Abstract
Background: The conventional treatment for community-acquired pneumonia (CAP) involves combination therapy consisting of a β-lactam penicillin or a cephalosporin with a macrolide. Alternatively, high-dose levofloxacin treatment has been used as single-agent therapy for treating CAP, covering atypical pathogens.
Objective: This study compared the clinical efficacy and safety of high-dose levofloxacin with combined ceftriaxone and azithromycin for the treatment of CAP.
Patients and Methods: This phase IV, prospective, randomized, open-label trial enrolled patients admitted to a tertiary referral hospital for CAP treatment from 2010 to 2011. Hospital admission was decided based on clinical judgement and the pneumonia severity index. Forty subjects were enrolled and assigned to two treatment arms using a random numbers table. The 20 subjects in the experimental group were given levofloxacin 750 mg intravenously once daily, followed by the same dose of oral levofloxacin at discharge when clinically improved and the 20 subjects in the control group were given ceftriaxone 2.0 g intravenously once daily plus oral azithromycin 500 mg for 3 consecutive days, followed by oral cefpodoxime 200 mg per day at discharge after clinical improvement. The primary outcome was the clinical success rate. Secondary outcomes were the microbiological success rate and adverse events during the study.
Results: Of the 40 subjects enrolled, 36 completed the study: 17 in the experimental group and 19 in the control group. The groups did not differ in terms of demographic factors or clinical findings at baseline. The clinical success rate (cured + improved) was 94% in the experimental (levofloxacin) group and 84% in the control group (p>0.05). The microbiological success rate and overall adverse events were also similar in both groups.
Conclusion: Single-agent, high-dose levofloxacin treatment exhibited excellent clinical and microbiological efficacy with a safety profile comparable to that of ceftriaxone plus azithromycin therapy. Large-scale clinical trials are required to verify these results.
Clinical Trial Registration: WHO International Clinical Trials Registry: KCT0000374; Daiichi-Sankyo Korea study code: T11-13-V1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite antibacterial therapy, the mortality rate of community-acquired pneumonia (CAP) remains at approximately 5–20%. Its extremely high mortality rate of 20–50% in patients in intensive care units is universally acknowledged.[1–3] The major microorganisms causing CAP are Streptococcus pneumoniae, Klebsiella pneumoniae and Haemophilus influenzae, of which S. pneumoniae is most frequently identified.[4] Pneumococcal bacteraemia in hospitalized CAP patients has a mortality rate of 20–41%.[1–3] Therefore, early antibacterial therapy to manage the causative microorganisms is considered vital in patients with mild to severe CAP, and a high antibacterial concentration must be achieved in both lung tissue and blood at an early stage. Although the early initiation of appropriate antibacterials has a beneficial effect on the prognosis, antibacterial therapy for CAP patients who require hospital admission must usually commence empirically because of the time required for microbiological identification.[5]
An appropriate antibacterial choice for CAP treatment is extremely important. In a number of retrospective studies of bacterial pneumonia, single-agent therapy with a fluoroquinolone antibacterial was very effective against mild to severe CAP.[6,7] In a randomized, prospective clinical study comparing azithromycin plus ceftriaxone and levofloxacin, daily injection of levofloxacin 500 mg achieved a clinical success rate of 94% and a microbiological eradication rate of 90%.[8] The Infectious Disease Society of America (IDSA) recommends doxycycline, macrolides or fluoroquinolones for the empirical treatment of CAP; it also promotes the use of fluoroquinolone alone, a combination of a β-lactam/β-lactamase inhibitor, or cephalosporin/macrolide therapy for atypical pathogens.[2] In recent years, a once-daily dose of levofloxacin 750 mg has been recommended, instead of a 500 mg dose,[9–12] as the bactericidal effect is maximized at a higher dose because of a concentration-dependent killing effect.
The present study evaluated the therapeutic effectiveness and safety of high-dose single-agent levofloxacin compared with ceftriaxone/azithromycin as an empirical treatment for CAP.
