Abstract
Purpose of Review
This review summarizes previous and ongoing neuroprotection trials in multiple system atrophy (MSA), a rare and fatal neurodegenerative disease characterized by parkinsonism, cerebellar, and autonomic dysfunction. It also describes the preclinical therapeutic pipeline and provides some considerations relevant to successfully conducting clinical trials in MSA, i.e., diagnosis, endpoints, and trial design.
Recent Findings
Over 30 compounds have been tested in clinical trials in MSA. While this illustrates a strong treatment pipeline, only two have reached their primary endpoint. Ongoing clinical trials primarily focus on targeting α-synuclein, the neuropathological hallmark of MSA being α-synuclein-bearing glial cytoplasmic inclusions.
Summary
The mostly negative trial outcomes highlight the importance of better understanding underlying disease mechanisms and improving preclinical models. Together with efforts to refine clinical measurement tools, innovative statistical methods, and developments in biomarker research, this will enhance the design of future neuroprotection trials in MSA and the likelihood of positive outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
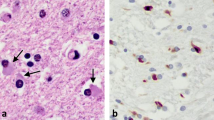
Multiple system atrophy (MSA) is a rare neurodegenerative disease characterized by parkinsonism, cerebellar symptoms, and autonomic dysfunction to various extents [1]. The neuropathological hallmark is the accumulation of alpha-synuclein (aSyn) aggregates in oligodendrocytes known as glial cytoplasmic inclusions (GCIs) but also neuronal deposits in smaller proportions [2]. These histopathological features contributed to the classification of MSA as a synucleinopathy, together with dementia with Lewy bodies (DLB) and Parkinson’s disease (PD). The average survival rate is 6–10 years after symptom onset [1,2,3]. No effective treatment can significantly alleviate symptoms or slow disease progression in MSA. Although the precise relation between aSyn accumulation and neural death is incompletely understood, the aggregation of native aSyn is believed to contribute to numerous cellular dysfunctions in MSA [4, 5]. GCIs correlate with cell loss and regional brain atrophy [6, 7]. GCIs-aSyn strains further differ from those in other synucleinopathies and show distinct seeding patterns [8, 910
This review summarizes previous and ongoing neuroprotection trials in MSA (Fig. 1). It also describes the preclinical therapeutic pipeline and provides some considerations relevant to successfully conducting clinical trials, i.e., diagnosis, endpoints, and trial design.
Diagnosis, Endpoints, and Trial Design
Neuroprotection trials usually rely on patients in the earliest disease stages, while the diagnosis of MSA may be challenging within the first years. The 2008 consensus diagnosis criteria defined two clinical categories, possible and probable MSA [11••]. Their limited sensitivity to detect early-stage patients led to a recent revision [12,13,14]. According to a post-mortem exercise, the revised criteria show improved sensitivity at earlier stages while maintaining high specificity [15•].
The Unified Multiple System Atrophy Rating Scale (UMSARS), introduced in 2004, is the most specific metric for assessing symptom severity and progression [16]. It has been used as the primary endpoint in almost all recent randomized clinical trials, while acknowledged limitations have led to an ongoing revision [17••]. For instance, some UMSARS items imperfectly correlate with disease progression or do not reflect the patient’s perspective [18]. In other words, each item may have a different informative contribution to progression changes. Recent efforts to address this limitation have resulted in the proposal of several abbreviated scales. Based on a 9-item subset, one aimed to provide a more patient-centered approach and demonstrated adequate psychometric properties [19, 20]. Two other versions adopted a data-driven approach; one used the mean standardized difference for each item after 1 year of progression [21], while the other employed an Item Response Theory (IRT) model with measurements taken at multiple time points [22]. IRT allows computing the percentage of information each item carries to explain an underlying construct, for example, disease severity. Thus, IRT could help identify better-suited subsets of items for describing the latent variable. Both approaches mentioned above yielded an 11-item scale despite differences in item selection [21, 22]. Although these initiatives reflect preliminary work, they provide evidence that selecting a subset of UMSARS items is a valuable strategy to reliably detect changes in disease progression.
Additional challenges are the rarity (limiting the number of available patients for enrollment) and the aggressiveness (substantial risk of loss to follow-up due to death) of MSA, demanding adapted statistical planning. While large-scale natural history cohorts have provided significant data on progression rates, these may have inadequately addressed the issue of missing data across longitudinal observations. This could introduce potential biases, particularly as surviving patients may exhibit a slower rate of disease progression. More suited statistical approaches like joint modeling may better estimate patients’ trajectories [23, 24]. In brief, joint models simultaneously analyze the time-varying, longitudinal data (e.g., UMSARS score) and the potentially associated time-to-event (e.g., time-to-death). Along the same line, estimating sample sizes and testing for primary endpoints in clinical trials should consider progression and dropout rates precisely. Classical approaches such as the Student’s t-test only consider the difference between two observed time points (e.g., the change of UMSARS scores over a year), i.e., the same number of observations between the two time points are required. Conversely, linear mixed models (LMM) can exploit additional information (e.g., intermediate UMSARS measures, exact time of the study visit), and handle incomplete follow-up, allowing better precision, which eventually is likely to reduce the necessary sample sizes.
By leveraging data from the French MSA cohort, we compared classical Student versus LMM for sample size determination using UMSARS sum scores based on the item combinations cited above. We extracted from our cohort a population that fulfills the common criteria for inclusion in clinical trials, that is, (1) symptom onset ≤ 4 years at first visit and (2) the absence of severe impairment of speech, swallowing, and walking as markers of advanced disease. Our simulations illustrate that using LMM instead of a Student’s t-test leads to a substantially smaller sample size. In contrast, decreasing the number of UMSARS items leads to higher required sample sizes (Table 1). Finally, the sample size increases with the data-driven subscales [21, 22] are almost negligible.
Finally, to increase diagnosis performance and precision of meaningful endpoints, there is a crucial need to incorporate biological markers reflecting the underlying disease mechanisms. To this extent, neuroimaging features have been added to the revised diagnostic criteria for MSA, and algorithms based on automated categorization may further enhance diagnostic accuracy in the future [25, 26]. More recently, a PET tracer for aSyn showed promising results in detecting specific MSA pathology compared to PD patients [27•]. Similarly, fluid biomarkers hold strong potential to improve diagnostic accuracy. In this line, increasing evidence suggests that aSyn seeding amplification assays allow the distinction between MSA and Lewy body disorders with high precision [9, 28, 29]. Moreover, recent studies have highlighted the potential of additional biomarkers. For instance, neurofilament light chain (NfL) blood and cerebrospinal fluid (CSF) levels may help distinguish MSA from other synucleinopathies and predict disease severity and progression in MSA [30, 31]. These advances will likely improve patient selection and stratification in future clinical trials.
Targeting Alpha-Synuclein
The following sections will highlight the attempts to target aSyn in humans and the preclinical pipeline of potential future compounds. These are summarized in Tables 2 and 3, respectively.
Reduction of Expression
Antisense oligonucleotides (ASO) modulate targeted gene expression [60]. This technology is tested on neurodegenerative diseases, such as amyotrophic lateral sclerosis and Huntington’s disease (HD). For instance, trials assessing ASO in HD failed to provide evidence for efficacy [32, 33]. In addition, a safety warning emerged in a phase 3 trial because of increased cerebrospinal fluid NfL levels and time- and dose-dependent expansion of ventricle volume in treated patients.
