Abstract
Purpose of the Review
Magnetoencephalography (MEG) is a functional neuroimaging technique that records neurophysiology data with millisecond temporal resolution and localizes it with subcentimeter accuracy. Its capability to provide high resolution in both of these domains makes it a powerful tool both in basic neuroscience as well as clinical applications. In neurology, it has proven useful in its ability to record and localize epileptiform activity. Epilepsy workup typically begins with scalp electroencephalography (EEG), but in many situations, EEG-based localization of the epileptogenic zone is inadequate. The complementary sensitivity of MEG can be crucial in such cases, and MEG has been adopted at many centers as an important resource in building a surgical hypothesis. In this paper, we review recent work evaluating the extent of MEG influence of presurgical evaluations, novel analyses of MEG data employed in surgical workup, and new MEG instrumentation that will likely affect the field of clinical MEG.
Recent Findings
MEG consistently contributes to presurgical evaluation and these contributions often change the plan for epilepsy surgery. Extensive work has been done to develop new analytic methods for localizing the source of epileptiform activity with MEG. Systems using optically pumped magnetometry (OPM) have been successfully deployed to record and localize epileptiform activity.
Summary
MEG remains an important noninvasive tool for epilepsy presurgical evaluation. Continued improvements in analytic methodology will likely increase the diagnostic yield of the test. Novel instrumentation with OPM may contribute to this as well, and may increase accessibility of MEG by decreasing cost.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The epilepsy presurgical evaluation has as its goal the estimation of the epileptogenic zone (EZ), the smallest brain volume whose ablation will result in remission of seizures [1]. The EZ is not measured directly and can only be estimated confidently after an ablative procedure, but is estimated empirically by several other zones whose locations and dimensions are known more or less definitely. These include, among others, the ictal onset zone (IOZ), the brain volume capable of generating electrographic seizures; the irritative zone (IZ), the brain volume capable of generating interictal epileptiform discharges; and the symptomatogenic zone, the brain volume capable of generating the patient’s ictal semiology. The strength of a presurgical hypothesis correlates with the degree of overlap between the various estimating zones. Although MEG is in principle capable of recording seizures, this is relatively rare, as MEG instrumentation (with a fixed helmet that requires that the patient lie or sit in one position) precludes the prolonged recordings that facilitate seizure capture on EEG. For this reason, MEG contributes to the presurgical evaluation primarily by estimating the IZ and not the IOZ.
IZ evaluation typically begins with scalp EEG, but further investigation with MEG is often warranted, for three reasons of decreasing significance. The first is that EEG and MEG have complementary sensitivities, with EEG more sensitive to radial sources, such as those arising from gyral crests of the cerebral convexities, whereas MEG is more sensitive to tangential sources, such as those arising from sulci, as well as obliquely oriented gyri such as the temporal tip [2, 3•]. MEG can therefore detect epileptiform activity not seen well (or at all) on EEG. The second reason is that MEG-based localization can be more accurate and precise than that based on EEG. This is due both to the smaller cortical area required to produce a spike on MEG compared to EEG [4], and the relative transparency of interposed tissues such as dura and skull to MEG compared to EEG [5,6,7]. The third advantage, which is least intrinsic to MEG, derives from methodologic factors: first, it is routinely implemented with a high number of sensors (further improving accuracy of localization), and second, its analyses are mapped to the patient’s MRI, providing a technique called magnetic source imaging (MSI). MSI results are therefore generally interpretable in terms of centimeter- and millimeter-scale individual anatomy, as opposed to the lobar or sublobar localization provided by routine scalp EEG [8•].
The American Clinical MEG Society (ACMEGS) has published multiple documents, including clinical practice guidelines, outlining the use of MEG for epilepsy presurgical evaluations, including specific clinical scenarios in which MEG is recommended [9,10,11,12]. In 2020 ACMEGs published a series of review articles exploring various aspects of clinical MEG and we have drawn on five of these extensively for the current paper [13,14,15,16,17]. For an article-length overview of clinical MEG practice, the reader is referred to Laohathai et al. [18•].
MEG and Surgical Outcomes
Research validating MEG for epilepsy evaluations focuses on comparing the MEG IZ against various other zones, some of which have been mentioned above. The most common comparator zone is the EZ; as mentioned, this can only be measured with a surgical intervention, and specifically one that has succeeded. Comparing the MEG IZ with the EZ therefore involves comparing the IZ as estimated by MEG to the volume of resected brain, and categorizing the surgical intervention as concordant or discordant with the MEG IZ. For a given series of patients, a confusion matrix can then be constructed, with which the performance of MEG concordance with resection as a predictor may be judged. In this analysis, a patient with concordant MEG and resection with a positive surgical outcome would be coded as a “true positive,” for example, and a patient with discordant MEG and resection with a poor surgical outcome would be coded as a “true negative.” Studies in the early 2000s, such as Fischer et al. [19], found that concordance between MEG and surgical resection was a significant predictor of positive surgical outcome, and this has largely been borne out by subsequent publications.
Mouthaan et al.[20•]. performed a meta-analysis of eight MSI and three electrographic source imaging (ESI) studies published between 2005 and 2016, that reported results with concordance of each to resection with respect to surgical outcome. Of the eight MEG papers, seven [21,22,23,24,25,26,27] reported that concordance with resection was a significant predictor of surgical outcome and one [28] did not. The aggregated MEG data indicated that concordance with surgical resection was a significant predictor of surgical outcome (odds ratio = 4.7), with a sensitivity of 83% and specificity of 22%. Concordance of MSI and concordance of ESI with surgical resection were not found to differ significantly with respect to predicting surgical outcome. Several studies [29, 30•, 31, 32, 33•] published since the Mouthaan review also reported MEG IZ-resection concordance to be a significant predictor of surgical outcome.
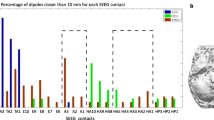
The next most common comparator zone is the intracranial ictal onset zone (IIOZ); this corresponds to the brain volume capable of creating seizures recorded with intracerebral or subdural electrodes. Papers emphasizing this comparison [34] note that there is a significant selection bias implicit in using the EZ as a comparator. Specifically, this restricts the analysis to a segment of the population able to undergo resection. We reviewed twelve papers that reported this comparison. Of these, seven [24, 26, 29, 31, 35,36,37] examined whether MEG IZ-IIOZ concordance was predictive of surgical outcome, and all found that it did. For the remaining papers, MEG IZ-IIOZ concordance was either an additional finding in a study reporting an EZ comparison [25, 33•, 38•], or part of a study aiming to identify specific MEG characteristics predictive of either the EZ or the IIOZ [34, 39•]. Predictive characteristics evaluated include measures of dipole clustering [33•, 34] and the timepoint chosen for dipole modeling [39•], and these features were found to be significant predictors of the specified zone.
The other main question in MEG literature pertinent to surgical outcome asks, with what frequency do MEG findings change surgical management? Two approaches have been used to answer this. The first is, given a cohort that has undergone both EEG and MEG, to scrutinize the subset for whom the basic workup with scalp EEG has been non-localizing, and ask how many of them had localizing findings on MEG. This fraction can be termed the “diagnostic gain” from MEG. Reported diagnostic gains from MEG are variable; early studies reported diagnostic gains of between 35 and 63% [40,41,42,43]. More recent work reported more modest (and consistent) gains of 16.8% [44] and 18% [45]. The second, and more arduous approach, is to modify the presurgical planning conference procedure and institute a multi-step presentation: first formulate a plan based on all non-MEG modalities, then review the MEG results, and finally note how often the plan changes based on those results. Changes in plan include added or changed location of implanted electrodes, as well as skipping phase 2 evaluation for resection or for no intervention. An early study with this design [46] reported that MEG changed the surgical plan in 33% of cases; more recent studies [47, 48] reported frequencies of 33% and 57%, respectively.
Though MEG has been shown to be a good predictor of surgical success, this should not be construed as a measurement of its localization accuracy. There are many factors that determine a good surgical outcome, in addition to MEG source location. It must be remembered that MEG localizes, in most instances, interictal sources and not seizure origins (i.e., the IZ and not the IOZ). As mentioned above, the IZ is an imperfect estimator of the EZ. Accordingly, that a patient continues to have seizures after resection does not mean that the interictal spike source was mislocated. A better question to ask, in terms of localization accuracy, would be whether the same spike persists after surgery.
MEG Methods for Mapping the Irritative Zone: Solutions to the Inverse Problem
Whole head MEG instrumentation became available in the late 1990’s, making it possible to view the entire distribution of magnetic fields associated with an epileptiform event. Typically the epileptologist would identify candidate waveforms in the simultaneously acquired EEG and then look at contour plots (iso-field lines) of the MEG amplitudes at the same time point. Depending on the sensor coil configuration a focal event might display as a single high intensity region (transverse gradient) or a small zero field region with extrema on either side (axial gradient). In either case a rough estimate of the source location could be determined visually. A better estimate of the three dimensional location of the source may be obtained by modeling the observed activity with that produced by a suitable current geometry in a volume conductor and then changing model parameters to minimize the differences between the measurements and the model values. This is process is referred to as solving the inverse problem. It is unfortunately an ill-posed problem with non-unique solutions that requires some level of a priori information and investigator input.
