Abstract
Despite all published literature, controversies remain about the optimal antibiotic treatment in community-acquired pneumonia. The most debated issue is whether it is necessary to empirically start one or two antibiotics, i.e. whether or not to cover atypical agents. A review of the literature published from 2005 to present was completed, searching for new insights in antibiotic treatment in community-acquired pneumonia (CAP) focusing on monotherapy versus combined therapy. Forty-one articles were identified enrolling outpatients, and patients admitted to the ward and to the intensive care unit: 11 were meta-analyses, 8 clinical trials and 22 observational—prospective and retrospective—studies. Although controversies remain in the treatment of CAP, the use of combination therapy seems to be associated with a lower mortality in case of severe CAP that requires intensive care unit (ICU) admission, especially when a beta-lactam–macrolide association is delivered. Moreover, combination therapy is associated with better outcomes—although not always with a lower mortality—in cases of non-ICU patients with risk factors for a poor outcome, bacteraemic pneumococcal pneumonia and high suspicion of infection by atypical agents. In this setting, it appears that the best choice of treatment may be a beta-lactam–macrolide regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Community-acquired pneumonia (CAP) is a common and potentially severe disease. In Europe, it is estimated that the annual incidence in younger adults is 1.2 cases per 1000 person-years, increasing up to 14 per 1000 in patients over 65 years old [1].
In Western countries, mortality due to CAP varies widely depending from the severity of the illness: less than 1 % in individuals treated outside the hospital; around 10 % in hospitalised non-intensive care unit (ICU) patients, and up to 20 to 40 % in severe forms, i.e. when ICU admission is required [2, 3•].
In CAP, antibiotic therapy is the cornerstone of treatment; after diagnosis of pneumonia is done, an adequate antimicrobial therapy is always recommended, as it has been associated with better outcomes [4, 5]. Adequate antibiotic therapy is defined as the treatment that covers all suspected pathogens, and it is usually started on the basis of epidemiological and clinic considerations as well as local guidelines [4]. Although CAP may be caused by many pathogens, a reduced number of microorganisms are responsible for the majority of cases; classically, they are classified into typical and atypical.
Guidelines for the management of CAP were published [4, 6], and the antibiotic regimens proposed are classified according with the site of care: outpatients, ward or intensive care unit (ICU).
What Do the Guidelines Recommend?
Outpatients
In outpatients with CAP, the Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) guidelines recommend administration of a macrolide (azithromycin, clarithromycin or erythromycin) or doxycycline. If a patient received antibiotic therapy within 3 previous months, or presents with some risk factor for a higher mortality for CAP (chronic heart disease, lung or liver disease, diabetes mellitus, alcohol abuse, malignancy, asplenia or hyposplenism, immunocompromised status), the recommended antibiotic regimen is a respiratory fluoroquinolone (moxifloxacin, gemifloxacin or high-dose levofloxacin), or a combination of a beta-lactam (high-dose amoxicillin or amoxicillin–clavulanate, ceftriaxone, cefuroxime or cefpodoxime) with a macrolide. In the same setting, European guidelines recommend the administration of amoxicillin or a tetracycline. If these agents are considered contraindicated or there is a high suspicion of infection by atypical agents, the indication is monotherapy with a macrolide or a respiratory fluoroquinolone. Both American and European guidelines suggest considering the local flora pattern of antibiotic resistance.
Ward
In the case of patients with CAP who require hospitalisation, the IDSA/ATS guidelines suggest administration of a respiratory fluoroquinolone, and a beta-lactam (cefotaxime, ceftriaxone, ampicillin or ertapenem) plus a macrolide or doxycycline if patients have a high risk of pneumonia due to Gram-negative bacilli. As stated in the guidelines, monotherapy with a macrolide should be avoided because of the high rate of macrolide-resistant pneumococci. In the same setting, European guidelines suggest the administration of an aminopenicillin with or without a beta-lactamase inhibitor or a cephalosporin (ceftriaxone or cefotaxime), and to consider the addition of azithromycin or clarithromycin. In the case of high suspicion for Streptococcus pneumoniae, as several publications have demonstrated that low-level resistance to penicillin is not associated with worsened outcomes [7], penicillin G plus a macrolide could be an alternative. If those antibiotics are considered inappropriate, a respiratory fluoroquinolone may be an alternative. As stated in the European guidelines, the use of a specific antibiotic pattern should be guided by the severity of the disease (most severe cases should be treated with combined therapy) and based on considerations of allergy, intolerance, previous use of penicillins, macrolides or fluoroquinolones, cost and potential adverse effects.
