Abstract
Purpose of Review
Brain tumor-related epilepsy is a heterogenous syndrome involving variability in incidence, timing, pathophysiology, and clinical risk factors for seizures across different brain tumor pathologies. Seizure risk and disability are dynamic over the course of disease and influenced by tumor-directed treatments, necessitating individualized patient-centered management strategies to optimize quality of life.
Recent Findings
Recent translational findings in diffuse gliomas indicate a dynamic bidirectional relationship between glioma growth and hyperexcitability. Certain non-invasive measures of hyperexcitability are correlated with survival outcomes, however it remains uncertain how to define and measure clinically relevant hyperexcitability serially over time. The extent of resection, timing of pre-operative and/or post-operative seizures, and the likelihood of tumor progression are critical factors impacting the risk of seizure recurrence. Newer anti-seizure medications are generally well-tolerated with similar efficacy in this population, and several rapid-onset seizure rescue agents are in development and available.
Summary
Seizures in patients with brain tumors are strongly influenced by the underlying tumor biology and treatment. An improved understanding of the interactions between tumor cells and the spectrum of hyperexcitability will facilitate targeted therapies. Multidisciplinary management of seizures should occur with consideration of tumor-directed therapy and prognosis, and anti-seizure medication decision-making tailored to the individual priorities and quality of life of the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain-tumor related epilepsy (BTRE) is a heterogenous syndrome associated with primary and metastatic brain tumors, accounting for 6–10% of all cases of epilepsy [1], with an average annual age-adjusted incidence rate of 24.71 per 100,000 [2]. Due to the variability in incidence, timing, mechanisms, and clinical risk factors for seizures across different brain tumor pathologies, evidence-based management is challenging and consensus guidelines often extrapolate data from non-tumor epilepsy syndromes. However, when considering seizures in the context of the natural course of disease of the underlying brain tumor, the management of BTRE does not necessarily involve a one-size-fits-all strategy and instead requires an individualized patient-centered approach to optimize quality of life (QoL). This approach is supported by recent translational mechanistic data indicating a dynamic and bidirectional relationship between hyperexcitability and diffuse gliomas [3, 4], such that seizures are increasingly considered as a biomarker of tumor response rather than a passive consequence [5]. Here, we will review these recent mechanistic clinical-translational findings, considerations for implementing seizure activity as a tumor biomarker, a framework for epilepsy phenotyping in the context of the natural course of disease, and recent advances to facilitate patient-centered seizure management strategies.
Emerging Interactions Between Tumor Biology and Epileptogenesis
Recent preclinical studies in animal glioma models have transformed our mechanistic understanding of BTRE. While non-synaptic glutamate release and altered ion homeostasis in the peritumoral microenvironment facilitate neuronal excitability [6,7,8], it is now established that glioma cells integrate with peritumoral neurons through the development of functional neuron-glioma glutamatergic synapses, and that increased neuronal hyperactivity and functional connectivity drives glioma cell proliferation [3, 4, 9]. Neuronal-derived neuroligin-3 (NLGN3) is secreted and leads to PI3K-mTOR pathway activation and mTOR-dependent feedforward NLGN3 upregulation in glioma cells [10].
Variability in BTRE rates both within and between tumor pathologic subtypes suggest the presence of intrinsic tumor characteristics that modify seizure risk. The most established genetic predictor of glioma-related epilepsy is the IDH mutation, which is strongly associated with pre-operative seizures and in the 2021 WHO CNS tumor classification differentiates oligodendroglioma and astrocytoma from IDH-wildtype glioblastoma [11]. IDH1/2 mutations result in the production of 2-hydroxyglutarate (2-HG), which may serve as an analog of glutamate in excitatory synaptic activation [12], as well as leading to mTOR-dependent metabolic reprogramming [13]. Compared to pre-operative clinical seizures, IDH mutations are not strongly associated with persistent excessive electrographic hyperexcitability or post-operative clinical seizures [14,15,16]. Indeed, about 70% of patients with IDH-mutated glioma-related epilepsy are seizure-free after resection [17, 18].
Somatic mutations in other cancer genes, many of which are involved in PI3K/mTOR and MAPK pathway signaling, have been implicated in glioma peritumoral synaptogenesis [19], electrophysiologic hyperexcitability [14, 19, 20], and the clinical response to anti-seizure medications (ASM) [21]. A prime example of targeting genetically-mediated mTOR pathway dysregulation for BTRE is the superior response of subependymal giant-cell astrocytoma and seizure control in patients with tuberous sclerosis with the use of the mTOR inhibitor everolimus [22, 23]. Additional pre-clinical studies indicate the potential for novel targeted therapeutic strategies in diffuse gliomas by inhibiting excessive mTOR pathway activation [24, 25].
In summary, instead of seizures occurring as a passive consequence of cortical injury by tumor mass lesions, these recent findings indicate a dynamic bidirectional relationship between glioma growth and hyperexcitability. Similar mechanisms in non-glial primary brain tumors and metastatic tumors remain to be determined, however tumor genetic variation is a likely contributor to epileptogenic potential [26, 27]. Finally, there is much we do not understand about how peritumoral hyperexcitability affects adjacent brain networks to impact cognitive functioning independent of seizures [28], although recent data suggest that glioblastoma cells integrate into adjacent functionally connected language circuits through secretion of synaptogenic factors and result in remodeling of task-related neural activation [9].
Implementing Seizure Activity as a Tumor Biomarker in Clinical Practice
The shared mechanistic pathways underlying gliomagenesis and epileptogenesis align with clinical observations of seizure frequency correlating with tumor progression and improving with anti-tumor treatments [29, 30]. As such, peritumoral hyperexcitability and clinical seizures may serve as biomarkers of tumor status [5]. In practice, the development of new seizures or a significant increase in seizure frequency from baseline should prompt expedited neuroimaging for tumor surveillance. In patients with worsening seizures on their current ASM regimen associated with recurrent/progressive disease, it may even be reasonable to observe the seizure response to a change in tumor treatment rather than starting additional ASM and increasing the risk of adverse effects from polytherapy. For example, treatment with bevacizumab for the first recurrence of glioblastoma is associated with improved seizure control compared to treatment without a bevacizumab-containing regimen [31]. Under this framework, ASM decision-making should take into account the tumor natural history and planned tumor treatments to optimize the balance among seizure control, medication burden, and adverse effects.
