Abstract
Despite remarkable progress in diagnosis and antibiotic therapy, mortality due to pneumonia has not changed significantly and ICU admissions are increasing. The management includes early evaluation of severity, collection of microbiological cultures, and appropriate antibiotic administration. The prognostic scores as the ATS/IDSA rule, the PIRO, or SCAP system are valuable in timely recognition of critically ill patients with community-acquired pneumonia (CAP) requiring admission to ICU. Implementation of guidelines for CAP treatment should be emphasized in order to increase survival. Guidelines for antibiotic management for severe CAP are based on illness severity, covering most likely bacterial and atypical pathogens and the level of ICU antibiotic resistance. Combination therapy suggested in patients with nonrefractory septic shock and severe sepsis pneumococcal bacteremia also. Recent studies suggest that steroid therapy may be valuable in nonrefractory septic shock from sCAP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generally, the population of severe community-acquired pneumonia (sCAP) represents 10 % of patients hospitalized with CAP, with an incidence that increases in recent years. Particularly, in a study of Woodhead et al. [1], an 128 % increase in admissions for CAP from 12.8/unit to 29.2/unit during the 9-year study period compared to a 24 % rise in total ICU admissions (p < 0.001) was reported. After ICU admission, mortality is elevated reaching up to 30–40 % and the length of hospital stay is prolonged, often with complications and chronic rehabilitation is needed.
CAP is a complex and evolving inflammatory disease, and critical deterioration could be present with respiratory failure, circulatory insufficiency, aggravation of comorbidities, or hospital-acquired illnesses.
sCAP is a progressive disease, and in the event of evolution from a local to a systemic infection, the following spectrum of sepsis-related complications may develop: sepsis, severe sepsis, septic shock, and multiple-organ dysfunction [2]. CAP is the most common cause of sepsis and septic shock worldwide. In the USA, CAP is responsible for 1.2 out of 2.05 million (59 %) yearly hospital admissions for sepsis [3]. In a interesting study including 1339 patients hospitalized for CAP in the USA and Canada, Dremsizov and colleagues [4] reported that severe sepsis developed early in 48 % of the 639 hospitalized CAP patients while 4.5 % (61 patients) of them presenting with septic shock. Additionally, delayed ICU transfer for respiratory arrest or shock is associated with 2–2.6-fold increased risk for hospital mortality compared with direct admission from the emergency department (ED) [5, 6••, 7••].
The main aim of this review is to describe the optimal treatment of patients with sCAP admitted in the ICU, in order to improving patient outcomes.
Severity Assessment: Prognostic Scores
The identification of patients with severe pneumonia requiring ICU admission is vital. The admission of a patient with CAP to the ICU is a serious and individualized decision, depending on the hospital facilities, ICU availability, disease severity, and the patient’s medical history.
Multiple scoring systems have been developed to help recognize patients with CAP at risk for ICU admission from ED. The IDSA/ATS guidelines of 2007 for the management of CAP defined a prediction rule consisting of one of two major criteria or three or more of the nine minor criteria (Table 1) that would indicate ICU admission [8]. The two major criteria of the IDSA/ATS rule refer to patients with acute respiratory failure requiring invasive mechanical ventilation (MV) or septic shock.
A new generation of scores (SCAP rule, SMART-COP, and REA-ICU), specifically developed to predict sCAP, focuses on the severity of the pneumonia on presentation rather than on age and underline diseases. The main characteristic of these scores is their high negative predictive value, in all the studies, suggesting that these scores could be more applicable for the exclusion of sCAP than categorizing pneumonia patients into severity classes.
In Australia, Charles and colleagues [9] developed the SMART-COP, a relatively simple eight-point-based severity tool to predict which patients will require intensive respiratory or vasopressor support (IRVS) during hospitalization.
A mixed French-American score called the REA-ICU index [6••] identified 11 baseline characteristics to be predictors for early ICU admission between first and third day from ED or ward. The REA-ICU index stratified patients into four risk classes with an ICU admission rate on days 1 to 3 ranging from 0.7 to 31 %.
Other investigators developed a severity assessment tool to predict mortality in CAP based on the predisposition, insult, response, organ dysfunction (PIRO) and had a better performance than APACHE II and ATS/IDSA criteria in patients with sCAP [10, 11].
There is a growing interest in the use of new biomarkers as procalcitonin [12], endothelin-1 [13], co-peptin [14], proatrial natriuretic peptide [15, 16], or adrenomedullin [17] to improve the diagnosis and stratification of CAP, combined with severity scores in some studies.