Intensive Care Unit
According to both the American and the European guidelines, a patient in an ICU setting should be covered for all suspected microorganisms (resistant Streptococcus pneumoniae and atypical pathogens) because it was observed in severe CAP that an inadequate antibiotic treatment is associated with an increased mortality [8].
IDSA/ATS guidelines suggest initiating a combination regimen with a beta-lactam (cefotaxime, ceftriaxone or ampicillin–sulbactam) plus either azithromycin or a respiratory fluoroquinolone. Likewise, European guidelines suggest combination therapy in the form of a non-antipseudomonal third-generation cephalosporin (ceftriaxone or cefotaxime) plus either a macrolide (azithromycin or clarithromycin) or a respiratory fluoroquinolone. Both guidelines recommend that if an infection by methicillin-resistant Staphylococcus aureus or Pseudomonas aeruginosa is suspected, the antibiotic treatment should empirically cover these microorganisms. Conversely, it was demonstrated that the regular coverage of resistant agents did not decreased mortality [9].
Controversies regarding the optimal antibiotic regimen persist; the most debated issues are whether it is necessary to empirically cover atypical microorganisms, and if it is better to start one antibiotic or two. In the present review, all articles aimed at the study of monotherapy versus combination therapy in CAP were reviewed.
Material and Methods
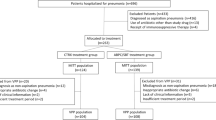
A review of the literature was performed searching for any recent article about antibiotic treatment in CAP. The search process was performed in PubMed in March 2015; articles in English, performed in adults and published from January 1, 2005 to March 1, 2015, were selected. The search key was “community-acquired pneumonia” plus “antibiotic”.
Of all the studies individuated, the ones that assessed differences in outcomes after the administration of different antibiotic regimens were selected; finally, the articles that compared monotherapy versus combination therapy or compared different patterns of combination therapy were chosen for the present review. Publications on health-care-associated pneumonia and aspiration pneumonia were excluded from the analysis. The items found in the review were then analysed and classified as meta-analysis, clinical trial or observational study.
Those articles that included either outpatients and patients proceeding from the ward were categorized in the present review as outpatients. Likewise, articles enrolling both patients from the ward and ICU patients were categorized in the present review as ward-patients.
Results
The PubMed search obtained 2233 results. The screen resulted in a total of 41 selected articles: 11 meta-analyses, 8 clinical trials and 22 observational—prospective and retrospective—studies.
What Is New in the Literature?
Since 2005, several studies were published assessing monotherapy versus combination therapy in CAP.
Outpatients
Four papers were identified: three meta-analyses and one observational study (Table 1).
The most recent article is a Cochrane meta-analysis published in 2014 by Pakhale et al. [10] that explored changes in mortality by using different antibiotic prescriptions—in monotherapy and combined therapy—in outpatients with CAP: 11 clinical trials were included without observing differences in mortality or in the incidence of adverse effects. A meta-analysis by Skalsky et al. [11] included 16 trials enrolling both outpatients and ward patients exploring whether the administration of a macrolide-based versus fluoroquinolone-based regimen was associated with different outcomes. As a conclusion, no differences were observed in all-cause mortality between the two regimens of antibiotics. Treatment failure and microbiological failure decreased significantly when a fluoroquinolone was administered, and a higher incidence of adverse event and antibiotic discontinuation was associated with macrolide prescription, mainly attributed to digestive complications. Thus, although these finding were not associated with changes in mortality, authors conclude that fluoroquinolones may be superior when compared with macrolides.
Finally, An et al. in 2010 published a meta-analysis [12] comparing outcomes after administration of moxifloxacin versus a beta-lactam-based combination with a macrolide. Seven trials were identified including around 4000 patients. Again, no differences were observed regarding mortality, clinical success and adverse effects rates. Conversely, microbiological failure was significantly lower with moxifloxacin.
One observational study by Ye et al. [13] compared outcome and costs of treatment in outpatients with CAP after administration of levofloxacin (500 or 750 mg) versus macrolides: Although the rate of treatment failure was lower for the levofloxacin group, no differences were observed in term of costs, CAP-related hospitalisations and mortality.