There are several current limitations and knowledge gaps in implementing seizure activity as a tumor biomarker. Self-reporting of clinical seizure counts is highly variable by seizure type and overall unreliable, in part due to the considerable rate of unrecognized events with impaired awareness or occurring during sleep [32]. Furthermore, it is expected that synaptic changes and hyperexcitability at the molecular scale precede the development of clinical seizure activity, such that a non-invasive measurement of peritumoral neuronal activity would be desired. This raises the questions of what defines clinically relevant hyperexcitability and how best to measure it. The problem is magnified by variability in definitions and methodologies used across studies to investigate hyperexcitability, ranging from the scale of individual neuronal firing to broad field potentials and network metrics.
Non-invasive measurements of field potential oscillations by scalp electroencephalography (EEG) and magnetoencephalography (MEG) are clinically available and amenable to serial measurements over time, although there is little data on longitudinal measurements over the natural course of disease [33]. In patients with newly diagnosed IDH-wildtype glioma, early clinical EEG hyperexcitability defined by lateralized periodic discharges and/or electrographic seizures within 1 month of resection and prior to chemoradiation is independently associated with shorter overall survival [34]. Post-operative MEG broadband oscillatory activity is increased in the peritumoral region and higher broadband power is associated with increased NLGN3 expression and shorter survival in patients with diffuse glioma [35,36,37]. These reports indicate the relevance of non-invasive electrophysiologic measurements to tumor outcomes, however standardized longitudinal assessments and definitions are necessary to validate and implement a hyperexcitability biomarker.
Roles for EEG in Brain Tumor-Related Epilepsy
Since the use of EEG in patients with brain tumors is currently limited to the evaluation of clinical seizures, analyses of existing EEG data from neuro-oncology cohorts are inherently biased by the clinical indication, institutional practices in the use of EEG, and the type of studies performed. In the United States, EEG is performed in both inpatient and outpatient settings, with durations ranging from 20 min to multi-day long-term monitoring or ambulatory recordings. The clinical indications for EEG in the management of BTRE include confirmation of a diagnosis of epilepsy, characterization of seizure type and localization, evaluation for subclinical seizure burden, guidance for real-time ASM adjustments, and to stratify risk of ASM tapering versus continuation.
The diagnosis of BTRE typically does not require confirmation with EEG, however it may be helpful in situations where there is diagnostic uncertainty. These often occur when patients present with atypical and non-specific spells, in situations where neurologic symptoms are difficult to differentiate from those caused by the tumor itself or adverse effects of treatment, as well as in cases with cognitive complaints wherein subclinical seizures are suspected. It is also important to recognize the potential for comorbid epilepsy and non-epileptic spells. For example, in a recent small series of patients with BTRE, comorbid non-epileptic spells developed subsequent to epileptic seizures in all cases and within 1 month of their tumor diagnosis in about half of patients [38]. Patients with brain tumors may also be susceptible to seizure activity in the setting of critical illness. In a single center cohort of all cancer patients admitted to the ICU and undergoing either routine or continuous EEG, 27% had seizures, with an increased risk of clinical and/or electrographic seizures in patients with brain metastases and increased risk of electrographic seizures in patients with primary brain tumors [39].
Continuous EEG monitoring, both as inpatient long-term monitoring and as outpatient ambulatory recordings, are increasingly available in the United States, in part due to the rise of commercial EEG monitoring services that provide in-home EEG technologist support. Continuous EEG increases the yield for detection of electrographic seizures compared to routine EEG in patients with BTRE and has been used to develop a measure of hyperexcitability in patients with glioma-related epilepsy [14, 34, 39]. In a cohort of patients with grades 1–4 glioma who underwent inpatient continuous EEG pre-operatively and/or post-operatively, hyperexcitability defined by lateralized periodic discharges and/or electrographic seizures was associated with clinical seizure control, supporting the notion that hyperexcitability may be an enduring property of certain gliomas [14]. In practice, ASMs are often escalated for these EEG findings, however there is limited evidence that treatment improves long-term seizure or tumor outcomes [34, 40]. Hence, in patients with BTRE, the benefits of aggressive treatment of highly epileptiform patterns seen on continuous EEG without clinical correlate should be weighed against potential adverse effects of escalation of ASMs.
Variable Phenotypes of Tumor-Related Seizures and Epilepsy
The impact of the initial resective surgery on seizure outcomes cannot be overstated. In addition to obtaining adequate tissue for pathologic diagnosis and targeted tumor therapy, the presence of gross total resection has consistently been demonstrated as a strong predictor of post-operative seizure freedom. Since seizures are often the first sign leading to discovery of a brain tumor and followed soon after by resective surgery, it is a common scenario to have a single isolated pre-operative seizure. ASM is indicated in all cases, however the post-operative epilepsy prognosis and optimal duration of ASM treatment is highly variable. In the latest International League Against Epilepsy (ILAE) criteria [41], epilepsy is defined by the presence of seizure(s) and at least 60% risk of recurrence over the next 10 years. While the natural course of unresected or incompletely resected tumors pose a high risk of seizure recurrence, seizure outcomes reported after gross total resection for many tumor pathologies indicate recurrence risks well below this 60% threshold. In an analysis of the multicenter European Epilepsy Brain Bank consortium, 76% of patients with low grade neuroepithelial tumors were seizure-free at 5 years and 47% had completely discontinued ASMs, while in patients with other brain tumor pathologies 68% were seizure-free and 33% were off all ASMs at 5 years [42].