Microbiology
Streptococcus pneumoniae is the main pathogen that causes CAP worldwide, independent of age and severity [8]. Other pathogens associated with sCAP include the gram(−)s Haemophilus influenza, Klebsiella pneumoniae, from the atypicals the Legionella spp., Staphylococcus aureus and respiratory viruses. In a study of Choi et al., using PCR testing, about one third of patients with sCAP had viral infections, 9.1 % (18 of 198) of patients had bacterial-viral coinfection, but there was no difference in mortality between the two groups of patients [18]. Recently, Cilloniz and colleagues, including 362 patients, reported that polymicrobial infection was common in sCAP (11 % of patients) with respiratory viruses diagnosed in 15(39 %) of cases of polymicrobial pneumonia [19]. Mixed infections with atypical pathogens count for 5–40 % of cases, according to studies, and should be covered in the initial antimicrobial regimen.
P. aeruginosa is a frequent gram(−) pathogen in sCAP with specific risk factors, especially in those with severe COPD with frequent hospitalizations, bronchiectasis, cystic fibrosis, those taking antibiotics for a long time(>10 mg for > 1 month) and immunosuppressed patients (HIV, corticosteroid therapy, malnutrition) [20].
Multidrug-resistant pathogens (MDRs) that cause sCAP represent an emerging problem, because of the increasing number of residents living in health care facilities and the appearance of community-acquired methicillin-resistant S. aureus (CA-MRSA). Asian studies show high frequency of MDR pathogens in CAP [21], especially in elderly who received antibiotics recently or have comorbidities. In a cohort of patients presenting to the hospital with CAP complicated by respiratory failure, Schreiber et al. [22] diagnosed resistant pathogens in 33 % of the study population.
In attempts to evaluate risk factors for acquiring MDR bacteria in CAP, Aliberti et al. [23] and Shorr et al. [24••] discovered simple risk scores representing an improvement over an HCAP-based approach. Further studies are needed for validation of these scores and early identification of patients with MDR CAP.
Treatment
In order to achieve a more uniform approach toward empirical treatment of CAP, guidelines for the management of CAP have been developed in many countries and by different scientific committees in the past 20 years. The guidelines focused on the significance of timely, appropriate and aggressive management of patients presented with sCAP [8].
The two most fatal complications of CAP in the first month are respiratory failure and multiple organ dysfunction syndrome. A subanalysis of PORT was reported within 90 days after hospitalization for CAP; only half of the deaths are related to acute illness, and other factors as underlying diseases as dementia, immunosuppression, and active cancer may influence mortality [25].
Both common sense physiologic interpretation and several studies have recommended that delay in appropriate therapy with broad spectrum antibiotics is related with increased mortality in sepsis due to CAP [26]. In patients with CAP progressing to septic shock, delay must not be >1 h after diagnosis [1, 25]. In a multicenter study including 2154 septic shock patients, Kumar et al. [27] demonstrated that initiation of appropriate antibiotic therapy into the first hour of documented hypotension was associated with increased hospital survival.
Initial Resuscitation
The initial measures includes blood cultures before antibiotics, fluid resuscitation with 30 mL/kg/body weight to target a mean arterial blood pressure (MAP) of at least 65 mmHg, central venous pressure (CVP) of 8–12 mmHg, and a central venous oxygen saturation (ScvO2) < 70 % within 6 h of diagnosis.
Resuscitation requires the use of intravenous fluids and vasopressors, oxygen therapy and MV provided as necessary.
Aggressive fluid resuscitation is considered the most crucial part of all the major interventions forming the Surviving Sepsis Campaign (SSC) bundles. The recommended choice is the colloids or crystalloids—in fluid challenge aliquots of 1000 mL of crystalloid or 300–500 mL—to reach a minimum of 30 ml/kg of crystalloids and not the hydroyethyl starch (HES) [2]. Furthermore, the use of albumin-containing solutions for the resuscitation of patients with sepsis was associated with lower mortality compared with other fluid resuscitation regimens, in a meta-analysis published in 2011 [28].
Another suggestion of resuscitation is the addition of resolution of lactate elevation or lactate clearance—especially during the first 6 h—to the SSC resuscitation bundles [29].
One of the benefits of aggressive fluid therapy is a 15 % reduction in vasopressor use during the first 6 h. This early reduction in vasopressor therapy further reduces the need for controversial therapies such as vasopressin and corticosteroid therapy (Table 2).