ASO targeting the mRNA of the SNCA gene that codes for aSyn reduced endogenous aSyn expression and pathology in several preclinical models of PD [34, 61, 62]. It also restored behavioral and cognitive functions [35, 36] and mitigated neural loss [61,62,63]. In another study using a transgenic mouse model of PD, the reduction of aSyn expression by ASO restored dopaminergic neurotransmission deficits but failed to provide behavioral improvement [64]. Furthermore, treated animals in one study showed behavioral deficits, such as altered motor coordination, reduced food intake, and impaired sleep [62]. These findings raise potential safety concerns about therapeutic approaches reducing the genetic expression of aSyn due to possible interference with its physiological roles [65]. A phase 1 study on healthy subjects and MSA patients with the ION464 compound started in July 2022 (NCT04165486).
Immune Therapy
Passive Immunization
Two monoclonal antibodies targeting aSyn are currently being assessed in MSA, i.e., TAK-341 and Lu AF82422. Both compounds are supposed to bind to aggregated isoforms of aSyn while more effectively inhibiting the formation of aSyn oligomers [39]. While these molecules were primarily evaluated in animal models of PD, there is also evidence that passive immunization strategies induce aSyn clearance in transgenic models of MSA [37, 66]. TAK-341 (formerly MEDI1341) prevented aSyn accumulation and neural propagation in mice models using lentiviral vector-mediated overexpression of aSyn [38]. Phase 1 studies on healthy subjects (NCT03272165) and PD patients (NCT04449484) provided evidence for safety and dose-dependent target engagement [67]. Lu AF82422 was well tolerated in naive animals, healthy humans, and patients with PD [68, 69]. Both compounds are currently evaluated in phase 2 studies in MSA patients (NCT05526391, NCT05104476).
Another strategy combines immunization (CD5-5) with an anti-inflammatory agent (lenalidomide). This combination attenuated behavioral deficits and reduced aSyn levels, astrogliosis, and microgliosis in transgenic MSA mice [66]. This strategy has yet to be implemented in studies in humans.
Active Immunization
Active immunization may be therapeutic by requiring less frequent administration than passive immunization. One concern in the past has been cross-reactivity and T-cell-mediated toxicity [70]. Recent advances in the bioengineering of antigenic candidates have allowed the overcoming of these limitations by producing neo-epitopes inducing a specific humoral response while preventing T-cell activation [40]. When tested in transgenic PD, LBD, and MSA models, the neo-epitope AFF1 generated sustained plasma levels of IgG against aSyn oligomers and targeted both intracellular and axonal aSyn. AFF1 effectively mitigated neurodegeneration and behavioral deficits in these preclinical models [71,72,73].
The two epitope variants PD01 (corresponds to AFF1 in preclinical studies) and PD03 were evaluated in phase 1 studies in patients with PD and MSA. All studies showed a good safety profile, and both compounds induced antibodies against the immunizing peptide and, to a lesser extent, against the alpha-synuclein epitope, with reactivation after booster injections [74, 75]. When tested in MSA patients, PD01 induced higher antibody titers against aSyn than PD03, and both compounds were well tolerated except for transient injection-site reactions [76]. As expected, the number of adverse events was higher than those observed in PD patients due to the overall severity of MSA compared to PD. Notably, none of the studies reported a neuroinflammatory event. More recently, another immunizing peptide targeting specifically oligomeric and fibrillar aSyn (UB-312) was tested on healthy subjects. It induced anti-aSyn antibodies in CSF and showed a good safety profile [77]. Further development includes enrolling patients with PD, MSA, and LBD in a phase 1/2 study ([78], NCT05634876).
Aggregation Inhibitors
Rifampicin was the first drug tested in MSA patients for its potential anti-aggregation properties against aSyn. It successfully reduced oligomeric forms of aSyn and inhibited phosphorylation in a mouse model of MSA [79]. However, a phase 1/2 study including 100 participants failed to demonstrate any significant effect [80].
Epigallocatechin gallate (EGCG) is a green tea polyphenol with a specific affinity for various beta-sheet structured proteins. It prevented aSyn aggregation and reduced neuroinflammation and oxidative stress in mouse and non-human primate models of PD [43]. However, a phase 3 trial in MSA failed to demonstrate efficacy on clinical outcomes. A small MRI sub-analysis showed lower atrophy progression in the striatum and precentral gyrus [41].
ATH434 is believed to reduce the conversion of aSyn protofibrils to fibrils through its ability to reduce the iron pool within brain structures [42]. In mouse models of MSA, it decreased aSyn burden, preserved midbrain dopamine neuron loss, and reduced motor and behavioral impairments [42, 81, 82]. ATH434 displayed favorable safety profiles and pharmacokinetics in healthy subjects [44]. A phase 2 study recruiting MSA patients is underway, with an estimated completion date in 2024 (NCT05109091). The primary endpoint is the change in the brain iron content, as MRI measured. The concept of iron chelation for treating synucleinopathies has been recently challenged. Despite promising preclinical and phase 1/2 results, deferiprone led to a deterioration of motor function in de-novo, untreated (i.e., not receiving dopamine replacement therapy) PD patients in a recent phase 3 trial [45]. This outcome was attributed to excessive iron depletion, impeding its catalytic action on tyrosine hydroxylase and causing decreased dopamine synthesis. Unlike deferiprone, ATH434 was designed to chelate iron with lower affinity [42].
Anle138b, an inhibitor of amyloid compound aggregation, has a high affinity to oligomeric forms of aSyn. It reduces the accumulation of aSyn and mitigates behavioral deficits and neurodegeneration in MSA and PD animal models [83, 84]. Phase 1 trials involving healthy subjects and PD patients showed no safety concerns and good pharmacokinetics [85, 86].
Other potential candidates for reducing aSyn aggregation are being investigated in preclinical and clinical studies. Preclinical studies reported beneficial effects of the molecular tweezer CLR01. This nano-chaperone molecule prevents the formation of oligomeric forms of aSyn and attenuates nigral neurodegeneration [46, 47]. Similarly, belnacasan, a caspase-1 inhibitor preventing the C-terminal truncation of aSyn, decreased the formation of high molecular weight species of aSyn and mitigated inclusion formation and neurodegeneration in a transgenic mouse model of MSA [48].
Clearance Enhancer
Several candidates have been considered to enhance the clearance of aSyn through the lysosomal pathway and macroautophagy. This approach is based on preclinical studies showing that aSyn is degraded via chaperone-mediated autophagy and that aSyn aggregation impairs macroautophagy [87, 88]. Decreased nuclear levels of transcription factor EB (TFEB), a master regulator of autophagy, were found in MSA [49], and overexpression of TFEB in oligodendrocytes provided neuroprotection and decreased aSyn burden in a mouse model of MSA [49]. Given that autophagy is negatively regulated by the mammalian target of the rapamycin (mTOR) complex, mTOR inhibition with sirolimus was tested in a clinical trial. A futility analysis showed that rapamycin did not affect clinical progression or biological and neuroimaging disease markers in MSA patients [89]. This study recorded an unexpectedly high dropout rate with 22 of the 47 randomized patients who completed the required visits. Beyond early termination because of futility, one additional explanation may be a more advanced disease (i.e., patients eligible for up to 4 years after diagnosis).
Additional targets for increasing aSyn clearance are currently studied in preclinical proof-of-concept studies (Table 3) or PD/DLB clinical trials. Among these are inhibitors targeting cellular Abelson tyrosine kinase (c-Abl), which inhibits the phosphorylation of aSyn at residue 39, thereby enhancing its clearance through autophagy [50]. Several kinase inhibitors acting through the c-Abl pathway are currently being examined in clinical trials in patients with PD (NCT04691661, NCT04350177) and DLB (NCT03888222). In MSA, the compound nilotinib showed no beneficial effects in transgenic mice, but other candidates are considered [51, 52]. Additional compounds include monophosphoryl lipid A, an agonist of the Toll-like Receptor 4 that promotes microglial activation [90], the use of microRNAs of targeted genes or transcription factors that promote autophagy [91], and enzymatic degradation using the kallikrein-6 protease [92, 93].