We consider the extent of resection, timing of pre-operative and/or post-operative seizures, and the likelihood of tumor progression or recurrence to be among the most relevant factors in counseling patients on the risks of seizure recurrence to guide ASM decision-making (Table 1). In patients with exclusively post-operative seizures and gross total resection, the distinction between early and late seizures after craniotomy may also impact seizure recurrence risk, with early seizures occurring less than 1–2 weeks post-operatively representing acute symptomatic seizures and a lower risk of recurrence [43, 44]. Malignant brain tumors with high rates of progression or recurrence are typically managed with radiation and/or chemotherapy; our practice is to continue ASM for the duration of tumor treatment and over some period of observation for tumor stability afterwards. Newer generation targeted therapies for brain metastases (e.g. the tyrosine kinase inhibitors, osimertinib and lorlatinib) and diffuse gliomas (e.g. the IDH inhibitor, vorasidenib) have demonstrated promising results, although their impact on tumor-related epilepsy and concurrent ASM treatment is uncertain.
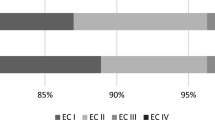
A subset of patients with BTRE, including IDH-mutated and IDH-wildtype diffuse gliomas, have evidence of persistent severe electrographic hyperexcitability on the ictal-interictal continuum and/or drug-resistant epilepsy [14]. These patients typically require multiple ASMs and frequent use of benzodiazepine seizure rescue medications. Since sustained seizure-freedom may be challenging to achieve in drug-resistant epilepsy, it is critical to determine patient-specific priorities and the extent to which seizures are disabling or bothersome to the individual and family. This will allow for a patient-centered seizure management plan that optimizes QoL by balancing the individual’s priorities regarding seizure control, seizure-related activity restrictions or disability, and ASM adverse effects (Fig. 1). For example, an increased frequency of non-disabling focal aware seizures on two ASMs may be preferred to fewer seizures with excessive daytime fatigue on three ASMs.
Anti-Seizure Medication Selection
With the exception of certain epilepsy syndromes, there is limited evidence to support the superiority of one ASM over another [45]. The choice of ASM in BTRE requires many considerations similar to other etiologies of epilepsy; decision-making is largely based on a balance of known efficacy, side effect profile, and drug-drug interactions. There are additional nuances in BTRE, particularly early in the course of disease around the time of craniotomy, in which tumor-related neurologic dysfunction, post-surgical recovery, varying or tapering corticosteroid doses, and mood symptoms secondary to the new diagnosis of a serious medical condition all impact ASM tolerability. After the initial diagnosis, it is critical to minimize potential interactions of ASMs with current or future anti-tumor therapy, as well as avoiding agents that may affect clinical trial eligibility.
There are few randomized controlled trials (RCTs) examining the efficacy of specific ASMs for BTRE. Most studies are retrospective or observational, often limited by heterogenous inclusion criteria (particularly regarding tumor pathology and tumor-specific treatment), small numbers of patients, variable follow-up times, and incomplete epilepsy phenotyping [46]. Here we will focus on the most recently developed ASMs that are increasingly used for the treatment of BTRE in the United States (Table 2). These newer generation ASMs are typically trialed as second-line agents after failure of first-line levetiracetam, and in combination with or in place of lamotrigine, oxcarbazepine, or valproic acid [29].
Levetiracetam is the standard of care first-line treatment for BTRE – in a survey of 198 neuro-oncologists, 90% reported levetiracetam as choice for first-line of treatment, citing efficacy and fewer adverse effects as the reasons for their choice [47]. A small RCT comparing levetiracetam to phenytoin for prevention of post-operative glioma-related seizures reported similar rates of seizure-freedom over 6 month follow-up, with fewer adverse effects from levetiracetam [48]. Another small RCT comparing levetiracetam to pregabalin in patients with primary brain tumors found similar rates of seizure control and tolerability [49]. Across non-controlled studies in glioma-related epilepsy, levetiracetam as monotherapy has demonstrated seizure-freedom rates of 39–96% and > 50% seizure reduction rates of 71–100%.46
Lacosamide is a newer generation ASM frequently used for BTRE as monotherapy or in combination with levetiracetam. Its mechanism of action involves enhancing the slow inactivation of voltage-gated sodium channels. A multicenter retrospective study that included brain tumor patients with heterogenous histopathology showed seizure-freedom rates of 55% at 6 months following lacosamide monotherapy, with no significant differences in efficacy among different histological subtypes [50]. A multicenter, retrospective study of 139 patients with seizures in the setting of grade 2–4 diffuse glioma showed similar efficacy of lamotrigine and lacosamide after failure of first-line levetiracetam or valproic acid, with a cumulative incidence of treatment failure of 38% vs. 30% at 12 months, respectively [51]. As prophylactic therapy, a RCT of lacosamide in patients with newly diagnosed high-grade glioma without prior seizures was terminated early after enrollment of 37 patients, in which 0/18 (0%) patients randomized to lacosamide and 1/19 (5.3%) patients randomized to placebo had seizures during follow-up (NCT01432171).
Other more recently developed ASMs evaluated for efficacy and tolerability in BTRE include brivaracetam, clobazam, and perampanel. Brivaracetam is an analog of levetiracetam with greater binding affinity to the synaptic vesicle protein 2A (SV2A) target. A retrospective multicenter study of 33 patients with brain tumors of heterogenous pathologies reported seizure freedom in 60% at mean follow-up of 10 months with brivaracetam as add-on therapy or as replacement of levetiracetam in monotherapy [52]. A similar study of 33 patients with BTRE treated with clobazam, a long-acting GABA-A receptor agonist, reported seizure freedom in 30% of patients and > 50% seizure reduction in 94% at six months [53]. In an observational study of 21 patients with drug-resistant BTRE, adjunctive treatment with perampanel, a selective glutamatergic AMPA-R antagonist, achieved a seizure-freedom rate of 33% and > 50% seizure reduction in 90% at 12 months [54].
