Abstract
Purpose of Review
Metabolic syndrome (MetS), a cluster of risk factors including central obesity, metabolic abnormalities, and arterial hypertension, is a well-known determinant of arterial wall remodeling and stiffening. The mechanisms whereby MetS promotes arterial stiffening include increased sympathetic activity with the associated fast heart rate, enhanced activity of the renin-angiotensin-aldosterone system, increased production of inflammatory cytokines and reactive oxygen species, and reduction of nitric oxide availability. These adverse effects can explain why aerobic physical activity can retard the age-related decline in arterial elasticity in subjects with MetS.
Recent Findings
A large number of studies have shown that in patients with MetS, exercise can reduce body weight and blood pressure and improve the metabolic profile. In addition, regular exercise training can counterbalance the detrimental effects of MetS by reducing sympathetic activity and improving endothelial function with a beneficial effect on arterial elasticity. Indeed, the majority of published data have shown a favorable effect of aerobic exercise on pulse wave velocity, augmentation index, central blood pressure, and small artery compliance.
Summary
Special attention should be paid by clinicians to people with MetS in whom the adverse effect of metabolic disturbances on arterial structure and function can be offset by a program of physical training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome (MetS), a cluster of risk factors including central obesity, insulin resistance, dyslipidemia, and arterial hypertension, is a well-known predictor of cardiovascular (CV) disease [1]. General population studies have shown that about one quarter to one third of adults have MetS and its prevalence continues to increase [2, 3] being recognized as a major public health issue. MetS is also associated with a chronic inflammatory and prothrombotic state [1] and with increased oxidative stress [4], which promotes vascular arterial wall remodeling and arterial stiffness (AS) [5, 6]. A large number of studies have documented that AS increases with the number of MetS components [7••, 8] as each risk factor acts independently through different mechanisms with adverse effects on the structure and function of the vascular system. On the opposite side, several authors observed a favorable effect of regular physical activity on arterial elasticity [9, 10••], which is confined to aerobic endurance training. In a recent meta-analysis, aerobic but not resistance exercise was associated with a significant reduction of AS [10••]. This protective role may be independent from weight loss [9], blood pressure (BP) reduction [11••], or improvement of lipid profile [11••, 12].
Parameters of Arterial Distensibility
The most popular index of large artery stiffness is pulse wave velocity (PWV) which was included in the 2007 European Society of Hypertension Guidelines [13] because of its good CV predictive value. PWV was confirmed by the 2013 ESH/ESC guidelines as a useful marker for reclassifying intermediate-risk patients into a higher or lower CV risk class [14]. Also, in the most recent American Society of Hypertension Guidelines, this index was included among the parameters useful for estimating CV target organ damage and atherosclerosis [15]. However, other indices can provide complementary information in the assessment of arterial elasticity. The augmentation index (AIx) gives an estimate of wave reflection [16, 17] and has been found to be a predictor of mortality and CV events independently of peripheral pressures [18, 19].
In the last decades, other distensibility parameters have been proposed as they proved to be predictive of increased risk of CV morbidity and mortality [20]. Among these, parameters determined by diastolic pulse contour wave analysis have attracted the interest of some investigators, because they provide information on the characteristics not only of large capacitance arteries but also of smaller conduit arteries [20]. Another interesting index of arterial distensibility derived from the analysis of the pulse wave contour is central BP, which usually is lower than the corresponding brachial BP, due to the phenomenon known as pressure amplification [21], which is inversely correlated to AS. Central BP has been found to be a stronger determinant of target organ damage [22, 23] than brachial BP and a stronger predictor of hypertension development [23], CV events [24], and kidney disease [25].
Several noninvasive techniques have been proposed to measure AS parameters. The majority of the authors have used applanation tonometry performed with Shygmocor device (AtCor Medical, Australia), which acquires sequential waveforms at the radial artery. Besides measuring central BP, the device also returns the radial AIx. PWV is determined by simultaneous applanation tonometry and electrocardiographic recording and is calculated as the ratio of the distance between the two recording sites (radial and carotid artery) and the time of travel of the pulse wave over this distance [26]. Other devices, such as Omron HEM-9000AI (Omron, Japan), a cuff-based technique, calculate central systolic BP from the second systolic peak. Another possible estimation of the central systolic BP is through direct tonometry of the carotid artery, a procedure that was validated against invasive pressure [27]. Finally, ultrasound or MRI techniques can give an estimation of aortic BP by measuring the local wall distension usually at the carotid level.
