Abstract
Purpose of Review
As the most severe form of tuberculosis (TB), TB meningitis disproportionately affects developing countries and results in significant morbidity and mortality. In this report, we review recent updates in the epidemiology, diagnosis, and management of TB meningitis.
Recent Findings
Young children and people living with HIV continue to be at highest risk for TB meningitis. Early diagnosis remains challenging, especially since conventional diagnostic tests have sub-optimal sensitivity and specificity. Recently, nucleic acid amplification testing emerged as the preferred diagnostic modality due to its rapid turnaround time and high specificity.
Summary
Several recent studies have assessed the optimal treatment for TB meningitis. While the benefit of treatment intensification, by increasing rifampin dosing or adding a fluoroquinolone, is unclear, a growing body of evidence suggests that steroids confer a survival advantage, particularly in patients with mild disease. Additionally, TB meningitis management is further complicated by high rates of HIV co-infection. Recent data suggest that unlike other forms of TB, early initiation of antiretroviral therapy in patients with TB meningitis is associated with higher rates of adverse reactions, without improved survival.
TB meningitis continues to be a significant problem worldwide. Despite recent advances, more studies are warranted to improve early disease detection and optimize therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculous meningitis is the most severe form of tuberculosis (TB), associated with significant morbidity—including severe and irreversible neurologic sequelae—and mortality [1]. Following inhalation of infectious droplet nuclei containing Mycobacterium tuberculosis, hematogenous dissemination occurs, seeding oxygen-rich areas of the body, including the brain and other parts of the central nervous system (CNS) [2,3,4]. Meningitis occurs when infection spreads into the subarachnoid space, resulting in an exudative inflammatory response that can be complicated by obstruction of cerebrospinal fluid (CSF) flow and vascular compression and occlusion, with occasional involvement of the cranial nerves in the brain stem [2,3,4]. In this review, we highlight updates from the past 5 years in the epidemiology, diagnosis, and management of TB meningitis.
Epidemiology
Globally, the World Health Organization estimated that in 2015, there were 10.4 million new cases and 1.4 million deaths from tuberculosis [5]. Prior studies estimated that 10% of patients with active tuberculosis develop CNS disease, resulting in an incidence as high as 20.6 per 100,000 in high-burden countries [6]. Young children [7] and persons living with HIV (PLWH) [8,9,10] are at the highest risk for TB meningitis. The disease also disproportionately affects resource-limited countries with a high prevalence of poverty, lack of public health infrastructure, and limited access to healthcare [11]. While mortality associated with TB meningitis has decreased with anti-tuberculosis treatment [2, 11], it continues to be as high as 55–75%, especially in PLWH and those with advanced disease on presentation [12]. Up to 50% of survivors suffer from long-term neurologic sequelae [12] such as developmental delay [7], blindness [13], stroke, and seizures [11, 14].
In 2016, 9287 new cases of tuberculosis were reported in the USA, with an estimated incidence rate of 2.9 cases per 100,000 [15]. Of the incident cases, 68% were in persons born outside of the USA [15]. US surveillance data for 2015 from the Centers for Disease Control and Prevention (CDC) reported 1933 incident cases of extrapulmonary tuberculosis, of which 92 (4.5%) involved the meninges [16]. Prior CDC surveillance data from 1993 to 2006 had noted similar findings: 19% of tuberculosis patients had extrapulmonary disease, of whom 5.4% had meningeal involvement [17].
Diagnosis
Presenting Symptoms
The diagnosis of TB meningitis is often challenging, as clinical symptoms are typically subacute and nonspecific [3]. Compared to bacterial meningitis, patients with TB meningitis typically report longer symptom duration—up to 1 month in a recent study [18]. Adults with TB meningitis commonly present with stiff neck, headache, fever and vomiting—symptoms generally seen with other forms of bacterial meningitis. TB meningitis, however, is characterized by a higher likelihood of neurologic symptoms, with altered consciousness, personality changes, and coma seen in 59, 28, and 21% of TB meningitis patients, respectively [18]. Additionally, cranial nerve palsies, most frequently involving cranial nerve VI, are other common features, occurring in almost one-third of patients [19]. Unfortunately, by the time more advanced neurological symptoms are apparent (cranial nerve palsies, elevated intracranial pressure, altered level of consciousness), patients may have already suffered irreversible long-term sequelae.
Evaluation of Cerebrospinal Fluid
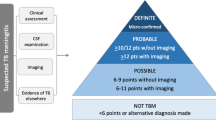
Several algorithms have been proposed to distinguish TB meningitis from other more common causes of meningitis [20,21,22]. Common features in the cerebrospinal fluid (CSF) analysis are included in Table 1. Compared to bacterial meningitis, patients with TB meningitis have higher relative lymphocytosis in the CSF [23].
Staining and Microscopy
The isolation of acid-fast bacilli in the CSF by culture is the gold standard for diagnosing TB meningitis. The Ziehl-Neelsen stain, also known as the acid-fast stain, has poor sensitivity for the diagnosis of TB meningitis, reported to be as low as 30% [27] and generally not exceeding 60% [28]. Sensitivity can be improved through serial sampling and meticulous microscopic evaluation [28]. Performing cytospin with Triton X-100 prior to acid-fast staining, the modified Ziehl-Neelsen stain [29], as well as staining of early secretory antigen target (ESAT)-6 [30], has significantly better performance than the conventional acid-fast stain.
CSF mycobacterial culture provides a definitive diagnosis of TB meningitis and allows for phenotypic drug susceptibility testing. However, cultures require an incubation period of up to 2 months and have imperfect sensitivity. The microscopic observation drug susceptibility (MODS) assay provides faster results than standard culture and is based on microscopic evaluation of M. tuberculosis grown in liquid culture [31]. However, MODS is not routinely available.
Adenosine Deaminase Testing
Adenosine deaminase (ADA) testing can be used in the diagnosis of pleural, pericardial, or peritoneal tuberculosis; however, it has not been useful for the diagnosis of TB meningitis. In a meta-analysis of 13 studies evaluating ADA in the diagnosis of TB meningitis, test utility was highly dependent on the cut-off used, with a lower sensitivity and higher specificity as the cut-off value increased [32]. Similar findings were noted in PLWH [33]. An ADA cut-off value that optimizes both sensitivity and specificity has been difficult to establish.