Other Approaches
Studies have explored the potential neuroprotective properties of molecules in preventing neural loss through mechanisms that differ from the aSyn pathway. These encompass neurotrophic support, apoptosis, inflammatory processes, or mitochondrial function. Since the tested molecules may interfere with multiple pathways, the categorization below is intended to enhance understanding. The following studies are summarized in Tables 2 and 3.
For instance, riluzole was one of the first molecules tested in a large cohort of MSA patients [94]. This study achieved the most extensive recruitment of patients with MSA, with over 400 individuals. Notably, no specific outcome assessment was available during this study. Inclusions were based on operational criteria that displayed good accuracy according to a subsequent pathological validation, and the primary endpoint was overall survival. This effort highlighted the feasibility of recruiting large cohorts of patients and using survival as the primary endpoint, but the study failed its primary endpoint.
Neurotrophic Support
Selective serotonin reuptake inhibitors (SSRI) were found to have a potential effect on motor symptoms [95]. One study explored the symptomatic effect of fluoxetine but was inefficient in reducing disease progression in patients [96]. Exploratory analyses in this study showed a modest reduction in motor scores in the treated group. This ancillary result raised the question about the study’s potential lack of statistical power to achieve its primary endpoint. Preclinical evidence also suggests a possible involvement of the serotonin system in MSA. Precisely, serotoninergic depletion was found in animal models of MSA, and pathological studies of patients with MSA [97, 98] and SSRI could act as neuroprotective agents in a mouse model of MSA [97, 99]
Autologous mesenchymal cell (MSC) therapy is the only intervention that significantly attenuated disease progression in MSA in a small single-center trial [100]. MSCs were administered intravenously and intra-arterially. The recruitment was limited to MSA-C patients (n=33), and the trial raised safety concerns since approximately one-third of study participants receiving intra-arterial administration experienced infraclinical ischemic stroke. Another small open-label trial (n=24) evaluated the safety and tolerability of intrathecal administration of MSCs. Patients in the high-dose group frequently complained about low back pain, in line with the thickening/enhancement of lumbar nerve roots on MRI [101]. Following the small open-label trial, a randomized phase 2 trial assessing the efficacy of intrathecal MSCs is currently recruiting patients (NCT05167721).
The monoamine oxidase inhibitor (MAOI) rasagiline was tested in a large randomized trial involving 174 patients following an indication of a neuroprotective effect in a transgenic mouse model of MSA [102]. This study failed to demonstrate any significant effect on the primary outcome, i.e., the change in total UMSARS score or other endpoints, including neuroimaging [103]. Safinamide, another MAOI, was recently tested in an exploratory study involving 49 patients, 32 of whom received active treatment. Preliminary results showed that the proportion of adverse events was similar to that of the placebo group, but no publication of the full results is available (NCT03753763).
Other candidates are currently investigated in preclinical PD models but are also considered potential targets for MSA. KM-819, an FAF1 inhibitor, demonstrated neuroprotection in PD animal models [104]. It also exhibited favorable safety and pharmacokinetics in healthy subjects [105]. It is undergoing phase 2 trials for MSA (NCT05695378) and PD patients (NCT05670782). Phenotypic screening identified the potential of Stearoyl-CoA Desaturase (SCD) inhibition to reduce aSyn neurotoxicity [106, 107]. The SCD inhibitor YTX-7739 was well tolerated in healthy participants and PD patients, but further developments are pending [108].
Potential targets include FTY720-Mitoxy, a non-phosphorylated version of the sphingosine-1 phosphate receptor (S1PR) agonist fingolimod. It promotes neurotrophic factor release without T-cell immunosuppression and has demonstrated benefits in a mouse model, affecting aSyn pathology, neurotrophic factors, and motor functions [55, 109]. One S1PR agonist has already been tested on healthy participants (NCT04578028) and is currently recruiting MSA patients for a safety study (NCT05923866).
Epigenetic factors, like the pan-histone deacetylase inhibitor (HDACi), improved survival and motor function in an MSA mouse model [110]. Another approach involves benztropine, a muscarinic acetylcholine receptor antagonist that may enhance myelination and prevent neural cell loss [111].
Mitochondrial Dysfunction
Ubiquinol is the reduced form of coenzyme Q10 (CoQ10) essential to mitochondrial function. This approach followed the identification of rare variants and mutations in the COQ2 gene involved in CoQ10 biosynthesis and the reduction of COQ10 levels in CSF and cerebellar tissues of patients [112,113,114,115]. High doses of CoQ10 were well tolerated in healthy subjects, and patients (n=69) receiving CoQ10 demonstrated significantly slower motor progression compared to placebo (n=70) [57, 116]. Notably, the observed benefits could not be solely attributed to patients with a COQ2 mutation. Some limitations are still to be considered. Firstly, the study recruited a majority of the MSA-C subtype. Secondly, the effect size (−1.7 point difference in the UMSARS motor scale after 48 weeks of follow-up) is below what is considered clinically meaningful [117]
Modulating the Insulin/IGF1 Pathway
Growth hormone (GH) has neurotrophic effects and acts as a prohormone for IGF-1. Insulin/IGF-1 signaling contributes to nerve cell metabolism and exerts prosurvival effects. Many preclinical studies showed that IGF-1 preserves neural loss due to experimental injury, and impaired insulin/IGF1 signaling exacerbates dopamine cell loss in animal models of synucleinopathies [118]. Markers of insulin resistance correlate with aSyn burden in the brain of patients with MSA, suggesting a role in aSyn accumulation, and the antidiabetic glucagon-like peptide-1 agonist exenatide showed neuroprotective effects in transgenic MSA mice [53]. A small open-label phase 2 trial assessing the efficacy of exenatide in MSA patients is currently being conducted (NCT04431713). Similarly, knocking down GRK2, a key inhibitor of insulin signaling, showed positive effects on neural cell loss and aSyn load in a mouse model of MSA [119].
The use of recombinant GH has been assessed in a randomized placebo-controlled study involving 43 patients with MSA. Despite a trend for a positive effect on the evolution of motor symptoms, it did not reach its primary endpoint. A high dropout rate (37% of participants), leading to lower statistical power, may have contributed to this negative result [58].
Neuroinflammation and Oxidative Stress
Other strategies investigated the impact on neuroinflammation [120]. To this extent, previous trials using intravenous immunoglobulins or the antimicrobial agent minocycline failed to demonstrate a neuroprotective effect [54, 56]. The production of inflammatory oxidative species by phagocytic cells was also studied in a mouse model of MSA. When treated with a myeloperoxidase inhibitor, animals showed contrasting results on behavioral impairment and reduction of neural loss [121, 122]. In human studies, a small PET study in patients with PD showed that the myeloperoxidase inhibitor verdiperstat affects microglial activation but failed to demonstrate any clinical effect [123]. Conversely, exploratory analyses of a phase 2 study revealed a reduction in the total UMSARS progression among patients with MSA who received verdiperstat, while no significant effect was observed on microglial activation as assessed by PET imaging [59]. A larger multicentric randomized trial of 336 participants assessed the efficacy of verdiperstat on MSA patients. Notably, this study used a modified version of the UMSARS, comprising a subset of UMSARS I and II items reflecting activities of daily living, as a primary endpoint. The study failed its primary (based on clinical progression) and key secondary outcomes (NCT03952806).