When aggressive fluid administration cannot provide an adequate MAP, vasopressors should be promptly initiated, as the longer that hypotension goes on, the lower the survival rate. The SSC [2] suggests to start with norepinephrine and add epinephrine or vasopressin (0.03 U/min) when is needed to restore MAP > 70 mmHg. Dopamine should be used only in patients with absolute or relative bradycardia.
This is followed by early hemodynamic optimization of DO2 guided by preload (fluid administration guided by CVP), afterload (vasopressor use based on MAP), arterial oxygen content (CaO2), blood transfusion for low central ScvO2 and contractility (augmentation by inotropes for a persistently low SvO2) [2].
General Supportive Care
Recommendations for (a) blood transfusion if hemoglobin is <7 g/dL in the absence of tissue hypoperfusion, ischemic coronary artery disease, or acute hemorrhage and (b) blood glucose management, to obtain blood glucose ≤180 mg/dL [30].
Ventilation: Invansive (MV) or Noninvansive (NIV)
The delivery of oxygen is paramount and begins with either supplemental oxygen, or noninvasive or invasive positive pressure mechanical ventilation (PPMV).
The indications are severe hypoxia, hypercapnia, severe metabolic acidosis, altered mental status, and a persistently low ScvO2.
During mechanical ventilation, the use of a lung protective-ventilation strategy (with low VT 6–8 ml/kg PBW and plateau pressure goal % 30 cm H2O) in patients who have ALI/ARDS, including those who have sCAP is recommended [5].
The benefits of noninvasive ventilation (NIV) in ARF of patients with sCAP have been demonstrated with different degrees of evidence in several studies.
In one of the first studies, Confalonieri et al. report that in patients with sCAP and ARF (refractory hypoxemia and/or hypercapnia with acidosis), NIV was found useful to significantly decrease endotracheal intubation rate and length of ICU stay and mortality in the subgroup of COPD patients [31]. Later, in a study from three hospitals in Spain, including 105 patients with hypoxemic ARF, Ferrer et al. confirmed the benefits of NIV in avoiding intubation (OR 0.20; p = 0.003), and improving 90-day survival (p = 0.025), in patients with severe respiratory failure [32].
Antibiotic Therapy
Antimicrobial treatment for sCAP remains largely empirical, targeting the most likely pathogens.
Before the initiation of antibiotics, at least two samples of blood cultures should be obtained, one intravenous and the other from a vascular catheter.
According to the guidelines for the management of sCAP in Europe and USA [8, 20], patients should be stratified CAP according to the presence of risk factors for P. aeruginosa infection (Table 2).
-
For patients without pseudomonal risk an intravenous β-lactam plus either a macrolide or a respiratory fluoroquinolone is recommended.
-
If pseudomonal infection is a consideration, an antipseudomonal β-lactam should be combined with either levofloxacin or ciprofloxacin or the antipseudomonal β-lactam can be combined with both an aminoglycoside and either azithromycin or a respiratory quinolone.
-
Anaerobic coverage with the combination of a cephalosporin with clindamycin is indicated only in patients with a risk for aspiration, such as alcoholism, loss of consciousness and oropharyngeal dysphagia due to neurological disease.
Combination Antibiotic Therapy
The controversy regarding combination antibiotic therapy in patients with sCAP is coming from the lack of randomized controlled trials (RCT) comparing combination therapy versus monotherapy in patients with sCAP in the ICU [5].
Initially, Waterer et al. [33] reported in a study of 225 patients with severe bacteremic pneumococcal pneumonia that mortality was threefold greater when a regimen of single effective therapy was used than in a regimen of dual effective therapy. A recently published RCT [34], consisting of 580 adults with moderately sCAP, did not find noninferiority of β-lactam monotherapy compared to β-lactam and a macrolide regimen regarding outcomes (mortality, complications, length of stay, recurrence of pneumonia).
From several studies, it has become increasingly clear that the advantage of dual antibiotic therapy in sCAP is seen mainly when a macrolide is part of the combination, especially in pneumococcal bacteremia [35•]. This effect is presumed to be secondary to the immunomodulatory effect rather than the antimicrobial effects of macrolides.
A multicenter study from Europe which include 270 patients with sCAP and shock confirmed that patients who were treated with a third-generation cephalosporin plus a macrolide compared to those treated with FQ had a higher 28-day in-ICU survival (hazard ratio [HR] = 2.69, 95 % CI 1.09–2.60) [36••]. But, combination therapy did not increased survival in patients without shock. In addition, Martin Loeches et al., in a prospective observational study of 208 patients with sCAP from 27 ICUs, showed that combination therapy with macrolides associated with lower ICU mortality in intubated patients [37••].