Early modeling work in biomagnetism involved the equivalent current dipole (ECD) in an infinite conductive half space or cylinder. Baule and McFee [49] noted that for axially symmetric volumes, including spheres, a dipole at the center as well as radially oriented dipoles would not produce an external magnetic field. This result was also described by Grynszpan and Geselowitz in a 1973 paper [50]. They further noted that for tangentially oriented dipoles, the external field is unchanged by the presence of concentric inhomogeneities such as shells of differing conductivity or even spherical holes removed from the center. Cohen and Hosaka [51] treated the model as being composed of two currents; that of the dipole itself, and the so-called “volume return currents” or just “volume currents.” They observed that if only radial fields are being measured, the contribution of the volume currents can be ignored as only the tangential field components will be nonzero. In the later 1970’s, Cuffin and Cohen [52, 53] made several studies of modeling error due to deviations from sphericity in the volume conductor and also whether a single point source dipole could serve as an equivalent when there were more dipoles some distance apart. Their results for prolate spheroids suggested that for radial measurements near the source dipole the volume current contributions could still be neglected, and for oblate spheroids the radial field components were small everywhere compared to those produced by the dipole itself. The case for more distributed sources (in this case aligned dipoles) were not as encouraging, as the field distribution will still appear quite similar to that of a single equivalent dipole but the model will produce significant errors, especially in depth, if only one dipole is employed.
By the end of the 1980’s, the single ECD (SECD) in a homogeneous conductive sphere had become the standard forward solution for use with magnetic field measurements that arose from a patch of active cortex, e.g., a focal epileptic source. The solution in Cartesian coordinates published by Sarvas in 1987 [54] combined with the Marquardt algorithm [55] to minimize the error between the measured and calculated values is the most common source localization method used with MEG for epilepsy [9, 56]. Alternate models attempt to improve on the volume conductor by incorporating MRI data to utilize a realistic head shape rather than a simple sphere and then use the boundary element method (BEM) to solve the forward problem [57]. To overcome the limitations of an SECD, multiple dipoles [58, 59] or distributed currents [7] as in the minimum norm estimates (MNE) are employed, especially when the recorded field pattern is more diffuse. In 1997, Van Veen [60] applied the beamformer method to EEG and MEG data using a grid constructed in the brain space with dipole sources evaluated at each grid node. The algorithm minimizes the dipole moment co-variance matrix at each location to determine likely contributors. This spatial filtering technique does not require knowledge of the number of dipoles nor of their locations in advance. It creates a grid of potential source currents within the brain, the nodes of which are often referred to as ‘virtual sensors’ as if there were electrodes at each grid location. As of 2023, ECD analysis is dominant in clinical MEG practice and is endorsed by ACMEGS, with use of other analyses recommended only in a supplementary fashion [9, 13].
The field of source modeling is too broad for a comprehensive review in this section, and we refer the reader to Tenney et al.[13]. for a good overview of the various methods in use beyond the SECD. We will focus the remaining discussion on significant work since that review. Recent efforts to improve modeling for MEG in general and for epilepsy in particular often focus on removing investigator/physician bias and automating the process as much as possible. Many reports from the last five years or so use the beamformer approach in conjunction with other signal processing or statistical methods, and we will here present some of the more significant recent papers based on this analysis.
Shibata et al. [61] used a beamformer to create voxel sources for interictal events and then measured the duration that the individual currents exceeded predefined threshold values. These sources were then randomly resampled and those that were reproducible were defined to represent temporal spread images (TSI) which were determined to be as accurate as the ECD models with the same data sets. Wilenius et al. [62] used a beamformer to evaluate 17 parietal lobe epilepsy patients and applied a kurtosis metric to automatically detect spike activity in the virtual sensors. They report that there were no significant differences between the locations determined using this method and those determined using the standard ECD model. Another paper describing kurtosis applied to beamformed data [63] found retrospectively that kurtosis used to identify spike activity in 3-min segments of beamformed MEG data was concordant with overlap relative to the resected region in 5 out 8 patients with Engel 1 surgical outcomes and concordant at the lobar level for the remaining 3. Another retrospective study of 28 pediatric patients [64] employed beamforming and bandpass (80–200 Hz) filter-based ripple detection to examine ripple propagation from the virtual sensors and compared the detected locations with those obtained from intracranial EEG. In 27 cases, there were no significant distance errors for either the ripple zone or the propagation onset locations between the two estimates. Another pediatric retrospective study [65] used a beamformer on 10-min segments of MEG in 30 patients (35 hippocampi) to estimate virtual sensor activity in the hippocampus; stereotactic EEG (SEEG) was available for comparison. Nineteen of these deep sources showed epileptiform activity in the MEG determined virtual sensors in agreement with the SEEG. The authors suggest that the observance of epileptic activity in virtual sensors may help to guide the placement of SEEG electrodes for these deep structures.
A particularly useful study [66•] comparing activity estimated from beamformed MEG virtual sensors with that recorded simultaneously from SEEG electrodes used independent component analysis (ICA) to identify those virtual sensors with maximal activity. For most of the patients (9/12) where the activity was reasonably confined, i.e., not broadly spread in both time and space, there was good agreement between the two measuring modalities, especially when a zero-lag condition was evaluated. The virtual sensor ICA determined time series were well correlated with the adjacent SEEG electrodes (ρ = 0.27– − 0.57) and were located within 20 mm of same. Interestingly, virtual sensor depth was not a limiting factor suggesting that this combination of techniques may be complementary in that regard although the authors caution that their MEG system has magnetometers rather than the more common gradiometers whose sensitivity drops off more rapidly as source depth increases. A follow-up study from this same group [67] used some of the same MEG/SEEG data as well as simulated data to compare the ICA and beamformer methods with regard to network dynamics. In this case, ICA was used to compute sources from the MEG data and then the ECD model was used to localize these sources. The beamformer was applied (without ICA) and a kurtosis-based detector was used to identify interictal epileptiform discharges. Correlations between the two methods and the SEEG data were then used to compare performance which indicated that the ICA method had the greater correlation with SEEG time series but the beamformer had better spatial localization for the simulated data but more similar results with respect to the patient data. The authors concluded that neither method by itself was clearly better, but the combination represented a useful complementarity.
While beamformers are seeing greater and greater application in epilepsy modeling, other methods remain in use or are seeing new implementations. A Bayesian multiple dipole method (SESAME) was recently compared [68] with the standard ECD model as well as RAP-MUSIC and a depth weighted minimum norm (wMNE) distributed source model. This iterative method normally increases the dipole count as iterations increase but in this study the model was terminated at the last iteration employing a single dipole. The ECD model as usual required an expert user, but the other three models are all at least semi-automated. Using the ECD results as the baseline the investigators found that for 22 patients, the SESAME process had a median Euclidean distance difference of 9 mm, while RAP-MUSIC was 11 mm, and wMNE was 16 mm. They concluded that these automated, less subjective methods were at least feasible with regard to replacing the need for both time and expertise in modeling epilepsy data.
Long-range temporal correlations (LRTCs) in the brain are thought to be modulated by the ratio of neuronal excitation to inhibition and may be estimated by calculating detrended fluctuation analysis (DFA) scaling exponents. Auno and colleagues [69] used DFA to evaluate interictal MEG recordings in patients with parietal lobe epilepsy. They used MRI data to create 200 brain parcels and sLORETA to estimate average time series in each parcel. The parcel time series were then used to compute DFA exponents which were then projected back onto the MR images. The largest exponents were assumed to be correlated with increased excitability or epileptiform activity and these parcel centroid locations were compared to previously determined ECD locations as well as resection regions. Results were significant only for those patients with type II focal cortical displasia, but the authors concluded that this method may be helpful in localizing the epileptogenic zone using spontaneous MEG.