Nucleic Acid Amplification Testing
Nucleic acid amplification tests (NAATs) are PCR-based assays that are highly specific but not sensitive for the diagnosis of TB meningitis, making them more useful as confirmatory rather than diagnostic screening tests [34]. While higher sensitivities have been reported with novel real-time PCR assays [35, 36], they are still insufficient to exclude a diagnosis of TB meningitis. The Xpert MTB/Rif assay (Cepheid, Sunnyvale, CA, USA) is increasingly being used for molecular diagnosis of pulmonary tuberculosis [37, 38]. With a 2-h turnaround time, this commercial NAAT provides a rapid, highly sensitive method for detection of tuberculosis and rifampin resistance in pulmonary disease [39]. While NAAT is highly specific for tuberculosis in patients with extrapulmonary disease, including TB meningitis, the sensitivity of NAAT in these conditions is highly variable [40,41,42]. In 2013, WHO recommended using it preferentially over conventional microscopy and culture for initial TB meningitis testing in resource-limited settings [43]. However, Xpert MTB/Rif test quality is highly dependent on the CSF volume [44] and sample processing [40]. Additionally, Xpert MTB/Rif has a low positive predictive value in countries with low tuberculosis prevalence, which could result in false positive results [45]. To overcome the imperfect sensitivity of Xpert MTB/Rif, a next-generation assay—Xpert MTB/Rif Ultra—has been developed by Cepheid [46]. A recent WHO report found Ultra to be non-inferior to Xpert MTB/Rif in the diagnosis of TB, with improved sensitivity of the new assay in smear-negative culture-positive specimens, and in specimens obtained from PLWH [47]. Accordingly, WHO plans to update their policy in 2018, recommending the use of Ultra [47].
Interferon Gamma Release Assays
Interferon gamma release assays (IGRAs) detect the immune response to synthetic mycobacterial peptides present in M. tuberculosis, through measuring the amount of interferon gamma released, and providing results that are not influenced by prior bacilli Calmette-Guérin (BCG) vaccination [48]. IGRAs are not able to distinguish between latent M. tuberculosis infection and active TB disease. Their role in the diagnosis of TB meningitis has been evaluated in several studies [49, 50]. A recent systematic review evaluated the use of IGRA on blood (8 studies) and CSF samples (6 studies) for the diagnosis of TB meningitis [51]. The sensitivities for blood and CSF IGRA tests were 77 and 78%, respectively, while the specificity was lower for blood than that for CSF (61 vs. 88%) [51]. The performance of the test is significantly improved when combined with other diagnostic tools. Combined with a low CSF ADA (< 5.8 U/L), CSF IGRA has a sensitivity of 94% [50] and a high negative predictive value. When combined with a negative CSF bacterial Gram stain and a negative cryptococcal antigen latex test, the specificity is almost 100% [49], resulting in a high positive predictive value.
Radiographic Imaging
While there are no definitive radiographic findings that are pathognomonic for TB meningitis, brain imaging commonly shows basilar meningeal enhancement, hydrocephalus, basal ganglion enhancement, and infarcts. While several of these findings can be detected on computerized tomography (CT), magnetic resonance imaging (MRI) is a superior imaging modality for TB meningitis [52]. MRI also allows for better detection of early infarcts [53], identification of basal ganglion enhancement [54], enhancing exudates in basal cisterns, as well as carotid and cerebral vascular involvement [55].
Treatment
Treatment Regimens
The treatment of TB meningitis is based on the standard anti-tuberculosis regimen of a 2-month induction phase of isoniazid, rifampin, pyrazinamide, and ethambutol, followed by a continuation phase with isoniazid and rifampin [56,57,58]. Guidelines recommend a longer continuation phase for TB meningitis than pulmonary TB, with a total treatment duration of 9–12 months for TB meningitis [56,57,58,59]. Table 2 summarizes recommended doses and expected CSF penetration for common anti-tuberculosis medications.
Recent studies have focused on the role of higher rifampin doses as well as the addition of fluoroquinolones in the treatment of TB meningitis [61•, 62, 63]. A phase 2 trial conducted in Indonesia evaluating the role of intensified TB meningitis regimens (increased rifampin dose and/or adding moxifloxacin) for the first 2 weeks of treatment (together with isoniazid, pyrazinamide, and corticosteroids) showed that the higher rifampin dose (13 mg/kg intravenous vs. 10 mg/kg oral) was associated with an almost 50% decrease in 6-month mortality, more rapid resolution of coma, and higher likelihood of complete neurologic recovery after 6 months of treatment [62]. Moxifloxacin did not appear to have any survival benefit at either the 400 or 800-mg dose [62].
One study evaluating the efficacy and pharmacokinetics of adding fluoroquinolones to the standard TB meningitis regimen suggested that fluoroquinolones improve TB meningitis outcomes if they are started early in the disease course [63]. However, these results [62, 63] were not replicated in a larger randomized trial involving both PLWH- and HIV-uninfected patients that evaluated the effect of intensified anti-tuberculosis therapy on mortality in patients with TB meningitis [61•]. Compared to standard anti-tuberculosis regimens, researchers concluded that neither the addition of levofloxacin (20 mg/kg/day) nor the increase in the dose of rifampin (15 mg/kg compared to the traditional 10 mg/kg) reduced mortality by 9 months from initiating therapy. However, this intensified regimen was associated with an increased risk of seizures and visual impairment [61•].
A recent study involving PLWH diagnosed with TB meningitis found that the standard dosing regimen for rifampin results in sub-optimal CSF and systemic rifampin exposure. In addition, standard pyrazinamide dosing resulted in elevated CSF concentrations that were independently associated with neurological toxicity and increased mortality [64].