ASMs with strong hepatic cytochrome P450 (CYP) induction effects are generally avoided in BTRE due to the potential for drug-drug interactions and decreased efficacy of chemotherapy, corticosteroids, and targeted therapies [29, 55]. Table 3 summarizes common ASMs and their hepatic CYP induction effects. Most newer generation ASMs are negligible or weak CYP inducers, with the exception of cenobamate, a novel ASM that has shown improved efficacy as adjunctive therapy in drug-resistant epilepsy, but has clinically significant CYP induction effects in a dose-dependent manner [56]. Outcomes of cenobamate specifically in BTRE remain unclear, however in our experience adjunctive treatment in patients with drug-resistant glioma-related epilepsy has generally led to improved seizure frequency with dose-dependent fatigue necessitating reduction of other medications.
Additional factors that influence the choice of ASMs include comorbidities and idiosyncratic side effect profiles. The use of ASMs with potential adverse mood effects, such as levetiracetam and perampanel should generally be avoided in patients with active mood symptoms, in favor of agents with mood stabilizing effects such as lamotrigine or oxcarbazepine. The use of valproic acid, topiramate, or zonisamide may be helpful for treatment of comorbid migraines. Topiramate and zonisamide also may promote mild to moderate weight loss in patients with obesity. Fatigue is the most common adverse effect across ASMs and oversedation may be significant enough to impair daily activities or limit participation in rehab. Similar to non-tumor epilepsy, in our experience lamotrigine is the least sedating ASM and among the best tolerated overall as either monotherapy or in combination with other agents. Use of once daily dosing of ASMs with long half-lives (e.g., lamotrigine, zonisamide, perampanel) may also improve daytime fatigue while facilitating adherence and decreasing pill burden.
Management of Drug-Resistant Brain Tumor-Related Epilepsy
In patients with uncontrolled seizures despite trials of multiple ASMs as monotherapy or in combination, a common priority for patients and families is to avoid seizure-related hospitalizations. While most seizures are isolated and stop spontaneously, some patients are at risk of acute repetitive seizures, seizure clustering, or status epilepticus. In this context, the use of seizure rescue medications at home may aid in preventing prolonged seizures or recurrent clustering, seizure-related injury and complications, and avoid the need for escalation of medical care.
Recent advances in seizure rescue medications include benzodiazepines with intranasal drug delivery, which are preferred due to faster onset of action and ease of administration. Presently, intranasal midazolam and diazepam formulations are the only FDA-approved therapies for seizure clustering other than rectal diazepam. Oral benzodiazepines are commonly used for seizure rescue but are limited by variable absorption and difficulty with administration in cases of seizures with face motor involvement, impaired awareness, or convulsions. Additionally, a novel formulation of inhaled alprazolam is currently in Phase 3 trials (Table 4). The dosing strategies for these medications can be highly individualized based on specific seizure types and patterns. In patients with a history of isolated prolonged seizures or status epilepticus, administration may be considered as soon as possible after seizure onset, whereas for other patients rescue medication may be administered after a second or third seizure within a specified time period.
As in non-tumor epilepsy, surgical intervention should be considered for patients with disabling seizures refractory to ASMs. Resection with or without intra-operative electrocorticography is most commonly employed [29], although in some cases long-term intracranial EEG monitoring may be employed to elucidate areas of seizure onset and early spread, and facilitate functional mapping of motor, sensory, and language cortex. In a series of patients with primary brain tumors undergoing intracranial EEG, the seizure onset zone extended > 1.5 cm from the radiologic tumor margin in 91% of cases [60]. Recently, laser interstitial thermal therapy (LITT) has been increasingly used for the surgical treatment of both brain tumors and focal epilepsy, and the technique advanced to allow awake minimally-invasive ablation with continuous neuropsychologic testing to preserve neurologic function [61]. In patients who are not good candidates for resective/ablative interventions, neuromodulation with the use of chronically implanted stimulators may be considered on a case by case basis. Novel strategies for placement of the internal pulse generator [62], increased compatibility with MRI scanners, and advances in non-invasive stimulation technology will likely expand eligibility for neuromodulation in patients with brain tumors.
Anti-Seizure Medication Tapering and Discontinuation
As described earlier, the treatment of brain tumors with resection and adjuvant therapies alters the natural course of disease and decreases the risk of recurrent seizures. Therefore, the long-term seizure risk and indication for continued ASM is not constant, and instead is strongly influenced by the individual’s tumor and treatment status (Table 1). All ASM adjustments should involve shared decision-making between the patient, caregivers, oncologist, and epileptologist. While certain factors may be predictive of seizure-freedom, there is a notable lack of equipoise amongst clinicians regarding ASM tapering and withdrawal, and in one series the clinicians’ decision to continue post-operative ASMs was the strongest independent predictor of post-operative seizures in multivariate analysis [63]. Prolonged treatment (> 2 years) is often encouraged due to clinicians’ goals of minimizing seizures, however in practice patients may also have strong preferences to trial earlier tapering of ASMs as a result of cost, fatigue, mood and cognitive changes, and pill burden. In contrast, the potential risk of losing driving privileges is a common motivation to remain on ASM. Thus, discussions should weigh the patient-specific risks of continuing ASMs against the risk of seizure-related disability from both physician and patient perspectives.
In a prospective trial of shared decision-making for ASM withdrawal in patients with low-grade gliomas on observation and at least 1 year seizure-free, 65% elected to pursue ASM withdrawal, of whom 26% had seizure recurrence (more than half in the setting of tumor progression), compared to 8% in patients with ASM continuation [64]. The optimal timing of ASM tapering is unclear, with wide variability in practices. In a retrospective observational study of 109 glioma patients, the risk of seizure recurrence over 3-year follow-up was similar between patients who were seizure-free at the time of ASM withdrawal for 3–12 months, 12–24 months, and > 24 months, with less than half in each group experiencing recurrent seizures [65]. We typically continue ASMs while on active tumor treatment and consider ASM tapering after 6–24 months of seizure freedom, with a bias towards longer or indefinite therapy in patients with subtotal resection or post-operative seizures.