The guidelines recommend antibiotic therapy for 7–10 days. Longer treatments suggesting to slow response, nondrainable focci, S. aureus bacteremia, some fungal or viral infections and immunological deficiencies (neutropenia).
The recent SCC guidelines correlate the levels of biomarkers, especially procalcitonin (PCT), with the duration of antibiotic treatment (de-escalation or stop treatment) and when considering the diagnosis of candidiasis.
After the first 6 h of resuscitation, we must think of four points: (i) fluid resuscitation must be continued; (ii) further or additional vassopressors, as dobutamine, epinephrine, or vasopressin; (iii) adjunctive therapies, as corticoids; and (iv) reevaluation of antibiotic choices.
When the causative pathogen has been identified, de-escalation should be performed by selecting the most effective and safe antibiotic against the causative pathogen.
GCs and the Inflammatory Response
Despite decades of experimental animal and human trials, the role of corticosteroid therapy in sCAP remains uncertain and controversial, more vague than in septic shock.
Firstly, a pilot study by Monton et al. [38], including intubated patients with sCAP, suggested that treatment with GCs decrease systemic and lung inflammatory responses in mechanically ventilated patients with severe pneumonia. On the contrary, a large multicentric RCT published in 2008, involving 499 patients with septic shock, concluded that hydrocortisone at a physiological dose does not decrease mortality, even if the drug hastens reversal of shock [39••].
Prospective, randomized trials referring to GCs in sCAP are the Confalonieri et al. [40] in 2005, Sabry and Omar [41] and Fernandez-Serrano et al. [42] in 2011, and Torres et al. [43••] in 2015.
The results of the last RCT of Torres et al. [43••] support that the addition of low dosages of GCs in the initial antibiotic empiric regimen can diminish inflammatory response and reduce the risk of treatment failure in patients with sCAP.
Meduri et al. [44] in a RCT with 91 patients with early ARDS due to sCAP showed that patients treated with prolonged methylprednisolone infusion (1 mg/kg/day) had a higher rate of extubation (p = 0.07) and significant reduction in C-reactive protein levels( p = 0.06) by day 7. GC treatment reduce the duration of MV (p = 0.13) and ICU mortality (p = 0.3) but not significantly.
These trials that investigated steroid treatment for sCAP for at least 5 days showed improvement in oxygenation (PO2/FiO2); however, only the trial by Confalonieri et al. found a mortality benefit.
The value of GCs seems to have been proven in bacterial meningitis and pneumonia caused by Pneumocystis jiroveci.
For patients with sCAP, risk assessment should take into consideration patients with severe chronic obstructive pulmonary disease and asthma that may have received intermittent treatment with steroids before their septic episode, and, therefore, have iatrogenic adrenal insufficiency, needing steroid replacement [8].
Recent guideline for sepsis recommended that corticosteroids are not to be used for treating septic shock, unless the patients’ endocrine function is not intact or that patients have corticosteroid history [28].
Conclusion
When managing patients with CAP, implementation of guidelines for CAP treatment should be emphasized in order to increase survival. In sCAP, scientific evidence is limited until now.
The use of appropriate initial broad antimicrobial therapy, the combination treatment in septic patients, the de-escalation when causative pathogen has been identified and the efficacy of using steroids in the nonrefractory septic patient have lead to considerable advance in pneumonia’s outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Woodhead M, Welch CA, Harrison DA, Bellingan G, Ayres JG. Community-acquired pneumonia on the intensive care unit: Secondary analysis of 17,869 cases in the ICNARC Case Mix Programme Database. Crit Care. 2006;10(2):S1.
Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign guidelines committee including the pediatric subgroup. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2012;39(2):165–228.
Centers for Disease Control and Prevention. Number and rate of discharges from short-stay hospitals and of days of care, with average length of stay and standard error, by selected first-listed diagnostic categories: United States, 2010. www.cdc.gov/nchs/data/nhds/2average/2010ave2_firstlist.pdf Date last accessed: 2013. Date last updated: 2010.
Dremsizov T, Clermont G, Kellum JA, et al. Severe sepsis in community-acquired pneumonia: when does it happen, and do systemic inflammatory response syndrome criteria help predict course? Chest. 2006;129(4):968–78.