Ward
Twenty-seven articles were identified: 7 meta-analyses (Table 2), 7 clinical trials (Table 3) and 13 observational studies (Table 4).
A Cochrane meta-analysis by Eliakim-Raz et al. [16] explored changes in mortality depending on coverage for atypical agents; 28 clinical trials were included, and no difference in mortality or in the development of adverse effects was observed. Patients who received atypical coverage showed a non-significant trend toward clinical and microbiological resolution. This trend was statistically significant in patients with pneumonia due to Legionella pneumophila, still without observing changes in mortality.
Two meta-analyses found a decreased mortality after addition of a macrolide to the treatment; Nie et al. [14] compared a beta-lactam–macrolide regimen versus beta-lactam monotherapy in a meta-analysis that only included observational studies enrolling ward and ICU patients. In the conclusions, combined therapy resulted in a significant decrease of mortality. Likewise, Asadi et al. [18] in a meta-analysis that included 23 studies of in-hospital patients with CAP—either clinical trials or observational studies—observed a significant reduction of mortality in individuals who received a macrolide regimen. Importantly, this trend was not significant when only the clinical trials were analysed, or in patients who received guideline-concordant antibiotics.
Three meta-analyses compared outcomes after administration of a respiratory fluoroquinolone versus a beta-lactam regimen. After comparing oral gemifloxacin with a beta-lactam regimen in mild to moderately severe patients with CAP and bronchial exacerbations, Zhang et al. [15] observed a comparable mortality between the two arms. Gemifloxacin was associated with a higher rate of adverse effects, mostly in form of gastrointestinal complications. Two other meta-analyses in 2008 and 2012 achieved similar conclusions; Vardakas et al. [20] compared the use of monotherapy with fluoroquinolones versus a combination beta-lactam regimen documenting a comparable mortality, although a higher eradication rate after fluoroquinolone administration was observed. Yuan et al. [17] observed a comparable mortality and a higher rate of microbial eradication after administration of moxifloxacin versus a beta-lactam antibiotic regimen.
Finally, a meta-analysis by Varner et al. [19] explored the benefit of the addition of rifampicin to the standard treatment of CAP due to L. pneumophila, without observing different outcomes. Authors concluded that rifampicin should not be added to treat CAP due to Legionella spp. unless pneumonia is severe or is refractory to the standard treatment.
In the last years, several clinical trials were published assessing outcomes after comparing monotherapy versus combination therapy. In a recent study, Postma et al. [21] did not find differences in mortality after comparing fluoroquinolone monotherapy versus beta-lactam monotherapy versus beta-lactam–macrolide combination in non-ICU hospitalised patients; thus, authors concluded that beta-lactam monotherapy was non-inferior to other regimens. Garin et al. [22] obtained similar conclusions: No differences in mortality, length of stay and ICU admission were observed after administration of a beta-lactam alone versus a beta-lactam–macrolide regimen. Patients with a pneumonia severity index (PSI) score of IV or V and patients infected by atypical microorganisms presented delayed clinical stability with monotherapy. Other studies documented similar conclusions; a comparable mortality and adverse effect rates, and a higher eradication rate in the fluoroquinolone group were observed by Lee et al. [23] after comparing high-dose levofloxacin versus ceftriaxone plus azithromycin. No differences in mortality or an increased eradication rate in the fluoroquinolone arm were found when comparing a fluoroquinolone versus a beta-lactam plus a macrolide [25–27]. One clinical trial by Torres et al. [24] did not observe differences in mortality after comparing moxifloxacin monotherapy with ceftriaxone plus levofloxacin in a cohort of CAP patients including 10 % with severe pneumonia (PSI score IV or V).
Thirteen observational studies were identified. Several studies, either prospective or retrospective, compared fluoroquinolone monotherapy with a beta-lactam monotherapy regimen. Asadi et al. [28] did not find a difference in mortality after comparing fluoroquinolone monotherapy with a beta-lactam–macrolide regimen, in ward and ICU patients. When comparing high-dose levofloxacin with ceftriaxone plus azithromycin, a similar mortality was observed, but a decrease in costs of treatment was documented after fluoroquinolone administration [30, 33–35, 38, 39].