The modeling methods so far described do not explicitly offer an estimate of the extent of the epileptogenic region. An effort to address this called fast spatiotemporal iteratively reweighted edge sparsity minimization (FAST-IRES) has recently been used with MEG data (Jiang et al. 2022) [70•]. Using both simulated and clinical data (8 patients), the algorithm performed well with cortical sources. Intracranial EEG recordings were used to identify seizure onset zone (SOZ) electrodes whose location and extent were then compared to the FAST-IRES estimates. The average location error was 17 mm and the average spatial dispersion (weighted sum of minimum distances between SOZ electrodes and each point in the FAST-IRES solution) was 21.3 mm. This improved to 15.5 and 20.8 mm for the six patients who had post-surgical Engel I outcomes. A method for objectively defining MEG data as containing interictal activity has been described by Fujita et al. [71]. The primary purpose of this work was to enlist phase amplitude coupling (PAC) metrics to improve the automated diagnosis of epilepsy. Resting state MEG was divided into 2.4-s epochs and cortical current estimates were calculated for delta, theta, alpha, beta, low gamma and high gamma frequency bands. Eight PAC values were estimated by computing the ratio of the phase in the four lower bands relative to the amplitudes in the two gamma bands. Ninety patients and ninety control subjects were evaluated using a shallow neural network (SNN) and a deep convolutional neural network (DCNN), both methods augmented with the PAC values in addition to previously used power and functional connectivity measures which had successfully discriminated patients from controls. The addition of the PACs significantly improved the DCNN discrimination to 90%. The study did not address the specific role that the PACs might have but the authors note that previous work has identified abnormal PACs in the SOZ [72] and that while not significant, the theta/low gamma and theta/high gamma PAC values were higher in the patient group suggesting that this measure may have some value in defining the SOZ using interictal MEG.
The ill-posed nature of the MEG inverse problem and the non-unique solutions remain as challenges for epilepsy mapping that generally require additional information and physician input. However, the increasing performance of deep learning methods and artificial intelligence coupled with the availability of large data sets hold the promise of future improvements in accuracy and automated processing.
MEG and HFOs
Special claims have been made with respect to epileptiform high-frequency activity (HFA). Epileptiform HFA has two basic forms. The first is as an electrographic seizure onset feature, in which case “fast” is typically defined as beta range and higher (> 12 Hz), and the second is as a discrete burst (high-frequency oscillation, HFO) that may occur either during a seizure or interictally, in which case “fast” is defined as high gamma range and above (> 80 Hz). Intracranial seizure onset HFA indicates that the IOZ has been particularly well localized [73], and its presence predicts superior outcomes [74]. HFOs, in turn, are split, according to frequency, into ripples (80–250 Hz) and fast ripples (> 250 Hz). Whereas ripples are often physiologic and are implicated specifically in information processing and memory consolidation [75], fast ripples are rarely physiologic [76]. Animal studies indicate that HFOs reflect the activation of small neural populations, on the order of 1–5 mm in diameter [77, 78], much smaller than the several square centimeters known to be activated for a spike detected on scalp EEG [79]. This motivates the main claim for HFOs that they are more anatomically constrained and, therefore, are more specific, estimators of the EZ. Indeed, an influential early study found that resection of intracranial HFOs was predictive of superior surgical outcome, but resection of intracranial spikes was not [80]. Subsequent studies have had more equivocal results [81, 82].
These latter results notwithstanding, much work has been done to develop noninvasive methods for recording and localizing HFOs. Work over the last 10 years has demonstrated that this is feasible with MEG, but this work has had to contend with two fundamental challenges: distinguishing physiologic from pathologic HFOs (low specificity), and detecting HFOs despite their low signal- to-noise ratio (SNR; low sensitivity). The first problem is particularly acute, as work on noninvasive HFOs has focused on ripples, and not the more pathological fast ripples; it appears this is due to concerns that fast ripples are too focal to be detected non-invasively [83]. We reviewed seventeen papers for this section (references 64 and 84–100); all but Velmurungan et al.[84]. analyzed interictal HFOs. Interestingly, only seven of the papers [85,86,87,88,89,90,91] directly controlled for this confound. The most common strategy was to use only HFOs coinciding with epileptiform discharges, but Xiang et al. [90, 91]. utilized kurtosis and skewness (statistical properties of the MEG signal) to identify pathologic HFOs. A proposed third approach [76], to compare observed ripple rates with a “physiologic HFO atlas” based on documented normal brain tissue, has yet to be adopted in a MEG HFO study. To solve the SNR issue, most groups [64, 86, 89, 90, 92,93,94,95,96,97,98] use an automated HFO detector, with or without verification by an expert reviewer. Low SNR motivated all groups to use an inverse solution other than ECD for localization. Beamformer analyses were utilized most frequently [64, 84, 85, 87, 88, 90, 92, 95, 98, 99], followed by wavelet maximum entropy on the mean (wMEM) [86, 89, 94, 96] and accumulated source imaging [90, 97, 100].
The substantive clinical questions for MEG HFOs are analogous to those discussed for conventional interictal discharges. Two specific questions arise: 1) is the MEG HFO zone (MHZ) a superior estimator of the EZ and 2) in com- parison to scalp EEG, is it a superior estimator of the intracranial HFO zone? Eight of the papers reviewed [64, 84, 88, 89, 95, 98,99,100] reported surgical outcome as a function of MHZ resection. For three papers [84, 95, 98], the utility of MHZ resection was reported only qualitatively and without comparator, and all 3 reported that MHZ resection was consistent with good outcome, but do not support stronger or more specific conclusions. The remaining papers compared MHZ resection with resection of some other zone, e.g., scalp EEG HFO zone [99], MEG IZ [64, 100], zones oscillating in other frequency bands [88], zones including HFO propagation [64], or zones with HFOs not coinciding with spikes [89]. All of these studies reported significant superiority of MHZ resection as a predictor of surgical outcome with respect to the comparator.
Five papers [64, 89, 94, 96, 99] compared the HFO zones detected by MEG and scalp EEG with intracranial findings. For two papers [94, 96], the intracranial zone was not the HFO zone but a hybrid zone “region of interest” (ROI) comprising neuroimaging abnormalities and IEEG seizure onsets, among others. These studies both reported lower sensitivity but higher specificity for MEG in detecting the ROI. Of the remaining three, two [64, 96] reported good concordance between MEG and HD-EEG HFO zones and the intracranial HFO zone, without a significant difference between the two. Tamilia et al. [89], by contrast, found that the MHZ (as defined by ripples on spikes) was more specific than the scalp HFO zone for identifying the intracranial HFO zone.
In summary, as of 2023, considerable work has been done to demonstrate the feasibility of recording HFOs on MEG, but HFO analysis remains highly heterogeneous in methodology, and the question of the added value of HFOs in presurgical workup remains open.
MEG for Functional Mapping
The discussion to this point has focused on MEG applications in developing the surgical hypothesis, specifically, elucidating the IZ and EZ for the purpose of ablation or modulation of the latter. A standard presurgical evaluation, however, includes not only designation of areas to be targeted for treatment, but also designation of eloquent areas that could adjoin or overlap with those targeted areas [101]. Functional mapping, i.e., localization of neurologic function via neurophysiology or neuroimaging, is done to assess the risks associated with an ablative procedure, whenever the hypothesized EZ is thought to adjoin or overlap eloquent cortex. Sensorimotor mapping is indicated for cases with hypotheses near the central sulcus, visual mapping for hypotheses near occipital cortex, auditory mapping for hypotheses near Heschl’s gyrus, memory mapping for hypotheses near the mesial temporal lobe, and language mapping for hypotheses near the dominant frontal or temporal lobes [10, 102].
Functional mapping can be either invasive or noninvasive. Invasive functional mapping is typically done via direct cortical stimulation, either intraoperatively, or at the bedside, in patients with implanted electrodes; the intracarotid amobarbital (Wada) test (IAT) is the main non-electrical invasive functional testing modality. With invasive mapping, the location of the intervention is taken to be well-localized, i.e., its location is known to the clinician with high confidence. For electrical stimulation, not only is the intervention well-localized, but it is also anatomically precise, i.e., the stimulation delivered affects only a small volume of brain. Because of these considerations, the invasive modalities are generally regarded as the gold standard [103]; work over the last two decades scrutinizing the predictive value of these tests has, however, raised questions regarding whether this status is merited [103,104,105]. The primary drawback of the invasive tests is, not surprisingly, their invasive nature, which reduces their accessibility and necessarily involves some morbidity [106, 107]. Significant work, therefore, has gone into developing noninvasive modalities for functional mapping, and evaluating their performance in comparison to the invasive ones.
Noninvasive modalities for functional mapping include MEG, functional magnetic resonance imaging (fMRI), single-photon emission computed tomography (SPECT), positron emission tomography (PET), and transcranial magnetic stimulation (TMS) [101, 103]. Because of its relative accessibility, integration with the structural information provided by diffusion tensor imaging, and independence of both ionizing radiation and radioligands, fMRI has become the most widely-used noninvasive modality for presurgical functional mapping [108]. MEG has two advantages that motivate its use in functional mapping. The first is its independence of neurovascular coupling. The blood oxygenation level-dependent (BOLD) signal, upon which fMRI is based, is known to be altered in hyper- or hypovascular lesions, and therefore, functional mapping in tumor cases is susceptible to both false positives and false negatives [109]; for tumor cases, therefore, MEG mapping may be superior. Secondly, as noted, has superior time resolution that allows deeper characterization of dynamic processes characteristic of higher cognitive function. Processes such as language and memory, in particular, for which function depends on the dynamic interaction among several networked nodes [110], will likely benefit from the deeper characterization MEG allows [14].