Urate serum levels are negatively correlated with disease severity [124] and were associated with white matter integrity in a diffusion-based MRI study in patients with MSA [125]. Increasing urate levels were then tested on a tolerability study using inosine 5’-monophosphate, which showed no safety concerns and may represent a potential new target for efficacy studies [126].
Other candidates are currently investigated in preclinical PD models but are also considered potential targets for MSA. KM-819, an FAF1 inhibitor, demonstrated neuroprotection in PD animal models. It also exhibited favorable safety and pharmacokinetics in healthy subjects. It is undergoing phase 2 trials in MSA (NCT05695378) and PD patients (NCT05670782). Phenotypic screening identified the potential of Stearoyl-CoA Desaturase (SCD) inhibition to reduce aSyn neurotoxicity. The SCD inhibitor YTX-7739 was presented as well tolerated in healthy participants and PD patients, but further developments are pending.
Potential targets include FTY720-Mitoxy, a non-phosphorylated version of the sphingosine-1 phosphate receptor (S1PR) agonist fingolimod. It promotes neurotrophic factor release without T-cell immunosuppression and has demonstrated benefits in a mouse model, affecting aSyn pathology, neurotrophic factors, and motor functions. One S1PR agonist has already been tested on healthy participants (NCT04578028) and is currently recruiting MSA patients for a safety study (NCT05923866).
Epigenetic factors, like the pan-histone deacetylase inhibitor (HDACi), improved survival and motor functions in an MSA mouse model. Another approach involves benztropine, a muscarinic acetylcholine receptor antagonist that may enhance myelination and prevent neural cell loss.
Conclusion
Over 30 compounds have been tested in clinical trials in MSA over the past few decades. While this illustrates a strong treatment pipeline, only two have reached their primary endpoint. Negative outcomes contrast the many preclinical studies showing positive results for compounds that later failed, highlighting the importance of better understanding underlying disease mechanisms and improving preclinical models. Finally, efforts to refine clinical measurement tools, innovative statistical methods, and developments in biomarker research will undoubtedly enhance the design of future neuroprotection trials in MSA and the likelihood of positive outcomes. Biomarkers will play an increasing role in assessing target engagement, increasing diagnostic accuracy, efficacy endpoints, and patient stratification.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Poewe W, Stankovic I, Halliday G, Meissner WG, Wenning GK, Pellecchia MT, Seppi K, Palma J-A, Kaufmann H. Multiple system atrophy. Nat Rev Dis Primers. 2022;8:1–21.
Cykowski MD, Coon EA, Powell SZ, Jenkins SM, Benarroch EE, Low PA, Schmeichel AM, Parisi JE. Expanding the spectrum of neuronal pathology in multiple system atrophy. Brain. 2015;138:2293–309.
Wenning GK, Geser F, Krismer F, et al. The natural history of multiple system atrophy: a prospective European cohort study. The Lancet Neurology. 2013;12:264–74.
Luk KC, Kehm V, Carroll J, Zhang B, O’Brien P, Trojanowski JQ, Lee VM-Y. Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in non-transgenic mice. Science. 2012;338:949–53.
Wong YC, Krainc D. α-Synuclein toxicity in neurodegeneration: mechanism and therapeutic strategies. Nat Med. 2017;23:1–13.
Inoue M, Yagishita S, Ryo M, Hasegawa K, Amano N, Matsushita M. The distribution and dynamic density of oligodendroglial cytoplasmic inclusions (GCIs) in multiple system atrophy: a correlation between the density of GCIs and the degree of involvement of striatonigral and olivopontocerebellar systems. Acta Neuropathol. 1997;93:585–91.
Ozawa T, Paviour D, Quinn NP, et al. The spectrum of pathological involvement of the striatonigral and olivopontocerebellar systems in multiple system atrophy: clinicopathological correlations. Brain. 2004;127:2657–71.
Peng C, Gathagan RJ, Covell DJ, et al. Cellular milieu imparts distinct pathological α-synuclein strains in α-synucleinopathies. Nature. 2018;557:558–63.
• Shahnawaz M, Mukherjee A, Pritzkow S, et al. Discriminating α-synuclein strains in Parkinson’s disease and multiple system atrophy. Nature. 2020;578:273–7. This article explores the accuracy of a seed amplification assay to detect different patterns of alpha-synuclein aggregation between MSA and PD patients. They combined different methods to compare these patterns and observed distinct conformational strains of alpha-synuclein between MSA and PD
• Schweighauser M, Shi Y, Tarutani A, et al. Structures of α-synuclein filaments from multiple system atrophy. Nature. 2020;585:464–9. Using cryo-electron microscopy, the authors observed different structures of alpha-synuclein filaments in MSA and between MSA and DLB patients. This suggests that different alpha-synuclein strains could be related to distinct synucleinopathies
•• Wenning GK, Stankovic I, Vignatelli L, et al. The movement disorder society criteria for the diagnosis of multiple system atrophy. Movement Disorders. 2022;37:1131–48. This revision of diagnostic criteria of MSA aims to improve diagnosis accuracy at earlier stages of the disease and describes a new category of clinically established MSA that requires the presence of brain imaging features
Miki Y, Foti SC, Asi YT, Tsushima E, Quinn N, Ling H, Holton JL. Improving diagnostic accuracy of multiple system atrophy: a clinicopathological study. Brain. 2019;142:2813–27.
Koga S, Aoki N, Uitti RJ, van Gerpen JA, Cheshire WP, Josephs KA, Wszolek ZK, Langston JW, Dickson DW. When DLB, PD, and PSP masquerade as MSA. Neurology. 2015;85:404–12.
Osaki Y, Ben-Shlomo Y, Lees AJ, Wenning GK, Quinn NP. A validation exercise on the new consensus criteria for multiple system atrophy. Mov Disord. 2009;24:2272–6.
• Virameteekul S, Revesz T, Jaunmuktane Z, Warner TT, De Pablo-Fernández E. Pathological validation of the MDS criteria for the diagnosis of multiple system atrophy. Movement Disorders. 2023;38:444–52. This article provides evidence of enhanced diagnostic performances of the new diagnostic criteria of MSA and excellent accuracy of the new category of clinically established MSA, even at the early stages of the disease
Wenning GK, Tison F, Seppi K, et al. Development and validation of the Unified Multiple System Atrophy Rating Scale (UMSARS). Mov Disord. 2004;19:1391–402.
•• Krismer F, Palma J-A, Calandra-Buonaura G, et al. The unified multiple system atrophy rating scale: status, critique, and recommendations. Movement Disorders. 2022;37:2336–41. This review article describes the main limitation of the UMSARS and provides a roadmap to a revised version of the scale. The authors announced the creation of a task force of experts and the preparatory steps for an exhaustive documentation to provide a more comprehensive and patient-centered scale
Krismer F, Seppi K, Jönsson L, et al. Sensitivity to change and patient-centricity of the unified multiple system atrophy rating scale items: a data-driven analysis. Movement Disorders. 2022;37:1425–31.
Potashman M, Brady L, Durham S, et al (2023) Psychometric validation of a modified united multiple system atrophy rating scale (S43.002). In: Wednesday, April 26. Lippincott Williams & Wilkins, p 1958
Potashman M, Huang I, Durham S, et al. Patient concept elicitation interviews: insights into multiple system atrophy (MSA) patient experiences and relevance of a modified united multiple system atrophy rating scale (P8-9.003). In: Tuesday, April 25. Lippincott Williams & Wilkins; 2023. p. 2057.