Leroy O, Santre C, Beuscart C, et al. A five-year study of severe community-acquired pneumonia with emphasis on prognosis in patients admitted to an intensive care unit. Intensive Care Med. 1995;21(1):24–31.
Renaud B, Santin A, Coma E, et al. Association between timing of intensive care unit admission and outcomes for emergency department patients with community-acquired pneumonia. Crit Care Med. 2009;37:2867–74. Secondary analysis of two multicenter studies resulting that CAP patients without major criteria for Scap would benefit from ICU admission.
Restrepo MI, Mortensen EM, Rello J, et al. Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest. 2010;137:552–7. A retrospective cohort study of 161 ICU subjects with CAP reported that late ICU admission have increased 30-day mortality after adjustment for illness severity.
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community acquired pneumonia in adults. Clin InfectDis. 2007;44 Suppl 2:S27–72.
Charles PG, Wolfe R, Whitby M, et al. Australian Community-Acquired Pneumonia Study Collaboration. SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis. 2008;47(3):375–84.
Rello J, Rodriguez A, Lisboa T, et al. PIRO score for community-acquired pneumonia: a new prediction rule for assessment of severity in intensive care unit patients with community-acquired pneumonia. Crit Care Med. 2009;37(2):456–62.
Rello J. Demographics, guidelines, and clinical experience in severe community-acquired pneumonia. Crit Care. 2008;12 Suppl 6:S2.
Schuetz P, Suter-Widmer I, Chaudri A, et al. Prognostic value of procalcitonin in community- acquired pneumonia. Eur Respir J. 2011;37:384–92.
Schuetz P, Christ-Crain M, Zimmerli W, Mueller B. Repeated measurements of endothelin-1 precursor peptides predict the outcome in community-acquired pneumonia. Intensive Care Med. 2011;37:970–80.
Kruger S, Ewig S, Kunde J, et al. C terminal provasopressin (copeptin) in patients with community-acquired pneumonia: influence of antibiotic pre-treatment: results from the German competence network CAPNETZ. J Antimicrob Chemother. 2009;64:159–62.
Christ-Crain M, Breidthardt T, Stolz D, et al. Use of B-type natriuretic peptide in the risk stratification of community-acquired pneumonia. J Intern Med. 2008;264:166–76.
Kruger S, Ewig S, Kunde J, Hartmann O, Suttorp N, Welte T. Pro-atrial natriuretic peptide and pro-vasopressin for predicting short-term and long-term survival in community-acquired pneumonia: results from the German Competence Network CAPNETZ. Thorax. 2010;65:208–14.
Christ-Crain M, Morgenthaler NG, Stolz D, et al. Pro-adrenomedullin to predict severity and outcome in community-acquired pneumonia. Crit Care. 2006;10:R96.
Choi S-H, Hong S-B, Ko G-B, et al. Viral infection in patients with severe pneumonia requiring intensive care unit admission. Am J Respir Crit Care Med. 2012;186(4):325–32.
Cillóniz C, Ewig S, Ferrer M, Polverino E, Gabarrús A, Puig de la Bellacasa J, et al. Community-acquired polymicrobial pneumonia in the intensive care unit: aetiology and prognosis. Crit Care. 2011;15(5):R209.
Woodhead M, Blasi F, Ewig S, et al. Guidelines for the management of adult lower respiratory tract infections––full version. Clin Microbiol Infect. 2011;17(6):E1–59.
Wu CL, Ku SC, Yang KY, et al. Antimicrobial drug-resistant microbes associated with hospitalized community-acquired and healthcare-associated pneumonia: a multi-center study in Taiwan. J Formos Med Assoc. 2013;112(1):31–40.
Schreiber MP, Chan CM, Shorr AF. Resistant pathogens in non-nosocomial pneumonia and respiratory failure: is it time to refine the definition of health-care-associated pneumonia? Chest. 2010;137(6):1283–8.
Aliberti S, Zanaboni AM, Blasi F. Pneumonia in the community caused by multidrug-resistant organisms: keep working on probabilistic scores. Clin Infect Dis. 2012;54:1519–20.
Shorr AF, Zilberberg MD, Reichley R, et al. Validation of a clinical score for assessing the risk of resistant pathogens in patients with pneumonia presenting to the emergency department. Clin Infect Dis. 2012;54:193–8. A study validating a previously developed score for determining the risk for an multidrug-resistant and to compare it with the HCAP definition. The score performed moderately well at classifying patients regarding their risk for an multidrug-resistant.
Mortensen EM, Coley CM, Singer DE, et al. Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med. 2002;162(9):1059–64.