ACMEGs has published statements endorsing the use of MEG for presurgical functional mapping and detailing its indications [10, 111], and in 2020 published a series of review articles on the main modalities: somatosensory [15], visual [16], auditory [17], and language [14] evoked fields. These and the comprehensive review by Kreidenhuber et al. [102] remain authoritative and are detailed beyond the scope possible here, so the remaining discussion will focus on work since their publication.
Because of the dominance of the IAT for language lateralization and the interest in supplanting it with a non-invasive alternative, language mapping has been the most active domain for MEG functional mapping work. Bowyer et al.[14]. review several studies establishing good concordance between MEG functional mapping results and the IAT. A significant challenge has been that the main inverse solution, the SECD, is likely ill-suited for characterizing language, which is known to be implemented by a network of brain regions [14]. Recent work has therefore focused on developing alternate inverse solutions appropriate for language mapping. Two groups have implemented methods based on mapping task-related beta-frequency changes [112, 113], another implemented a modified SECD methodology [114], and a third used a graph-theoretic approach [115]. At this time, no methodology has replaced the SECD for language mapping, however.
The Advent of Optically Pumped Magnetometry
For more than thirty years, conventional clinical MEG instrumentation has been based on sensors utilizing superconducting quantum interference devices (SQUIDs) [7]. Because SQUIDs depend on superconductivity to sense magnetic fields, they operate only at exceedingly low temperatures and must be housed in a liquid helium dewar. This arrangement imposes two limitations on SQUID-based MEG. The first is the dewar distances the sensors from the scalp and brain, which necessarily decreases the amplitude of the magnetic signal recorded [116]. Lower amplitude, in turn, reduces the device’s sensitivity. Secondly, the SQUID instrumentation requires that the sensor array be housed in a rigid, fixed structure that requires that the patient lie still for the duration of the study. This necessarily imposes a limit on the duration of studies possible with SQUID MEG systems. Over the last 5 years, however, clinical systems utilizing sensors based on optically-pumped magnetometry (OPM) have become available [117, 118•, 119]; see Tierney et al. [116]. for a synopsis of the underlying physics. OPM sensors operate at room temperature and therefore do not require a rigid dewar housing. Because of this, the sensors are closer to the scalp, offering higher signal amplitudes, and can be assembled into helmets that can move with the patient. In principle, this may allow significantly longer MEG studies, greatly increasing the chances for ictal recordings [117, 119]. Individual magnetometers can even be used intra-orally to record from deep structures [120]. Another advantage of OPM systems pertains to cost. SQUID-based MEG facilities typically have liquid Helium supply as a significant component of their operating costs, and there have been significant disruptions to this supply in 2022–2023 [121, 122]; the authors are aware of at least one US MEG center that was forced to suspend operation temporarily in 2022 due to insufficient helium supply. In summary, the prospect of room-temperature on-scalp MEG with OPM raises hopes for improved studies, due to increased duration and decreased sensor distance from scalp, as well as increased accessibility of MEG due to reduced cost.
Conclusions
Because it has anatomic sensitivity that is complementary to that of EEG, and due to the methodology of MSI, MEG is an important noninvasive tool in building a surgical hypothesis for cases of refractory focal epilepsy. It is additionally established as a tool in evaluating eloquent brain areas via measurement and localization of evoked fields. Work continues in the refinement of new algorithms for solving the inverse problem, and the development of new room temperature magnetometers based on OPM raises the prospects for longer studies and increased availability of MEG.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Carreno M, Lüders HO. Chap. 47: General principles of presurgical evaluation. In: Lüders HO, editor. Textbook of epilepsy surgery. 2008. p. 409–22.
Ebersole JS, Ebersole SM. Combining MEG and EEG source modeling in epilepsy evaluations. J Clin Neurophysiol. 2010;27:360–71. https://doi.org/10.1097/WNP.0b013e318201ffc4.
Piastra MC, Nu¨ßing A, Vorwerk J, Clerc M, Engwer C, Wolters CH. A comprehensive study on electroencephalography and magnetoencephalography sensitivity to cortical and subcortical sources. Hum Brain Mapp. 2021;42:978–92. https://doi.org/10.1002/hbm.25272. A detailed modeling study comparing relative sensitivities of EEG and MEG for different brain regions. EEG was found to more sensitive for radial and deep sources, and MEG more sensitive for tangential sources.
Mikuni N, Nagamine T, Ikeda A, Terada K, Taki W, Kimura J, Kikuchi H, Shibasaki H. Simultaneous recording of epileptiform discharges by MEG and subdural electrodes in temporal lobe epilepsy. Neuroimage. 1997;5:298–306. https://doi.org/10.1006/nimg.1997.0272.
Okada YC, Lahteenmäki A, Xu C. Experimental analysis of distortion of magnetoencephalography signals by the skull. Clin Neurophysiol. 1999;110:230–8. https://doi.org/10.1016/S0013-4694(98)00099-6.
Okada Y, Lahteenmaki A, Xu C. Comparison of MEG and EEG on the basis of somatic evoked responses elicited by stimulation of the snout in the juvenile swine. Clin Neurophysiol. 1999;110:214–29. https://doi.org/10.1016/S0013-4694(98)00111-4.
Hämäläinen MS, Hari R, Ilmoniemi RJ, Knuutila J, Lounasmaa OV. Magnetoencephalography—theory, instrumentation, and applications to noninvasive studies of the working human brain. Rev Mod Phys. 1993;65:413–515.
Tamilia E, AlHilani M, Tanaka N, Tsuboyama M, Peters JM, Grant PE, Madsen JR, Stufflebeam SM, Pearl PL, Papadelis C. Assessing the localization accuracy and clinical utility of electric and magnetic source imaging in children with epilepsy. Clin Neurophysiol. 2019;130:491–504. https://doi.org/10.1016/j.clinph.2019.01.009. A study comparing localization accuracy for EEG and MEG, utilizing intracranial EEG and resection as the ground truth. MEG was found to have smaller localization error than both conventional and high-density scalp EEG.
Bagić AI, Knowlton RC, Rose DF, Ebersole JS. American Clinical Magnetoencephalography Society clinical practice guideline 1: recording and analysis of spontaneous cerebral activity. J Clin Neurophysiol. 2011;0:1. https://doi.org/10.1097/WNP.0b013e3182272fed.
Burgess RC, Funke ME, Bowyer SM, Lewine JD, Kirsch HE, Bagić AI. American Clinical Magnetoencephalography Society clinical practice guideline 2: presurgical functional brain mapping using magnetic evoked fields. J Clin Neurophysiol. 2011;28:1. https://doi.org/10.1097/WNP.0b013e3182272ffe.
Bagić AI, Knowlton RC, Rose DF, Ebersole JS. American Clinical Magnetoencephalography Society clinical practice guideline 3. J Clin Neurophysiol. 2011;0:1. https://doi.org/10.1097/WNP.0b013e3182272fed.
Bagić AI, Knowlton RC, Rose DF, Ebersole JS. American Clinical Magnetoencephalography Society clinical practice guideline 4. J Clin Neurophysiol. 2011;0:1. https://doi.org/10.1097/WNP.0b013e3182272fed.
Tenney JR, Fujiwara H, Rose DF. The value of source localization for clinical magnetoencephalography: beyond the equivalent current dipole. J Clin Neurophysiol. 2020;37:537–44. https://doi.org/10.1097/WNP.0000000000000487.
Bowyer SM, Zillgitt AJ, Greenwald M, Lajiness-O’Neill R. Language mapping with magnetoencephalography: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:554–63. https://doi.org/10.1097/WNP.0000000000000489.
De Tiège X, Bourguignon M, Piitulainen H, Jousmäki V. Sensorimotor mapping with MEG: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:564–73. https://doi.org/10.1097/WNP.0000000000000481.
Zillgitt AJ, Barkley GL, Bowyer SM. Visual mapping with magnetoencephalography: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:585–91. https://doi.org/10.1097/WNP.0000000000000483.
Shvarts V, Mäkelä JP. Auditory mapping with MEG: an update on the current state of clinical research and practice with considerations for clinical practice guidelines. J Clin Neurophysiol. 2020;37:574–84. https://doi.org/10.1097/WNP.0000000000000518.
Laohathai C, Ebersole JS, Mosher JC, Bagić AI, Sumida A, Von Allmen G, Funke ME. Practical fundamentals of clinical MEG interpretation in epilepsy. Front Neurol. 2021;12:1–22. https://doi.org/10.3389/fneur.2021.722986. An excellent overview of clinical MEG as used for epilepsy.