A decreased mortality was observed after the administration of a beta-lactam–macrolide combination when compared with beta-lactam monotherapy [29, 32, 40]. In the paper by Rodrigo et al., these conclusions were not observed in the mildest forms of CAP. On the other hand, in patients with severe CAP with pneumococcal bacteraemia, a difference in mortality was not found between the administration of a beta-lactam plus a macrolide and monotherapy with a beta-lactam [37].
Two observational studies explored changes in mortality after the addition of a macrolide. Restrepo et al. [31] found that patients with CAP and severe sepsis had a decreased mortality when a macrolide was added. Metersky et al. [36] achieved the same conclusions in patients with bacteraemic CAP admitted to the ward or in the ICU.
Intensive Care Unit
Ten studies were identified: one meta-analysis, one clinical trial and eight observational studies (Table 5).
In 2014, Sligl et al. [41] published a meta-analysis exploring outcomes after administration of combined therapy with a macrolide regimen versus monotherapy or combined therapy without a macrolide; 28 observational studies enrolling critically ill patients with CAP were included, accounting for nearly 10,000 patients. As a conclusion, mortality was lower in patients who received combination therapy with a macrolide, when compared with that in those who received monotherapy or combination therapy without a macrolide.
Leroy et al. [42] performed a clinical trial enrolling 398 critical patients without shock or a requirement for mechanical ventilation and compared levofloxacin with ceftriaxone plus ofloxacin; no differences in mortality, clinical resolution and adverse event rate were observed.
Five observational studies obtained similar results. Our group of research in pneumonia, in a case-control analysis published in 2014 [3], observed an increased survival after combination therapy; this association was found in the main cohort and in all analysed subgroups: patients with shock or a need for mechanical ventilation, and critically ill patients without shock or a need for mechanical ventilation. Adrie et al. [43] documented a decreased mortality after combination therapy; interestingly, this association was stronger in patients with shock or with pneumococcal infection. Rello et al. documented the same trend [45] in patients with severe CAP by L. pneumophila and shock, Rodriguez et al. [47] in patients with severe CAP with shock and Martin-Loeches et al. [46] in intubated patients with CAP.
Only one study published by Harbarht in 2005 [48] documented a comparable mortality between monotherapy and combination therapy in patients with CAP and severe sepsis or shock.
Finally, two studies explored outcomes after administration of a beta-lactam–macrolide regimen compared with a beta-lactam–fluoroquinolone regimen; Mortensen et al. [49] found a lower mortality after administration of the macrolide-based regimen in a cohort of 172 critical patients with severe CAP. Conversely, Wilson et al. [44] did not find differences in mortality in elderly patients with CAP. It was noteworthy that a higher length of stay was documented in the beta-lactam–fluoroquinolone group.
Discussion
In the present article, we reviewed the available literature regarding monotherapy versus combined therapy in CAP. Although recent publications have not resolved all the remaining controversies, a majority of the meta-analyses and the observational studies support combination therapy with macrolide therapy, but the outcomes measured in clinical trials did not favour either arm.
In summary, outpatients with CAP without risk factors for a poor clinical outcome did not benefit from combined therapy; hence, monotherapy with either a macrolide, a fluoroquinolone or a beta-lactam may be proposed as no differences in mortality were observed by any specific antibiotic class. This controversy reflects the differences between the European and American guidelines. In fact, unlike the American guidelines, the European guidelines do not recommend empiric atypical coverage as a first-line treatment.
On one side, fluoroquinolone administration appears to be associated with a higher eradication rate, a lower treatment failure and possibly less cost of treatment; however, concerns about an increased resistance rate after fluoroquinolone administration have been raised [50]. In the case of a social environment with high rates of pulmonary tuberculosis, the empiric use of a fluoroquinolone could actually mask pulmonary tuberculosis delaying its diagnosis [51]. Thus, antibiotic prescription should be done considering local epidemiological data, i.e. the most frequent aetiologies of CAP and the local resistance pattern.
In the case of outpatients with CAP and with risk factors for poor clinical evolution, there is evidence supporting atypical coverage, although no differences in mortality were observed, and there was a decreased cost of treatment because of reduced treatment failures and secondary hospital admissions. Although the American guidelines recommend a fluoroquinolone or a beta-lactam plus a macrolide equally, some authors advocate the use of a beta-lactam plus macrolide combination. A decision should be guided by local guidelines based on epidemiological data.