Duration of Treatment
The optimal duration of treatment for TB meningitis is not clearly established. Current guidelines from the World Health Organization [57, 59], American Thoracic Society, Centers for Disease Control and Prevention, Infectious Diseases Society of America [56], and British Infection Society [58] recommend 12 months of treatment. To date, no randomized trials have directly compared 6-month vs. longer (9–12 months) treatment durations for TB meningitis. While an earlier systematic review suggested that shorter treatment duration for TB meningitis (6 months compared to 9–12 months) is not associated with increased mortality, residual neurological deficits, or relapse [65], the findings were based on observational studies that had highly variable results. In contrast, a more recent Cochrane review evaluating the same question noted that mortality risk was higher among patients in cohorts treated for more than 6 months [66]. However, most deaths occurred in the first 6 months, indicating that the difference is likely a reflection of other confounding factors and not the duration of therapy [66].
Drug-Resistant Tuberculous Meningitis
Isoniazid (INH) is a key component of anti-tuberculosis regimens and has high CSF penetration [67]. Unfortunately, INH resistance has been reported in 6% [68]—18% [69] of TB meningitis cases. Prior studies showed similar treatment outcome in patients with isoniazid-resistant pulmonary tuberculosis compared to those with drug-susceptible infection. However, CDC surveillance data from 1993 to 2005 demonstrated that isoniazid resistance on initial susceptibility testing is associated with a significant increase in mortality risk among patients with CSF culture-positive TB meningitis [68]. The most effective treatment for isoniazid-resistant TB meningitis remains unclear [67], although several guidelines recommend treatment with daily rifampin, ethambutol, and pyrazinamide with or without adding a fluoroquinolone to the regimen [58, 70].
Adjunctive Interventions in Management of TB Meningitis
Steroids
A 2016 Cochrane review of nine randomized trials, including 1337 patients with TB meningitis, evaluated the effects of adding corticosteroids to anti-tuberculosis medications [71]. The mortality of TB meningitis in patients who were treated with an anti-tuberculosis regimen alone was 40%; the addition of corticosteroids reduced the risk of death by one-fourth. The survival benefit of corticosteroids was mostly seen in patients with mild disease; there was no significant advantage in patients with advanced neurologic symptoms [12]. Additionally, improvement in survival was not associated with a decrease in disabling neurological deficits [71]. However, there was no increased risk of adverse events in patients receiving steroids. Similar results were found in a 2013 systematic review evaluating the role of steroids in all patients with tuberculosis [72], with pooled results from trials evaluating the role of steroids in TB meningitis showing a lower mortality and no increased risk of adverse events.
Surgery
Surgical management is infrequently warranted in the treatment of TB meningitis. Indications for surgery include persistent hydrocephalus, in which a ventriculoperitoneal shunt is placed to alleviate the increased intracranial pressure; this intervention has been associated with improved clinical outcomes [73]. Cerebral abscesses and extradural lesions with resultant cerebral or vertebral compression and neurologic deficits are other indications for surgical intervention.
Aspirin
Patients with TB meningitis are at risk for ischemic strokes secondary to vascular occlusion, and hemorrhagic strokes associated with venous sinus thrombosis. Two randomized controlled trials evaluated the role of aspirin in decreasing the risk of stroke in adults [74] and children [75] with TB meningitis. Both trials failed to show a significant association between aspirin and stroke prevention.
Tuberculous Meningitis in People Living with HIV
Prevalence of TB Meningitis in PLWH
HIV infection is associated with a significant increase in TB risk [8, 9] and particularly an increase in the risk of extrapulmonary TB. Globally, PLWH are 20–30 times more likely to develop TB disease compared to HIV-uninfected persons, with 12% of patients with TB worldwide being co-infected with HIV [5]. In the USA, HIV co-infection in patients with TB was as high as 48% in 1993, dropping to 5.5% in 2015 [16]. The prevalence of HIV co-infection in patients with TB is the highest in the 25–44-year age group [16]. Among patients with TB, 40% of all cases in PLWH are extrapulmonary, compared to 10% in HIV-uninfected counterparts [9, 10, 17, 76]. Similarly, for patients with TB, PLWH have a five-fold increase in the likelihood of having CNS involvement [11, 58] and disseminated TB [10] compared to HIV-uninfected persons [8, 60]. This risk significantly increases among patients with CD4+ lymphocyte cell count < 100 cells/mL [10]. In a prospective cohort study conducted in Uganda involving PLWH not on antiretroviral therapy (ART) with suspected meningitis, M. tuberculosis was the third most commonly identified CSF pathogen after Cryptococcus and Epstein Barr virus [77].
Disease Presentation in PLWH
The symptoms of TB meningitis are similar regardless of HIV serostatus [60]. However, it has been noted that PLWH commonly present with extra meningeal involvement [78] and are more likely to suffer from altered mental status [60]. Previous studies have reported lower lumbar puncture opening pressure, lower pleocytosis in cerebrospinal fluid [79, 80], and higher AFB culture yield among PLWH patients with TB meningitis compared to those of HIV-uninfected persons [81].
Immune Reconstitution Inflammatory Syndrome
The management of TB meningitis in PLWH is usually complicated by multiple drug-drug interactions as well as the risk of immune reconstitution [82]. Immune reconstitution inflammatory syndrome (IRIS) is a phenomenon that results from an excessive immune response against Mycobacterium tuberculosis after initiation of antiretroviral therapy. Extrapulmonary tuberculosis, low CD4+ counts, and high HIV viral load prior to initiating ART are factors associated with significant increase in risk of tuberculosis-associated IRIS [83]. TB IRIS is seen in nearly half of PLWH with TB meningitis [84] and is associated with high morbidity and mortality rates [85]. Manifestations of TB meningitis IRIS include worsening headaches, decreased level of consciousness, new onset seizures, and paresis [84]. Studies suggest a higher risk of IRIS in patients with positive CSF cultures, indicating that high baseline tuberculosis antigen load drives an inflammatory response manifesting as TB IRIS [84, 86]. Additionally, it was noted that higher neutrophil counts and percentage as well as higher levels of inflammatory cytokines such as interferon (IFN)-γ and tumor necrosis factor (TNF)-α at the time of TB meningitis presentation were associated with higher likelihood of developing TB IRIS [84, 86,87,88].