Potential Anti-Tumor Effects of Anti-Seizure Medications
Given the recent preclinical evidence for a bidirectional relationship between gliomagenesis and epileptogenesis, there is renewed interest in determining whether certain ASMs may be more effective than others at targeting glioma-related hyperexcitability and improving oncologic outcomes. The current and historical first-line ASMs for BTRE (i.e., levetiracetam and valproic acid, respectively) were evaluated in a pooled analysis of contemporary clinical trials for newly-diagnosed glioblastoma, and neither initial nor maintenance exposure were associated with survival outcomes [66].
The increased glutamate signaling in the glioma microenvironment and formation of glutamatergic AMPA-R neuron-glioma synapses has made the FDA-approved AMPA-R antagonist, perampanel, an attractive target of investigation, although there are few clinical studies to date. In a surgical window-of-opportunity trial of patients with newly-diagnosed high-grade glioma with or without seizures, perampanel given as a pre-operative load and levetiracetam administered per standard of care demonstrated similar rates of peritumoral high gamma oscillations by intraoperative electrocorticography [40]. In a small series of patients with drug-resistant glioma-related epilepsy treated with perampanel, a reduction in tumor size was observed within 6 months in 8/9 patients, although nearly all were also on active treatment with chemotherapy or recently completed radiation therapy [67]. Additionally, a prior RCT of the perampanel analog, talampanel, in patients with recurrent high-grade glioma demonstrated no impact on overall survival [68] and a phase 2 trial of talampanel in newly diagnosed glioblastoma was inconclusive [69].
Future Directions for Targeted Therapy
The current approach to the management of BTRE involves the treatment of clinical seizures with ASMs designed to raise the seizure threshold and decrease the chance of recurrent events. The development of targeted therapies will likely require a shift from intervening on ictogenesis (i.e. the transition from interictal to seizure state) to the prevention of epileptogenesis. This type of proactive strategy necessitates a more advanced understanding of the genetic and molecular profiles of the tumor microenvironment, and improved hyperexcitability biomarkers predictive of both clinical seizures and tumor aggressiveness. Due to the potential shared mechanisms between tumorigenesis and epileptogenesis, treatments targeting tumor driver mutations and pathways may also be effective in blocking hyperexcitability.
Conclusion
BTRE is a heterogenous and dynamic syndrome that is closely associated with the underlying tumor pathology. An improved understanding of the interactions between tumor cells and the spectrum of hyperexcitability in genetically diverse tumor microenvironments will facilitate targeted therapies. Multidisciplinary management of seizures should occur in the context of tumor-directed therapy and the tumor status, with the aggressiveness and choice of ASM treatment tailored to the individual priorities of the patient and their QoL.
Data Availability
No datasets were generated or analysed during the current study.
References
Maschio M, Sperati F, Dinapoli L, et al. Weight of epilepsy in brain tumor patients. J Neurooncol. 2014;118(2):385–93. https://doi.org/10.1007/s11060-014-1449-7.
Ostrom QT, Price M, Neff C, et al. CBTRUS Statistical Report: primary brain and other Central Nervous System tumors diagnosed in the United States in 2015–2019. Neuro-Oncol. 2022;24(Suppl 5):v1–95. https://doi.org/10.1093/neuonc/noac202.
Venkataramani V, Tanev DI, Strahle C, et al. Glutamatergic synaptic input to glioma cells drives brain tumour progression. Nature. 2019;573(7775):532–8. https://doi.org/10.1038/s41586-019-1564-x.
Venkatesh HS, Morishita W, Geraghty AC, et al. Electrical and synaptic integration of glioma into neural circuits. Nature. 2019;573(7775):539–45. https://doi.org/10.1038/s41586-019-1563-y.
Avila EK, Chamberlain M, Schiff D, et al. Seizure control as a new metric in assessing efficacy of tumor treatment in low-grade glioma trials. Neuro-Oncol. 2017;19(1):12–21. https://doi.org/10.1093/neuonc/now190.
Buckingham SC, Campbell SL, Haas BR, et al. Glutamate release by primary brain tumors induces epileptic activity. Nat Med. 2011;17(10):1269–74. https://doi.org/10.1038/nm.2453.
Pallud J, Le Van Quyen M, Bielle F, et al. Cortical GABAergic excitation contributes to epileptic activities around human glioma. Sci Transl Med. 2014;6(244):244ra89. https://doi.org/10.1126/scitranslmed.3008065.
Curry RN, Aiba I, Meyer J, et al. Glioma epileptiform activity and progression are driven by IGSF3-mediated potassium dysregulation. Neuron. 2023;111(5):682–e6959. https://doi.org/10.1016/j.neuron.2023.01.013.
Krishna S, Choudhury A, Keough MB et al. Glioblastoma remodelling of human neural circuits decreases survival. Nature. 2023;617(7961):599–607. https://doi.org/10.1038/s41586-023-06036-1 (This study demonstrated that glioblastoma cells functionally integrate into language circuits contributing to task-relevant neural activity and high-gamma hyperexcitability in tumor infiltrated regions. Tumor cells in areas with high alpha-band connectivity were found to secrete synaptogenic factors, and greater connectivity was associated with decreased survival).
Venkatesh HS, Johung TB, Caretti V, et al. Neuronal activity promotes Glioma Growth through Neuroligin-3 secretion. Cell. 2015;161(4):803–16. https://doi.org/10.1016/j.cell.2015.04.012.