Palma J-A, Vernetti PM, Perez MA, et al. Limitations of the Unified Multiple System Atrophy Rating Scale as outcome measure for clinical trials and a roadmap for improvement. Clin Auton Res. 2021;31:157–64.
Foubert-Samier A, Pavy-Le Traon A, Saulnier T, Le-Goff M, Fabbri M, Helmer C, Rascol O, Proust-Lima C, Meissner WG. An item response theory analysis of the unified multiple system atrophy rating scale. Parkinsonism & Related Disorders. 2022;94:40–4.
Foubert-Samier A, Pavy-Le Traon A, Guillet F, Le-Goff M, Helmer C, Tison F, Rascol O, Proust-Lima C, Meissner WG. Disease progression and prognostic factors in multiple system atrophy: a prospective cohort study. Neurobiol Dis. 2020;139:104813.
Saulnier T, Philipps V, Meissner WG, Rascol O, Pavy-Le Traon A, Foubert-Samier A, Proust-Lima C. Joint models for the longitudinal analysis of measurement scales in the presence of informative dropout. Methods. 2022;203:142–51.
Péran P, Barbagallo G, Nemmi F, Sierra M, Galitzky M, Traon AP-L, Payoux P, Meissner WG, Rascol O. MRI supervised and unsupervised classification of Parkinson’s disease and multiple system atrophy. Mov Disord. 2018;33:600–8.
Chougar L, Faouzi J, Pyatigorskaya N, et al. Automated categorization of Parkinsonian syndromes using magnetic resonance imaging in a clinical setting. Movement Disorders. 2021;36:460–70.
• Smith R, Capotosti F, Schain M, et al. The α-synuclein PET tracer [18F] ACI-12589 distinguishes multiple system atrophy from other neurodegenerative diseases. Nat Commun. 2023;14:6750. This article shows a promising perspective for the use of an alpha-synuclein PET tracer to enhance diagnostic performances. The authors presented a specific biding to strategic brain regions related to MSA pathology and the ability of the tracer to distinguish between MSA patients and healthy controls or other synucleinopathies
• Poggiolini I, Gupta V, Lawton M, et al. Diagnostic value of cerebrospinal fluid alpha-synuclein seed quantification in synucleinopathies. Brain. 2022;145:584–95. In this article, the authors explored the ability of seed amplification assay to distinguish between synucleinopathies and predict disease conversion of REM-sleep behavior disorder. This highlights the potential use of this method to detect synucleinopathy at prodromal stages
Rossi M, Candelise N, Baiardi S, et al. Ultrasensitive RT-QuIC assay with high sensitivity and specificity for Lewy body-associated synucleinopathies. Acta Neuropathol. 2020;140:49–62.
Chelban V, Nikram E, Perez-Soriano A, et al. Neurofilament light levels predict clinical progression and death in multiple system atrophy. Brain. 2022;145:4398–408.
Singer W, Schmeichel AM, Shahnawaz M, et al. Alpha-synuclein oligomers and neurofilament light chain in spinal fluid differentiate multiple system atrophy from Lewy body synucleinopathies. Ann Neurol. 2020;88:503–12.
Tabrizi SJ, Leavitt BR, Landwehrmeyer GB, et al. Targeting huntingtin expression in patients with Huntington’s disease. New England Journal of Medicine. 2019;380:2307–16.
Wave Life Sciences Provides Update on Phase 1b/2a PRECISION-HD Trials - Wave Life Sciences. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-provides-update-phase-1b2a-precision-hd. Accessed 17 May 2023
Alarcón-Arís D, Recasens A, Galofré M, et al. Selective α-synuclein knockdown in monoamine neurons by intranasal oligonucleotide delivery: potential therapy for Parkinson’s disease. Mol Ther. 2018;26:550–67.
Uehara T, Choong C-J, Nakamori M, et al. Amido-bridged nucleic acid (AmNA)-modified antisense oligonucleotides targeting α-synuclein as a novel therapy for Parkinson’s disease. Sci Rep. 2019;9:7567.
Miquel-Rio L, Alarcón-Arís D, Torres-López M, et al. Human α-synuclein overexpression in mouse serotonin neurons triggers a depressive-like phenotype. Rescue by oligonucleotide therapy. Transl Psychiatry. 2022;12:79.
Kallab M, Herrera-Vaquero M, Johannesson M, Eriksson F, Sigvardson J, Poewe W, Wenning GK, Nordström E, Stefanova N. Region-specific effects of immunotherapy with antibodies targeting α-synuclein in a transgenic model of synucleinopathy. Front Neurosci. 2018;12:452.
Schofield DJ, Irving L, Calo L, et al. Preclinical development of a high affinity α-synuclein antibody, MEDI1341, that can enter the brain, sequester extracellular α-synuclein and attenuate α-synuclein spreading in vivo. Neurobiol Dis. 2019;132:104582.
Knecht L, Folke J, Dodel R, Ross JA, Albus A. Alpha-synuclein immunization strategies for synucleinopathies in clinical studies: a biological perspective. Neurotherapeutics. 2022;19:1489–502.
Schneeberger A, Mandler M, Mattner F, Schmidt W. AFFITOME® technology in neurodegenerative diseases: the doubling advantage. Hum Vaccin. 2010;6:948–52.
Levin J, Maaß S, Schuberth M, et al. Safety and efficacy of epigallocatechin gallate in multiple system atrophy (PROMESA): a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2019;18:724–35.
Finkelstein DI, Billings JL, Adlard PA, et al. The novel compound PBT434 prevents iron mediated neurodegeneration and alpha-synuclein toxicity in multiple models of Parkinson’s disease. Acta Neuropathol Commun. 2017;5:53.
Levin J, Maaß S, Schuberth M, et al. The PROMESA-protocol: progression rate of multiple system atrophy under EGCG supplementation as anti-aggregation-approach. J Neural Transm. 2016;123:439–45.
Stamler D, Bradbury M, Wong C, Offman E. A phase 1 study of PBT434, a novel small molecule inhibitor of α-synuclein aggregation, in adult and older adult volunteers (4871). Neurology. 2020;94:4871
Devos D, Labreuche J, Rascol O, et al. Trial of deferiprone in Parkinson’s disease. N Engl J Med. 2022;387:2045–55.
Herrera-Vaquero M, Bouquio D, Kallab M, et al. The molecular tweezer CLR01 reduces aggregated, pathologic, and seeding-competent α-synuclein in experimental multiple system atrophy. Biochim Biophys Acta Mol Basis Dis. 2019;1865:165513.
Bengoa-Vergniory N, Faggiani E, Ramos-Gonzalez P, et al. CLR01 protects dopaminergic neurons in vitro and in mouse models of Parkinson’s disease. Nat Commun. 2020;11:4885.
Bassil F, Fernagut P-O, Bezard E, Pruvost A, Leste-Lasserre T, Hoang QQ, Ringe D, Petsko GA, Meissner WG. Reducing C-terminal truncation mitigates synucleinopathy and neurodegeneration in a transgenic model of multiple system atrophy. Proc Natl Acad Sci U S A. 2016;113:9593–8.
Arotcarena M-L, Bourdenx M, Dutheil N, et al. Transcription factor EB overexpression prevents neurodegeneration in experimental synucleinopathies. JCI Insight. 2019;4(e129719):129719.
Mahul-Mellier A-L, Fauvet B, Gysbers A, et al. c-Abl phosphorylates α-synuclein and regulates its degradation: implication for α-synuclein clearance and contribution to the pathogenesis of Parkinson’s disease. Hum Mol Genet. 2014;23:2858–79.