Factors Affecting Arterial Distensibility
Several modifiable and unmodifiable risk factors can affect arterial distensibility. Among the unmodifiable risk factors, aging plays the most important role. In particular, age together with BP has been shown to account for up to 70% of the variance in AS [28]. Hypertension, diabetes, and smoking also have an important influence on the progression of AS assessed by PWV. According to some authors, patients with hypertension have a higher annual progression rate of PWV almost three times higher than normotensive subjects [29•]. Lipid abnormalities have also been considered as important determinants of stiffening [30], and the two factors combined showed a synergistic effect (4× higher) [29•]. The role of smoking appeared more controversial. Terentes-Pritnzios et al. [29•] did not find any significant progression in vascular stiffening according to smoking habits. In contrast, a number of studies have found that chronic cigarette smoking is associated with increased AS [31, 32]. Also, central BP was found to be unfavorably affected by smoking habits. In a study [33] involving 344 untreated young to middle-age (mean age 37 ± 10 years), stage I hypertensive subjects from the HARVEST cohort, we observed that central systolic BP and pulse pressure were higher in smokers than in non-smokers (systolic BP 121.9 ± 13.1 mmHg in non-smokers, 127.2 ± 16.5 mmHg in light smokers, 126.7 ± 15.3 mmHg in those who smoked > 5 cigarettes/day, p = 0.009; pulse pressure 37.7 ± 9.8, 41.5 ± 13.1, and 41.9 ± 10.5 mmHg, respectively, p = 0.005). Also, AIx was higher in smokers than in non-smokers (p = 0.024). Finally, in a two-way ANCOVA analysis, systolic BP amplification markedly declined across the three age groups (p = 0.0002) and from non-smokers to smokers (p = 0.0001), with a significant interaction between smoking and age group (p = 0.05), indicating that in young hypertensives, smoking has a detrimental effect on central BP accelerating the age-related decline in BP amplification.
Contrary to the observation by Terentes-Pritnzios et al. [29•], AS was found by most investigators to be greater in patients with diabetes mellitus [34] and in subjects with MetS [35]. Insulin resistance and chronic hyperinsulinemia increase the local activity of renin-angiotensin-aldosterone system and the expression of angiotensin II receptors in vascular tissue, leading to vessel wall hypertrophy and fibrosis [36]. Moreover, impaired glucose tolerance promotes non-enzymatic glycation and cross-linking of collagen [37]. Another factor promoting AS is high salt intake [38], which increases BP and sympathetic tone, favoring the development of cardiac hypertrophy and large artery stiffening. An abnormal response of the renin-angiotensin-aldosterone system to high sodium level and a reduction in the bioavailability of nitric oxide were proposed as other possible mechanisms for sodium-dependent AS [39]. In a recent meta-analysis of 11 randomized controlled trials [40•], the pooled analysis showed that a lower sodium intake, measured by 24-h sodium urinary excretion, was associated with a lower average PWV (RR − 2.84, 95% CI − 5.08 to − 0.51), though this trend reached the level of statistical significance only in two studies [41, 42].
Arterial Distensibility, Obesity, and the Metabolic Syndrome
Among the modifiable risk factors for AS, several authors demonstrated that the MetS and its components can increase the risk of AS [4, 7••, 43]. Several studies have documented an increase in AS level according not only to the presence/absence of MetS [44, 45••] but also to the number of MetS components [45••]. In the TRIPLE A-Stiffness study, a multicenter longitudinal study performed in a large European population, the authors investigated the values of AS according to the presence or absence of MetS and observed a higher PWV in patients with MetS (9.65 ± 2.57 m/s) compared to those without it (8.42 ± 2.09 m/s, p < 0.001). This difference remained statistically significant also after adjustment for age and sex (p < 0.001) [45••]. Moreover, the authors explored the effect of different MetS components on AS and observed that the presence of any of these five components (waist circumference, triglycerides, HDL cholesterol, BP, and serum glucose) was associated with higher PWV values (all age- and sex-adjusted p < 0.0001). In multivariate analysis, older age, BP, glycaemia, and HDL cholesterol components were demonstrated to be independent determinants of high PWV [45••]. Sex, waist circumference, and triglycerides did not show an independent effect on AS in this study [45••].