Louis DN, Perry A, Wesseling P, et al. The 2021 WHO classification of tumors of the Central Nervous System: a summary. Neuro-Oncol. 2021;23(8):1231–51. https://doi.org/10.1093/neuonc/noab106.
Chen H, Judkins J, Thomas C, et al. Mutant IDH1 and seizures in patients with glioma. Neurology. 2017;88(19):1805–13. https://doi.org/10.1212/WNL.0000000000003911.
Mortazavi A, Fayed F, Bachani M, et al. IDH-mutated gliomas promote epileptogenesis through d-2-hydroxyglutarate-dependent mTOR hyperactivation. Neuro-Oncol. 2022;24(9):1423–35. https://doi.org/10.1093/neuonc/noac003 (Using in vitro neuron-glioma cultures with microelectrode arrays, this study found that d-2-HG promotes hyperexcitability through a metabolic shift involving upregulation of lactate dehydrogenase A expression in an mTOR-dependent manner).
Tobochnik S, Dorotan MKC, Ghosh HS et al. Glioma genetic profiles associated with electrophysiologic hyperexcitability. Neuro-Oncol. 2024;26(2):323–334. https://doi.org/10.1093/neuonc/noad176 (In this glioma cohort, targeted exome sequencing of cancer genes revealed selective somatic mutations that were over-represented in patients with continuous EEG hyperexcitability, defined by lateralized periodic discharges and/or electrographic seizures, and independent of integrated pathologic diagnosis (including IDH mutations).
Jo J, Nevel K, Sutyla R, Smolkin M, Lopes MB, Schiff D. Predictors of early, recurrent, and intractable seizures in low-grade glioma. Neuro-Oncol Pract. 2021;8(1):40–7. https://doi.org/10.1093/nop/npaa054.
Song L, Quan X, Chen C, Chen L, Zhou J. Correlation between tumor molecular markers and Perioperative Epilepsy in patients with glioma: a systematic review and Meta-analysis. Front Neurol. 2021;12:692751. https://doi.org/10.3389/fneur.2021.692751.
Englot DJ, Berger MS, Barbaro NM, Chang EF. Predictors of seizure freedom after resection of supratentorial low-grade gliomas: a review. J Neurosurg. 2011;115(2):240–4. https://doi.org/10.3171/2011.3.JNS1153.
Ius T, Pauletto G, Tomasino B, et al. Predictors of postoperative seizure outcome in low Grade Glioma: from volumetric analysis to Molecular Stratification. Cancers. 2020;12(2):397. https://doi.org/10.3390/cancers12020397.
Yu K, Lin CCJ, Hatcher A et al. PIK3CA variants selectively initiate brain hyperactivity during gliomagenesis. Nature. 2020;578(7793):166–171. https://doi.org/10.1038/s41586-020-1952-2 (This study evaluated the effect of PIK3CA driver mutations on epileptogenicity in a mouse glioblastoma model, demonstrating that certain gain-of-function somatic mutations promote excitatory-inhibitory synaptic imbalance, and indicating the relevance of the tumor genetic profile to hyperexcitability and seizure risk).
Cases-Cunillera S, van Loo KMJ, Pitsch J, et al. Heterogeneity and excitability of BRAFV600E-induced tumors is determined by Akt/mTOR-signaling state and Trp53-loss. Neuro-Oncol. 2022;24(5):741–54. https://doi.org/10.1093/neuonc/noab268.
Tobochnik S, Pisano W, Lapinskas E, Ligon KL, Lee JW. Effect of PIK3CA variants on glioma-related epilepsy and response to treatment. Epilepsy Res. 2021;175:106681. https://doi.org/10.1016/j.eplepsyres.2021.106681.
Krueger Darcy A, Care Marguerite M, Katherine H, et al. Everolimus for Subependymal Giant-Cell Astrocytomas in Tuberous Sclerosis. N Engl J Med. 2010;363(19):1801–11. https://doi.org/10.1056/NEJMoa1001671.
French JA, Lawson JA, Yapici Z, et al. Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study. Lancet. 2016;388(10056):2153–63. https://doi.org/10.1016/S0140-6736(16)31419-2.
Goldberg AR, Dovas A, Torres D, et al. Glioma-Induced alterations in excitatory neurons are reversed by mTOR inhibition. BioRxiv Prepr Serv Biol. (Published Online January 2024);2024.01.10.575092.
Roy A, Skibo J, Kalume F et al. Mouse models of human PIK3CA-related brain overgrowth have acutely treatable epilepsy. In: Morrison SJ, ed. ELife. 2015;4:e12703. https://doi.org/10.7554/eLife.12703.
Gupte TP, Li C, Jin L, et al. Clinical and genomic factors associated with seizures in meningiomas. J Neurosurg Published Online Dec. 2020;4:1–10. https://doi.org/10.3171/2020.7.JNS201042.
Koh HY, Kim SH, Jang J, et al. BRAF somatic mutation contributes to intrinsic epileptogenicity in pediatric brain tumors. Nat Med. 2018;24(11):1662–8. https://doi.org/10.1038/s41591-018-0172-x.
Maas DA, Douw L. Multiscale network neuroscience in neuro-oncology: how tumors, brain networks, and behavior connect across scales. Neuro-Oncol Pract. 2023;10(6):506–17. https://doi.org/10.1093/nop/npad044.
Avila EK, Tobochnik S, Inati SK, et al. Brain tumor-related epilepsy management: a Society for Neuro-oncology (SNO) consensus review on current management. Neuro-Oncol. 2024;26(1):7–24. https://doi.org/10.1093/neuonc/noad154.
Bruno F, Pellerino A, Conti Nibali M, et al. Association of Clinical, Tumor, and treatment characteristics with seizure control in patients with IDH1/2-Mutant Lower-Grade Glioma. Neurology. 2024;102(10):e209352. https://doi.org/10.1212/WNL.0000000000209352.