Fischer MJ, Scheler G, Stefan H. Utilization of magnetoencephalography results to obtain favourable outcomes in epilepsy surgery. Brain. 2005;128:153–7. https://doi.org/10.1093/brain/awh333.
Mouthaan BE, Rados M, Boon PAJM, Carrette E, Diehl B, Jung J, Kimiskidis VK, Kobulashvili T, Kuchukhidze G, Larsson PG, Leitinger M, Ryvlin P, Rugg-Gunn F, Seeck M, Vulli’emoz S, Huiskamp G, Lei-jten FSS, Van Eijsden P, Trinka E, Braun KPJ. Diagnostic accuracy of interictal source imaging in presurgical epilepsy evaluation: a systematic review from the E-PILEPSY consortium. Clin Neurophysiol. 2019;130:845–55. https://doi.org/10.1016/j.clinph.2018.12.016. A meta-analysis of several studies comparing the relative contributions of EEG and MEG to epilepsy presurgical evaluation. No statistical difference was found between the contributions of the two modalities.
Papanicolaou AC, Pataraia E, Billingsley-Marshall RL, Castillo EM, Wheless JW, Swank P, Breier JI, Sarkari S, Simos PG. Toward the substitution of invasive electroencephalography in epilepsy surgery. J Clin Neurophysiol. 2005;22:231–7. https://doi.org/10.1097/01.WNP.0000172255.62072.E8.
Knowlton RC, Elgavish RA, Bartolucci A, Ojha B, Limdi N, Blount J, Burneo JG, Ver Hoef L, Paige L, Faught E, Kankirawatana P, Riley K, Kuzniecky R. Functional imaging: II. Prediction of epilepsy surgery outcome. Ann Neurol. 2008;64:35–41. https://doi.org/10.1002/ana.21419.
Jeong W, Chung CK, Kim JS. Magnetoencephalography interictal spike clustering in relation with surgical outcome of cortical dysplasia. J Korean Neurosurg Soc. 2012;52:466–71. https://doi.org/10.3340/jkns.2012.52.5.466.
Schneider F, Irene Wang Z, Alexopoulos AV, Almubarak S, Kakisaka Y, Jin K, Nair D, Mosher JC, Najm IM, Burgess RC. Magnetic source imaging and ictal SPECT in MRI-negative neocortical epilepsies: additional value and comparison with intracranial EEG. Epilepsia. 2013;54:359–69. https://doi.org/10.1111/epi.12004.
Wilenius J, Medvedovsky M, Gaily E, Metsähonkala L, Mäkelä JP, Pae-tau A, Valanne L, Paetau R. Interictal MEG reveals focal cortical dysplasias: special focus on patients with no visible MRI lesions. Epilepsy Res. 2013;105:337–48. https://doi.org/10.1016/j.eplepsyres.2013.02.023.
Almubarak S, Alexopoulos A, Von-Podewils F, Wang ZI, Kakisaka Y, Mosher JC, Bulacio J, González-Martínez J, Bingaman W, Burgess RC. The correlation of magnetoencephalography to intracranial EEG in localizing the epileptogenic zone: a study of the surgical resection outcome. Epilepsy Res. 2014;108:1581–90. https://doi.org/10.1016/j.eplepsyres.2014.08.016.
Mu J, Rampp S, Carrette E, Roessler K, Sommer B, Schmitt FC, De Tiège X, Hamer HM, Boon PAJM, Pauli E, Blümcke I, Zhou D, Buchfelder M, Stefan H. Clinical relevance of source location in frontal lobe epilepsy and prediction of postoperative long-term outcome. Seizure. 2014;23:553–9. https://doi.org/10.1016/j.seizure.2014.04.006.
Kim H, Kankirawatana P, Killen J, Harrison A, Oh A, Rozzelle C, Blount J, Knowlton R. Magnetic source imaging (MSI) in children with neocortical epilepsy: surgical outcome association with 3D post-resection analysis. Epilepsy Res. 2013;106:164–72. https://doi.org/10.1016/j.eplepsyres.2013.04.004.
Murakami H, Wang ZI, Marashly A, Krishnan B, Prayson RA, Kakisaka Y, Mosher JC, Bulacio J, Gonzalez-Martinez JA, Bingaman WE, Najm IM, Burgess RC, Alexopoulos AV. Correlating magnetoencephalography to stereo-electroencephalography in patients undergoing epilepsy surgery. Brain a J Neurol. 2016;139:2935–47. https://doi.org/10.1093/brain/aww215.
Rampp S, Stefan H, Wu X, Kaltenhauser M, Maess B, Schmitt FC, Wolters CH, Hamer HM, Kasper BS, Schwab S, Doerfler A, Blumcke I, Rössler K, Buchfelder M. Magnetoencephalography for epileptic focus localization in a series of 1000 cases. Brain. 2019;142:3059–71. https://doi.org/10.1093/brain/awz231. A detailed retrospective study of a large cohort of patients who underwent MEG and epilepsy surgery. Extent of resection of MEG IZ was a postive prognostic factor.
He X, Zhou J, Teng P, Wang X, Guan Y, Zhai F, Li T, Luan G. The impact of MEG results on surgical outcomes in patients with drug-resistant epilepsy associated with focal encephalomalacia: a single-center experience. J Neurol. 2020;267:812–22. https://doi.org/10.1007/s00415-019-09638-w.
Chourasia N, Quach M, Gavvala J. Insular Magnetoencephalography dipole clusters in patients with refractory focal epilepsy. J Clin Neurophysiol. 2021;38:542–6. https://doi.org/10.1097/WNP.0000000000000718.
Ntolkeras G, Tamilia E, AlHilani M, Bolton J, Ellen Grant P, Prabhu SP, Madsen JR, Stufflebeam SM, Pearl PL, Papadelis C. Presurgical accuracy of dipole clustering in MRI-negative pediatric patients with epilepsy: validation against intracranial EEG and resection. Clin Neurophysiol. 2022;141:126–38. https://doi.org/10.1016/j.clinph.2021.01.036. This retrospective study evaluated dipole clustering for conventional and high-density scalp EEG as well as MEG. Dipole clustering was found to be a positive prognostic factor for surgical outcome.
Anand A, Magnotti JF, Smith DN, Gadot R, Najera RA, Hegazy MI, Gavvala JR, Shofty B, Sheth SA. Predictive value of magnetoencephalography in guiding the intracranial implant strategy for intractable epilepsy. J Neurosurg. 2022;137:1237–47. https://doi.org/10.3171/2022.1.JNS212943.
Oishi M, Kameyama S, Masuda H, Tohyama J, Kanazawa O, Sasagawa M, Otsubo H. Single and multiple clusters of magnetoencephalographic dipoles in neocortical epilepsy: significance in characterizing the epileptogenic zone. Epilepsia. 2006;47:355–64. https://doi.org/10.1111/j.1528-1167.2006.00428.x.
Englot DJ, Nagarajan SS, Imber BS, Raygor KP, Honma SM, Mizuiri D, Mantle M, Knowlton RC, Kirsch HE, Chang EF. Epileptogenic zone localization using magnetoencephalography predicts seizure freedom in epilepsy surgery. Epilepsia. 2015;56:949–58. https://doi.org/10.1111/epi.13002.
Zhang C, Liu W, Zhang J, Zhang X, Huang P, Sun B, Zhan S, Cao C. Utility of magnetoencephalography combined with stereo-electroencephalography in resective epilepsy surgery: a 2-year follow-up. Seizure. 2022;97:94–101. https://doi.org/10.1016/j.seizure.2022.03.013.
Duez L, Tankisi H, Hansen PO, Sidenius P, Sabers A, Pinborg LH, Fabricius M, Rubboli G, Pedersen B, Leffers AM, Uldall P, Jespersen B, Brennum J, Fuglsang-frederiksen A, Beniczky S. Electromagnetic source imaging in presurgical workup of patients with epilepsy. Neurology. 2019;92:e576–86. https://doi.org/10.1212/WNL.0000000000006877. A prospective study of combined EEG-MEG (EMSI) evaluating the consistency of localizations provided by different algorithms and across two popular software packages (Curry and BESA), as well as the diagnostic yield. EMSI was found to pro- vide new information in 34% of cases.
Plummer C, Vogrin SJ, Woods WP, Murphy MA, Cook MJ, Liley DTJ. Interictal and ictal source localization for epilepsy surgery using high-density EEG with MEG: a prospective long-term study. Brain. 2019;142:932–51. https://doi.org/10.1093/brain/awz015. A detailed retrospective study of patients who underwent both MEG and hd-EEG evaluating the localization accuracy of ECD solutions based on different latencies of the spike waveform, as validated against resection-based EZ. Earliest solutions were found to have greatest accuracy. MEG alone was not found to have superior localization accuracy.
