BCL2 and sensitive to venetoclax. Cancer Discov. 2017;7(2):156–64.
Grushchak S, Joy C, Gray A, Opel D, Speiser J, Reserva J, et al. Novel treatment of blastic plasmacytoid dendritic cell neoplasm: a case report. Medicine (Baltimore). 2017;96(51):e9452.
Philippe L, Ceroi A, Bole-Richard E, Jenvrin A, Biichle S, Perrin S, et al. Bortezomib as a new therapeutic approach for blastic plasmacytoid dendritic cell neoplasm. Haematologica. 2017;102(11):1861–8.
Khwaja R, Daly A, Wong M, Mahe E, Cerquozzi S, Owen C. Azacitidine in the treatment of blastic plasmacytoid dendritic cell neoplasm: a report of 3 cases. Leuk Lymphoma. 2016;57(11):2720–2.
Gruson B, Vaida I, Merlusca L, Charbonnier A, Parcelier A, Damaj G, et al. L-asparaginase with methotrexate and dexamethasone is an effective treatment combination in blastic plasmacytoid dendritic cell neoplasm. Br J Haematol. 2013;163(4):543–5.
Tanikawa S, Sakuranaka H, Chong JM, Okada Y, Takimoto M. Sustained remission of blastic plasmacytoid dendritic cell neoplasm with ABVD chemotherapy. Rinsho Ketsueki. 2012;53(2):246–51.
Betrian S, Guenounou S, Luquet I, Demur C, Huynh A, Ysebaert L, et al. Bendamustine for relapsed blastic plasmacytoid dendritic cell leukaemia. Hematol Oncol. 2017;35(2):252–5.
Arranto C, Tzankov A, Halter J. Blastic plasmacytoid dendritic cell neoplasm with transient response to pralatrexate. Ann Hematol. 2017;96(4):681–2.
Sato S, Tanaka E, Tamai Y. Blastic plasmacytoid dendritic cell neoplasm with response to pralatrexate. Ann Hematol. 2019;98(3):801–3.
Ulrickson ML, Puri A, Lindstrom S, Cassaday RD, De PN, Becker PS. Gemcitabine and docetaxel as a novel treatment regimen for blastic plasmacytoid dendritic cell neoplasm. Am J Hematol. 2017;92(5):E75–7.
Ceroi A, Masson D, Roggy A, Roumier C, Chague C, Gauthier T, et al. LXR agonist treatment of blastic plasmacytoid dendritic cell neoplasm restores cholesterol efflux and triggers apoptosis. Blood. 2016;128(23):2694–707.
Fournier N, Jacque E, Fontayne A, Derache D, Dupont G, Verhaeghe L, et al. Improved in vitro and in vivo activity against CD303-expressing targets of the chimeric 122A2 antibody selected for specific glycosylation pattern. MAbs. 2018;10(4):651–63.
Martin-Martin L, Almeida J, Pomares H, Gonzalez-Barca E, Bravo P, Gimenez T, et al. Blastic plasmacytoid dendritic cell neoplasm frequently shows occult central nervous system involvement at diagnosis and benefits from intrathecal therapy. Oncotarget. 2016;7(9):10174–81.
Gao NA, Wang XX, Sun JR, Yu WZ, Guo NJ. Blastic plasmacytoid dendritic cell neoplasm with leukemic manifestation and ETV6 gene rearrangement: a case report. Exp Ther Med. 2015;9(4):1109–12.
Yu G, Wang W, Han Y, Liu J, Pan X, Qu G. Blastic plasmacytoid dendritic cell neoplasm presenting with a cutaneous tumor alone as the first symptom of onset: a case report and review of literature. Oncol Lett. 2015;9(2):819–21.
Kharfan-Dabaja MA, Al Malki MM, Deotare U, Raj RV, El-Jurdi N, Majhail N, et al. Haematopoietic cell transplantation for blastic plasmacytoid dendritic cell neoplasm: a North American multicentre collaborative study. Br J Haematol. 2017;179(5):781–9.
• Kharfan-Dabaja MA, Reljic T, Murthy HS, Ayala E, Kumar A. Allogeneic hematopoietic cell transplantation is an effective treatment for blastic plasmacytoid dendritic cell neoplasm in first complete remission: systematic review and meta-analysis. Clin Lymphoma Myeloma Leuk. 2018;18(11):703–9 A large meta-analysis evaluating the role of allografting in BPDCN treatment.
Dietrich S, Andrulis M, Hegenbart U, Schmitt T, Bellos F, Martens UM, et al. Blastic plasmacytoid dendritic cell neoplasia (BPDC) in elderly patients: results of a treatment algorithm employing allogeneic stem cell transplantation with moderately reduced conditioning intensity. Biol Blood Marrow Transplant. 2011;17(8):1250–4.