Hertler C, Seystahl K, Le Rhun E, et al. Improved seizure control in patients with recurrent glioblastoma treated with bevacizumab. Neuro-Oncol. 2022;24(11):2001–4. https://doi.org/10.1093/neuonc/noac172.
Hoppe C, Poepel A, Elger CE. Epilepsy: accuracy of patient seizure counts. Arch Neurol. 2007;64(11):1595–9. https://doi.org/10.1001/archneur.64.11.1595.
Montgomery MK, Kim SH, Dovas A, et al. Glioma-Induced alterations in neuronal activity and neurovascular coupling during Disease Progression. Cell Rep. 2020;31(2):107500. https://doi.org/10.1016/j.celrep.2020.03.064.
Tobochnik S, Lapinskas E, Vogelzang J, Ligon KL, Lee JW. Early EEG hyperexcitability is associated with decreased survival in newly diagnosed IDH-wildtype glioma. J Neurooncol. 2022;159(1):211–8. https://doi.org/10.1007/s11060-022-04059-8.
Belgers V, Numan T, Kulik SD, et al. Postoperative oscillatory brain activity as an add-on prognostic marker in diffuse glioma. J Neurooncol. 2020;147(1):49–58. https://doi.org/10.1007/s11060-019-03386-7.
Numan T, Kulik SD, Moraal B, et al. Non-invasively measured brain activity and radiological progression in diffuse glioma. Sci Rep. 2021;11(1):18990. https://doi.org/10.1038/s41598-021-97818-y.
Derks J, Wesseling P, Carbo EWS, et al. Oscillatory brain activity associates with neuroligin-3 expression and predicts progression free survival in patients with diffuse glioma. J Neurooncol. 2018;140(2):403–12. https://doi.org/10.1007/s11060-018-2967-5.
Sumangala S, Liang D, Samarasekera S. Nonepileptic attacks in patients with brain tumor-related epilepsy. Epilepsy Behav EB. 2022;129:108656. https://doi.org/10.1016/j.yebeh.2022.108656.
Azary S, Caravanos C, Reiner AS, Panageas KS, Dhawan V, Avila EK. Incidence of Seizure and Associated Risk factors in patients in the Medical Intensive Care Unit (ICU) at Memorial Sloan Kettering Cancer Center (MSK) from 2016–2017. J Intensive Care Med. 2022;37(10):1312–7. https://doi.org/10.1177/08850666211066080.
Tobochnik S, Regan MS, Dorotan MKC et al. Pilot trial of perampanel on peritumoral hyperexcitability and clinical outcomes in newly diagnosed high-grade glioma. medRxiv. Published online April 18, 2024:2024.04.11.24305666. https://doi.org/10.1101/2024.04.11.24305666.
Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–82. https://doi.org/10.1111/epi.12550.
Lamberink HJ, Otte WM, Blümcke I, et al. Seizure outcome and use of antiepileptic drugs after epilepsy surgery according to histopathological diagnosis: a retrospective multicentre cohort study. Lancet Neurol. 2020;19(9):748–57. https://doi.org/10.1016/S1474-4422(20)30220-9.
Horiuchi S, Kanaya K, Horiuchi T. The occurrence and relationship of postoperative seizure and de novo Epilepsy after Craniotomy surgery: a retrospective single-Center Cohort Study. Front Surg. 2022;9:881874. https://doi.org/10.3389/fsurg.2022.881874.
Mauritz M, Hirsch LJ, Camfield P, et al. Acute symptomatic seizures: an educational, evidence-based review. Epileptic Disord. 2022;24(1):26–49. https://doi.org/10.1684/epd.2021.1376.
Perucca E, Brodie MJ, Kwan P, Tomson T. 30 years of second-generation antiseizure medications: impact and future perspectives. Lancet Neurol. 2020;19(6):544–56. https://doi.org/10.1016/S1474-4422(20)30035-1.
de Bruin ME, van der Meer PB, Dirven L, Taphoorn MJB, Koekkoek JAF. Efficacy of antiepileptic drugs in glioma patients with epilepsy: a systematic review. Neuro-Oncol Pract. 2021;8(5):501–17. https://doi.org/10.1093/nop/npab030.
van der Meer PB, Dirven L, van den Bent MJ, et al. Prescription preferences of antiepileptic drugs in brain tumor patients: an international survey among EANO members. Neuro-Oncol Pract. 2022;9(2):105–13. https://doi.org/10.1093/nop/npab059.
Lim DA, Tarapore P, Chang E, et al. Safety and feasibility of switching from phenytoin to levetiracetam monotherapy for glioma-related seizure control following craniotomy: a randomized phase II pilot study. J Neurooncol. 2009;93(3):349–54. https://doi.org/10.1007/s11060-008-9781-4.
Rossetti AO, Jeckelmann S, Novy J, Roth P, Weller M, Stupp R. Levetiracetam and Pregabalin for antiepileptic monotherapy in patients with primary brain tumors. A phase II randomized study. Neuro-Oncol. 2014;16(4):584–8. https://doi.org/10.1093/neuonc/not170.
Mo F, Meletti S, Belcastro V, et al. Lacosamide in monotherapy in BTRE (brain tumor-related epilepsy): results from an Italian multicenter retrospective study. J Neurooncol. 2022;157(3):551–9. https://doi.org/10.1007/s11060-022-03998-6.
van Opijnen MP, van der Meer PB, Dirven L, et al. The effectiveness of antiepileptic drug treatment in glioma patients: lamotrigine versus lacosamide. J Neurooncol. 2021;154(1):73–81. https://doi.org/10.1007/s11060-021-03800-z.
Maschio M, Maialetti A, Mocellini C, et al. Effect of Brivaracetam on Efficacy and Tolerability in patients with brain tumor-related Epilepsy: a retrospective Multicenter Study. Front Neurol. 2020;11:813. https://doi.org/10.3389/fneur.2020.00813.