A similar phenomenon referred to as a “paradoxical worsening” is also seen among HIV-uninfected patients with TB meningitis, who can experience worsening of symptoms after TB treatment initiation [89,90,91,92,93•].
Initiating Antiretroviral Therapy
Since ART initiation and secondary IRIS can unmask previously undiagnosed tuberculosis, or cause paradoxical worsening of known tuberculosis disease [94], it is critical to gauge the timing of ART initiation in relation to anti-tuberculosis treatment.
The concomitant treatment of tuberculosis and HIV is associated with improved survival compared to starting ART after completion of anti-tuberculosis treatment [95]. However, it has been noted that the initiation of ART within 2–3 weeks of starting anti-tuberculosis therapy is associated with an increased risk of IRIS [96,97,98,99], particularly in persons with < 50 CD4+ lymphocytes/mm3. Despite the IRIS risk, initiating ART within 2–3 weeks in persons with < 50 CD4+ lymphocytes/mm3 is associated with improved survival. However, this does not appear to be true for TB meningitis. In a recent trial involving PLWH diagnosed with TB meningitis, no improvement in 9- or 12-month mortality was seen in those who started ART soon after anti-tuberculosis treatment [100••]. Further, patients with TB meningitis who were immediately started on ART had significantly higher rate of adverse events. Therefore, among persons with advanced HIV and TB meningitis, the control of the opportunistic infection maybe necessary prior to starting ART and reconstituting the immune system. This finding is similar to that seen with cryptococcal meningitis among persons with advanced HIV, in which early initiation of ART is associated with worse outcomes than delaying ART initiation until after at least 5 weeks of treatment of cryptococcal meningitis [101, 102].
Disease Prognosis in PLWH
The prognosis of TB meningitis is worse, and the risk of death is higher for PLWH than that of HIV-uninfected persons. [78]. Additionally, while the rate of TB meningitis relapse is similar in PLWH compared to that of HIV-uninfected persons, the mortality risk after relapse is significantly higher for PLWH (83 vs. 51%) [78].
Conclusion
TB meningitis, while relatively rare in the USA, continues to be a significant cause of meningitis worldwide, especially among children and PLWH. It presents with non-specific signs and symptoms and can progress to severe and irreversible neurologic sequelae, including death. The diagnosis of TB meningitis requires a high level of clinical suspicion, supported by available diagnostic tests: acid-fast staining, nucleic acid amplification testing, and cultures. Treatment involves a 2-month induction phase of isoniazid, rifampin, pyrazinamide, and ethambutol with adjunctive steroids followed by 10 months of isoniazid and rifampin.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Van TT, Farrar J. Tuberculous meningitis. J Epidemiol Community Health. 2014;68(3):195–6. https://doi.org/10.1136/jech-2013-202525.
Rock RB, Olin M, Baker CA, Molitor TW, Peterson PK. Central nervous system tuberculosis: pathogenesis and clinical aspects. Clin Microbiol Rev. 2008;21(2):243–261, table of contents. https://doi.org/10.1128/CMR.00042-07.
Thwaites GE, van Toorn R, Schoeman J. Tuberculous meningitis: more questions, still too few answers. Lancet Neurol. 2013;12(10):999–1010. https://doi.org/10.1016/S1474-4422(13)70168-6.
Torok ME. Tuberculous meningitis: advances in diagnosis and treatment. Br Med Bull. 2015;113(1):117–31. https://doi.org/10.1093/bmb/ldv003.
World Health Organization. Global tuberculosis report 2016. 2016.
Murthy JM. Tuberculous meningitis: the challenges. Neurol India. 2010;58(5):716–22. https://doi.org/10.4103/0028-3886.72178.
van Well GT, Paes BF, Terwee CB, Springer P, Roord JJ, Donald PR, et al. Twenty years of pediatric tuberculous meningitis: a retrospective cohort study in the western cape of South Africa. Pediatrics. 2009;123(1):e1–8.
Berenguer J, Moreno S, Laguna F, Vicente T, Adrados M, Ortega A, et al. Tuberculous meningitis in patients infected with the human immunodeficiency virus. N Engl J Med. 1992;326(10):668–72. https://doi.org/10.1056/NEJM199203053261004.
Kingkaew N, Sangtong B, Amnuaiphon W, Jongpaibulpatana J, Mankatittham W, Akksilp S, et al. HIV-associated extrapulmonary tuberculosis in Thailand: epidemiology and risk factors for death. Int J Infect Dis. 2009;13(6):722–9. https://doi.org/10.1016/j.ijid.2008.11.013.
Leeds IL, Magee MJ, Kurbatova EV, del Rio C, Blumberg HM, Leonard MK, et al. Site of extrapulmonary tuberculosis is associated with HIV infection. Clin Infect Dis. 2012;55(1):75–81.
Schoeman JF, Donald PR. Chapter 117—tuberculous meningitis. In: Olivier Dulac ML, Harvey BS, editors. Handbook of clinical neurology. Elsevier; 2013. p. 1135–8.
Thwaites GE, Nguyen DB, Nguyen HD, Hoang TQ, Do TT, Nguyen TC, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004;351(17):1741–51. https://doi.org/10.1056/NEJMoa040573.
Sinha MK, Garg RK, Anuradha H, Agarwal A, Singh MK, Verma R, et al. Vision impairment in tuberculous meningitis: predictors and prognosis. J Neurol Sci. 2010;290(1–2):27–32. https://doi.org/10.1016/j.jns.2009.12.012.
Mai NT, Thwaites GE. Recent advances in the diagnosis and management of tuberculous meningitis. Curr Opin Infect Dis. 2017;30(1):123–8. https://doi.org/10.1097/QCO.0000000000000331.
Schmit KM, Wansaula Z, Pratt R, Price SF, Langer AJ. Tuberculosis—United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(11):289–94. https://doi.org/10.15585/mmwr.mm6611a2.
Centers for Disease Control and Prevention (CDC). Reported tuberculosis in the United States, 2015. Atlanta: US Department of Health and Human Services, CDC; 2016.
Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49(9):1350–7. https://doi.org/10.1086/605559.