As mentioned above, the larger the number of the MetS components, the greater the increase in PWV, as shown by Lopes-Vicente et al. [7••]. These authors examined 64 patients with 3 to 5 components of MetS (n = 8 with 5 components, n = 27 with 4 components, and n = 29 with 3 components) and 17 control subjects. The increase in the number of risk factors was associated with a progressive impairment of PWV: mean value was 7.2 ± 0.3 m/s in control group, 7.5 ± 0.2 m/s in the group with 3 risk factors (p = n.s vs controls), 7.9 ± 0.2 m/s in the group with 4 risk factors (p = 0.047 vs control), and 8.5 ± 0.4 m/s in the group with 5 risk factors (p = 0.011 vs controls and p = 0.012 vs group with 3 risk factors) [7••]. Discrepant results have been found in the literature about the specific importance of the single MetS components due to regional differences in subjects’ characteristics and to the different selection criteria used for enrolling the study participants. In general, high BP, waist circumference, and high blood glucose showed the strongest impact on AS [44].
The mechanisms whereby MetS and visceral obesity with the associated sedentary lifestyle may favor AS are manifold including increased sympathetic activity with the associated fast heart rate, enhanced activity of the renin-angiotensin-aldosterone system, and production of inflammatory cytokines. Impairment of endothelial function with the associated reduction of nitric oxide availability and increased production of reactive oxygen species are other factors that promote AS [29•, 35, 36, 43]. In addition, MetS and obesity are associated with high levels of leptin and decreased adiponectin which facilitates vascular smooth muscle cell proliferation and migration, thereby increasing collagen synthesis [46].
Arterial Distensibility and Physical Activity
A large number of epidemiologic studies have documented an association between regular physical activity and decline in the risk of CV and all-cause mortality [47, 48]. According to data from the Framingham Heart study, life expectancy is 3.7 years longer in physically active subjects compared to sedentary people [49]. Due to its multiple positive and protective effects, physical activity is included in all guidelines as one of the main non-pharmacological measures for the treatment of hypertension [14, 15], diabetes [50], and ischemic heart disease [51].
The protective role of regular exercise in attenuating CV disease and mortality risk may be due to several different factors including a decrease in BP and BMI, better lipid profile, and improvement of insulin sensitivity [52,53,54]. The decrease in BP has been documented in several meta-analytic studies. Cornelissen et al. [55] investigated the effect of at least 4 weeks of exercise on BP in healthy subjects, examining different types of physical activity: endurance, dynamic resistance, combined training, and isometric resistance. All types of exercise, except combined training, were able to reduce both systolic and diastolic BP: endurance − 3.5 (confidence limits − 4.6 to − 2.3)/− 2.5 (− 3.2 to − 1.7) mmHg, dynamic resistance − 1.8 (− 3.7 to − 0.011)/− 3.2 (− 4.5 to − 2.0) mmHg, and isometric resistance − 10.9 (− 14.5 to − 7.4)/− 6.2 (− 10.3 to − 2.0). Of note, the BP reduction with aerobic exercise was particularly elevated among hypertensive individuals, − 8.3 (− 10.7 to − 6.0)/− 5.2 (− 6.8 to − 3.4) mmHg [55].
Another important mechanism that contributes to the reduction of CV risk is the effect of exercise on body fatness and metabolic variables. The influence of regular aerobic endurance training on waist circumference, lipid profile, glucose, and HOMA index was reported in another meta-analysis by Cornelissen et al. [53]. The authors observed that all components of the MetS were improved by exercise, but the strongest effects were found for HDL cholesterol, serum glucose, fasting insulin, and the HOMA index (Fig. 1). These effects can explain why aerobic physical activity can retard the age-related decline in arterial elasticity measured with PWV [56], as shown in a recent meta-analysis [10••]. Although there were some neutral studies, the majority of published data were in favor of a beneficial effect of aerobic exercise on PWV (0.63 m/s, 95% CI − 0.90 to − 0.35) [10••]. In addition, exercise was proved effective in improving small artery compliance in young hypertensive adults [57].