Patients and Methods
The subjects of this randomized, open-label study were adults admitted to the respiratory medical unit of Ewha Womans University Mokdong Hospital for the treatment of CAP from 2010 to 2011. Hospital admission was based on clinical judgement and the pneumonia severity index (PSI).[13] The study was approved by the Institutional Review Board of Mokdong Hospital (222-1-46), and written informed consent was obtained from all subjects.
The principal investigator used random numbers to divide the 40 enrolled patients into two groups. The 20 patients in the experimental group received a once-daily intravenous injection of high-dose levofloxacin 750 mg, followed by the same dose of oral levofloxacin at discharge when clinically improved. The 20 patients in the control group received once-daily intravenous ceftriaxone 2 g and oral azithromycin 500 mg for 3 consecutive days, followed by oral cefpodoxime 200 mg per day at discharge when clinically improved. The length of the hospital stay ranged from 5 to 14 days depending on the severity of the pneumonia, and the total duration of antibacterial use was based on clinical judgement. All subjects were given physical examinations at the time of enrollment, and medical records were created.
The severity of the CAP was classified using the PSI,[13] which is based on age, the presence of coexisting disease, abnormal physical findings, and abnormal laboratory findings at presentation. The PSI score was categorized into five risk classes according to mortality. Patients with a PSI score <70, indicating risk class 2, can be treated as outpatients. The presence of other diseases, use of antibacterials before admission, hospital admission history, alcohol (ethanol) consumption greater than 80 g per day, corticosteroid use, swallowing difficulty and use of other drugs were investigated. Chest x-rays, Gram and Ziehl-Neelsen staining, cultures for bacteriology and tuberculosis, blood cultures for suspected bacteraemia, serology for atypical pathogens, and the pneumococcal urinary antigen test were performed. Clinical symptoms and signs were recorded on days 5–7 of antibacterial treatment and again at completion of the treatment, at which time the physical examination, chest x-ray, cultures and serological tests were repeated. Patients were interviewed about the side effects experienced during treatment.
The primary criteria for subject selection were radiological evidence of pneumonia on a chest x-ray and the presence of at least one of the following: oral temperature higher than 38°C or lower than 35.5°C, leukocytosis (white blood cell count [WBC] >10 000/mm3), or more than 10% banded neutrophils. Subjects were enrolled when they had typical clinical signs and symptoms of pneumonia and were able to produce sputum samples. The following exclusion criteria were used: suspected infection in areas other than the respiratory system; suspected intolerance to the experimental and control drugs; allergy to or severe side effects from azithromycin, ceftriaxone, quinolones, macrolides or β-lactams; recent hospital admission more than 2 weeks before the beginning of the study; receipt of intravenous antibacterials within 24 hours before enrolment; creatinine clearance less than 20 mL/min; empyema requiring chest drainage; chronic lung disease with impaired lung function; clinical suspicion of tuberculosis; evidence of aspiration pneumonia; human immunodeficiency virus infection or immunosuppression; long-term use of an antiepileptic drug for the treatment of epilepsy; co-morbidity likely to confound the clinical evaluation; receipt of any drug for other clinical experiments within 30 days; pregnancy; and breast-feeding.
The primary outcome of this study was the clinical success rate. Secondary outcomes were the microbiological success rate and adverse events. Treatment efficacy was evaluated by assessing the level of clinical and microbiological improvement.[8] The clinical efficacy was determined by comparing the clinical symptoms and signs and chest x-rays obtained on days 5–7 after initiating drug treatment and at the end of therapy with those obtained at admission.[14] Clinical improvement was classified according to the following four categories:[8]
-
Clinically cured: no further antibacterials required; no remaining symptoms or signs of CAP.
-
Improved: no further antibacterials required; some clinical symptoms or signs remaining despite clear improvement.
-
Failed: additional antibacterial treatment required; no improvement in clinical symptoms or signs.
-
Unable to evaluate: unequivocal classification difficult, insufficient follow-up, use of non-study antibacterials, or violation of study protocol.
The microbiological response was determined by comparing the results of sputum cultures and blood tests obtained at the end of therapy with those obtained at admission. The level of microbiological improvement was designated according to the following five categories:[8]
-
Eradicated: none of the isolated microorganisms remaining.