Stefan H, Hummel C, Scheler G, Genow A, Druschky K, Tilz C, Kaltenhäuser M, Hopfengärtner R, Buchfelder M, Romstöck J. Magnetic brain source imaging of focal epileptic activity: a synopsis of 455 cases. Brain. 2003;126:2396–405. https://doi.org/10.1093/brain/awg239.
Pataraia E, Simos PG, Castillo EM, Billingsley-Marshall RL, Sarkari S, Wheless JW, Maggio V, Maggio W, Baumgartner JE, Swank PR, Breier JI, Papanicolaou AC. Does magnetoencephalography add to scalp video-EEG as a diagnostic tool in epilepsy surgery? Neurology. 2004;62:943–8. https://doi.org/10.1212/WNL.63.10.1987.
Paulini A, Fischer M, Rampp S, Scheler G, Hopfengärtner R, Kaltenhäuser M, Dörfler A, Buchfelder M, Stefan H. Lobar localization information in epilepsy patients: MEG-A useful tool in routine presurgical diagnosis. Epilepsy Res. 2007;76:124–30. https://doi.org/10.1016/j.eplepsyres.2007.07.006.
Colon AJ, Ossenblok PP, Nieuwenhuis L, Stam KJ, Boon PAJM. Use of routine MEG in the primary diagnostic process of epilepsy. J Clin Neurophysiol. 2009;26:326–32. https://doi.org/10.1097/WNP.0b013e3181baabef.
Koster I, Ossenblok PP, Brekelmans GJ, van der Linden I, Hillebrand A, Wijnen BF, Colon AJ. Sensitivity of magnetoencephalography as a diagnostic tool for epilepsy: a prospective study. Epileptic Disord. 2020;22:264–72. https://doi.org/10.1684/epd.2020.1160.
Duez L, Beniczky S, Tankisi H, Hansen PO, Sidenius P, Sabers A, Fuglsang-Frederiksen A. Added diagnostic value of magnetoencephalography (MEG) in patients suspected for epilepsy, where previous, extensive EEG workup was unrevealing. Clin Neurophysiol. 2016;127:3301–5. https://doi.org/10.1016/j.clinph.2016.08.006.
Sutherling WW, Mamelak AN, Thyerlei D, Maleeva T, Minazad Y, Philpott L, Lopez N. Influence of magnetic source imaging for planning intracranial EEG in epilepsy. Neurology. 2008;71:990–6. https://doi.org/10.1212/01.wnl.0000326591.29858.1a.
Mohamed IS, Toffa DH, Robert M, Cossette P, Bérubé AA, Saint-Hilaire JM, Bouthillier A, Nguyen DK. Utility of magnetic source imaging in nonlesional focal epilepsy: a prospective study. Neurosurg Focus. 2020;48:1–11. https://doi.org/10.3171/2020.1.FOCUS19877.
Tripathi M, Kaur K, Ramanujam B, Viswanathan V, Bharti K, Singh G, Singh V, Garg A, Bal CS, Tripathi M, Sharma MC, Pandey R, Dash D, Mandal P, Chandra PS. Diagnostic added value of interictal magnetic source imaging in presurgical evaluation of persons with epilepsy: a prospective blinded study. Eur J Neurol. 2021;28:2940–51. https://doi.org/10.1111/ene.14935.
Baule G, McFee R. Theory of magnetic detection of the heart’s electrical activity. J Appl Phys. 1965;36:2066–73. https://doi.org/10.1063/1.1714404.
Grynszpan F, Geselowitz DB. Model studies of the magnetocardiogram. Biophys J. 1973;13:911–25. https://doi.org/10.1016/S0006-3495(73)86034-5.
Cohen D, Hosaka H. Part II magnetic field produced by a current dipole. J Electrocardiol. 1976;9:409–17. https://doi.org/10.1016/S0022-0736(76)80041-6.
Cuffin BN, Cohen D. Magnetic fields produced by models of biological current sources. J Appl Phys. 1977;48:3971–80. https://doi.org/10.1063/1.324230.
Cuffin BN, Cohen D. Magnetic fields of a dipole in special volume conductor shapes. IEEE Trans Biomed Eng. 1977;24:372–81.
Sarvas J. Basic mathematical and electromagnetic concepts of the biomagnetic inverse problem. Phys Med Biol. 1987;32:11–22. https://doi.org/10.1088/0031-9155/32/1/004.
Marquardt DW. An algorithm for least-squares estimation of non-linear parameters. J Soc Ind Appl Math. 1963;11:431–41.
Knowlton RC, Laxer KD, Aminoff MJ, Roberts TP, Wong ST, Row-ley HA. Magnetoencephalography in partial epilepsy: clinical yield and localization accuracy. Ann Neurol. 1997;42:622–31. https://doi.org/10.1002/ana.410420413.
de Munk JC. A linear discretization of the volume conductor bound- ary integral equation using analytically integrated elements. IEEE Trans Biomed Eng. 1992;39:986–90.
Scherg M, Hari R, Hämäläinen MS. Frequency-specific sources of the auditory N19-P30-P50 response detected by a multiple source analysis of evoked magnetic fields and potentials. In: Williamson SJ, Hoke M, Stroink G, Kotani M, editors. Advances in biomagnetism. Plenum; 1989. p. 97–100.
Mosher JC, Spencer ME, Leahy RM, Lewis PS. Error bounds for EEG and MEG dipole source localization. Electroencephalogr Clin Neurophysiol. 1993;86:303–21. https://doi.org/10.1016/0013-4694(93)90043-U.
Van Veen BD, Van Drongelen W, Yuchtman M, Suzuki A. Localization of brain electrical activity via linearly constrained minimum variance spatial filtering. IEEE Trans Biomed Eng. 1997;44:867–80. https://doi.org/10.1109/10.623056.
Shibata S, Matsuhashi M, Kunieda T, Yamao Y, Inano R, Kikuchi T, Imamura H, Takaya S, Matsumoto R, Ikeda A, Takahashi R, Mima T, Fukuyama H, Mikuni N, Miyamoto S. Magnetoencephalography with temporal spread imaging to visualize propagation of epileptic activity. Clin Neurophysiol. 2017;128:734–43. https://doi.org/10.1016/j.clinph.2017.01.010.
Wilenius J, Lauronen L, Kirveskari E, Gaily E, Metsähonkala L, Paetau R. Interictal magnetoencephalography in parietal lobe epilepsy – comparison of equivalent current dipole and beamformer (SAMepi) analysis. Clin Neurophysiol Pract. 2020;5:64–72. https://doi.org/10.1016/j.cnp.2020.02.003.
Li R, Plummer C, Vogrin SJ, Woods WP, Kuhlmann L, Boston RC, Liley DT, Cook MJ, Grayden DB. Interictal spike localization for epilepsy surgery using magnetoencephalography beamforming. Clin Neurophysiol. 2021;132:928–37. https://doi.org/10.1016/j.clinph.2020.12.019.
Tamilia E, Matarrese MAG, Ntolkeras G, Grant PE, Madsen JR, Stuffle-beam SM, Pearl PL, Papadelis C. Noninvasive mapping of ripple onset predicts outcome in epilepsy surgery. Ann Neurol. 2021;89:911–25. https://doi.org/10.1002/ana.26066.
Sidler E, Greiner H, Mangano FT, Skoch J, Arya R, Holland K, Aun-garoon G, Arthur TM, Fujiwara H, Horn PS, Tenney JR. Improving detection of hippocampal epileptiform activity using magnetoencephalography. J Clin Neurophysiol. 2022;39:240–6. https://doi.org/10.1097/WNP.0000000000000822.
Velmurugan J, Badier JM, Pizzo F, Medina Villalon S, Papageorgakis C, Lopez-Madrona V, Jegou A, Carron R, Bartolomei F, Benar CG. Virtual MEG sensors based on beamformer and independent component analysis can reconstruct epileptic activity as measured on simultaneous intracerebral recordings. Neuroimage. 2022;264:119681. https://doi.org/10.1016/j.neuroimage.2022.119681. This study and citation 67 report the results of simultaneous MEG and SEEG, which allows rare direct correlation between these modalities. Beamformer analysis of MEG allowed localization of hippocampal spikes, which is the subject of controversy.
Coelli S, Medina Villalon S, Bonini F, Velmurugan J, Lopez-Madrona VJ, Carron R, Bartolomei F, Badier JM, B’enar CG. Comparison of beamformer and ICA for dynamic connectivity analysis: a simultaneous MEG-SEEG study. Neuroimage. 2023;265:119806. https://doi.org/10.1016/j.neuroimage.2022.119806.
Luria G, Duran D, Visani E, Rossi Sebastiano D, Sorrentino A, Tassi L, Granvillano A, Franceschetti S, Panzica F. Towards the automatic localization of the irritative zone through magnetic source imaging. Brain Topogr. 2020;33:651–63. https://doi.org/10.1007/s10548-020-00789-y.