Changes in metabolic data induced by endurance training. Meta-analysis of 39 trials. a Changes in cholesterol level. b Changes in serum glucose and triglyceride levels. c Changes in insulin level and HOMA index. Adapted from Cornelissen VA et al. [53]
One of the main mechanisms underlying the favorable effect of exercise on AS is the reduction of heart rate. Studies in human beings have shown that there is a progressive increase in PWV with increasing hear rate with pacing independent from pressure changes [58], documenting that heart rate is cross-sectionally associated with AS. This effect has been quantified as an increase of 0.17 m/s for each 10 beats/min increment in heart rate [58]. A positive association between heart rate and AS has been documented also in longitudinal studies by Tomiyama et al. [59] and by Benetos et al. [60] either among normotensive or hypertensive subjects. Heart rate, however, has an opposite effect on other determinants of arterial distensibility such as central systolic BP and AIx. Several cross-sectional studies have shown that a lower resting hear rate is associated with higher aortic systolic BP and AIx [17, 61]. This negative relationship has been attributed to a shift of the backward wave reflected from the periphery into late systole secondary to the prolongation of left ventricle ejection time and to the increase in stroke volume at low heart rates [16, 17, 62]. This finding led some authors to claim that heart rate reduction in hypertension is detrimental because it may favor the risk of CV events [62]. However, a recent meta-analysis of 16 studies [10••] has shown that regular physical activity reduced the AIx by 2.63%.
In a recent analysis of the short-term and long-term effects of heart rate on arterial distensibility [63•], Palatini et al. confirmed the negative relationship of heart rate with AIx recorded in the same session. However, ambulatory heart rate turned out to be an independent positive predictor of AIx and central BP measured 8 years later (Fig. 2). These findings suggest that heart rate reduction in the long run has a favorable effect and not a detrimental one on all parameters of arterial distensibility and contribute to explain why people with lower heart rate have a reduced risk of CV events and mortality in hypertension.
Relationship of baseline night-time heart rate with central systolic blood pressure and the augmentation index measured 8 years later in 346 participants from the HARVEST cohort. Adapted from Palatini P et al. [63•]. SBP indicates systolic blood pressure
In summary, training-induced bradycardia may have an unfavorable effect on central hemodynamic due to the prolongation of ejection time so that the reflected wave may return in systole. On the other hand, improved small artery compliance and reduced peripheral resistance in athletes can decrease the magnitude of the reflected wave. The different combination of these effects can account for the discordant findings in previous literature. Differences in subject characteristics (age, cardiorespiratory fitness levels, etc.), study methodologies, and lack of adjustment for important confounding factors are other possible sources of between-study variability. Other mechanisms by which the reduction of the sympathetic tone associated with physical training can improve endothelial function and arterial elasticity are the decrease in peripheral vasoconstriction and the prevention of small artery remodeling with an increase in the lumen/wall ratio [64] and the cross-sectional area of the microcirculation [65]. Also, humoral factors may contribute to the beneficial effect of dynamic sport activities on small artery distensibility. Maeda et al. [66] after 8 weeks of exercise observed a reduction in endothelin-1 and an increase in nitric oxide concentrations with an inverse correlation between these two factors. Reductions of inflammatory cytokines and of oxidative stress are other mechanisms by which exercise can prevent AS in MetS [67].
Effect of Exercise on Arterial Distensibility in Subjects with the Metabolic Syndrome
From the above data, one can understand why physical activity may retard the development of AS in people with the MetS. Indeed, several cross-sectional studies have shown that exercise can have beneficial effects on arterial distensibility in this clinical condition. Within a group of participants with the MetS, Pasha et al. [68] observed that carotid β-stiffness index was lower in the individuals who performed regular physical activity than in those who were sedentary. In the former, the β-stiffness index was similar to that in a group of healthy individuals, indicating that physical activity may be effective in mitigating the adverse effects of high BP, visceral adiposity, and metabolic abnormalities on the vessel wall. In a similar study, Bohn and coworkers [69] explored the effect of different levels of physical activity (sedentary, light, moderate-to-vigorous), among 197 middle-age patients (116 without and 81 with MetS). Patients with MetS had higher PWV compared to patients without MetS (10.2 ± 1.9 vs 8.3 ± 1.5 m/s, p < 0.001). However, participants with MetS who were more sedentary showed significantly greater PWV than those who were more active and of people without MetS regardless of the level of physical activity [69].