Brahmbhatt N, Stupp R, Bushara O, Bachman E, Schuele SU, Templer JW. Efficacy of clobazam as add-on therapy in brain tumor-related epilepsy. J Neurooncol. 2021;151(2):287–93. https://doi.org/10.1007/s11060-020-03664-9.
Coppola A, Zarabla A, Maialetti A, et al. Perampanel confirms to be effective and well-tolerated as an Add-On treatment in patients with brain tumor-related Epilepsy (PERADET Study). Front Neurol. 2020;11:592. https://doi.org/10.3389/fneur.2020.00592.
Fink KL, Deo AK. Chapter 3 - Antiepileptic drugs and chemotherapy: Potential interactions and impact on treatment of patients with cancer. In: Newton HB, editors. Handbook of Brain Tumor Chemotherapy, Molecular Therapeutics, and Immunotherapy. 2nd ed. Academic Press; 2018:45–58. https://doi.org/10.1016/B978-0-12-812100-9.00003-6.
Greene SA, Kwak C, Kamin M, et al. Effect of cenobamate on the single-dose pharmacokinetics of multiple cytochrome P450 probes using a cocktail approach in healthy subjects. Clin Transl Sci. 2022;15(4):899–911. https://doi.org/10.1111/cts.13204.
French J, Biton V, Dave H, et al. A randomized phase 2b efficacy study in patients with seizure episodes with a predictable pattern using Staccato® alprazolam for rapid seizure termination. Epilepsia. 2023;64(2):374–85. https://doi.org/10.1111/epi.17441.
Lelis IR, Krauss GL. Sublingual lorazepam as rescue therapy for seizure emergencies in adults. Epilepsy Behav EB. 2023;145:109294. https://doi.org/10.1016/j.yebeh.2023.109294.
Penovich PE, Rao VR, Long L, Carrazana E, Rabinowicz AL. Benzodiazepines for the treatment of seizure clusters. CNS Drugs. 2024;38(2):125–40. https://doi.org/10.1007/s40263-023-01060-1.
Mittal S, Barkmeier D, Hua J, et al. Intracranial EEG analysis in tumor-related epilepsy: evidence of distant epileptic abnormalities. Clin Neurophysiol off J Int Fed Clin Neurophysiol. 2016;127(1):238–44. https://doi.org/10.1016/j.clinph.2015.06.028.
Nielsen SH, Skjøth-Rasmussen J, Moldrup SD, Engelmann CM, Jespersen B, Rasmussen R. Awake laser ablation with continuous neuropsychological testing during treatment of Brain tumors and Epilepsy. Neurosurg Clin N Am. 2023;34(2):239–45. https://doi.org/10.1016/j.nec.2022.11.003.
Masri AR, Yekzaman BR, Estes BJ, Park CS, Landazuri P, Kinsman M. Infraclavicular de novo placement of a responsive neurostimulator for a patient with eloquent glioma-associated epilepsy: illustrative case. J Neurosurg Case Lessons. 2023;5(26):CASE22528. https://doi.org/10.3171/CASE22528.
Das RR, Artsy E, Hurwitz S, et al. Outcomes after discontinuation of antiepileptic drugs after surgery in patients with low grade brain tumors and meningiomas. J Neurooncol. 2012;107(3):565–70. https://doi.org/10.1007/s11060-011-0779-y.
Kerkhof M, Koekkoek JaF, Vos MJ, et al. Withdrawal of antiepileptic drugs in patients with low grade and anaplastic glioma after long-term seizure freedom: a prospective observational study. J Neurooncol. 2019;142(3):463–70. https://doi.org/10.1007/s11060-019-03117-y.
van der Meer PB, Dirven L, Fiocco M et al. Impact of timing of antiseizure medication withdrawal on seizure recurrence in glioma patients: a retrospective observational study. J Neurooncol. 2023;164(3):545–555. https://doi.org/10.1007/s11060-023-04450-z (In this cohort study of glioma patients who underwent withdrawal of anti-seizure medication, there was no difference in seizure recurrence risk between patients who had short-term (3–12 months), medium-term (12–24 months), or long-term (> 24 months) seizure freedom after tumor-directed therapy).
Happold C, Gorlia T, Chinot O, et al. Does valproic acid or levetiracetam improve survival in glioblastoma? A pooled analysis of prospective clinical trials in newly diagnosed glioblastoma. J Clin Oncol. 2016;34(7):731–9. https://doi.org/10.1200/JCO.2015.63.6563.
Izumoto S, Miyauchi M, Tasaki T, et al. Seizures and Tumor Progression in Glioma patients with Uncontrollable Epilepsy treated with Perampanel. Anticancer Res. 2018;38(7):4361–6. https://doi.org/10.21873/anticanres.12737.
Iwamoto FM, Kreisl TN, Kim L, et al. Phase 2 trial of talampanel, a glutamate receptor inhibitor, for adults with recurrent malignant gliomas. Cancer. 2010;116(7):1776–82. https://doi.org/10.1002/cncr.24957.
Grossman SA, Ye X, Piantadosi S, et al. Survival of patients with newly diagnosed glioblastoma treated with radiation and temozolomide in research studies in the United States. Clin Cancer Res off J Am Assoc Cancer Res. 2010;16(8):2443–9. https://doi.org/10.1158/1078-0432.CCR-09-3106.
Author information
Authors and Affiliations
Contributions
S.T. and M.K.C.D. wrote and edited the main manuscript text and prepared the figure and tables.
Corresponding author
Ethics declarations
S.T. has received non-financial research support from Eisai and has served in consulting roles for Blackrock Neurotech. M.K.C.D. reports no competing interests.
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dorotan, M.K.C., Tobochnik, S. Patient-Centered Management of Brain Tumor-Related Epilepsy. Curr Neurol Neurosci Rep 24, 413–422 (2024). https://doi.org/10.1007/s11910-024-01360-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-024-01360-z