Auno S, Lauronen L, Wilenius J, Peltola M, Vanhatalo S, Palva JM. Detrended fluctuation analysis in the presurgical evaluation of parietal lobe epilepsy patients. Clin Neurophysiol. 2021;132:1515–25. https://doi.org/10.1016/j.clinph.2021.03.041.
Jiang X, Ye S, Sohrabpour A, Bagić AI, He B. Imaging the extent and location of spatiotemporally distributed epileptiform sources from MEG measurements. NeuroImage Clin. 2022;33:102903. https://doi.org/10.1016/j.nicl.2021.102903. The authors employ the FAST-IRES algorithm to define the spatial extent of the source of epileptiform discharges. This addresses a significant problem with the standard ECD analysis, which models epileptiform discharges via a point source, which is known to be non-physiologic.
Fujita Y, Yanagisawa T, Fukuma R, Ura N, Oshino S, Kishima H. Abnormal phase-amplitude coupling characterizes the interictal state in epilepsy. J Neural Eng. 2022;19:026056. https://doi.org/10.1088/1741-2552/ac64c4.
Edakawa K, Yanagisawa T, Kishima H, Fukuma R, Oshino S, Khoo HM, Kobayashi M, Tanaka M, Yoshimine T. Detection of epileptic seizures using phase-amplitude coupling in intracranial electroencephalography. Sci Rep. 2016;6:1–8. https://doi.org/10.1038/srep25422.
Bartolomei F, Chauvel P, Wendling F, Timone D, Clinique SDN, Saint-pierre R. Epileptogenicity of brain structures in human temporal lobe epilepsy: a quantified study from intracerebral EEG. Brain. 2008;131:1818–30. https://doi.org/10.1093/brain/awn111.
Michalak AJ, Greenblatt A, Wu S, Tobochnik S, Dave H, Raghupathi R, Esengul YT, Guerra A, Tao JX, Issa NP, Cosgrove GR, Lega B, Warnke P, Chen HI, Lucas T, Sheth SA, Banks GP, Kwon CS, Feldstein N, Youngerman BE, McKhann GM, Davis KA, Schevon CA. Seizure on- set patterns predict outcome after stereo-electroencephalography-guided laser amygdalohippocampotomy. Epilepsia. 2023;64:1568–81. https://doi.org/10.1111/epi.17602.
Staba RJ. Normal and pathological high-frequency oscillations. Jasper’s basic mech. epilepsies. Ed. by Noebels JL, Avoli M, Rogawski MA, Olsen RW, and Delgado-Escueta AV. 4th ed. Oxford University Press, 2012. Chap. 16:202–12
Frauscher B, von Ellenrieder N, Zelmann R, Rogers C, Nguyen DK, Ka-hane P, Dubeau F, Gotman J. High-frequency oscillations in the normal human brain. Ann Neurol. 2018;84:374–85. https://doi.org/10.1002/ana.25304.
Chrobak JJ, Buzsaki G. High-frequency oscillations in the output networks of the hippocampal-entorhinal axis of the freely behaving rat. J Neurosci. 1996;16:3056–66. https://doi.org/10.1523/jneurosci.16-09-03056.
Bragin A, Mody I, Wilson CL, Engel J. Local generation of fast ripples in epileptic brain. J Neurosci. 2002;22:2012–21. https://doi.org/10.1523/jneurosci.22-05-02012.2002.
Zelmann R, Lina JM, Schulze-Bonhage A, Gotman J, Jacobs J. Scalp EEG is not a blur: it can see high frequency oscillations although their generators are small. Brain Topogr. 2014;27:683–704. https://doi.org/10.1007/s10548-013-0321-y.
Jacobs J, Zijlmans M, Zelmann R, Chatillon CE, Hall JA, Olivier A, Dubeau F, Gotman J. High-frequency electroencephalographic oscillations correlate with outcome of epilepsy surgery. Ann Neurol. 2010;67:209–20. https://doi.org/10.1002/ana.21847.
Jacobs J, Wu JY, Perucca P, Zelmann R, Mader M, Dubeau F, Mathern GW, Schulze-Bonhage A, Gotman J. Removing high-frequency oscillations: a prospective multicenter study on seizure outcome. Neurology. 2018;91:e1040–52. https://doi.org/10.1212/WNL.0000000000006158.
Roehri N, Pizzo F, Lagarde S, Lambert I, Nica A, McGonigal A, Giu-siano B, Bartolomei F, B’enar CG. High-frequency oscillations are not better biomarkers of epileptogenic tissues than spikes. Ann Neurol. 2018;83:84–97. https://doi.org/10.1002/ana.25124.
Schevon CA, Trevelyan AJ, Schroeder CE, Goodman RR, McKhann G, Emerson RG. Spatial characterization of interictal high frequency oscillations in epileptic neocortex. Brain. 2009;132:3047–59. https://doi.org/10.1093/brain/awp222.
Velmurugan J, Nagarajan SS, Mariyappa N, Kandavel GR, Ravindranadh T, Kenchaiah CM, Rose R, Bharath D, Saini J, Arivazhagan A, Rajan J, Mahadevan A, Rao MB, Satishchandra P, Sinha S. Magnetoencephalographic imaging of ictal high-frequency oscillations (80–200 Hz) in pharmacologically resistant focal epilepsy. Epilepsia. 2018;59:190–202. https://doi.org/10.1111/epi.13940.
Nissen IA, van Klink NE, Zijlmans M, Stam CJ, Hillebrand A. Brain areas with epileptic high frequency oscillations are functionally isolated in MEG virtual electrode networks. Clin Neurophysiol. 2016;127:2581–91. https://doi.org/10.1016/j.clinph.2016.04.013.
Papadelis C, Tamilia E, Stufflebeam SM, Grant PE, Madsen JR, Pearl PL, Tanaka N. Interictal high frequency oscillations detected with simultaneous magnetoencephalography and electroencephalography as biomarker of pediatric epilepsy. J Vis Exp. 2016;2016:1–13. https://doi.org/10.3791/54883.
van Klink N, Hillebrand A, Zijlmans M. Identification of epileptic high frequency oscillations in the time domain by using MEG beamformer-based virtual sensors. Clin Neurophysiol. 2016;127:197–208. https://doi.org/10.1016/j.clinph.2015.06.008.
Velmurugan J, Nagarajan SS, Mariyappa N, Mundlamuri RC, Raghaven-dra K, Bharath RD, Saini J, Arivazhagan A, Rajeswaran J, Mahadevan A, Malla BR, Satishchandra P, Sinha S. Magnetoencephalography imaging of high frequency oscillations strengthens presurgical localization and outcome prediction. Brain. 2019;142:3514–29. https://doi.org/10.1093/brain/awz284.
Tamilia E, Dirodi M, Alhilani M, Grant PE, Madsen JR, Stufflebeam SM, Pearl PL, Papadelis C. Scalp ripples as prognostic biomarkers of epileptogenicity in pediatric surgery. Ann Clin Transl Neurol. 2020;7:329–42. https://doi.org/10.1002/acn3.50994.
Xiang J, Maue E, Tong H, Mangano FT, Greiner H, Tenney JR. Neuromagnetic high frequency spikes are a new and noninvasive biomarker for localization of epileptogenic zones. Seizure. 2021;89:30–7. https://doi.org/10.1016/j.seizure.2021.04.024.
Xiang J, Maue E, Fujiwara H, Mangano FT, Greiner H, Tenney JR. Delineation of epileptogenic zones with high frequency magnetic source imaging based on kurtosis and skewness. Epilepsy Res. 2021;172:1–10. https://doi.org/10.1016/j.eplepsyres.2021.106602.
Shi LJ, Li CC, Lin YC, Ding CT, Wang YP, Zhang JC. The association of magnetoencephalography high-frequency oscillations with epilepsy types and a ripple-based method with source-level connectivity for mapping epilepsy sources. CNS Neurosci Ther. 2023;29:1423–33. https://doi.org/10.1111/cns.14115.
Vasilica AM, Litvak V, Cao C, Walker M, Vivekananda U. Detection of pathological high-frequency oscillations in refractory epilepsy patients undergoing simultaneous stereo-electroencephalography and magnetoen- cephalography. Seizure. 2023;107:81–90. https://doi.org/10.1016/j.seizure.2023.03.015.
von Ellenrieder N, Pellegrino G, Hedrich T, Gotman J, Lina JM, Grova C, Kobayashi E. Detection and magnetic source imaging of fast oscillations (40–160 Hz) recorded with magnetoencephalography in focal epilepsy patients. Brain Topogr. 2016;29:218–31. https://doi.org/10.1007/s10548-016-0471-9.
van Klink NEC, van Rosmalen F, Nenonen J, Burnos S, Helle L, Taulu S, Furlong PL, Zijlmans M, Hillebrand A. Automatic detection and visualisation of MEG ripple oscillations in epilepsy. NeuroImage Clin. 2017;15:689–701. https://doi.org/10.1016/j.nicl.2017.06.024.