In case of a hospitalised non-ICU patient, contrasting conclusions do not allow supporting the administration of monotherapy rather than combination therapy. As a general indication, in case of a mild to moderate pneumonia without risk factors for a poor clinical evolution, the use of a beta-lactam or a fluoroquinolone in monotherapy is probably the best choice. Conversely, in case of moderate to severe CAP with PSI score of IV or V, bacteraemia due to Streptococcus pneumoniae, the presence of risk factors for a poor outcome, or a high suspicion of atypical pneumonia, the use of beta-lactam monotherapy is probably not enough. Again, because of the current lack of evidence, the use of a fluoroquinolone monotherapy rather than a beta-lactam and macrolide association should be based on local epidemiological considerations. It is noteworthy that levofloxacin 750 mg per day is more effective than standard dose (500 mg), without an increase of adverse effects [22].
Finally, in case of severe CAP and ICU admission, stronger evidence for promoting the use of combined therapy was published. In fact, a meta-analysis and several observational studies documented an increased survival after dual antibiotic administration. This statement seems to be conclusive in patients with septic shock, although it was not always confirmed in the rest of ICU patients. However, despite the contrasting results in ICU patients without shock and because of the high mortality of severe CAP, it seems safer to administer combination therapy to all ICU patients with CAP. Furthermore, according with the meta-analysis of Sligl et al., the combination regimen associated with the highest survival appears to be a beta-lactam plus a macrolide as opposed to without a macrolide.
The main argument to justify combination therapy in mild to moderate pneumonia is the coverage of atypical agents; although contrasting results were obtained regarding mortality, it appears that in certain subgroups (i.e. the presence of risk factors for a poor outcome or bacteraemic pneumococcal pneumonia), atypical coverage is likely beneficial in terms of cost of treatment, eradication rate and clinical resolution. Alternatively, in case of severe CAP, the use of combined therapy is almost always associated with a decreased mortality; in fact, it was observed that the lack of atypical coverage in atypical pneumonia was associated with an increased mortality [52]; moreover, the association between macrolide use and a reduced mortality may be explainable by the antiinflammatory effects attributed to macrolides [41, 46]. In fact, severe CAP is often associated with sepsis or septic shock, and macrolide administration may decrease the inflammatory reaction. A reason that might explain why not all studies observed a reduced mortality after macrolide administration is because only patients with a high inflammatory response may benefit from it. However, this is a hypothesis and should be confirmed with a well-designed randomised controlled trial.
The use of combined therapy aroused concerns about the development of antibiotic resistance. In the present review, only one study [43] explored this issue, without differences in the development of new bacterial resistances after either monotherapy or combination therapy. Follow-up studies exploring microbial resistance after monotherapy or combination therapy would be beneficial.
Conclusions
Although many controversies remain in the optimal treatment of CAP, the use of combined therapy seems to be associated with an improved mortality in cases of severe CAP that requires ICU admission, especially when a beta-lactam–macrolide is prescribed. Moreover, it appears that combination therapy may be associated with better outcomes in cases of outpatient or ward hospitalised patients with risk factors for a poor outcome, with bacteraemic pneumococcal pneumonia and with a high suspicion of infection by atypical agents. In this setting, it appears that the best choice of treatment may be a beta-lactam–macrolide regimen.
In the next years, forthcoming challenges will be to better identify the subgroups of patients that are benefited by combination therapy, and to study the impact of monotherapy and combination therapy in the emergence of new antimicrobial resistances.
Abbreviations
- CAP:
-
Community-acquired pneumonia
- ICU:
-
intensive care unit
- PSI:
-
Pneumonia severity index
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Torres A, Peetermans WE, Viegi G, Blasi F. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax. 2013;68(11):1057–65.
Nair GB, Niederman MS. Community-acquired pneumonia: an unfinished battle. Med Clin N Am. 2011;95(6):1143–61.
Gattarello S, Borgatta B, Solé-Violán J, Vallés J, Vidaur L, Zaragoza R, et al. Decrease in mortality in severe community-acquired pneumococcal pneumonia: impact of improving antibiotic strategies (2000-2013). Chest. 2014;146(1):22–31.
Woodhead M, Blasi F, Ewig S, Garau J, Huchon G, Ieven M, et al. Guidelines for the management of adult lower respiratory tract infections—full version. Clin Microbiol Infect. 2011;17 Suppl 6:E1–59.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44 Suppl 2:S27–72.
Iannini PB, Paladino JA, Lavin B, Singer ME, Schentag JJ. A case series of macrolide treatment failures in community acquired pneumonia. J Chemother. 2007;19:536–45.