Lopez-Cuina M, Guerin PA, Canron M-H, Delamarre A, Dehay B, Bezard E, Meissner WG, Fernagut P-O. Nilotinib fails to prevent synucleinopathy and cell loss in a mouse model of multiple system atrophy. Mov Disord. 2020;35:1163–72.
Inhibikase therapeutics announces FDA has lifted the full clinical hold on IkT-148009 in multiple system atrophy. In: Inhibikase Therapeutics, Inc. 2023 https://www.inhibikase.com/news/press-releases/detail/77/inhibikase-therapeutics-announces-fda-has-lifted-the-full. Accessed 3 Nov 2023
Bassil F, Canron M-H, Vital A, Bezard E, Li Y, Greig NH, Gulyani S, Kapogiannis D, Fernagut P-O, Meissner WG. Insulin resistance and exendin-4 treatment for multiple system atrophy. Brain. 2017;140:1420–36.
Dodel R, Spottke A, Gerhard A, et al. Minocycline 1-year therapy in multiple-system-atrophy: effect on clinical symptoms and [(11)C] (R)-PK11195 PET (MEMSA-trial). Mov Disord. 2010;25:97–107.
Vidal-Martinez G, Segura-Ulate I, Yang B, Diaz-Pacheco V, Barragan JA, De-Leon Esquivel J, Chaparro SA, Vargas-Medrano J, Perez RG. FTY720-Mitoxy reduces synucleinopathy and neuroinflammation, restores behavior and mitochondria function, and increases GDNF expression in Multiple System Atrophy mouse models. Exp Neurol. 2020;325:113120.
Novak P, Williams A, Ravin P, Zurkiya O, Abduljalil A, Novak V. Treatment of multiple system atrophy using intravenous immunoglobulin. BMC Neurol. 2012;12:131.
Mitsui J, Matsukawa T, Uemura Y, et al. High-dose ubiquinol supplementation in multiple-system atrophy: a multicentre, randomised, double-blinded, placebo-controlled phase 2 trial. eClinicalMedicine. 2023; https://doi.org/10.1016/j.eclinm.2023.101920.
Holmberg B, Johansson J-O, Poewe W, et al. Safety and tolerability of growth hormone therapy in multiple system atrophy: a double-blind, placebo-controlled study. Movement Disorders. 2007;22:1138–44.
Mullen JA, Savage AB, Minkwitz MC, Jucaite A, Cselényi Z, Johnström P, Posener J, Kugler A, Wenning G, Kaufmann H, Barone P, Meissner W, Carson R, Kreisl WC, Rabiner EA, Farde L, Poewe W, on behalf of the MSA Study Group. Safety, biomarker effects, and efficacy of the myeloperoxidase inhibitor AZD3241 in patients with multiple system atrophy: a 12-week randomized multicenter PET study (P.6016). Abstracts of the 6th international multiple system atrophy congress. Clin Auton Res 2018;28:137–60.
Roberts TC, Langer R, Wood MJA. Advances in oligonucleotide drug delivery. Nat Rev Drug Discov. 2020;19:673–94.
Cole TA, Zhao H, Collier TJ, et al. α-Synuclein antisense oligonucleotides as a disease-modifying therapy for Parkinson’s disease. JCI Insight. 2021;6(e135633):135633.
Boutros SW, Raber J, Unni VK. Effects of alpha-synuclein targeted antisense oligonucleotides on Lewy body-like pathology and behavioral disturbances induced by injections of pre-formed fibrils in the mouse motor cortex. J Parkinsons Dis. 2021;11:1091–115.
Yang J, Luo S, Zhang J, Yu T, Fu Z, Zheng Y, Xu X, Liu C, Fan M, Zhang Z. Exosome-mediated delivery of antisense oligonucleotides targeting α-synuclein ameliorates the pathology in a mouse model of Parkinson’s disease. Neurobiol Dis. 2021;148:105218.
Pavia-Collado R, Cóppola-Segovia V, Miquel-Rio L, et al. Intracerebral administration of a ligand-ASO conjugate selectively reduces α-synuclein accumulation in Monoamine Neurons of Double mutant human A30P*A53T*α-synuclein transgenic mice. Int J Mol Sci. 2021;22:2939.
Abeliovich A, Schmitz Y, Fariñas I, et al. Mice lacking alpha-synuclein display functional deficits in the nigrostriatal dopamine system. Neuron. 2000;25:239–52.
Valera E, Spencer B, Fields JA, Trinh I, Adame A, Mante M, Rockenstein E, Desplats P, Masliah E. Combination of alpha-synuclein immunotherapy with anti-inflammatory treatment in a transgenic mouse model of multiple system atrophy. Acta Neuropathol Commun. 2017;5:2.
Shering C, Pomfret M, Kubiak R, et al. Reducing α-synuclein in human CSF; an evaluation of safety, tolerability, pharmacokinetics and pharmacodynamics of MEDI1341, an α-synuclein-specific antibody, in healthy volunteers and Parkinson’s disease patients (P1-11.007). Neurology. 2023; https://doi.org/10.1212/WNL.0000000000202579.
Fjord-Larsen L, Thougaard A, Wegener KM, Christiansen J, Larsen F, Schrøder-Hansen LM, Kaarde M, Ditlevsen DK. Nonclinical safety evaluation, pharmacokinetics, and target engagement of Lu AF82422, a monoclonal IgG1 antibody against alpha-synuclein in development for treatment of synucleinopathies. MAbs. 13:1994690.
Buur L, Wiedemann J, Larsen F, Ben Alaya-Fourati F, Kallunki P, Ditlevsen D, Sørensen M, Meulien D. The anti-alpha-synuclein antibody Lu AF82422 was safe and well tolerated in a FIH-SAD study in healthy subjects and patients with PD [abstract]. Mov Disord. 2022;37(suppl 2).
Gilman S, Koller M, Black RS, et al. Clinical effects of Abeta immunization (AN1792) in patients with AD in an interrupted trial. Neurology. 2005;64:1553–62.
Mandler M, Valera E, Rockenstein E, et al. Next-generation active immunization approach for synucleinopathies: implications for Parkinson’s disease clinical trials. Acta Neuropathol. 2014;127:861–79.
Mandler M, Valera E, Rockenstein E, et al. Active immunization against alpha-synuclein ameliorates the degenerative pathology and prevents demyelination in a model of multiple system atrophy. Mol Neurodegener. 2015;10:10.
Mandler M, Rockenstein E, Overk C, et al. Effects of single and combined immunotherapy approach targeting amyloid β protein and α-synuclein in a dementia with Lewy bodies-like model. Alzheimers Dement. 2019;15:1133–48.
Volc D, Poewe W, Kutzelnigg A, et al. Safety and immunogenicity of the α-synuclein active immunotherapeutic PD01A in patients with Parkinson’s disease: a randomised, single-blinded, phase 1 trial. Lancet Neurol. 2020;19:591–600.
Poewe W, Volc D, Seppi K, et al. Safety and tolerability of active immunotherapy targeting α-synuclein with PD03A in patients with early Parkinson’s disease: a randomized, placebo-controlled, phase 1 study. J Parkinsons Dis. 2021;11:1079–89.
Meissner WG, Traon AP-L, Foubert-Samier A, et al. A phase 1 randomized trial of specific active α-synuclein immunotherapies PD01A and PD03A in multiple system atrophy. Movement Disorders. 2020;35:1957–65.
Yu HJ, Thijssen E, van Brummelen E, van der Plas JL, Radanovic I, Moerland M, Hsieh E, Groeneveld GJ, Dodart J-C. A randomized first-in-human study with UB-312, a UBITh® α-synuclein peptide vaccine. Mov Disord. 2022;37:1416–24.