Pehlivanoglu F, Yasar KK, Sengoz G. Tuberculous meningitis in adults: a review of 160 cases. ScientificWorldJournal. 2012;2012:169028. https://doi.org/10.1100/2012/169028.
Sharma P, Garg RK, Verma R, Singh MK, Shukla R. Incidence, predictors and prognostic value of cranial nerve involvement in patients with tuberculous meningitis: a retrospective evaluation. Eur J Intern Med. 2011;22(3):289–95. https://doi.org/10.1016/j.ejim.2011.01.007.
Youssef FG, Afifi SA, Azab AM, Wasfy MM, Abdel-Aziz KM, Parker TM, et al. Differentiation of tuberculous meningitis from acute bacterial meningitis using simple clinical and laboratory parameters. Diagn Microbiol Infect Dis. 2006;55(4):275–8.
Hristea A, Olaru ID, Baicus C, Moroti R, Arama V, Ion M. Clinical prediction rule for differentiating tuberculous from viral meningitis. Int J Tuberc Lung Dis. 2012;16(6):793–8. https://doi.org/10.5588/ijtld.11.0687.
Vibha D, Bhatia R, Prasad K, Srivastava MP, Tripathi M, Kumar G, et al. Validation of diagnostic algorithm to differentiate between tuberculous meningitis and acute bacterial meningitis. Clin Neurol Neurosurg. 2012;114(6):639–44.
Zhang YL, Lin S, Shao LY, Zhang WH, Weng XH. Validation of Thwaites’ diagnostic scoring system for the differential diagnosis of tuberculous meningitis and bacterial meningitis. Jpn J Infect Dis. 2014;67(6):428–31.
Cohen DB, Zijlstra EE, Mukaka M, Reiss M, Kamphambale S, Scholing M, et al. Diagnosis of cryptococcal and tuberculous meningitis in a resource-limited African setting. Tropical Med Int Health. 2010;15(8):910–7. https://doi.org/10.1111/j.1365-3156.2010.02565.x.
Patel VB, Singh R, Connolly C, Kasprowicz V, Zumla A, Ndungu T, et al. Comparison of a clinical prediction rule and a LAM antigen-detection assay for the rapid diagnosis of TBM in a high HIV prevalence setting. PLoS One. 2010;5(12):e15664. https://doi.org/10.1371/journal.pone.0015664.
Jackson A, van der Horst C. New insights in the prevention, diagnosis, and treatment of cryptococcal meningitis. Curr HIV/AIDS Rep. 2012;9(3):267–77. https://doi.org/10.1007/s11904-012-0127-7.
Erdem H, Ozturk-Engin D, Elaldi N, Gulsun S, Sengoz G, Crisan A, et al. The microbiological diagnosis of tuberculous meningitis: results of Haydarpasa-1 study. Clin Microbiol Infect. 2014;20(10):O600–8. https://doi.org/10.1111/1469-0691.12478.
Thwaites GE, Chau TT, Farrar JJ. Improving the bacteriological diagnosis of tuberculous meningitis. J Clin Microbiol. 2004;42(1):378–9.
Chen P, Shi M, Feng GD, Liu JY, Wang BJ, Shi XD, et al. A highly efficient Ziehl-Neelsen stain: identifying de novo intracellular Mycobacterium tuberculosis and improving detection of extracellular M. tuberculosis in cerebrospinal fluid. J Clin Microbiol. 2012;50(4):1166–70. https://doi.org/10.1128/JCM.05756-11.
Feng GD, Shi M, Ma L, Chen P, Wang BJ, Zhang M, et al. Diagnostic accuracy of intracellular mycobacterium tuberculosis detection for tuberculous meningitis. Am J Respir Crit Care Med. 2014;189(4):475–81. https://doi.org/10.1164/rccm.201309-1686OC.
Caws M, Dang TM, Torok E, Campbell J, Do DA, Tran TH, et al. Evaluation of the MODS culture technique for the diagnosis of tuberculous meningitis. PLoS One. 2007;2(11):e1173. https://doi.org/10.1371/journal.pone.0001173.
Tuon FF, Higashino HR, Lopes MI, Litvoc MN, Atomiya AN, Antonangelo L, et al. Adenosine deaminase and tuberculous meningitis—a systematic review with meta-analysis. Scand J Infect Dis. 2010;42(3):198–207. https://doi.org/10.3109/00365540903428158.
Corral I, Quereda C, Navas E, Martin-Davila P, Perez-Elias MJ, Casado JL, et al. Adenosine deaminase activity in cerebrospinal fluid of HIV-infected patients: limited value for diagnosis of tuberculous meningitis. Eur J Clin Microbiol Infect Dis. 2004;23(6):471–6. https://doi.org/10.1007/s10096-004-1110-z.
Pai M, Flores LL, Pai N, Hubbard A, Riley LW, Colford JM Jr. Diagnostic accuracy of nucleic acid amplification tests for tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2003;3(10):633–43.
Takahashi T, Nakayama T. Novel technique of quantitative nested real-time PCR assay for Mycobacterium tuberculosis DNA. J Clin Microbiol. 2006;44(3):1029–39. https://doi.org/10.1128/JCM.44.3.1029-1039.2006.
Bhigjee AI, Padayachee R, Paruk H, Hallwirth-Pillay KD, Marais S, Connoly C. Diagnosis of tuberculous meningitis: clinical and laboratory parameters. Int J Infect Dis. 2007;11(4):348–54. https://doi.org/10.1016/j.ijid.2006.07.007.
Boehme CC, Nabeta P, Hillemann D, Nicol MP, Shenai S, Krapp F, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010;363(11):1005–15. https://doi.org/10.1056/NEJMoa0907847.
Lawn SD, Nicol MP. Xpert® MTB/RIF assay: development, evaluation and implementation of a new rapid molecular diagnostic for tuberculosis and rifampicin resistance. Future Microbiol. 2011;6(9):1067–82.
Chang K, Lu W, Wang J, Zhang K, Jia S, Li F, et al. Rapid and effective diagnosis of tuberculosis and rifampicin resistance with Xpert MTB/RIF assay: a meta-analysis. J Inf Secur. 2012;64(6):580–8. https://doi.org/10.1016/j.jinf.2012.02.012.