Rosón B, Carratalà J, Fernández-Sabé N, Tubau F, Manresa F, Gudiol F. Causes and factors associated with early failure in hospitalized patients with community-acquired pneumonia. Arch Intern Med. 2004;164(5):502–8.
Griffin AT, Peyrani P, Wiemken TL, Ramirez JA, Arnold FW. Empiric therapy directed against MRSA in patients admitted to the intensive care unit does not improve outcomes in community-acquired pneumonia. Infection. 2013;41(2):517–23.
Pakhale S, Mulpuru S, Verheij TJ, Kochen MM, Rohde GG, Bjerre LM. Antibiotics for community-acquired pneumonia in adult outpatients. Cochrane Database Syst Rev. 2014;10:CD002109.
Skalsky K, Yahav D, Lador A, Eliakim-Raz N, Leibovici L, Paul M. Macrolides vs. quinolones for community-acquired pneumonia: meta-analysis of randomized controlled trials. Clin Microbiol Infect. 2013;19(4):370–8.
An MM, Zou Z, Shen H, Gao PH, Cao YB, Jiang YY. Moxifloxacin monotherapy versus beta-lactam-based standard therapy for community-acquired pneumonia: a meta-analysis of randomised controlled trials. Int J Antimicrob Agents. 2010;36(1):58–65.
Ye X, Sikirica V, Schein JR, Grant R, Zarotsky V, Doshi D, et al. Treatment failure rates and health care utilization and costs among patients with community-acquired pneumonia treated with levofloxacin or macrolides in an outpatient setting: a retrospective claims database analysis. Clin Ther. 2008;30(2):358–71.
Nie W, Li B, Xiu Q. β-Lactam/macrolide dual therapy versus β-lactam monotherapy for the treatment of community-acquired pneumonia in adults: a systematic review and meta-analysis. J Antimicrob Chemother. 2014;69(6):1441–6.
Zhang L, Wang R, Falagas ME, Chen LA, Liu YN. Gemifloxacin for the treatment of community-acquired pneumonia and acute exacerbation of chronic bronchitis: a meta-analysis of randomized controlled trials. Chin Med J (Engl). 2012;125(4):687–95.
Eliakim-Raz N, Robenshtok E, Shefet D, Gafter-Gvili A, Vidal L, Paul M. Empiric antibiotic coverage of atypical pathogens for community-acquired pneumonia in hospitalized adults. Cochrane Database Syst Rev. 2012;9:CD004418.
Yuan X, Liang BB, Wang R, Liu YN, Sun CG, Cai Y, et al. Treatment of community-acquired pneumonia with moxifloxacin: a meta-analysis of randomized controlled trials. J Chemother. 2012;24(5):257–67.
Asadi L, Sligl WI, Eurich DT, Colmers IN, Tjosvold L, Marrie TJ, et al. Macrolide-based regimens and mortality in hospitalized patients with community-acquired pneumonia: a systematic review and meta-analysis. Clin Infect Dis. 2012;55(3):371–80.
Varner TR, Bookstaver PB, Rudisill CN, Albrecht H. Role of rifampin-based combination therapy for severe community-acquired Legionella pneumophila pneumonia. Ann Pharmacother. 2011;45(7-8):967–76.
Vardakas KZ, Siempos II, Grammatikos A, Athanassa Z, Korbila IP, Falagas ME. Respiratory fluoroquinolones for the treatment of community-acquired pneumonia: a meta-analysis of randomized controlled trials. CMAJ. 2008;179(12):1269–77.
Postma DF, van Werkhoven CH, van Elden LJ, Thijsen SF, Hoepelman AI, Kluytmans JA, et al. Antibiotic treatment strategies for community-acquired pneumonia in adults. N Engl J Med. 2015;372(14):1312–23.
Garin N, Genné D, Carballo S, Chuard C, Eich G, Hugli O, et al. β-Lactam monotherapy vs β-lactam-macrolide combination treatment in moderately severe community-acquired pneumonia: a randomized noninferiority trial. JAMA Intern Med. 2014;174(12):1894–901.
Lee JH, Kim SW, Kim JH, Ryu YJ, Chang JH. High-dose levofloxacin in community-acquired pneumonia: a randomized, open-label study. Clin Drug Investig. 2012;32(9):569–76.