-
Presumed eradicated: improvement without additional treatment despite pre-treatment evidence of infection in blood tests.
-
Persistent: isolated microorganisms persistently identified.
-
Presumed persistent: no available specimen, but microorganism likely persistent in cases with clinical failure.
-
Unable to evaluate: no confirmed pre-treatment results available, and evaluation after treatment impossible because follow-up cultures were absent or patient dropped out of the study.
Clinical tolerability was assessed by tabulating the adverse events noted during physical examinations, evidenced by the laboratory results, or reported by the patients themselves. Adverse events that became severe or frequent and required emergency medical intervention were classified as moderate or severe; in the case of these events, the medications were stopped or changed as deemed appropriate by the study physicians.
The SPSS software package for Windows (Version 18.0; SPSS, Chicago, IL, USA) was used for the statistical analysis. The unpaired t-test was used to compare results between groups. The presence and absence of a parameter was compared between groups using the chi-squared (χ2) test. The lack of statistical differences between groups was not taken as evidence of inferiority. Differences were considered statistically significant at p < 0.05.
Results
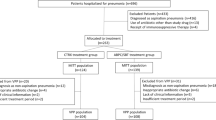
The 40 enrolled patients were divided equally into experimental and control groups. Four enrolled participants dropped out after an average of 4 days. The one subject in the control group who dropped out had suddenly developed a pleural effusion. In the experimental group, one subject refused to continue the study after experiencing dizziness and vomiting; another subject dropped out due to sudden-onset acute coronary syndrome; and the third dropped out because of a drug-related rash (figure 1).
The basic initial demographic and clinical values for the remaining 17 experimental and 19 control subjects were similar between the groups. Five experimental subjects and nine control subjects had PSI scores >70, indicating risk class 3. Those patients with PSI scores <70 required hospital admission because there was no improvement or symptomatic worsening following treatment in private clinics, multilobar pneumonia, lung co-morbidity or an uncontrolled high fever. There was no significant difference in disease severity between the two groups (table I).
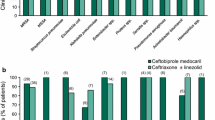
The clinical responses on days 5–7 were similar in both groups, and the final treatment outcomes for the experimental and control groups showed clinical cure rates of 88% and 79%, respectively. Outcomes better than improvement were seen in 94% (16/17) of the experimental subjects and 84% (16/19) of the control subjects, with no significant difference between the two groups. The experimental group had one failed case, and the control group had three failed cases. Eleven (28%) of the 40 original subjects were positive on microbiological testing. All patients tested by culture, serological tests or urinary antigen tests showed eradication or presumed eradication (table II).
Of the 40 enrolled subjects, 13 (33%) experienced adverse events: six cases in the experimental group and seven cases in the control group. Two adverse events in the experimental group and one adverse event in the control group were considered unconnected to the study drugs. There were four mild, three moderate and two severe adverse events in the experimental group, and two mild, six moderate and no severe adverse events in the control group. Neither the frequency nor severity of drug-related adverse events differed between the two groups. Two severe adverse events in the experimental group, one of which was a non-drug-related admission and one sudden-onset acute coronary syndrome, were deemed unconnected to the study drugs (table III).