Dirodi M, Tamilia E, Grant PE, Madsen JR, Stufflebeam SM, Pearl PL, and Papadelis C. Noninvasive localization of high-frequency oscillations in children with epilepsy: validation against intracranial gold-standard. Proc Annu Int Conf IEEE Eng Med Biol Soc EMBS 2019 :1555–8. https://doi.org/10.1109/EMBC.2019.8857793
Meng L. A Magnetoencephalography study of pediatric interictal neuromagnetic activity changes and brain network alterations caused by epilepsy in the high frequency (80–1000 Hz). IEEE Trans Neural Syst Rehabil Eng. 2019;27:389–99. https://doi.org/10.1109/TNSRE.2019.2898683.
Foley E, Quitadamo LR, Walsh AR, Bill P, Hillebrand A, Seri S. MEG detection of high frequency oscillations and intracranial-EEG vali- dation in pediatric epilepsy surgery. Clin Neurophysiol. 2021;132:2136–45. https://doi.org/10.1016/j.clinph.2021.06.005.
van Klink NEC, Zijlmans M. High frequency oscillations in MEG: next steps in source imaging for focal epilepsy. Brain. 2019;142:3318–20. https://doi.org/10.1093/brain/awz318.
Yin C, Zhang X, Chen Z, Li X, Wu S, Lv P, Wang Y. Detection and localization of interictal ripples with magnetoencephalography in the presurgical evaluation of drug-resistant insular epilepsy. Brain Res. 2019;1706:147–56. https://doi.org/10.1016/j.brainres.2018.11.006.
Reis J, Rosenow F. Chap. 95: Eloquent cortex and tracts: overview and noninvasive evaluation methods. In: Lüders HO, editor. Textbook of epilepsy surgery. 2008. p. 871–80.
Kreidenhuber R, De Tiège X, Rampp S. Presurgical functional cortical mapping using electromagnetic source imaging. Front Neurol. 2019;10:1–14. https://doi.org/10.3389/fneur.2019.00628.
Papanicolaou AC, Rezaie R, Narayana S, Choudhri AF, Boop FA, Wheless JW. On the relative merits of invasive and non-invasive pre-surgical brain mapping: new tools in ablative epilepsy surgery. Epilepsy Res. 2018;142:153–5. https://doi.org/10.1016/j.eplepsyres.2017.07.002.
Binder JR, Sabsevitz DS, Swanson SJ, Hammeke TA, Raghavan M, Mueller WM. Use of preoperative functional MRI to predict verbal memory decline after temporal lobe epilepsy surgery. Epilepsia. 2008;49:1377–94. https://doi.org/10.1111/j.1528-1167.2008.01625.x.
Sanai N, Mirzadeh Z, Berger MS. Functional outcome after language mapping for glioma resection. N Engl J Med. 2008;358:18–27. https://doi.org/10.1056/nejmoa067819.
Loddenkemper T, Morris HH, Möddel G. Complications during the Wada test. Epilepsy Behav. 2008;13:551–3. https://doi.org/10.1016/j.yebeh.2008.05.014.
Tandon N, Tong BA, Friedman ER, Johnson JA, Von Allmen G, Thomas MS, Hope OA, Kalamangalam GP, Slater JD, Thompson SA. Analysis of morbidity and outcomes associated with use of subdural grids vs stereoelectroencephalography in patients with intractable epilepsy. JAMA Neurol. 2019;76:672–81. https://doi.org/10.1001/jamaneurol.2019.0098.
Stippich C. Presurgical functional MRI and diffusion tensor imaging. Clin. funct. MRI presurical funct. neuroimaging. Ed. by Stippich C. 3rd ed. Springer, 2022. Chap. 1:1–20
Chougar L, Leclercq D, Van de Moortele PF, and Lehericy S. Presurgical functional localization possibilities limitations, and validity. Clin. funct. MRI presurical funct. neuroimaging. Ed. by Stippich C. 3rd ed. Springer, 2022. Chap. 9:343–72
Sporns O. Contributions and challenges for network models in cognitive neuroscience. Nat Neurosci. 2014;17:652–60. https://doi.org/10.1038/nn.3690.
Bagić AI, Bowyer SM, Kirsch HE, Funke ME, Burgess RC. American clinical MEG society (ACMEGS) position statement #2: the value of magnetoencephalography (MEG)/magnetic source imaging (MSI) in noninvasive presurgical mapping of eloquent cortices of patients preparing for surgical interventions. J Clin Neurophysiol. 2017;34:189–95. https://doi.org/10.1097/WNP.0000000000000366.
Youssofzadeh V, Stout J, Ustine C, Gross WL, Conant LL, Humphries CJ, Binder JR, Raghavan M. Mapping language from MEG beta power modulations during auditory and visual naming. Neuroimage. 2020;220: 117090. https://doi.org/10.1016/j.neuroimage.2020.117090.
Herfurth K, Harpaz Y, Roesch J, Mueller N, Walther K, Kaltenhaeuser M, Pauli E, Goldstein A, Hamer HM, Buchfelder M, Doerfler A, Prell J, Rampp S. Localization of beta power decrease as measure for lateralization in pre-surgical language mapping with magnetoencephalography, compared with functional magnetic resonance imaging and validated by Wada test. Front Hum Neurosci. 2022;16:1–21. https://doi.org/10.3389/fnhum.2022.996989.
Babajani-Feremi A, Pourmotabbed H, Schraegle WA, Calley CS, Clarke DF, Papanicolaou AC. MEG language mapping using a novel automatic ECD algorithm in comparison with MNE, dSPM, and DICS beamformer. Front Neurosci. 2023;17:1–17. https://doi.org/10.3389/fnins.2023.1151885.
Foley E, Wood AG, Furlong PL, Walsh AR, Kearney S, Bill P, Hillebrand A, Seri S. Mapping language networks and their association with verbal abilities in paediatric epilepsy using MEG and graph analysis. NeuroImage Clin. 2020;27: 102265. https://doi.org/10.1016/j.nicl.2020.102265.
Tierney TM, Holmes N, Mellor S, Lopez JD, Roberts G, Hill RM, Boto E, Leggett J, Shah V, Brookes MJ, Bowtell R, Barnes GR. Optically pumped magnetometers: from quantum origins to multi-channel magne- toencephalography. Neuroimage. 2019;199:598–608. https://doi.org/10.1016/j.neuroimage.2019.05.063.
Feys O, Corvilain P, Van Hecke A, Sculier C, Rikir E, Legros B, Gaspard N, Leurquin-Sterk G, Holmes N, Brookes MJ, Goldman S, Wens V, De Tiège X. Recording of ictal epileptic activity using on-scalp magnetoencephalography. Ann Neurol. 2022;93:419–21. https://doi.org/10.1002/ana.26562.
Alem O, Hughes KJ, Buard I, Cheung TP, Maydew T, Griesshammer A, Holloway K, Park A, Lechuga V, Coolidge C, Gerginov M, Quigg E, Seames A, Kronberg E, Teale P, Knappe S. An integrated full-head OPM-MEG system based on 128 zero-field sensors. Front Neurosci. 2023;17:1–8. https://doi.org/10.3389/fnins.2023.1190310. One of the first reports of a high-density whole-head OPM MEG system.
Hillebrand A, Holmes N, Sijsma N, Neill GCO, Tierney TM, Liberton N, Stam AH, van Klink N, Stam CJ, Bowtell R, Brookes MJ, Barnes GR. Non-invasive measurements of ictal and interictal epileptiform activity using optically pumped magnetometers. Nat Sci Reports. 2023;13:1–15. https://doi.org/10.1038/s41598-023-31111-y.
Tierney TM, Levy A, Barry DN, Meyer SS, Shigihara Y, Everatt M, Mel-lor S, Lopez JD, Bestmann S, Holmes N, Roberts G, Hill RM, Boto E, Leggett J, Shah V, Brookes MJ, Bowtell R, Maguire EA, Barnes GR. Mouth magnetoencephalography: a unique perspective on the human hippocampus. Neuroimage. 2021;225:117443. https://doi.org/10.1016/j.neuroimage.2020.117443.
Kramer D. Helium is again in short supply. Phys Today. 2022. https://doi.org/10.1063/PT.6.2.20220404a.
Kramer D. Helium prices surge to record levels as shortage continues. Phys Today. 2023;76:18–20. https://doi.org/10.1063/pt.3.5305.
Author information
Authors and Affiliations
Contributions
ASG, PT, and JSE wrote the manuscript. All authors reviewed its content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics Approval
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geller, A.S., Teale, P., Kronberg, E. et al. Magnetoencephalography for Epilepsy Presurgical Evaluation. Curr Neurol Neurosci Rep 24, 35–46 (2024). https://doi.org/10.1007/s11910-023-01328-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-023-01328-5