Patel VB, Theron G, Lenders L, Matinyena B, Connolly C, Singh R, et al. Diagnostic accuracy of quantitative PCR (Xpert MTB/RIF) for tuberculous meningitis in a high burden setting: a prospective study. PLoS Med. 2013;10(10):e1001536. https://doi.org/10.1371/journal.pmed.1001536.
Nhu NT, Heemskerk D, do DA T, Chau TT, Mai NT, Nghia HD, et al. Evaluation of GeneXpert MTB/RIF for diagnosis of tuberculous meningitis. J Clin Microbiol. 2014;52(1):226–33. https://doi.org/10.1128/JCM.01834-13.
Denkinger CM, Schumacher SG, Boehme CC, Dendukuri N, Pai M, Steingart KR. Xpert MTB/RIF assay for the diagnosis of extrapulmonary tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2014;44(2):435–46. https://doi.org/10.1183/09031936.00007814.
World Health Organization. Xpert MTB/RIF assay for the diagnosis of pulmonary and extrapulmonary TB in adults and children: policy update. 2013.
Bahr NC, Tugume L, Rajasingham R, Kiggundu R, Williams DA, Morawski B, et al. Improved diagnostic sensitivity for tuberculous meningitis with Xpert((R)) MTB/RIF of centrifuged CSF. Int J Tuberc Lung Dis. 2015;19(10):1209–15. https://doi.org/10.5588/ijtld.15.0253.
Bahr NC, Marais S, Caws M, van Crevel R, Wilkinson RJ, Tyagi JS, et al. GeneXpert MTB/RIF to diagnose tuberculous meningitis: perhaps the first test but not the last. Clin Infect Dis. 2016;62(9):1133–5.
Cepheid. 2017 launch of new TB test Ultra backed by WHO recommendation. http://www.cepheid.com/us/about-us/news-events/press-releases/216-2017-launch-of-new-tb-test-ultra-backed-by-who-recommendation. Accessed 08/10/2017.
WHO meeting report of a technical expert consultation: non-inferiority analysis of Xpert MTF/RIF Ultra compared to Xpert MTB/RIF. Geneva: World Health Organization; 2017 (WHO/HTM/TB/2017.04). Licence: CC BY-NCSA 3.0 IGO.
Mazurek GH, Jereb J, Vernon A, LoBue P, Goldberg S, Castro K, et al. Updated guidelines for using interferon gamma release assays to detect Mycobacterium tuberculosis infection-United States, 2010. MMWR Recomm Rep. 2010;59(RR-5):1–25.
Patel VB, Singh R, Connolly C, Coovadia Y, Peer AK, Parag P, et al. Cerebrospinal T-cell responses aid in the diagnosis of tuberculous meningitis in a human immunodeficiency virus- and tuberculosis-endemic population. Am J Respir Crit Care Med. 2010;182(4):569–77. https://doi.org/10.1164/rccm.200912-1931OC.
Kim SH, Cho OH, Park SJ, Lee EM, Kim MN, Lee SO, et al. Rapid diagnosis of tuberculous meningitis by T cell-based assays on peripheral blood and cerebrospinal fluid mononuclear cells. Clin Infect Dis. 2010;50(10):1349–58. https://doi.org/10.1086/652142.
Yu J, Wang ZJ, Chen LH, Li HH. Diagnostic accuracy of interferon-gamma release assays for tuberculous meningitis: a meta-analysis. Int J Tuberc Lung Dis. 2016;20(4):494–9. https://doi.org/10.5588/ijtld.15.0600.
Torres C, Riascos R, Figueroa R, Gupta RK. Central nervous system tuberculosis. Top Magn Reson Imaging. 2014;23(3):173–89. https://doi.org/10.1097/RMR.0000000000000023.
Pienaar M, Andronikou S, van Toorn R. MRI to demonstrate diagnostic features and complications of TBM not seen with CT. Childs Nerv Syst. 2009;25(8):941–7. https://doi.org/10.1007/s00381-008-0785-3.
Botha H, Ackerman C, Candy S, Carr JA, Griffith-Richards S, Bateman KJ. Reliability and diagnostic performance of CT imaging criteria in the diagnosis of tuberculous meningitis. PLoS One. 2012;7(6):e38982. https://doi.org/10.1371/journal.pone.0038982.
Kalita J, Prasad S, Maurya PK, Kumar S, Misra UKMR. Angiography in tuberculous meningitis. Acta Radiol. 2012;53(3):324–9. https://doi.org/10.1258/ar.2012.110712.
Nahid P, Dorman SE, Alipanah N, Barry PM, Brozek JL, Cattamanchi A, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America clinical practice guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis. 2016;63(7):e147–e95. https://doi.org/10.1093/cid/ciw376.
World Health Organization, Stop TB Initiative. Treatment of tuberculosis: guidelines. Geneva: World Health Organization; 2010.
Thwaites G, Fisher M, Hemingway C, Scott G, Solomon T, Innes J, et al. British Infection Society guidelines for the diagnosis and treatment of tuberculosis of the central nervous system in adults and children. J Inf Secur. 2009;59(3):167–87. https://doi.org/10.1016/j.jinf.2009.06.011.
World Health Organization. Guidelines for the treatment of drug-susceptible tuberculosis and patient care, 2017 update. 2017.
Nelson CA, Zunt JR. Tuberculosis of the central nervous system in immunocompromised patients: HIV infection and solid organ transplant recipients. Clin Infect Dis. 2011;53(9):915–26. https://doi.org/10.1093/cid/cir508.
• Heemskerk AD, Bang ND, Mai NT, Chau TT, Phu NH, Loc PP, et al. Intensified antituberculosis therapy in adults with tuberculous meningitis. N Engl J Med. 2016;374(2):124–34. https://doi.org/10.1056/NEJMoa1507062. This randomized clinical trial conducted at two centers in Vietnam evaluated whether TB meningitis survival rates improved with treatment intensification through increased rifampin dosing and adding levofloxacin. During 9 months of follow-up and compared to patients treated with standard therapy, treatment intensification did not confer a significant survival benefit. Moreover, intensified treatment was associated with increased, albeit not statistically significant, rates of adverse events.