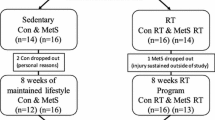
The above cross-sectional data have been confirmed by intervention trials investigating the effects of exercise training in patients with MetS. The effect of 6 months of high-intensity aerobic interval training was explored by Mora-Rodriguez et al. [11••] in a group of patients with MetS having a high prevalence of hypertension. PWV declined in the training group from 8.5 ± 2.1 to 7.8 ± 2.3 m/s (p = 0.05), while it remained unchanged in a group of subjects of control. Similarly, AIx was reduced after training from 24.7 ± 11.6 to 21.9 ± 9.2% (p = 0.038), with no changes in the group that remained sedentary. These beneficial effects were partly explained by the reduction in BP and partly by the improvement of the endothelial function documented by a 20% significant increase in cutaneous microcirculation reactive flow after training [11••]. Similar results were obtained by Koskinen et al. [70] in a longitudinal analysis of the Young Finns Study. After 6 years of follow-up, participants with baseline MetS who performed regular physical activity and recovered from the MetS had higher carotid artery distensibility compared with MetS people who remained sedentary and still had the MetS at study end [70].
In summary, according to the evidence mentioned above, several mechanisms can explain the favorable effect of exercise on arterial distensibility in people with MetS (Fig. 3). Exercise can counterbalance many detrimental effects of MetS: one main mechanism is the reduction in heart rate. Opposite effects of exercise and MetS have been observed also on inflammatory cytokines. The same applies to humoral factors, such as nitric oxide, leptin, adiponectin, and reactive oxygen species, which have an important impact on the endothelial function and the arterial structure.
Mechanisms for the beneficial effect of regular aerobic exercise on arterial elasticity in the metabolic syndrome. For heart rate and inflammatory markers, the sign + indicates an increase and the sign − a decrease. For humoral factors and endothelial function, the sign + indicates a favorable effect and the sign − a detrimental effect
Conclusions
Regular physical activity has shown beneficial effects in general populations and several clinical conditions and should thus be recommended to every subject for the prevention of CV disease. However, implementing a long-lasting program of physical training is a challenging task because of the low compliance to exercise shown by participants in long-term studies [11••, 70]. Thus, special attention should be paid by clinicians to people with MetS in whom the adverse effect of metabolic disturbances on the arteries can be offset by a program of physical activity. A number of studies have shown that in these patients, exercise can reduce body weight and BP and improve the metabolic profile with a beneficial effect on arterial elasticity. In addition, physical activity can counteract the pathogenetic mechanisms favoring the development of AS in MetS and thus represents one of the best tools for restoring arterial structure and function in patients with this clinical condition.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—a new worldwide definition. Lancet. 2005;366:1059–62.
Ford ES, Giles WH. A comparison of the prevalence of the metabolic syndrome using two proposed definitions. Diabetes Care. 2003;26:575–81.
Slivovskaja I, Ryliskyte L, Serpytis P, Navickas R, Badarienė J, Celutkiene J, et al. Aerobic training effect on arterial stiffness in metabolic syndrome. Am J Med. 2018;131:148–55.
Scuteri A, Najjar SS, Muller DC, Andres R, Hougaku H, Metter EJ, et al. Metabolic syndrome amplifies the age-associated increases in vascular thickness and stiffness. J Am Coll Cardiol. 2004;43:1388–95.
Scuteri A, Cunha PG, Rosei EA, Badariere J, Bekaert S, Cockcroft JR, et al. Arterial stiffness and influences of the metabolic syndrome: a cross-countries study. Atherosclerosis. 2014;233:654–60.
•• Lopes-Vicente WRP, Rodrigues S, Cepeda FX, et al. Arterial stiffness and its association with clustering of metabolic syndrome risk factors. Diabetol Metab Syndr. 2017;9:87. This study performed in subjects in the early stage of metabolic syndrome showed increased arterial stiffness in this condition. The risk was found to increase with increasing number of the components of the metabolic syndrome.