Discussion
The results of this study show that single-agent, high-dose therapy with levofloxacin is as effective in treating CAP as the standard cephalosporin/macrolide combination therapy recommended by the IDSA/American Thoracic Society (ATS)[2] and the British Thoracic Society (BTS).[1] The final clinical cure rates for the experimental and control groups were 88% and 79%, respectively, and 94% of the subjects in the experimental group and 84% of those in the control group experienced satisfactory results, i.e. a clinical cure or marked improvement, similar to previous studies.[8,12]
CAP is associated with high rates of hospitalization and mortality, and this has been addressed by developing guidelines for antibacterial treatment.[1–3] Many recent clinical research reports and literature reviews have suggested that resistance to CAP drugs is increasing and that CAP patients are becoming infected with drug-resistant organisms.[2–3] The IDSA/ATS2 and BTS recommend empirical treatment of early-stage CAP with β-lactam/macrolide combination therapy. However, this recommendation is based on retrospective studies, and the outcomes of its use are not convincing. The antibacterial effects of the macrolide against atypical bacteria and its additional anti-inflammatory effects are thought to contribute to the effectiveness of this therapy, but its exact mechanisms have not been identified.[15] Streptococcus pneumoniae, the most commonly identified causative microorganism in CAP, has a high rate of resistance to penicillin and macrolides in South Korea, but a relatively low frequency of resistance to fluoroquinolones.[16] The IDSA/ATS has reported that the efficacies of fluoroquinolone therapy and β-lactam/macrolide combination therapy are similar, making fluoroquinolones legitimate first-choice antibacterials for empirical treatment of CAP.[1]
Levofloxacin, a second-generation fluoroquinolone, is particularly beneficial in the treatment of respiratory infections because it has broad-spectrum activity against atypical infections, as well as those caused by Gram-negative or Gram-positive bacteria.[9,11,17] The effectiveness of fluoroquinolones is concentration-dependent, increasing at higher concentrations. It has high pulmonary and oral bioavailability,[11,17] which simplifies the change from intravenous to oral administration with once-daily dosing and facilitates rapid hospital discharge.[2]
Current research suggests that fluoroquinolones are slightly superior to β-lactam antibacterials in the treatment of CAP.[17–19] Vardakas et al.[20] noted a higher cure rate for levofloxacin therapy than for combination β-lactam/macrolide therapy. A retrospective review[21] and a prospective[22] study found higher survival rates in patients receiving levofloxacin than in those receiving β-lactam/macrolide combination therapy. In both of the above studies, levofloxacin 500 mg was given once daily. Noreddin et al.[11] reported that a 750 mg dose of levofloxacin resulted in better outcomes than a 500 mg dose. In our study, a 750 mg dose of levofloxacin resulted in a clinical cure rate comparable to that of existing combination protocols, although superiority was not verified.
Our study has some limitations. It was a single-centre, open-label trial with a small number of subjects. In addition, some of the patients were only mildly sick, with low PSI scores, and microbiological positivity was lower than that in previous reports.[4,8,11] Nevertheless, the strengths of this study are that it was randomized and that it demonstrated the safety of high-dose levofloxacin[10,23] in an understudied Asian population. Large-scale clinical trials are required to verify these results.
In this randomized clinical study, high-dose levofloxacin therapy was as successful as β-lactam/macrolide therapy for the treatment of mild to severe CAP. Compared with a dual regimen, quinolone as a single antibacterial agent has the advantage of treating atypical pathogens as well as common pathogens. However, in countries with a high prevalence of tuberculosis, the use of quinolone as a first-line defense against CAP should be reconsidered because it can delay the diagnosis of tuberculosis and increase the risk for quinolone-resistant mycobacteria.
Conclusion
High-dose single-agent levofloxacin therapy is clinically and microbiologically as efficient and safe for the treatment of CAP as the existing standard ceftriaxone/macrolide combination treatment.