Leclerc M, de Peffault LR, Michallet M, Blaise D, Chevallier P, Rohrlich PS, et al. Can a reduced-intensity conditioning regimen cure blastic plasmacytoid dendritic cell neoplasm? Blood. 2017;129(9):1227–30.
Kaloyannidis P, Zomas A, Paterakis G, Vadikoliou C, Mallouri D, Sakkas L, et al. GVL effect in plasmacytoid DC leukemia/lymphoma. Bone Marrow Transplant. 2010;45(5):961–2.
Sakashita K, Saito S, Yanagisawa R, Tanaka M, Yoshikawa K, Hirabayashi K, et al. Usefulness of allogeneic hematopoietic stem cell transplantation in first complete remission for pediatric blastic plasmacytoid dendritic cell neoplasm with skin involvement: a case report and review of literature. Pediatr Blood Cancer. 2013;60(11):E140–2.
•• Kim MJ, Nasr A, Kabir B, de Nanassy J, Tang K, Menzies-Toman D, et al. Pediatric blastic plasmacytoid dendritic cell neoplasm: a systematic literature review. J Pediatr Hematol Oncol. 2017;39(7):528–37 The most significant review presenting the experience from children with BPDCN.
Jegalian AG, Buxbaum NP, Facchetti F, Raffeld M, Pittaluga S, Wayne AS, et al. Blastic plasmacytoid dendritic cell neoplasm in children: diagnostic features and clinical implications. Haematologica. 2010;95(11):1873–9.
Deng W, Yang M, Kuang F, Liu Y, Zhang H, Cao L, et al. Blastic plasmacytoid dendritic cell neoplasm in children: a review of two cases. Mol Clin Oncol. 2017;7(4):709–15.
Hansford JR, Kotecha RS, Jevon G, Cole CH, Gottardo NG. Efficacy of acute myeloid leukemia therapy without stem-cell transplantation in a child with blastic plasmacytoid dendritic cell neoplasm. Haematologica. 2013;98(3):e30–1.
Nizza D, Simoneaux SF. Blastic plasmacytoid dendritic cell neoplasm presenting as a subcutaneous mass in an 8-year-old boy. Pediatr Radiol. 2010;40(Suppl 1):S40–2.
Nomura H, Egami S, Kasai H, Yokoyama T, Fujimoto A, Sugiura M, et al. Blastic plasmacytoid dendritic cell neoplasm in a 7-year-old girl with a solitary skin lesion mimicking traumatic purpura. Acta Derm Venereol. 2015;95(2):231–2.
Rajkumari BD, Munikoty V, Sreedharanunni S, Jain R, Sachdeva MUS, Varma N. Childhood blastic plasmacytoid dendritic cell neoplasm mimicking acute rheumatic fever: report of an unusual clinical presentation and review of literature. J Pediatr Hematol Oncol. 2018;40(5):e327–9.
Dreyer S, Mednik S, Truong A, Worswick S, Scumpia P, Neill D, et al. Skin lesions serve as clues to relapse of pediatric blastic plasmacytoid dendritic cell neoplasm. Pediatr Dermatol. 2018;35(2):e132–5.
Anargyrou K, Paterakis G, Boutsis D, Politou M, Papadhimitriou SI, Siakandaris M, et al. An unusual case of CD4+ CD7+ CD56+ acute leukemia with overlapping features of type 2 dendritic cell (DC2) and myeloid/NK cell precursor acute leukemia. Eur J Haematol. 2003;71(4):294–8.
Shi Y, Wang E. Blastic plasmacytoid dendritic cell neoplasm: a clinicopathologic review. Arch Pathol Lab Med. 2014;138(4):564–9.
Lee JM, Kim IS, Lee JN, Park SH, Kim HH, Chang CL, et al. Acute myeloid leukemia with MLL rearrangement and CD4+/CD56+ expression can be misdiagnosed as Blastic Plasmacytoid dendritic cell neoplasm: two case reports. Ann Lab Med. 2016;36(5):494–7.
Rai MP, Bedi PS, Kandola SK, Kavuturu S, Singhal R. Blastic plasmacytoid dendritic cell neoplasm. Clin Case Rep. 2018;6(4):770–2.
Cronin DM, George TI, Reichard KK, Sundram UN. Immunophenotypic analysis of myeloperoxidase-negative leukemia cutis and blastic plasmacytoid dendritic cell neoplasm. Am J Clin Pathol. 2012;137(3):367–76.
Contreras L, Mercado L, Delgado C, Cabezas C, Starke L, Romero M, et al. Blastic plasmacytoid dendritic cell neoplasm with complete clinical remission with chemotherapy and central nervous system relapse: report of one case. Rev Med Chil. 2017;145(1):115–20.