Kim M, Kim M, Yoo HJ, Lee SY, Lee SH, Lee JH. Age-specific determinants of pulse wave velocity among metabolic syndrome components, inflammatory markers, and oxidative stress. J Atheroscler Thromb. 2018;25:178–85.
Joo HJ, Cho SA, Cho JY, Lee S, Park JH, Yu CW, et al. Different relationship between physical activity, arterial stiffness, and metabolic status in obese subjects. J Phys Act Health. 2017;14:716–25.
•• Ashor AW, Lara J, Siervo M, et al. Effects of exercise modalities on arterial stiffness and wave reflection: a systematic review and meta-analysis of randomized controlled trials. PloS one. 2014;9:e110034. This meta-analysis of forty-two studies compared the effect of aerobic and resistance exercise lasting ≥4 weeks on arterial stiffness, demonstrating an improvement of PWV and AIx only with aerobic training.
•• Mora-Rodriguez R, Ramirez-Jimenez M, Fernandez-Elias VE, et al. Effects of aerobic interval training on arterial stiffness and microvascular function in patients with metabolic syndrome. J Clin Hypertens. 2018;20:11–8. The authors determined the effect of high-intensity aerobic interval training on arterial stiffness and microvascular dysfunction in patients with metabolic syndrome demonstrating that 6 months of aerobic exercise were able to reduce both arterial stiffness and microvascular dysfunction.
Donley DA, Fournier SB, Reger BL, DeVallance E, Bonner DE, Olfert IM, et al. Aerobic exercise training reduces arterial stiffness in metabolic syndrome. J Appl Physiol. 2014;116:1396–404.
Mancia G, De Backer G, Dominiczak A, et al. Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–87.
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017.
McEniery CM, Yasmin, Hall IR, et al. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol. 2005;46:1753–60.
Wilkinson IB, Mohammad NH, Tyrrell S, Hall IR, Webb DJ, Paul VE, et al. Heart rate dependency of pulse pressure amplification and arterial stiffness. Am J Hypertens. 2002;15:24–30.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, et al. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31:1865–71.
Janner JH, Godtfredsen NS, Ladelund S, Vestbo J, Prescott E. High aortic augmentation index predicts mortality and cardiovascular events in men from a general population, but not in women. Eur J Prev Cardiol. 2013;20:1005–12.
Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605.
Nichols W, O’Rourke MF, editors. McDonalds’ blood flow in arteries: theoretical, experimental and clinical principles. 5th ed. Oxford: Oxford University Press; 2005.
Roman MJ, Okin PM, Kizer JR, Lee ET, Howard BV, Devereux RB. Relations of central and brachial blood pressure to left ventricular hypertrophy and geometry: the Strong Heart Study. J Hypertens. 2010;28:384–8.
Saladini F, Mos L, Casiglia E, Malipiero G, Mazzer A, Palatini P. Central blood pressure is an independent predictor of future hypertension in young to middle-aged stage 1 hypertensives. Blood Press. 2013;22:9–16.
Jankowski P, Kawecka-Jaszcz K, Czarnecka D, Brzozowska-Kiszka M, Styczkiewicz K, Loster M, et al. Pulsatile but not steady component of blood pressure predicts cardiovascular events in coronary patients. Hypertension. 2008;51:848–55.
Cohen DL, Townsend RR. Central blood pressure and chronic kidney disease progression. Int J Nephrol. 2011;2011:407801.
Wilkinson IB, Fuchs SA, Jansen IM, Spratt JC, Murray GD, Cockcroft JR, et al. Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens. 1998;16:2079–84.
Van Bortel LM, Balkestein EJ, van der Heijden-Spek JJ, et al. Non-invasive assessment of local arterial pulse pressure: comparison of applanation tonometry and echo-tracking. J Hypertens. 2001;19:1037–44.
McEniery CM, Yasmin, Maki-Petaja KM, et al. The impact of cardiovascular risk factors on aortic stiffness and wave reflections depends on age: the Anglo-Cardiff collaborative trial (ACCT III). Hypertension. 2010;56:591–7.
• Terentes-Printzios D, Vlachopoulos C, Xaplanteris P, et al. Cardiovascular risk factors accelerate progression of vascular aging in the general population: results from the CRAVE Study (Cardiovascular Risk Factors Affecting Vascular Age). Hypertension. 2017;70:1057–64. In this general population study, the authors observed that numerous risk factors were associated with accelerated deterioration of specific indices of vascular aging, such as pulse wave velocity and augmentation index.
Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension. 2009;54:1328–36.
Li H, Srinivasan SR, Berenson GS. Comparison of the measures of pulsatile arterial function between asymptomatic younger adult smokers and former smokers: the Bogalusa Heart Study. Am J Hypertens. 2006;19:897–901.
Mahmud A, Feely J. Effect of smoking on arterial stiffness and pulse pressure amplification. Hypertension. 2003;41:183–7.
Saladini F, Benetti E, Fania C, Mos L, Casiglia E, Palatini P. Effects of smoking on central blood pressure and pressure amplification in hypertension of the young. Vasc Med. 2016;21:422–8.
Schram MT, Henry RM, van Dijk RA, et al. Increased central artery stiffness in impaired glucose metabolism and type 2 diabetes: the Hoorn Study. Hypertension. 2004;43:176–81.
Ho CT, Lin CC, Hsu HS, Liu CS, Davidson LE, Li TC, et al. Arterial stiffness is strongly associated with insulin resistance in Chinese; a population-based study (Taichung Community Health Study, TCHS). J Atheroscler Thromb. 2011;18:122–30.
Brillante DG, O’Sullivan AJ, Howes LG. Arterial stiffness in insulin resistance: the role of nitric oxide and angiotensin II receptors. Vasc Health Risk Manag. 2009;5:73–8.
Brownlee M, Cerami A, Vlassara H. Advanced glycosylation end products in tissue and the biochemical basis of diabetic complications. N Engl J Med. 1998;318:1315–21.
Park S, Park JB, Lakatta EG. Association of central hemodynamics with estimated 24-h urinary sodium in patients with hypertension. J Hypertens. 2011;29:1502–7.
Ni Z, Vaziri ND. Effect of salt loading on nitric oxide synthase expression in normotensive rats. Am J Hypertens. 2001;14:155–63.
• D’Elia L, Galletti F, La Fata E, et al. Effect of dietary sodium restriction on arterial stiffness: systematic review and meta-analysis of the randomized controlled trials. J Hypertens. 2018;36:734–43. In this meta-analysis the authors explored the effect of high sodium intake on arterial stiffness.
Todd AS, Macginley RJ, Schollum JB, et al. Dietary salt loading impairs arterial vascular reactivity. Am J Clin Nutr. 2010;91:557–64.
Jablonski KL, Fedorova OV, Racine ML, Geolfos CJ, Gates PE, Chonchol M, et al. Dietary sodium restriction and association with urinary marinobufagenin, blood pressure, and aortic stiffness. Clin J Am Soc Nephrol. 2013;8:1952–9.
Nilsson PM. Arterial stiffness, the metabolic syndrome, and the brain. Am J Hypertens. 2017;31:24–6.
Scuteri A, Najjar SS, Orru’ M, Usala G, Piras MG, Ferrucci L, et al. The central arterial burden of the metabolic syndrome is similar in men and women: the SardiNIA Study. Eur Heart J. 2010;31:602–13.
•• Topouchian J, Labat C, Gautier S, et al. Effects of metabolic syndrome on arterial function in different age groups: the Advanced Approach to Arterial Stiffness study. J Hypertens. 2018;35:000–000. This large prospective multicentre study investigated the effects of age and of the different metabolic syndrome components on arterial stiffness.
van den Munckhof ICL, Holewijn S, de Graaf J, Rutten JHW. Sex differences in fat distribution influence the association between BMI and arterial stiffness. J Hypertens. 2017;35:1219–25.
Lee DC, Sui X, Artero EG, Lee IM, Church TS, McAuley PA, et al. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the aerobics center longitudinal study. Circulation. 2011;124:2483–90.
Swift DL, Lavie CJ, Johannsen NM, Arena R, Earnest CP, O’Keefe JH, et al. Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J. 2013;77:281–92.
Franco OH, de Laet C, Peeters A, Jonker J, Mackenbach J, Nusselder W. Effects of physical activity on life expectancy with cardiovascular disease. Arch Intern Med. 2005;165:2355–60.