Ruslami R, Ganiem AR, Dian S, Apriani L, Achmad TH, van der Ven AJ, et al. Intensified regimen containing rifampicin and moxifloxacin for tuberculous meningitis: an open-label, randomised controlled phase 2 trial. Lancet Infect Dis. 2013;13(1):27–35. https://doi.org/10.1016/S1473-3099(12)70264-5.
Thwaites GE, Bhavnani SM, Chau TT, Hammel JP, Torok ME, Van Wart SA, et al. Randomized pharmacokinetic and pharmacodynamic comparison of fluoroquinolones for tuberculous meningitis. Antimicrob Agents Chemother. 2011;55(7):3244–53. https://doi.org/10.1128/AAC.00064-11.
Torok ME, Aljayyoussi G, Waterhouse D, Chau T, Mai N, Phu NH, et al. Suboptimal exposure to anti-TB drugs in a TBM/HIV+ population is not related to anti-retroviral therapy. Clin Pharmacol Ther. 2017; https://doi.org/10.1002/cpt.646.
van Loenhout-Rooyackers JH, Keyser A, Laheij RJ, Verbeek AL, van der Meer JW. Tuberculous meningitis: is a 6-month treatment regimen sufficient? Int J Tuberc Lung Dis. 2001;5(11):1028–35.
Jullien S, Ryan H, Modi M, Bhatia R. Six months therapy for tuberculous meningitis. Cochrane Database Syst Rev. 2016;9:CD012091. https://doi.org/10.1002/14651858.CD012091.pub2.
Garg RK, Jain A, Malhotra HS, Agrawal A, Garg R. Drug-resistant tuberculous meningitis. Expert Rev Anti-Infect Ther. 2013;11(6):605–21. https://doi.org/10.1586/eri.13.39.
Vinnard C, Winston CA, Wileyto EP, Macgregor RR, Bisson GP. Isoniazid resistance and death in patients with tuberculous meningitis: retrospective cohort study. BMJ. 2010;341:c4451. https://doi.org/10.1136/bmj.c4451.
Nagarathna S, Rafi W, Veenakumari HB, Mani R, Satishchandra P, Chandramuki A. Drug susceptibility profiling of tuberculous meningitis. Int J Tuberc Lung Dis. 2008;12(1):105–7.
World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. Geneva: World Health Organization; 2014.
Prasad K, Singh MB, Ryan H. Corticosteroids for managing tuberculous meningitis. Cochrane Database Syst Rev. 2016;4:CD002244. https://doi.org/10.1002/14651858.CD002244.pub4.
Critchley JA, Young F, Orton L, Garner P. Corticosteroids for prevention of mortality in people with tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):223–37. https://doi.org/10.1016/S1473-3099(12)70321-3.
Kilincoglu BF, Dalkilic T, Dincbal MN, Aydin Y. Shunting in hydrocephalus due to tuberculous meningitis. Cases presenting with high cerebrospinal fluid proteins in pediatric age. J Neurosurg Sci. 2009;53(2):49–53.
Misra UK, Kalita J, Nair PP. Role of aspirin in tuberculous meningitis: a randomized open label placebo controlled trial. J Neurol Sci. 2010;293(1–2):12–7. https://doi.org/10.1016/j.jns.2010.03.025.
Schoeman JF, Janse van Rensburg A, Laubscher JA, Springer P. The role of aspirin in childhood tuberculous meningitis. J Child Neurol. 2011;26(8):956–62. https://doi.org/10.1177/0883073811398132.
Yang Z, Kong Y, Wilson F, Foxman B, Fowler AH, Marrs CF, et al. Identification of risk factors for extrapulmonary tuberculosis. Clin Infect Dis. 2004;38(2):199–205. https://doi.org/10.1086/380644.
Rajasingham R, Rhein J, Klammer K, Musubire A, Nabeta H, Akampurira A, et al. Epidemiology of meningitis in an HIV-infected Ugandan cohort. Am J Trop Med Hyg. 2015;92(2):274–9. https://doi.org/10.4269/ajtmh.14-0452.
Thwaites GE, Duc Bang N, Huy Dung N, Thi Quy H, Thi Tuong Oanh D, Thi Cam Thoa N, et al. The influence of HIV infection on clinical presentation, response to treatment, and outcome in adults with tuberculous meningitis. J Infect Dis. 2005;192(12):2134–41. https://doi.org/10.1086/498220.
Cecchini D, Ambrosioni J, Brezzo C, Corti M, Rybko A, Perez M, et al. Tuberculous meningitis in HIV-infected and non-infected patients: comparison of cerebrospinal fluid findings [short communication]. Int J Tuberc Lung Dis. 2009;13(2):269–71.
Vidal J, Penalva de Oliveira A, Hernández A. CD4+ T-cell count and cerebrospinal fluid findings in HIV-infected patients with tuberculous meningitis [correspondence]. Int J Tuberc Lung Dis. 2010;14(11):1496–7.
Puccioni-Sohler M, Brandão CO. Factors associated to the positive cerebrospinal fuid culture in the tuberculous meningitis. Arq Neuropsiquiatr. 2007;65(1):48–53.
Chamie G, Marquez C, Luetkemeyer A. HIV-associated central nervous system tuberculosis. Semin Neurol. 2014;34(1):103–15. https://doi.org/10.1055/s-0034-1372347.
Laureillard D, Marcy O, Madec Y, Chea S, Chan S, Borand L, et al. Paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome after early initiation of antiretroviral therapy in a randomized clinical trial. AIDS. 2013;27(16):2577–86. https://doi.org/10.1097/01.aids.0000432456.14099.c7.
Marais S, Meintjes G, Pepper DJ, Dodd LE, Schutz C, Ismail Z, et al. Frequency, severity, and prediction of tuberculous meningitis immune reconstitution inflammatory syndrome. Clin Infect Dis. 2013;56(3):450–60. https://doi.org/10.1093/cid/cis899.
Pepper DJ, Marais S, Maartens G, Rebe K, Morroni C, Rangaka MX, et al. Neurologic manifestations of paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome: a case series. Clin Infect Dis. 2009;48(11):e96–107. https://doi.org/10.1086/598988.