Chang HJ, Lee MD, Yi HG, Lim JH, Lee MH, Shin JH, et al. A case of blastic plasmacytoid dendritic cell neoplasm initially mimicking cutaneous lupus erythematosus. Cancer Res Treat. 2010;42(4):239–43.
Chen KC, Su TC, Chen DR, Liou JH. A case report: blastic plasmacytoid dendritic cell neoplasm is misdiagnosed as breast infiltrating ductal carcinoma. Int J Surg Pathol. 2015;23(1):84–8.
Patel JL, Shetty S, Salama ME. An unusual case of cutaneous blastic plasmacytoid dendritic cell neoplasm with concomitant B-cell lymphoproliferative disorder. Am J Dermatopathol. 2011;33(3):e31–6.
Hamadeh F, Awadallah A, Meyerson HJ, Beck RC. Flow cytometry identifies a spectrum of maturation in myeloid neoplasms having plasmacytoid dendritic cell differentiation. Cytometry B Clin Cytom. 2020;98(1):43–51. https://doi.org/10.1002/cyto.b.21761. Accessed 5 Jan 2019.
Martin-Martin L, Lopez A, Vidriales B, Caballero MD, Rodrigues AS, Ferreira SI, et al. Classification and clinical behavior of blastic plasmacytoid dendritic cell neoplasms according to their maturation-associated immunophenotypic profile. Oncotarget. 2015;6(22):19204–16.
Brunetti L, Di Batista V, Venanzi A, Schiavoni G, Martelli MP, Ascani S, et al. Blastic plasmacytoid dendritic cell neoplasm and chronic myelomonocytic leukemia: a shared clonal origin. Leukemia. 2017;31(5):1238–40.
Hu Z, Sun T. Blastic plasmacytoid dendritic cell neoplasm associated with chronic myelomonocytic leukemia. Blood. 2016;128(12):1664.
Lebecque B, Vial JP, Pigneux A, Lechevalier N. Chronic myelomonocytic leukaemia followed by blastic plasmacytoid dendritic cell neoplasm. Br J Haematol. 2019;185(3):398. https://doi.org/10.1111/bjh.15794. Accessed 19 Feb 2019.
Voelkl A, Flaig M, Roehnisch T, Alpay N, Schmidmaier R, Oduncu F. Blastic plasmacytoid dendritic cell neoplasm with acute myeloid leukemia successfully treated to a remission currently of 26 months duration. Leuk Res. 2011;35(6):e61–3.
Xie W, Zhao Y, Cao L, Huang W, Wang Y, Huang H. Cutaneous blastic plasmacytoid dendritic cell neoplasm occurring after spontaneous remission of acute myeloid leukemia: a case report and review of literature. Med Oncol. 2012;29(4):2417–22.
Yasuda H, Takaku T, Tomomatsu J, Hosone M, Tanaka H, Komatsu N. Spontaneous regression of cutaneous blastic plasmacytoid dendritic cell neoplasm followed by acute monocytic leukemia evolving from myelodysplastic syndrome. Intern Med. 2014;53(23):2717–20.
Minetto P, Guolo F, Clavio M, Kunkl A, Colombo N, Carminati E, et al. A blastic plasmacytoid dendritic cell neoplasm-like phenotype identifies a subgroup of npm1-mutated acute myeloid leukemia patients with worse prognosis. Am J Hematol. 2018;93(2):E33–5.
Facchetti F, Pileri SA, Agostinelli C, Martelli MP, Paulli M, Venditti A, et al. Cytoplasmic nucleophosmin is not detected in blastic plasmacytoid dendritic cell neoplasm. Haematologica. 2009;94(2):285–8.
Zhong XD, Wang LZ, Wang X, Chang J. Diffuse lung metastases in a child with blastic plasmacytoid dendritic cell neoplasm and review. Eur J Pediatr. 2014;173(12):1667–70.
Pemmaraju N, Utengen A, Gupta V, Thompson MA, Lane AA. Blastic plasmacytoid dendritic cell neoplasm (BPDCN) on social media: #BPDCN-increasing exposure over two years since inception of a disease-specific twitter community. Curr Hematol Malig Rep. 2018;13(6):581–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nikolaos J. Tsagarakis and Georgios Paterakis declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Leukemia
Rights and permissions
About this article
Cite this article
Tsagarakis, N.J., Paterakis, G. Dendritic Cell Leukemia: a Review. Curr Oncol Rep 22, 55 (2020). https://doi.org/10.1007/s11912-020-00921-y
Published:
DOI: https://doi.org/10.1007/s11912-020-00921-y