Torres A, Garau J, Arvis P, Carlet J, Choudhri S, Kureishi A, et al. Moxifloxacin monotherapy is effective in hospitalized patients with community-acquired pneumonia: the MOTIV study—a randomized clinical trial. Clin Infect Dis. 2008;46(10):1499–509.
Lin TY, Lin SM, Chen HC, Wang CJ, Wang YM, Chang ML, et al. An open-label, randomized comparison of levofloxacin and amoxicillin/clavulanate plus clarithromycin for the treatment of hospitalized patients with community-acquired pneumonia. Chang Gung Med J. 2007;30(4):321–32.
Xu S, Xiong S, Xu Y, Liu J, Liu H, Zhao J, et al. Efficacy and safety of intravenous moxifloxacin versus cefoperazone with azithromycin in the treatment of community acquired pneumonia. J Huazhong Univ Sci Technol Med Sci. 2006;26(4):421–4.
Portier H, Brambilla C, Garre M, Paganin F, Poubeau P, Zuck P. Moxifloxacin monotherapy compared to amoxicillin-clavulanate plus roxithromycin for nonsevere community-acquired pneumonia in adults with risk factors. Eur J Clin Microbiol Infect Dis. 2005;24(6):367–76.
Asadi L, Eurich DT, Gamble JM, Minhas-Sandhu JK, Marrie TJ, Majumdar SR. Impact of guideline-concordant antibiotics and macrolide/β-lactam combinations in 3203 patients hospitalized with pneumonia: prospective cohort study. Clin Microbiol Infect. 2013;19(3):257–64.
Rodrigo C, Mckeever TM, Woodhead M. Single versus combination antibiotic therapy in adults hospitalised with community acquired pneumonia. Thorax. 2013;68(5):493–5.
Frei CR, Jaso TC, Mortensen EM, Restrepo MI, Raut MK, Oramasionwu CU, et al. Medical resource utilization among community-acquired pneumonia patients initially treated with levofloxacin 750 mg daily versus ceftriaxone 1000 mg plus azithromycin 500 mg daily: a US-based study. Curr Med Res Opin. 2009;25(4):859–68.
Restrepo MI, Mortensen EM, Waterer GW, Wunderink RG, Coalson JJ, Anzueto A. Impact of macrolide therapy on mortality for patients with severe sepsis due to pneumonia. Eur Respir J. 2009;33(1):153–9.
Bratzler DW, Ma A, Nsa W. Initial antibiotic selection and patient outcomes: observations from the National Pneumonia Project. Clin Infect Dis. 2008;47 Suppl 3:S193–201.
Bhavnani SM, Ambrose PG. Cost-effectiveness of oral gemifloxacin versus intravenous ceftriaxone followed by oral cefuroxime with/without a macrolide for the treatment of hospitalized patients with community-acquired pneumonia. Diagn Microbiol Infect Dis. 2008;60(1):59–64.
Lloyd A, Holman A, Evers T. A cost-minimisation analysis comparing moxifloxacin with levofloxacin plus ceftriaxone for the treatment of patients with community-acquired pneumonia in Germany: results from the MOTIV trial. Curr Med Res Opin. 2008;24(5):1279–84.
Lodise TP, Kwa A, Cosler L, Gupta R, Smith RP. Comparison of beta-lactam and macrolide combination therapy versus fluoroquinolone monotherapy in hospitalized Veterans Affairs patients with community-acquired pneumonia. Antimicrob Agents Chemother. 2007;51(11):3977–82.
Metersky ML, Ma A, Houck PM, Bratzler DW. Antibiotics for bacteremic pneumonia: improved outcomes with macrolides but not fluoroquinolones. Chest. 2007;131(2):466–73.
Dwyer R, Ortqvist A, Aufwerber E, Henriques Normark B, Marrie TJ, Mufson MA, et al. Addition of a macrolide to a ss-lactam in bacteremic pneumococcal pneumonia. Eur J Clin Microbiol Infect Dis. 2006;25(8):518–21.
Welte T, Petermann W, Schürmann D, Bauer TT, Reimnitz P, MOXIRAPID Study Group. Treatment with sequential intravenous or oral moxifloxacin was associated with faster clinical improvement than was standard therapy for hospitalized patients with community-acquired pneumonia who received initial parenteral therapy. Clin Infect Dis. 2005;41(12):1697–705.