American Diabetes Association. Standards of Medical Care in Diabetes—2016. Diabetes Care. 2016;39(Suppl. 1):S1–S111.
Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;64:1929–49.
Palatini P, Graniero G, Mormino P, et al. Relation between physical training and ambulatory blood pressure in stage I hypertensive subjects. Results of the HARVEST trial. Circulation. 1994;90:2870–6.
Cornelissen VA, Fagard RH. Effects of endurance training on blood pressure, blood pressure-regulating mechanisms, and cardiovascular risk factors. Hypertension. 2005;46:667–75.
Fagard RH. Exercise therapy in hypertensive cardiovascular disease. Prog Cardiovasc Dis. 2011;53:404–11.
Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2:e004473.
Theodore RF, Broadbent J, Nagin D, Ambler A, Hogan S, Ramrakha S, et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66:1108–15.
Saladini F, Benetti E, Mos L, Mazzer A, Casiglia E, Palatini P. Regular physical activity is associated with improved small artery distensibility in young to middle-age stage 1 hypertensives. Vasc Med. 2014;19:458–64.
Tan I, Spronck B, Kiat H, Barin E, Reesink KD, Delhaas T, et al. Heart rate dependency of large artery stiffness. Hypertension. 2016;68:236–42.
Tomiyama H, Hashimoto H, Tanaka H, Matsumoto C, Odaira M, Yamada J, et al. Synergistic relationship between changes in the pulse wave velocity and changes in the heart rate in middle-aged Japanese adults: a prospective study. J Hypertens. 2010;28:687–94.
Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K, et al. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation. 2002;105:1202–7.
Courand PY, Lantelme P. Significance, prognostic value and management of heart rate in hypertension. Arch Cardiovasc Dis. 2014;107:48–57.
Messerli FH, Rimoldi SF, Bangalore S, Bavishi C, Laurent S. When an increase in central systolic pressure overrides the benefits of heart rate lowering. J Am Coll Cardiol. 2016;68:754–62.
• Palatini P, Saladini F, Mos L, et al. Low night-time heart rate is longitudinally associated with lower augmentation index and central systolic blood pressure in hypertension. Eur J Appl Physiol. 2018;118:543–55. This study investigated the cross-sectional and longitudinal effect of heart rate on different arterial distensibility parameters.
Dao HH, McMartens F, Zaor A, de Champlain J, Moreau P. Role of endothelin in the hypertrophic remodeling of small arteries induced by exogenous norepinephrine. Arch Mal Coeur Vaiss. 1999;92:1059–62.
Green DJ. Exercise training as vascular medicine: direct impacts on the vasculature in humans. Exerc Sport Sci Rev. 2009;37:196–202.
Maeda S, Sugawara J, Yoshizawa M, Otsuki T, Shimojo N, Jesmin S, et al. Involvement of endothelin-1 in habitual exercise-induced increase in arterial compliance. Acta Physiol (Oxf). 2009;196:223–9.
Tolezani EC, Costa-Hong V, Correia G, Mansur AJ, Drager LF, Bortolotto LA. Determinants of functional and structural properties of large arteries in healthy individuals. Arq Bras Cardiol. 2014;103:426–32.
Pasha EP, Birdsill AC, Oleson S, Haley AP, Tanaka H. Physical activity mitigates adverse effect of metabolic syndrome on vessels and brain. Brain Imaging Behav. 2018; https://doi.org/10.1007/s11682-018-9830-3.
Bohn L, Ramoa A, Silva G, Silva N, Abreu SM, Ribeiro F, et al. Sedentary behavior and arterial stiffness in adults with and without metabolic syndrome. Int J Sports Med. 2017;38:396–401.
Koskinen J, Magnussen CG, Taittonen L, Rasanen L, Mikkila V, Laitinen T, et al. Arterial structure and function after recovery from the metabolic syndrome: the cardiovascular risk in Young Finns Study. Circulation. 2010;121:392–400.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Hypertension and Obesity
Rights and permissions
About this article
Cite this article
Saladini, F., Palatini, P. Arterial Distensibility, Physical Activity, and the Metabolic Syndrome. Curr Hypertens Rep 20, 39 (2018). https://doi.org/10.1007/s11906-018-0837-3
Published:
DOI: https://doi.org/10.1007/s11906-018-0837-3