References
Lim WS, Baudouin SV, George RC, et al. British Thoracic Society guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 2009; 64 Suppl. 3: iii1–55
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007; 44 Suppl. 2: 27–72
Woodhead M, Blasi F, Ewig S, et al. Guidelines for the management of adult lower respiratory tract infections. Eur Respir J 2005; 26: 1138–80
Cilloniz C, Ewig S, Polverino E, et al. Microbial etiology of community acquired pneumonia and its relation to severity. Thorax 2011; 66: 340–6
Ferrer M, Menendez R, Amaro R, et al. The impact of guidelines on the outcomes of community acquired and ventilator acquired pneumonia. Clin Chest Med 2011; 32: 491–505
Croom KF, Goa KL. Levofloxacin: a review of its use in the treatment of bacterial infections in the United States. Drugs 2003; 63: 2769–802
Grossman RF, Rotschafer JC, Tan JS. Antimicrobial treatment of lower respiratory tract infections in the hospital setting. Am J Med 2005; 118 Suppl. 7A: 29–38
Frank E, Liu J, Kinasewitz G, et al. A multicenter, open-label, randomized comparison of levofloxacin and azithromycin plus ceftriaxone in hospitalized adults with moderate to severe community acquired pneumonia. Clin Ther 2002; 24: 1292–308
Conte Jr JE, Golden JA, Mclver M, et al. Intrapulmonary pharmacokinetics and pharmacodynamics of high-dose levofloxacin in healthy volunteer subjects. Int J Antimicrob Agents 2006; 28: 114–21
Dunbar LM, Wunderink RG, Habib MP, et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis 2003; 37: 752–60
Noreddin AM, Marras TK, Sanders K, et al. Pharmacodynamic target attainment analysis against Streptococcus pneumoniae using levofloxacin 500mg, 750mg and 1000mg once daily in plasma and epithelial lining fluid of hospitalized patients with community acquired pneumonia. Int J Antimicrob Agents 2004; 24: 479–84
Dunbar LM, Khashab MM, Kahn JB, et al. Efficacy of 750 mg, 5 days levofloxacin in the treatment of community acquired pneumonia caused by atypical pathogens. Curr Med Res Opin 2004; 20: 555–63
Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336: 243–50
Echols RM, Tillotson GS, Song JX, et al. Clinical trial design for mild to moderate community acquired pneumonia: an industry perspective. CID 2008; 47 Suppl. 3: 166–75
File TM, Garau J, Blasi F, et al. Guidelines for empiric antimicrobial prescribing in community acquired pneumonia. Chest 2004; 125: 1888–901
Song JH, Jung KS, Kang MW, et al. Treatment guidelines for community acquired pneumonia in Korea: an evidence based approach to appropriate antimicrobial therapy. Tuberc Respir Dis 2009; 67: 281–302
File TM, Segreti J, Dunbar L, et al. A multicenter, randomized study comparing the efficacy and safety of intravenous and/or oral levofloxacin versus ceftriaxone and/or cefuroxime axetil in treatment of adults with community acquired pneumonia. Antimicrob Agents Chemother 1997; 41: 1965–72
File TM. Levofloxacin in the treatment of community acquired pneumonia. Can Respir J 1999; 6 Suppl. A: 35–9
Norrby SR, Petermann W, Willcox PA, et al. A comparative study of levofloxacin and ceftriaxone in the treatment of hospitalized patients with pneumonia. Scand J Infect Dis 1998; 30: 397–404
Vardakas KZ, Siempos II, Grammatikos A, et al. Respiratory fluoroquinolones for the treatment of community acquired pneumonia: a meta-analysis of randomized controlled trials. CMAJ 2008; 179: 1269–77
Houck PM, MacLehose RF, Niederman MS, et al. Empiric antibiotic therapy and mortality among Medicare pneumonia in patients in 10 Western states: 1993, 1995, and 1997. Chest 2001; 119: 1420–6
Ribelles JMQ, Tenias JM, Querol-Borras JMQ, et al. Levofloxacin versus ceftriaxone plus clarithromycin in the treatment of adults with community-acquired pneumonia requiring hospitalization. Int J Antimicrob Agents 2005; 25: 75–83
Kahn JB. Latest industry information on the safety profile of levofloxacin in the US. Chemotherapy 2001; 47 Suppl. 3: 32–7
Acknowledgements
This study was funded from Daiichi-Sankyo Korea Ltd and approved by the Institutional Review Board of Mokdong Hospital (222-1-46), Ewha Womans University, Seoul, Korea. The role of the funding company was limited to the study design. The funding company was not involved in conducting the study, the data analysis, data interpretation or manuscript preparation.
The role of the corresponding author was the study design; conducting the study; collection, management, analysis and interpretation of the data; and preparation of the manuscript.
None of the authors have any relevant conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.H., Kim, S.W., Kim, J.H. et al. High-Dose Levofloxacin in Community-Acquired Pneumonia. Clin Drug Investig 32, 569–576 (2012). https://doi.org/10.1007/BF03261911
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03261911