Marais S, Wilkinson KA, Lesosky M, Coussens AK, Deffur A, Pepper DJ, et al. Neutrophil-associated central nervous system inflammation in tuberculous meningitis immune reconstitution inflammatory syndrome. Clin Infect Dis. 2014;59(11):1638–47. https://doi.org/10.1093/cid/ciu641.
Marais S, Lai RPJ, Wilkinson KA, Meintjes G, O'Garra A, Wilkinson RJ. Inflammasome activation underlying central nervous system deterioration in HIV-associated tuberculosis. J Infect Dis. 2017;215(5):677–86. https://doi.org/10.1093/infdis/jiw561.
Meintjes G, Wilkinson RJ, Morroni C, Pepper DJ, Rebe K, Rangaka MX, et al. Randomized placebo-controlled trial of prednisone for paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome. AIDS. 2010;24(15):2381–90. https://doi.org/10.1097/QAD.0b013e32833dfc68.
Bell LC, Breen R, Miller RF, Noursadeghi M, Lipman M. Paradoxical reactions and immune reconstitution inflammatory syndrome in tuberculosis. Int J Infect Dis. 2015;32:39–45. https://doi.org/10.1016/j.ijid.2014.12.030.
Carvalho AC, De Iaco G, Saleri N, Pini A, Capone S, Manfrin M, et al. Paradoxical reaction during tuberculosis treatment in HIV-seronegative patients. Clin Infect Dis. 2006;42(6):893–5. https://doi.org/10.1086/500459.
Garg RK, Malhotra HS, Kumar N. Paradoxical reaction in HIV negative tuberculous meningitis. J Neurol Sci. 2014;340(1–2):26–36. https://doi.org/10.1016/j.jns.2014.03.025.
Geri G, Passeron A, Heym B, Arlet JB, Pouchot J, Capron L, et al. Paradoxical reactions during treatment of tuberculosis with extrapulmonary manifestations in HIV-negative patients. Infection. 2013;41(2):537–43. https://doi.org/10.1007/s15010-012-0376-9.
• Tai ML, Nor HM, Kadir KA, Viswanathan S, Rahmat K, Zain NR, et al. Paradoxical manifestation is common in HIV-negative tuberculous meningitis. Medicine (Baltimore). 2016;95(1):e1997. https://doi.org/10.1097/md.0000000000001997. This prospective study among HIV-uninfected persons at two centers in Malaysia evaluated the frequency of paradoxical worsening of TB meningitis after treatment initiation. This phenomenon occurred in more than half of the patients, with high rates of recurrence. The frequency was higher than previous estimates. New findings on neuroimaging and clinical deterioration were the most common features of paradoxical worsening.
Meintjes G, Lawn SD, Scano F, Maartens G, French MA, Worodria W, et al. Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. Lancet Infect Dis. 2008;8(8):516–23.
Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray A, et al. Timing of initiation of antiretroviral drugs during tuberculosis therapy. N Engl J Med. 2010;362(8):697–706. https://doi.org/10.1056/NEJMoa0905848.
Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray AL, et al. Integration of antiretroviral therapy with tuberculosis treatment. N Engl J Med. 2011;365(16):1492–501. https://doi.org/10.1056/NEJMoa1014181.
Havlir DV, Kendall MA, Ive P, Kumwenda J, Swindells S, Qasba SS, et al. Timing of antiretroviral therapy for HIV-1 infection and tuberculosis. N Engl J Med. 2011;365(16):1482–91. https://doi.org/10.1056/NEJMoa1013607.
Kendall MA, Nyirenda M, Wu X, Ive P, Benson CA, Andersen JW, et al. Tuberculosis immune reconstitution inflammatory syndrome in A5221 STRIDE: timing, severity and implications for HIV-TB programs. J Acquir Immune Defic Syndr. 2014;65(4):423.
Naidoo K, Yende-Zuma N, Padayatchi N, Naidoo K, Jithoo N, Nair G, et al. The immune reconstitution inflammatory syndrome after antiretroviral therapy initiation in patients with tuberculosis: findings from the SAPiT trial. Ann Intern Med. 2012;157(5):313–24. https://doi.org/10.7326/0003-4819-157-5-201209040-00004.
•• Torok ME, Yen NT, Chau TT, Mai NT, Phu NH, Mai PP, et al. Timing of initiation of antiretroviral therapy in human immunodeficiency virus (HIV)-associated tuberculous meningitis. Clin Infect Dis. 2011;52(11):1374–83. https://doi.org/10.1093/cid/cir230. After a large study from South Africa of HIV-infected TB patients demonstrated unequivocally that early initiation of antiretroviral therapy (ART) dramatically improved survival, this study evaluated whether a similar strategy could be applied to patients with TB meningitis. In a randomized, double-blind, placebo-controlled trial, patients living with HIV and diagnosed with TB meningitis were randomized to start ART within 7 days of TB treatment or after 2 months of TB treatment. Immediate ART in patients with TB meningitis did not improve survival, and was associated with higher risk of adverese events.
Makadzange AT, Ndhlovu CE, Takarinda K, Reid M, Kurangwa M, Gona P, et al. Early versus delayed initiation of antiretroviral therapy for concurrent HIV infection and cryptococcal meningitis in sub-saharan Africa. Clin Infect Dis. 2010;50(11):1532–8. https://doi.org/10.1086/652652.
Boulware DR, Meya DB, Muzoora C, Rolfes MA, Huppler Hullsiek K, Musubire A, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med. 2014;370(26):2487–98. https://doi.org/10.1056/NEJMoa1312884.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Bourgi, Fiske and Sterling declare no conflict of interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards.
Additional information
This article is part of the Topical Collection on Central Nervous System Infections
Rights and permissions
About this article
Cite this article
Bourgi, K., Fiske, C. & Sterling, T.R. Tuberculosis Meningitis. Curr Infect Dis Rep 19, 39 (2017). https://doi.org/10.1007/s11908-017-0595-4
Published:
DOI: https://doi.org/10.1007/s11908-017-0595-4