Vaxxinity completes enrollment in part B of UB-312 phase 1 clinical trial for Parkinson’s disease | Vaxxinity. https://ir.vaxxinity.com/news-releases/news-release-details/vaxxinity-completes-enrollment-part-b-ub-312-phase-1-clinical/. Accessed 12 Apr 2023
Ubhi K, Rockenstein E, Mante M, Patrick C, Adame A, Thukral M, Shults C, Masliah E. Rifampicin reduces alpha-synuclein in a transgenic mouse model of multiple system atrophy. Neuroreport. 2008;19:1271–6.
Low PA, Robertson D, Gilman S, et al. Efficacy and safety of rifampicin for multiple system atrophy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2014;13:268–75.
Finkelstein DI, Shukla JJ, Cherny RA, Billings JL, Saleh E, Stefanova N, Barnham KJ, Adlard PA. The compound ATH434 prevents alpha-synuclein toxicity in a murine model of multiple system atrophy. J Parkinsons Dis. 2022;12:105–15.
Heras-Garvin A, Refolo V, Schmidt C, Malfertheiner K, Wenning GK, Bradbury M, Stamler D, Stefanova N. ATH434 reduces α-synuclein-related neurodegeneration in a murine model of multiple system atrophy. Movement Disorders. 2021;36:2605–14.
Heras-Garvin A, Weckbecker D, Ryazanov S, Leonov A, Griesinger C, Giese A, Wenning GK, Stefanova N. Anle138b modulates α-synuclein oligomerization and prevents motor decline and neurodegeneration in a mouse model of multiple system atrophy. Movement Disorders. 2019;34:255–63.
Levin J, Schmidt F, Boehm C, Prix C, Bötzel K, Ryazanov S, Leonov A, Griesinger C, Giese A. The oligomer modulator anle138b inhibits disease progression in a Parkinson mouse model even with treatment started after disease onset. Acta Neuropathol. 2014;127:779–80.
Levin J, Sing N, Melbourne S, et al. Safety, tolerability and pharmacokinetics of the oligomer modulator anle138b with exposure levels sufficient for therapeutic efficacy in a murine Parkinson model: a randomised, double-blind, placebo-controlled phase 1a trial. eBioMedicine. 2022; https://doi.org/10.1016/j.ebiom.2022.104021.
Levin J, Singh N, Melbourne S, Morgan A, Carroll C, Fietzek U, Ryazanov S, Leonov A, Griesinger CH, Schmidt F, Weckbecker D, Prager K, Matthias T, Giese A. Anle138b-P1-02: a randomised, double-blinded, placebo-controlled phase 1b study to investigate safety, tolerability, pharmacokinetics and pharmacodynamics of the oligomer modulator anle138b in Parkinson’s disease [abstract]. Mov Disord. 2023;38(suppl 1).
Lee H-J, Khoshaghideh F, Patel S, Lee S-J. Clearance of α-synuclein oligomeric intermediates via the lysosomal degradation pathway. J Neurosci. 2004;24:1888–96.
Cuervo AM, Stefanis L, Fredenburg R, Lansbury PT, Sulzer D. Impaired degradation of mutant alpha-synuclein by chaperone-mediated autophagy. Science. 2004;305:1292–5.
Palma J-A, Martinez J, Millar Vernetti P, et al. mTOR inhibition with sirolimus in multiple system atrophy: a randomized, double-blind, placebo-controlled futility trial and 1-year biomarker longitudinal analysis. Mov Disord. 2022;37:778–89.
Venezia S, Refolo V, Polissidis A, Stefanis L, Wenning GK, Stefanova N. Toll-like receptor 4 stimulation with monophosphoryl lipid A ameliorates motor deficits and nigral neurodegeneration triggered by extraneuronal α-synucleinopathy. Mol Neurodegener. 2017;12:52.
Valera E, Spencer B, Mott J, et al. MicroRNA-101 modulates autophagy and oligodendroglial alpha-synuclein accumulation in multiple system atrophy. Front Mol Neurosci. 2017;10:329.
Spencer B, Valera E, Rockenstein E, Trejo-Morales M, Adame A, Masliah E. A brain-targeted, modified neurosin (kallikrein-6) reduces α-synuclein accumulation in a mouse model of multiple system atrophy. Mol Neurodegener. 2015;10:48.
Kiely AP, Miners JS, Courtney R, Strand C, Love S, Holton JL. Exploring the putative role of kallikrein-6, calpain-1 and cathepsin-D in the proteolytic degradation of α-synuclein in multiple system atrophy. Neuropathol Appl Neurobiol. 2019;45:347–60.
Bensimon G, Ludolph A, Agid Y, Vidailhet M, Payan C, Leigh PN. Riluzole treatment, survival and diagnostic criteria in Parkinson plus disorders: The NNIPPS Study. Brain. 2009;132:156–71.
Friess E, Kuempfel T, Modell S, Winkelmann J, Holsboer F, Ising M, Trenkwalder C. Paroxetine treatment improves motor symptoms in patients with multiple system atrophy. Parkinsonism Relat Disord. 2006;12:432–7.
Rascol O, Cochen de Cock V, Pavy-Le Traon A, et al. Fluoxetine for the symptomatic treatment of multiple system atrophy: the MSA-FLUO trial. Mov Disord. 2021;36:1704–11.
Ubhi K, Inglis C, Mante M, Patrick C, Adame A, Spencer B, Rockenstein E, May V, Winkler J, Masliah E. Fluoxetine ameliorates behavioral and neuropathological deficits in a transgenic model mouse of α-synucleinopathy. Exp Neurol. 2012;234:405–16.
Meyer M, Lamare F, Asselineau J, et al. Brain 5-HT1A receptor binding in multiple system atrophy: an [18 F]-MPPF PET study. Mov Disord. 2021;36:246–51.
Valera E, Ubhi K, Mante M, Rockenstein E, Masliah E. Antidepressants reduce neuroinflammatory responses and astroglial alpha-synuclein accumulation in a transgenic mouse model of multiple system atrophy. Glia. 2014;62:317–37.
Lee PH, Lee JE, Kim H-S, et al. A randomized trial of mesenchymal stem cells in multiple system atrophy. Ann Neurol. 2012;72:32–40.
Singer W, Dietz AB, Zeller AD, et al. Intrathecal administration of autologous mesenchymal stem cells in multiple system atrophy. Neurology. 2019;93:e77–87.
Stefanova N, Poewe W, Wenning GK. Rasagiline is neuroprotective in a transgenic model of multiple system atrophy. Exp Neurol. 2008;210:421–7.
Poewe W, Seppi K, Fitzer-Attas CJ, et al. Efficacy of rasagiline in patients with the parkinsonian variant of multiple system atrophy: a randomised, placebo-controlled trial. Lancet Neurol. 2015;14:145–52.
Park HS, Song YS, Moon BS, Yoo S-E, Lee JM, Chung Y-T, Kim E, Lee BC, Kim SE. Neurorestorative effects of a novel fas-associated factor 1 inhibitor in the MPTP model: an [18F]FE-PE2I positron emission tomography analysis study. Front Pharmacol. 2020;11:953.
Shin W, Lim KS, Kim M-K, et al. A first-in-human study to investigate the safety, tolerability, pharmacokinetics, and pharmacodynamics of KM-819 (FAS-associated factor 1 inhibitor), a drug for Parkinson’s disease, in healthy volunteers. Drug Des Devel Ther. 2019;13:1011–22.