Ibrahim EH, Sherman G, Ward S, et al. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118(1):146–55.
Kumar A, Ellis P, Arabi Y, et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest. 2009;136(5):1237–48.
Delaney AP, Dan A, McCaffrey J, Finfer S. The role of albumin as a resuscitation fluid for patients with sepsis: a systematic review and meta-analysis. Crit Care Med. 2011;39(2):386–91.
Nguyen HB, Kuan WS, Batech M, et al. Outcome effectiveness of the severe sepsis resuscitation bundle with addition of lactate clearance as a bundle item: a multinational evaluation. Crit Care. 2011;15(5):R229.
Wiener RS, Wiener DC, Larson RJ. Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA. 2008;300(8):933–44.
Confalonieri M, Potena A, Carbone G, et al. Acute respiratory failure in patients with severe community-acquired pneumonia. A prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1585–91.
Ferrer M, Esquinas A, Leon M, et al. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med. 2003;168:1438–44.
Waterer GW, Somes GW, Wunderink RG. Monotherapy may be suboptimal for severe bacteremic pneumococcal pneumonia. Arch Intern Med. 2001;161:1837–42.
Garin N, Genné D, Carballo S, et al. β-Lactam monotherapy vs β-lactam-macrolide combination treatment in moderately severe community-acquired pneumonia: a randomized noninferiority trial. JAMA Intern Med. 2014;174(12):1894–901.
Martínez JA, Horcajada JP, Almela M, et al. Addition of a macrolide to a β-lactam-based empirical antibiotic regimen is associated with lower in-hospital mortality for patients with bacteremic pneumococcal pneumonia. Clin Infect Dis. 2003;36:389–95. A retrospective study resulted that for patients with bacteremic pneumococcal pneumonia, not adding a macrolide to a beta-lactam-based initial antibiotic regimen is an independent predictor of in-hospital mortality.
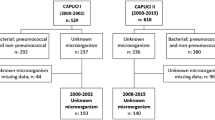
Rodríguez A, Mendia A, Sirvent J-M. for the CAPUCI Study Group. Combination antibiotic therapy improves survival in patients with community acquired pneumonia and shock. Crit Care Med. 2007;35:1493–8. A secondary analysis of the CAPUCI study group, including 529 patients with s CAP in patients with shock, combination antibiotic therapy was associated with significantly higher adjusted 28-day in-ICU survival.
Martin-Loeches I, Lisboa T, Rodriguez A, et al. Combination antibiotic therapy with macrolides improves survival in intubated patients with community-acquired pneumonia. Intensive Care Med. 2010;36:610–2. Prospective, observational cohort, multicenter study conducted in 27 ICUs of 9 European countries reported that combination therapy with macrolides was associated with lower ICU mortality.
Monton C, Ewig S, Torres A, et al. Role of glucocorticoids on inflammatory response in nonimmunosuppressed patients with pneumonia: a pilot study. Eur Respir J. 1999;14:218–20.
Sprung CL, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358:111–24. A multicenter, randomized, double-blind, placebo-controlled trial, included 251 patients with septic shock to receive 50 mg of intravenous hydrocortisone. In the hydrocortisone group, shock was reversed more quickly than in the placebo group.
Confalonieri M, Urbino R, Potena A, et al. Hydrocortisone infusion for severe community -acquired pneumonia: a preliminary randomized study. Am JRespir Crit CareMed. 2005;171:242–8.
Sabry NA, Omar EE-D. Corticosteroid sand ICU course of community acquired pneumonia in Egyptian settings. Pharmacol Pharm. 2011;2:73–81.
Fernandez-Serrano S, Dorca J, Garcia-Vidal C, et al. Effect of corticosteroids on the clinical course of community-acquired pneumonia: a randomized controlled trial. Crit Care. 2011;15:R96.
Torres A, Sibila O, Ferrer M, et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA. 2015;313(7):677–86. A RCT including 120 pts with severe CAP and high initial inflammatory response, the acute use of methylprednisolone compared with placebo decreased treatment failure.
Meduri GU, Golden E, Freire AX, et al. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest. 2007;131(4):954–63.
Compliance with ethical standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Respiratory Infections
Rights and permissions
About this article
Cite this article
Adamantia, L., Sotiria, M., Myrsini, M. et al. Managing CAP in the ICU. Curr Infect Dis Rep 17, 48 (2015). https://doi.org/10.1007/s11908-015-0504-7
Published:
DOI: https://doi.org/10.1007/s11908-015-0504-7