Querol-Ribelles JM, Tenías JM, Querol-Borrás JM, Labrador T, Nieto A, González-Granda D, et al. Levofloxacin versus ceftriaxone plus clarithromycin in the treatment of adults with community-acquired pneumonia requiring hospitalization. Int J Antimicrob Agents. 2005;25(1):75–83.
García Vázquez E, Mensa J, Martínez JA, Marcos MA, Puig J, Ortega M, et al. Lower mortality among patients with community-acquired pneumonia treated with a macrolide plus a beta-lactam agent versus a beta-lactam agent alone. Eur J Clin Microbiol Infect Dis. 2005;24(3):190–5.
Sligl WI, Asadi L, Eurich DT, Tjosvold L, Marrie TJ, Majumdar SR. Macrolides and mortality in critically ill patients with community-acquired pneumonia: a systematic review and meta-analysis. Crit Care Med. 2014;42(2):420–32.
Leroy O, Saux P, Bédos JP, Caulin E. Comparison of levofloxacin and cefotaxime combined with ofloxacin for ICU patients with community-acquired pneumonia who do not require vasopressors. Chest. 2005;128(1):172–83.
Adrie C, Schwebel C, Garrouste-Orgeas M, Vignoud L, Planquette B, Azoulay E, et al. Article Was Written on behalf of the Outcomerea Study Group. Initial use of one or two antibiotics for critically ill patients with community-acquired pneumonia: impact on survival and bacterial resistance. Crit Care. 2013;17(6):R265.
Wilson BZ, Anzueto A, Restrepo MI, Pugh MJ, Mortensen EM. Comparison of two guideline-concordant antimicrobial combinations in elderly patients hospitalized with severe community-acquired pneumonia. Crit Care Med. 2012;40(8):2310–4.
Rello J, Gattarello S, Souto J, Sole-Violan J, Valles J, Peredo R, et al. Community-acquired Legionella Pneumonia in the intensive care unit: Impact on survival of combined antibiotic therapy. Med Intensiva. 2013;37(5):320–6.
Martin-Loeches I, Lisboa T, Rodriguez A, Putensen C, Annane D, Garnacho-Montero J, et al. Combination antibiotic therapy with macrolides improves survival in intubated patients with community-acquired pneumonia. Intensive Care Med. 2010;36(4):612–20.
Rodríguez A, Mendia A, Sirvent JM, Barcenilla F, de la Torre-Prados MV, Solé-Violán J, et al. Combination antibiotic therapy improves survival in patients with community-acquired pneumonia and shock. Crit Care Med. 2007;35(6):1493–8.
Harbarth S, Garbino J, Pugin J, Romand JA, Pittet D. Lack of effect of combination antibiotic therapy on mortality in patients with pneumococcal sepsis. Eur J Clin Microbiol Infect Dis. 2005;24(10):688–90.
Mortensen EM, Restrepo MI, Anzueto A, Pugh J. The impact of empiric antimicrobial therapy with a β-lactam and fluoroquinolone on mortality for patients hospitalized with severe pneumonia. Crit Care. 2005;10(1):R8.
Heffelfinger JD, Dowell SF, Jorgensen JH, Klugman KP, Mabry LR, Musher DM, et al. Management of community-acquired pneumonia in the era of pneumococcal resistance: a report from the Drug-Resistant Streptococcus pneumoniae Therapeutic Working Group. Arch Intern Med. 2000;160(10):1399–408.
Grossman RF, Hsueh PR, Gillespie SH, Blasi F. Community-acquired pneumonia and tuberculosis: differential diagnosis and the use of fluoroquinolones. Int J Infect Dis. 2014;18:14–21.
Amin AN, Cerceo EA, Deitelzweig SB, Pile JC, Rosenberg DJ, Sherman BM. The hospitalist perspective on treatment of community-acquired pneumonia. Postgrad Med. 2014;126(2):18–29.
Compliance with Ethics Guidelines
Conflict of Interest
Simone Gattarello has no relevant disclosures to report.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Respiratory Infections
Rights and permissions
About this article
Cite this article
Gattarello, S. What Is New in Antibiotic Therapy in Community-Acquired Pneumonia? An Evidence-Based Approach Focusing on Combined Therapy. Curr Infect Dis Rep 17, 45 (2015). https://doi.org/10.1007/s11908-015-0501-x
Published:
DOI: https://doi.org/10.1007/s11908-015-0501-x