Tardiff DF, Lucas M, Wrona I, Chang B, Chung CY, Le Bourdonnec B, Rhodes KJ, Scannevin RH. Non-clinical pharmacology of YTX-7739: a clinical stage stearoyl-CoA desaturase inhibitor being developed for Parkinson’s disease. Mol Neurobiol. 2022;59:2171–89.
Vincent BM, Tardiff DF, Piotrowski JS, et al. Inhibiting stearoyl-CoA desaturase ameliorates α-synuclein cytotoxicity. Cell Rep. 2018;25:2742–2754.e31.
Inc YT (2021) Yumanity Therapeutics’ YTX-7739 achieved target engagement at doses that were generally well tolerated in a phase 1a multiple ascending dose study in healthy volunteers. In: GlobeNewswire News Room. https://www.globenewswire.com/news-release/2021/04/22/2214878/0/en/Yumanity-Therapeutics-YTX-7739-Achieved-Target-Engagement-at-Doses-That-Were-Generally-Well-Tolerated-in-a-Phase-1a-Multiple-Ascending-Dose-Study-in-Healthy-Volunteers.html. Accessed 2 Nov 2023
Vargas-Medrano J, Segura-Ulate I, Yang B, Chinnasamy R, Arterburn JB, Perez RG. FTY720-Mitoxy reduces toxicity associated with MSA-like α-synuclein and oxidative stress by increasing trophic factor expression and myelin protein in OLN-93 oligodendroglia cell cultures. Neuropharmacology. 2019;158:107701.
Sturm E, Fellner L, Krismer F, Poewe W, Wenning GK, Stefanova N. Neuroprotection by epigenetic modulation in a transgenic model of multiple system atrophy. Neurotherapeutics. 2016;13:871–9.
Ettle B, Kerman BE, Valera E, et al. α-Synuclein-induced myelination deficit defines a novel interventional target for multiple system atrophy. Acta Neuropathol. 2016;132:59–75.
Multiple-System Atrophy Research Collaboration. Mutations in COQ2 in familial and sporadic multiple-system atrophy. N Engl J Med. 2013;369:233–44.
Barca E, Kleiner G, Tang G, et al. Decreased coenzyme Q10 levels in multiple system atrophy cerebellum. Journal of Neuropathology & Experimental Neurology. 2016;75:663–72.
Compta Y, Giraldo DM, Muñoz E, et al. Cerebrospinal fluid levels of coenzyme Q10 are reduced in multiple system atrophy. Parkinsonism & Related Disorders. 2018;46:16–23.
Schottlaender LV, Bettencourt C, Kiely AP, Chalasani A, Neergheen V, Holton JL, Hargreaves I, Houlden H. Coenzyme Q10 levels are decreased in the cerebellum of multiple-system atrophy patients. PLOS ONE. 2016;11:e0149557.
Mitsui J, Matsukawa T, Tanaka M, et al. Randomized, double-blind, placebo-controlled phase 1 study to evaluate the safety and pharmacokinetics of high doses of ubiquinol in healthy adults. Neurology and Clinical Neuroscience. 2022;10:14–24.
Krismer F, Seppi K, Wenning GK, Abler V, Papapetropoulos S, Poewe W. Minimally clinically important decline in the parkinsonian variant of multiple system atrophy. Mov Disord. 2016;31:1577–81.
Bassil F, Fernagut P-O, Bezard E, Meissner WG. Insulin, IGF-1 and GLP-1 signaling in neurodegenerative disorders: targets for disease modification? Prog Neurobiol. 2014;118:1–18.
Lopez-Cuina M, Guérin P, Dutheil N, Martin C, Lasserre TL, Fernagut P-O, Meissner WG, Bezard E. GRK2-targeted knockdown as therapy for multiple system atrophy. Mov Disord. 2023; https://doi.org/10.1002/mds.29422.
Stefanova N, Reindl M, Neumann M, Kahle PJ, Poewe W, Wenning GK. Microglial activation mediates neurodegeneration related to oligodendroglial alpha-synucleinopathy: implications for multiple system atrophy. Mov Disord. 2007;22:2196–203.
Stefanova N, Georgievska B, Eriksson H, Poewe W, Wenning GK. Myeloperoxidase inhibition ameliorates multiple system atrophy-like degeneration in a transgenic mouse model. Neurotox Res. 2012;21:393–404.
Kaindlstorfer C, Sommer P, Georgievska B, Mather RJ, Kugler AR, Poewe W, Wenning GK, Stefanova N. Failure of neuroprotection despite microglial suppression by delayed-start myeloperoxidase inhibition in a model of advanced multiple system atrophy: clinical implications. Neurotox Res. 2015;28:185–94.
Jucaite A, Svenningsson P, Rinne JO, et al. Effect of the myeloperoxidase inhibitor AZD3241 on microglia: a PET study in Parkinson’s disease. Brain. 2015;138:2687–700.
Fukae J, Fujioka S, Yanamoto S, Mori A, Nomi T, Hatano T, Fukuhara K, Ouma S, Hattori N, Tsuboi Y. Serum uric acid level is linked to the disease progression rate in male patients with multiple system atrophy. Clinical Neurology and Neurosurgery. 2017;158:15–9.
Yoo HS, Chung SJ, Lee YH, Ye BS, Sohn YH, Kwon H, Lee PH. Urate is closely linked to white matter integrity in multiple system atrophy. Ann Clin Transl Neurol. 2020;7:1029–39.
Jung Lee J, Han Yoon J, Jin Kim S, et al. Inosine 5’-Monophosphate to Raise Serum Uric Acid Level in Multiple System Atrophy (IMPROVE-MSA study). Clinical Pharmacology & Therapeutics. 2021;109:1274–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
M.F. received Grants from MSA Coalition, HORIZON 2022, Honoraria to speak from BIAL, AbbVie, Orkyn, Elivie, LvL médical and consultancies from Bial, Convatec and LvL médicale.
A.F.S. received honoraria from Aguettant Laboratory and Sanofi, grants from the French Rare Disease Foundation, from the French regional health agency (Agence Régionale de Santé de nouvelle Aquitaine), and from France Parkinson association.
W.G.M. reports personal fees from Elsevier, from Biohaven, Lundbeck, Roche, Servier, Alterity, Inhibikase, Teva and Takeda, outside the submitted work; and 1. International Parkinson and movement disorder society (Treasurer and Officer) 2. MSA Coalition (Member research steering committee) 3. Clément Fayat Foundation (Board of directors).
A.P.L. reports honoraria from Biohaven, HAC Pharma and speaker fees from Alnylam, outside the submitted work.
O.R. is advising following compagnies AbbVie, Acorda, Aguettant, Alkahest, AlzProtect, Apopharma, Astrazeneca, Bial, Biogen, Britannia, Buckwang, Cerevel, Clevexel, Contera, GE Healthcare, Handltherapeutic, Ionis, Irlab, Jazz, Kyowa, LGD Nuvamid, Lundbeck, Merck, Merz, MundiPharma, Neuralight, Neuratris, Neuroderm, Novartis, ONO Pharma, Orion Pharma, Parexel, PD Neurotechnology, Pfizer, Polycaps, Prexton, Roche Therapeutics, Sanofi, Scienture, Servier, Sombiotech, Sunovion, Supernus, Synagile, Thelonius Mind, Takeda, Théranexus, Teva, Tools4patient, UCB, Vision 2 voice, Zambon.
C.P.L., D.B., F.S., P.O.F., and T.S. have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bendetowicz, D., Fabbri, M., Sirna, F. et al. Recent Advances in Clinical Trials in Multiple System Atrophy. Curr Neurol Neurosci Rep 24, 95–112 (2024). https://doi.org/10.1007/s11910-024-01335-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-024-01335-0